Author: Lisa-Marie Ryan
October is Breast Cancer Awareness Month
You may notice an increased amount of pink during this month, especially iconic pink ribbons, and it’s for a good reason: October is Breast Cancer Awareness Month.
This annual campaign aims to increase the awareness of the disease and to raise funds for research into its cause, prevention, diagnosis and treatment. With the hope that in the not too distant future, a cure will be found!
Breast Cancer is the most common cancer in the UK. 1 in 8 women in the UK will be diagnosed at some point in their lives.
In the UK, over 55,000 women each year are diagnosed with Breast Cancer which is the most common cancer. Thanks to research, more people are surviving breast cancer than ever before, yet there are still nearly 1,000 women who’ll die of breast cancer each month. Breast cancer is often thought of as something that only affects women, but men can get it in rare cases. It is important for males (especially those over 75 years with a high BMI) to check breast tissue for abnormalities as well.
We will be sharing important information on symptoms, causes and lifestyle alteration you can make to reduce your risk.
We are urging everyone, especially women, to check their breasts regularly and get checked out by a professional if something seems unusual for you.
REMEMBER: The earlier breast cancer is diagnosed, the easier it is to treat and the better the chance of successful treatment.
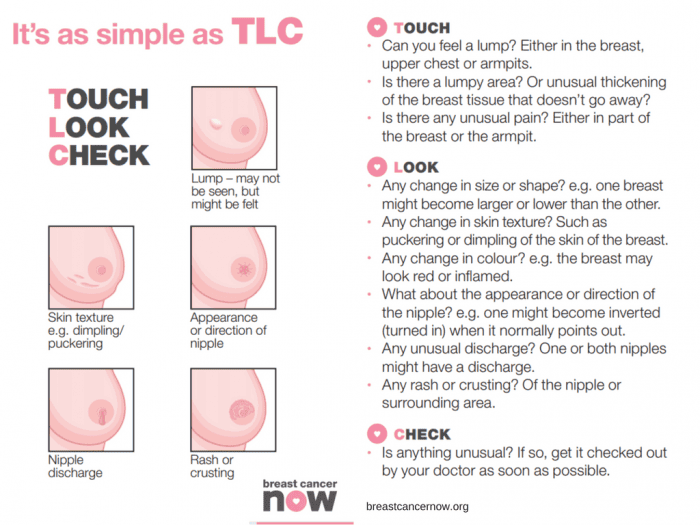
BREAST CANCER SYMPTOMS TO LOOK OUT FOR:
- a new lump or thickening in your breast, upper chest area or armpit
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
- Unexplained pain in your breast or armpit that’s there all or almost all the time
How to check your breasts
Checking your breasts yourself means you’ll get to know what is “normal” for you. As a society we are probably not that familiar with how our body currently is and so that makes it difficult to know what subtle changes happen. It’s most likely that unless a dramatic change has occurred a subtle change will go unnoticed.
So, how do you check your breasts?
There is no special technique and you don’t need any training to start checking your breasts. It may feel like you’re unsure what you’re doing but get to know your body and any breast check is better than no breast check.
The easiest and most accurate way is to divide the breasts into four quadrants; the upper outer quadrant, outer lower quadrant, inner lower quadrant and inner upper quadrant. Examine each quadrant with the flat of your hand. It is important to do this regularly so that you are familiar with what each breast feels like normally. That way, should you notice any changes, (hopefully not), you will pick them up straight away and changes won’t go unnoticed. It is important to remember to check your armpits as well. It is surprising how many breast lumps are discovered after an “axillary” or armpit lymph node is found and checked.
Breast Cancer Now advises the TLC method – “touch, look and check”.
Touch: Can you feel anything new or unusual?
Look: Does anything look different?
Check: Any changes with your GP
You should check your breasts Regularly
Get to know your “normal” by checking your breasts regularly. Get in the habit of checking your breasts at least every month. It can be easier whilst in the bath or shower.
Your breasts can change throughout your life for many reasons – like the menopause, pregnancy and breastfeeding, or puberty. So, if you check them regularly, you’ll be able to spot any new or unusual changes that should be checked out by a GP.
For young and pre-menopausal women it is advised to check mid-cycle (a week after their period finishes) if there are any changes this requires checking with your GP.
As older women are of a higher risk of breast cancer, due to age, it is advised they check even more frequently. Older women should check on a monthly basis without exception. It is advised for men to check also.
Any lump requires attention and checking with your GP immediately.
In addition to regular self-checks, it is important to never miss a mammogram appointment. They may be painful and momentarily uncomfortable, but a mammogram can save your life. If you have a long wait for a mammogram, are unable to access an appointment or just want an additional check, contact the Fleet Street Clinic and we should be pleased to help.
What are the causes of breast cancer?
There are several factors that contribute to increasing your risk of developing breast cancer. There is no single cause, and has to do with our lifestyle, environment and genetics. There are factors which we simply cannot control such as getting older, family history, inherited genes, dense breast tissue, hormones and age at which period started and stopped. However, there are some lifestyle choices that if altered can reduce your risk of breast cancer.
Lifestyle change that will reduce your risk of breast cancer
1. Your weight
Being overweight or obese has a high risk of breast cancer in both men and women (especially after menopause). You can work out your ideal weight using a BMI (Body Mass Index) calculator, this checks your height and weight to see if you are at a healthy weight. For the majority of adults an ideal BMI ranges from 18.5 to 24.9. A BMI between 25 – 30 means overweight. Obesity means a BMI of 30 and above.
2. How much alcohol you drink
Alcohol consumption increases the risk of breast cancer. The risk is greater with each extra unit per day, the latest UK guidelines state no more than 14 units a week.
3. How much exercise you do
Being inactive contributes to a small increased risk of breast cancer, this qualifies as doing less than 150min of moderate activity on a weekly basis. This does not necessarily mean sport and exercise, anything that makes you warmer and out of breath counts.
Throughout October we’ll be highlighting the reasons to support this campaign across our social media platforms. We will be sharing inspirational stories from those who have survived the disease and those who are currently battling. We will also hear from those who have supported a suffering loved one during treatment. Sharing these stories humanises the disease and can provide support/tips for those who may be struggling with a current diagnosis. We will be sharing ways of checking for early warning signs. We’ll also be encouraging all to undertake a Well-Woman or Well-Man health checks. Both of which contain a breast examination.
At Fleet Street Clinic, we specialise in women’s health and have four female GPs on-site to facilitate well-woman health checks. Our Executive Well Woman medical is focused on protecting your well-being and involves a full examination including breast examinations and cervical screen tests. Our comprehensive medical is designed to screen for health problems at the earliest possible stage.
Book Your Well Woman Medical Online. Or if you notice any changes to your breast or have any concerns, you should book a GP appointment as soon as possible.
_______________
To find out more from Breast Cancer Now, visit breastcancernow.org
Holidays are a time to relax, unwind and have fun!
However, this excitement can lead to us making decisions we may not usually make when we are at home. If you have unprotected sex whilst abroad whether it is oral, vaginal or anal you are at risk of catching sexually transmitted infections.
You could be at risk of catching these common STIs: HIV, chlamydia, HPV, herpes, syphilis and gonorrhoea.
What can you do to prevent an STI?
Abstaining from sex is the most reliable way to avoid infection. However, if you wish to be sexually active follow some of the tips below:
- Use a condom from start to finish every time during sex including oral, vaginal and anal.
- Get vaccinated to protect against diseases such as Hepatitis B and HPV.
- Do not assume that your partner is STI-free. Talk openly and discuss your sexual health histories.
- Taking drugs and/or alcohol can lead to bad decisions. Be cautious when having sex whilst inebriated as you are more likely to take risks. These include not wearing a condom or having sex with someone you usually would not.
What are the symptoms of an STI?
Symptoms are different depending on the infection. Some diseases also do not cause any symptoms which makes them very hard to spot. If symptoms do occur, they could be some of the following:
- Pain when you urinate or have sex
- Discharge from the vagina, penis, or anus
- Unexplained rash, sore, or ulcer on your skin, genitals, or throat
- Jaundice (yellow colour of the skin and eyes)
What do you do if you think you have an STI?
Having an open and honest conversation, discussing your sexual health with your doctor is a good start to help guide you towards any tests or medication that you may need.
Long-term problems can be prevented by testing for STIs early and also prevent the spreading to other partners.
If you are worried that you may have an STI you should:
- Not have sex with anyone. This will reduce the risk of spreading the disease to anyone else.
- See a doctor or nurse as soon as possible.
- Discuss your sexual history and international travel with the doctor or nurse as some diseases are more common in some countries.
- If you have a positive result notify your recent partners. They may also be infected and unaware.
Fleet Street Clinic offers a discreet and trusted sexual health service including confidential sexual health advice, instant testing, and comprehensive STI screening.
You can book a sexual health appointment online.
On 14th August 2024, the World Health Organization declared outbreaks of mpox in Africa to be a Public Health Emergency of International Concern.
What is mpox?
Mpox is a viral infection that was previously known as “monkeypox”.
It shares some similarities with smallpox, to the extent that smallpox vaccine may be cross-protective; however, the illness is much less severe. (Waning population immunity to smallpox, since vaccination programmes ended in 1980, is one possible reason for the increased tendency to outbreaks now.)
So far, there have been 14,000 cases reported in Africa, with 524 deaths. Sweden has just reported the first case of clade I mpox outside Africa in the current outbreak (see below).
Previously confined to central Africa, recent outbreaks have ultimately spread globally, which is why the WHO has now decided to urge a concerted global response.
How is it spread?
The infection is spread mainly by close direct / intimate contact with body fluids and secretions, and by sexual exposure.
It can also be spread by contact with animals, or their droppings, or by eating under-cooked contaminated meat – so-called “bush meat”. The animal reservoir of infection is mainly among rodents and non-human primates.
The illness
Infection may be symptomless, but in most cases, symptoms appear 7 to 14 days following exposure.
Mpox is characterised by blistering skin lesions that are often extremely painful (and highly infective to other people), occurring particularly on the skin, genitals and face. They can be sparse, or even single blisters.
Other symptoms include fever, chills, headache, muscle aches, fatigue and swollen lymph glands.
The blisters may appear first on the face, spreading to other parts of the body; or alternatively in the genital area if the infection was acquired by sexual contact. Extensive lesions around the mouth may make eating and drinking painful or impossible, requiring intravenous treatment.
The illness is considerably more serious in people with HIV infection or reduced immunity. Severity of infection is also linked to the degree of exposure.
Mpox strains
There are two strains (called clades – Clade I and Clade II) that differ in severity and ease of spread.
Clade II tends to be more severe (up to 1,000 times more virulent than clade II) and occurs in Central Africa, Clade II occurs mainly in West Africa and may sometimes be more easily transmissible. Mutations into sub-strains is also occurring, which makes testing more complicated, especially in countries where resources are poor.
Where are cases occurring?
It is important to bear in mind that official statistics generally underestimate true numbers of cases, since not everyone with symptoms seeks medical attention, and not all cases undergo full testing.
Laboratory-confirmed cases have been reported in:
- Burundi: over 100 cases (Clade Ib) throughout the country
- Central African Republic: 28 cases (Clade I) throughout the country
- Côte d’Ivoire: 6 cases (Clade II) in Abidjan and Bas-Sassandra districts
- Democratic Republic of the Congo: > 14,000 cases (Clades Ia and Ib) throughout the country, mainly in Équateur, Sankuru, South Kivu, and Sud Ubangi provinces
- Kenya: 1 case (Clade Ib) in Taita-Taveta County
- Republic of the Congo: > 120 cases (Clade I) throughout most of the country, mainly in Cuvette, Kouilou, Likouala, and Point-Noire departments
- Rwanda: 4 cases (Clade Ib); no specified locations
- South Africa: 24 cases (Clade IIb) in Gauteng (12 cases and 2 deaths), KwaZulu-Natal (11 cases and 1 death), and Western Cape (1 case) provinces
- Uganda: 2 cases (Clade Ib) in Kasese District; no secondary transmission has been reported
A previous outbreak in 2022 resulted in spread to over 40 countries – with over 30,000 cases in the USA, for example, mainly in the MSM community.
Are visitors at risk?
Although current news reports of mpox cases are alarming and intended to generate a global public health response, so as to raise awareness and help bring outbreaks under control, most tourists and travellers to Africa are not at risk.
Travel to Africa for the usual tourist activities (e.g. safari, outdoor activities, beach) should be unaffected by the outbreak.
Older travellers who have previously been vaccinated against smallpox may still have some additional cross-protection against mpox.
- Risk arises from close contact (especially sexual contact) with infected people.
- Those at highest risk are men who have sex with men (MSM).
- High-risk behaviour is easily avoided, and safe-sex precautions reduce the risk of infection.
- Risk also arises from close physical contact with infected animals, or by eating under-cooked bush meat – which should be avoided. (Thorough cooking kills the virus.)
- Healthcare workers may be at risk if caring for people who are ill with mpox
- Journalists and news media personnel should avoid physical contact, keep their distance and observe the usual hygiene precautions when reporting on the evolving mpox outbreak situation
Mpox vaccines and treatment
- In the UK, vaccination is available for MSM and healthcare workers via the NHS.
- Current vaccines protect against all strains.
- Vaccination within 14 days of possible exposure also appears to confer protection (post-exposure protection).
- Several antiviral drugs can provide benefit in the most severe cases.
More information:
Oropouche Virus Disease: A growing concern in Central and South America.
As of mid-2024, Central and South America are experiencing a significant outbreak of Oropouche virus disease, impacting countries such as Brazil, Bolivia, Colombia, Peru, and Cuba.
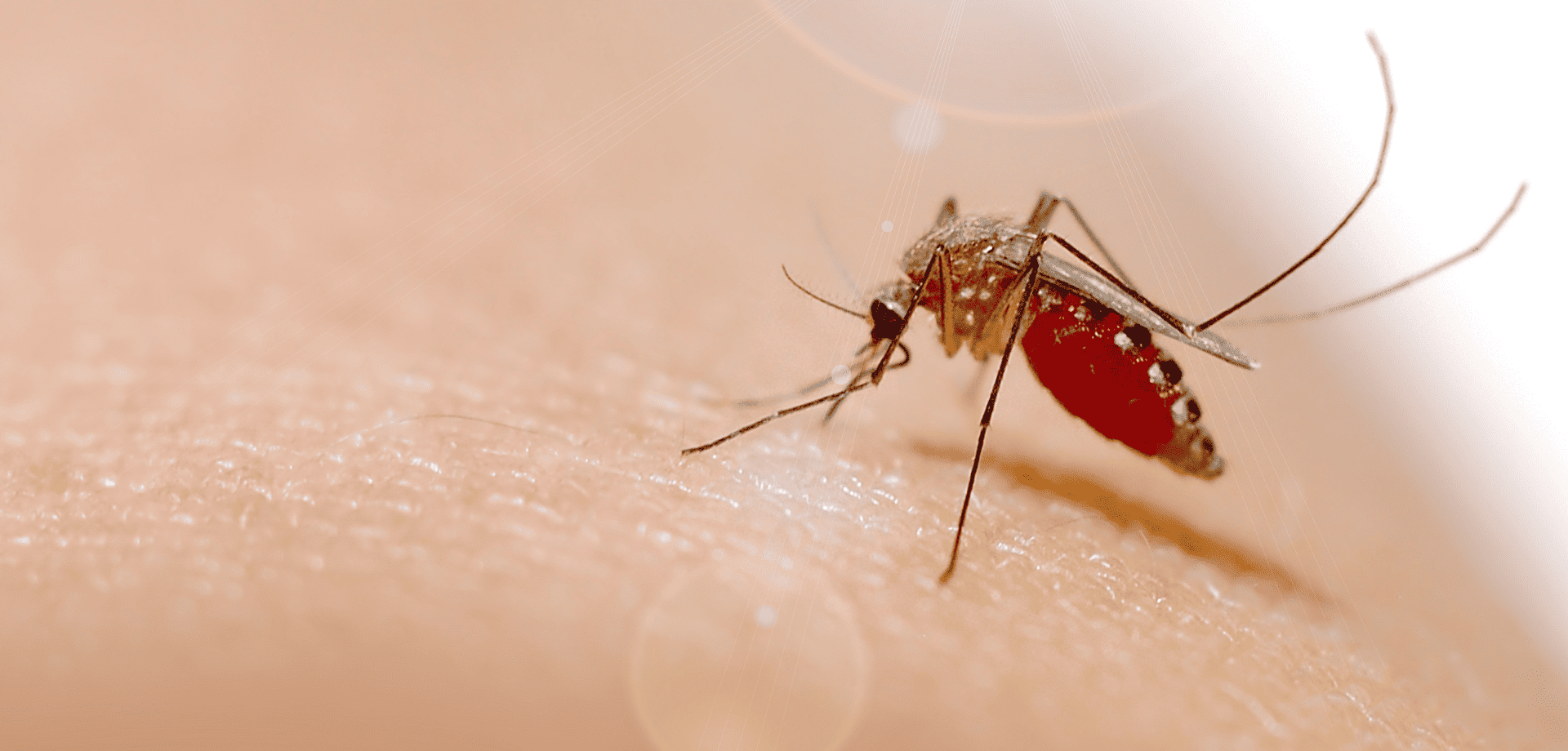
The Oropouche virus is primarily transmitted through the bites of infected midges (Culicoides paraensis) and mosquitoes. The virus is mainly spread in tropical and subtropical regions where these vectors are prevalent.
Symptoms of Oropouche virus disease include:
- sudden-onset fever,
- severe headaches,
- muscle and joint pain,
- rash,
- eye pain,
- nausea,
- and dizziness.
While most cases are mild and self-limiting, lasting 3 to 7 days, some individuals may experience more severe symptoms like meningitis and encephalitis.
There is no specific antiviral treatment or vaccine for the disease, so care focuses on symptom relief, such as rest, hydration, and pain management.
How to protect yourself from Oropouche virus
Preventing Oropouche virus disease involves reducing exposure to vector bites. Unlike mosquitoes, the main vector (midges) lacks a proboscis, and so is unable to bite through clothing.
Covering up, and wearing long-sleeved clothing, is therefore a keyway of preventing infective bites.
Other key measures include using plenty of insect repellent, impregnating clothing with Permethrin insecticide, using bed nets, and staying indoors during peak biting times.
Eliminating standing water where vectors breed is an important public health measure.
Prevention is key!
With no vaccine available, prevention remains the best defence against Oropouche virus disease.
Personal protective measures against insect bites also help protect against dengue, yellow fever, Zika, chikungunya, malaria, and a wide range of other tropical insect-borne infections, and should be followed carefully by travellers to tropical countries.
Cases found in Europe
Spain, Italy and Germany reported infections in numerous patients who had recently travelled to Cuba and Brazil.
The European Centre for Disease Prevention and Control (ECDC) warned of a moderate threat to travellers visiting Brazil, Bolivia, Colombia, Peru and Cuba, where Oropouche virus (Orov) is currently spreading.
If you’ve recently travelled to a known outbreak area and are experiencing any of the symptoms mentioned above, it is important to mention this to your doctor. This will help them rule out an Oropouche virus infection.
Worried about your upcoming travel plans?
Schedule a travel consultation with one of our specialist travel nurses.
They will guide you through potential health risks and recommend the necessary preventive measures and vaccinations to ensure your safety while travelling.
For more information on:
If caught and symptoms develop, rabies is almost invariably fatal.
Rabies is spread through the saliva of an infected animal and is present in over 150 countries worldwide. Up to 100 children die each day from rabies, and more than 55,000 people a year are killed from the disease, mainly in Asia and Africa.
If bitten or scratched by an infected animal you need to act quickly. Your pre-exposure vaccines simplify medical care in case of a potential rabies exposure, reducing the number of post-exposure vaccine doses needed and providing more time to seek medical care because your antibodies will start to respond. This is crucial when traveling to remote areas with limited access to medical facilities.
If you haven’t had pre-travel vaccinations, the treatment is much more complicated; it is also expensive and can be hard to access in lower income countries. If treatment is given correctly and promptly after exposure, it is 100% preventable.
It is extremely important that if you are travelling somewhere with a known risks of rabies it only seems sensible to protect yourself against it. Rabies is a vaccine-preventable disease, so make sure you get vaccinated before you travel.
For more information on rabies and travel health, visit our rabies page here.
The Fleet Street Clinic is passionate about travel. We have provided rabies vaccinations for over 20 years. Our team of expert travel medical professionals provide advice and detailed consultations to ensure you have a healthy trip.
You can book a travel consultation or rabies vaccination appointment online.
ESSENTIAL CHICKENPOX VACCINE FACTS:
- The chickenpox vaccine is not currently given by the NHS, but is part of the childhood vaccination schedule in other countries
- Chickenpox is a highly contagious infection caused by the varicella zoster virus
- In the UK, it mostly affects children
- It can be itchy and uncomfortable, can leave scars, and can sometimes cause severe disease – adults may suffer more serious symptoms, including pneumonia
- Chickenpox is spread by inhaling droplets coughed up by people infected with the virus
- People with chickenpox become contagious about 2 days before the appearance of the rash, which can make it difficult to avoid infection
- The chickenpox vaccine (varicella vaccine) can be administered from the age of twelve months onwards
- Two doses of vaccine are needed, with a 4 week gap between doses
- If your child is receiving the MMR vaccination or a Yellow Fever vaccine, the varicella vaccination must either be given on the same day, or 4 weeks later
HOW TO BOOK A VACCINATION APPOINTMENT
Fleet Street Clinic is dedicated to maintaining a good supply of the chickenpox vaccine.
Our private chickenpox vaccine service is undertaken by doctors and nurses with long experience of vaccinating children. Our family friendly clinic is sympathetic to parents’ needs and concerns, and we welcome any vaccine-related queries. We operate a Saturday vaccination clinic once a month, the next will be held on Saturday April 8th.
To book your chickenpox vaccination for yourself or your child, you can book online now.
Recent media reports have raised awareness of the effects of Meningitis B and the importance of the meningitis vaccine (if your child is aged under 12 months, the vaccine still readily available via your NHS doctor). Less well-known is the fact that there are different strains of Meningitis, with different vaccines protecting against them.
Strains and Meningitis Vaccines:
- Meningitis B: the protective single-strain meningitis B vaccine is Bexsero
- Meningitis A C W Y: the 4-strain vaccines Menquadfi and Nimenrix offer protection.
Meningococcal Meningitis and its Symptoms
Meningococcal meningitis is a bacterial infection that causes inflammation of the protective membranes surrounding the brain and spinal cord. It can affect people of any age, but those most commonly affected are children under 5, and teenagers and young adults heading off to university.
Initial symptoms may be similar to flu, progressing to:
- A high temperature/fever, with cold hands and feet
- Vomiting
- Refusal to eat
- Drowsiness
- Floppy and unresponsive
- Rapid breathing
- Neck stiffness
- Bright light sensitivity
- Pale, blotchy skin, and a red rash that doesn’t fade when a glass is rolled over it
- Convulsions or seizures
Further information: https://www.meningitisnow.org/meningitis-explained/
The specialists at the Fleet Street Clinic recommend getting your children vaccinated not just against Meningitis B, but against Meningitis A,C,W & Y strains as well (the vaccine is currently available and in stock).
Meningitis B Vaccines Availability
We currently have a good supply of Meningitis B vaccine, available on a first come, first served basis. You can book a Meningitis B vaccination appointment online.
Every year, Brits take more than 70 million trips abroad. Most notably for holidays, business trips and to visit family and friends. Whilst the majority of people have a safe trip, some people do experience illness or have an accident. In most cases, minor accidents and illnesses don’t require a visit to a medical centre or hospitalisation and can be self-treated with the help of a medical kit.
Where you are travelling to and the activities you plan to do there will dictate what type of medical kit(s) you would need.
Essential First Aid Kit £27
If you are planning to travel outside of a major city, you’re best to travel with an Essential First Aid Kit. It’s very easy to get scratched, twist an ankle or develop a blister. Particularly if you’re sight-seeing, hiking or even just taking a trip to the beach. Having a few essential supplies handy will reduce the need for a trip to the local chemist. Inside this kit, you will find items aimed at treating minor cuts, grazes, blisters, cleaning wounds, minor burns and sprains.
Worldwide Travellers’ Diarrhoea Kit £29.95
When you travel to a developing country, you have a high likelihood of catching a stomach bug. Also known as traveller’s diarrhoea. This is not always brought on by unsafe water and can be due to a change in diet or the high levels of impurities in the local water that you’re not used to. However, if the cause is a microorganism such as bacteria, parasite or virus, your symptoms may be much more severe and lead to complications. Travelling with a Worldwide Gastro Kit covers all eventualities. Including preventative items, plus medications for common symptoms such as nausea, vomiting, dehydration and travellers diarrhoea.
Sterile Needle Kit £9.50
The adventure traveller is likely to travel to remote areas where medical supplies are not sterilised to a safe standard or medical care in a hospital setting is not available at all. In these scenarios, it is safest to travel with a Sterile Needle Kit. This kit is to be provided to a medical professional to be used for medical emergencies such as a blood transfusion, fluid replacement, general vaccinations or blood tests. This kit is to reduce the spread of diseases such as HIV & Hep B.
Female Health Kit £29.95
There are many female-specific health concerns that may occur whilst travelling. Unfortunately, urinary tract infections (UTI’s) and thrush (yeast infections) are common among female travellers. Therefore travelling with a Female Health Kit is highly recommended.
Travelling with a fit-for-purpose medical kit is not glamorous. However, you’ll be glad you have it if you suffer any mishaps. Saving you time, money and stress involved in finding a local chemist, medical centre or hospital quickly when you are abroad. And if you don’t, then at worst you’ve lost out on a tiny amount of suitcase space.
Before International Travel you should consider a pre-travel consultation with a specialist travel nurse to discuss the health risks at your destination. You can book a travel appointment online or email us for more information at info@fleetstreetclinic.com.
SUMMER TREKKING
Do you enjoy the great outdoors and active holidays? If so, you may be contemplating a trekking adventure. Top summer trekking destinations include Cotopaxi, Ecuador, the Atlas Mountain Range in Morocco, The Ladakh Ranges in India and Mont Blanc in the French Alps.
Fleet Street Clinic offers travel tips for trekkers from Anna Chapman, one of our specialist travel nurses, to help prepare for your holiday and make the most of your adventure.
-
Ensure that you are up to date with vaccinations. It comes as a surprise to most people that vaccination should be considered before hiking in northern Europe. Tick borne Encephalitis is a serious viral infection that causes swelling of the brain. As the name suggests, it is spread by the bite of an infected tick, and it is endemic throughout northern Europe, Russia and China. If you’re heading further afield, to South America or Africa, you may need Yellow Fever vaccination for your own protection, or for border control.
- The most common illness amongst travellers is upset stomachs. Pack hand sanitiser to use when soap and water for hand washing is unavailable. Take water purification tablets if you have not got access to safe water. Medicines such as rehydration salts and anti-motility medicines can be helpful if you do become unwell.
- Most trekking routes are at high altitudes. Understand the effects of altitude sickness. Take time to acclimatise to altitudes and consider taking medication such as Diamox to reduce the severity of acute altitude sickness.
- Look after your feet. Invest in good trekking boots, socks and wear them in before you go. Keep your feet dry when trekking by changing your socks and using foot powder. Zinc oxide tape or Compeed dressings can be helpful if you do get blisters.
- Pack suitable clothing. Trekking in mountain ranges usually involves variable temperatures: Warm days, thin air, strong sunshine and cool nights. Pack breathable clothing, a waterproof jacket and warm base layers. Sun protection is essential, especially in high altitude ranges, so apply the “Slip, Slop, Slap” rule. Slip on a shirt, slop on some sunscreen and slap on a hat.
FLEET STREET TRAVEL CLINIC
Travelling with children can be an enlightening and wonderful experience for the family – creating memories and opening their minds to other cultures and ways of life. But on the flip side it also can be quite daunting, especially if this is your first time travelling with children. The best way to establish a safe travel experience abroad is to take early precautions.
Before Your Travels
When it comes to travelling with children, careful planning and preparation should be considered. It is highly advised to have a travel consultation well in advance of your travels. The travel nurse will make you aware of any travel risks and take into consideration your child’s current wellbeing. Depending on where you are travelling, your child may require certain vaccinations.
These preventative measures will safeguard your child from any diseases or illness.
Your may be advised the following vaccinations:
- Rabies
- Yellow Fever
– Some countries require this as a condition of entry and will ask for proof of vaccination when you arrive into the country. - Hepatitis A
- Typhoid
- Tick-borne Encephalitis
- Japanese Encephalitis
- Hepatitis B
- Meningitis ACWY
- Cholera
All vaccinations require a duration of time following vaccination to reach full protection, usually 10 – 14 days, so factor this time in before your travels. In addition, some vaccinations require a multi-course dose before they are considered effective, such as rabies which requires 3 vaccinations to be considered a complete course. Book a travel consultation early to ensure you have enough time before you travel.
In addition to travel vaccinations it is worth discussing any upcoming childhood vaccinations that could be beneficial to have at the same time so your child is protected against any other common diseases that aren’t necessarily associated with just travel.
If you intend to go to countries with a high malaria risk it is important to discuss antimalarial protection during your travel consultation. Malaria can be fatal and there is a higher risk for children. Antimalarials (malaria tablets) are generally taken for a duration before, during and after your trip and need to be purchased in advance of your travels. There are a number of different types and are suitable for different people so it is important to discuss your options with a travel health expert. The tablets work by ensuring the malaria parasite doesn’t reach unmanageable numbers, keeping you healthy whilst you travel.
Travelling abroad can be exhausting, especially for young children. Jet Lag is known to cause temporary sleep disturbance, which can have an impact on your mental health and other bodily functions. To prepare ahead, The Jet Lag Calculator can tell you how long it will take the body to adjust to your new time zone when you travel – and to adjust back again when you come home.
To undergo a Pre-Travel Consultation, book online or for more information on Travel Health Services.
During Your Travels
Travelling can sometimes result in unexpected situations. For the protection of your child/ren and your family in general, always carry a First Aid Kit. This will reduce your need to seek medical aid for minor accidents or journeys to a chemist, especially if local towns are at a further distance.
When travelling to warmer climates, sun safety is crucial as young children are more vulnerable to sunburn from outdoor activities. To protect the skin apply sunscreen of at least SPF 30, with broad spectrum UVA and UVB protection throughout the day. In addition, hot weather can also pose a risk of dehydration and heat stroke. Ensure you and your child are hydrated throughout the day by drinking water from a safe source. This can be bottled water, boiled water, or water that has been filtered.
To further avoid traveller’s diarrhoea:
- Wash your hands regularly, especially before eating
- Carry an alcohol-based sanitiser
- Keep children from crawling or sitting on the ground
- Avoid swimming in contaminated water
- Don’t swallow any shower or pool water
- Eat raw fruits and vegetables only if washed in clean water or peeled
- Stick to foods that are well cooked and served hot
- Stick to canned or bottled beverages
- Avoid food that has been sitting on a buffet to avoid contamination
We have launched a new, free online consultation for Travellers’ Diarrhoea – by answering a few simple medical questions about yourself, we can check if antibiotics are recommended for your trip. You can pay online and we’ll dispatch them directly to you if you are suitable.
Alternatively, you can have a more comprehensive travel consultation in-clinic with one of our experienced travel nurses.
For more information on the prevention and treatment of Travellers’ Diarrhoea.
The feeling of discomfort from bug bites can truly be a nightmare whilst travelling. Insect bites such as mosquitoes, ticks, biting fleas and kissing bugs can cause pain, irritation and even spread diseases. However, they can be avoided through protective clothing. Our Ultimate Bug Kit has everything you need from repellents to aftercare. Alternatively, you could purchase individual items and create your own kit.
After Your Travels
Travelling can expose your child to certain diseases. If your child falls unexpectedly ill – contact your doctor or emergency services right away. A high temperature/ fever could mean an infection. For most people, travellers’ diarrhoea usually clears up within a few days. However, if your stomach bug has been ongoing for weeks after returning home, then you will need to do testing to investigate the root cause. Viruses, bacteria or parasites all cause similar symptoms but require an entirely different treatment approach. Our Gastrointestinal (GI) Panel PCR test looks for any microbes that are causing your symptoms and can quickly identify the exact cause of your Travellers’ Diarrhoea. Results can be provided in as little as 1-hour, so that accurate and effective treatment can begin straight away.
I picked up Covid early in the pandemic and put my newly acquired immunity to good use by joining the Covid medical team at my local hospital for the weeks that followed. There was a side-effect however: a sense of invincibility that has perhaps made me take less care to protect myself from respiratory viruses ever since.
My luck ran out recently while looking after a group of patients with upper respiratory infections. Not all respiratory viruses are equal: we may call them “colds”, but some varieties are considerably more unpleasant than others.
Using PCR, we can now tell the difference between 22 different bugs with pinpoint accuracy, in about an hour. Mine turned out to be parainfluenza type 1 (there are four serotypes, who knew?) – a nasty virus, more common in the USA and among children.
My bout ranked alongside my experience with Covid: the symptoms lasted over three weeks and included a secondary lower respiratory infection requiring antibiotics to clear.
There’s no vaccine as yet against parainfluenza, but there are vaccines against other important respiratory infections – pneumococcal pneumonia, RSV, Covid-19, a newly-recommended adult top-up against whooping cough, and of course flu.
I shall be having all of these vaccines this winter and will take much greater care to protect myself when those around me have “colds”.
Women between the ages of 25 and 64 are invited for regular cervical screenings where a healthcare professional looks at the health of the cervix to detect any cell changes or abnormalities. However, in 2022-2023, the number of women who attended their cervical screen fell. Nearly a third of the women invited to do their cervical screen didn’t attend their appointments, this is around 4.6 million women, a deeply concerning number, as over 3000 women are diagnosed with cervical cancer each year and 99.8% of those cases are preventable. Prevention is better than curing, and the earlier you are aware of any cell changes, the easier it is to treat.
Why do some women not attend their cervical screenings?
One of our general practitioners, Dr Belinda Griffiths, has found that in her experience women don’t attend their cervical screenings for a number of reasons including: difficulties with taking time off work for a GP appointment, fear of embarrassment, and fear of the process being uncomfortable or painful.
However, to combat these concerns, the NHS has launched at-home HPV kits. Dr Griffiths explains how they work – “The HPV test is highly sensitive so it separates out those who are HPV-positive and HPV-negative. Those who are HPV-negative will be considered ‘low risk’ for cervical cancer and will be asked to do a future test. Those who are HPV-positive will be deemed ‘high risk’ and be asked to attend for follow-up with a clinician whereby they will conduct a cervical screening to check the health of their cervix and investigate if any abnormal cells are present.”
These new tests are the same process as at-home STI tests whereby a simple swab collects the sample from the vagina. Having the option of this sort of test at home removes the fear some women may have surrounding the slightly more intrusive cervical screen.
What is HPV?
HPV (human papillomavirus) is a common virus passed on via skin-to-skin contact, usually through genital contact. There are many types of HPV, most of which are harmless, don’t usually cause any symptoms and the infection will go away on its own. However, others are deemed ‘high risk’ as they can persist and cause cell changes which can lead to cancer. It is thought that these ‘high risk’ HPV strains are responsible for around 80% of cervical cancer cases, making the detection of HPV all the more important.
How can you prevent HPV?
You can be protected from certain HPV strains through vaccination. There are two HPV vaccines currently available in the UK: Gardasil which protects against 4 strains of HPV used in the NHS and the vaccine used here at the Fleet Street Clinic, Gardasil-9, which protects against 9 of the high-risk HPV strains.
When can you be vaccinated against HPV?
The NHS now routinely offers the Gardasil vaccine to girls and boys around age 12/13, before the age people generally become sexually active. However, the vaccination programme only came into full force in 2019, meaning many people are currently unvaccinated. It should be pointed out that adults can get vaccinated at any age and even if you have already been exposed to HPV, the vaccine can still offer protection against other strains to which you have not yet been exposed.
It is a particularly good idea for people to get vaccinated before they attend university or before they go travelling on a ‘gap year’, as these are typically times where young people are more sexually active and therefore more likely to be exposed to HPV.
It is important to note that getting the HPV vaccination most certainly doesn’t mean missing or not participating in HPV tests or cervical screenings. A combination of these preventative measures gives you the highest possible chance of preventing cervical cancer.
Book your Cervical Screen or HPV vaccine online today.
Trusted London clinic now offers private Covid-19 vaccines.
As a trusted name in healthcare for the past three decades, Fleet St. Clinic are proud to announce the expansion of our services to include private Covid-19 vaccination for individuals and businesses alike. We offer the most up-to-date Pfizer Covid vaccines at a cost of £95 per dose.
Covid Vaccinations for Individuals
Until now, Covid vaccination has only been available through the NHS, which has rightly prioritised access those most likely to suffer complications. However, coronavirus infection remains a hazard for everyone, and many other people also wish to be protected. Protection can be especially important for people keen to avoid illness abroad, for people in key occupations, and for those in close contact with vulnerable friends and relatives.
Covid vaccination will now be available year-round for all those who would like to be protected, including those who have not been eligible for NHS care. Whether you need a booster vaccination or would like to consider having the Covid vaccine for the first time, we can help.
Book your private covid vaccination here.
Covid Vaccinations for Businesses
Fleet St. Clinic has provided large-scale flu vaccination initiatives for businesses across the United Kingdom since 1995. These programmes are now being expanded to include long-awaited vaccination against Covid-19. Many of our clients have been keen to protect those in business-critical roles as well as to protect employee health and wellbeing more generally.
Workplace vaccination programmes are offered as a straightforward and fully-managed service, enabling employees to access vaccinations they might otherwise find challenging to obtain. Introducing vaccination against Covid-19 reflects our longstanding commitment to keeping companies and their employees healthy.
Book your private covid vaccination workplace programme here.
Fleet St. Clinic Medical Director, Dr Richard Dawood commented:
“We are delighted to be one of the first medical practices in the UK to offer Covid-19 vaccinations outside the NHS. Now that Covid has transitioned from being a pandemic to an endemic disease, it is important that vaccination against Covid should become as “normal” and accessible as vaccination against other infectious diseases.
As a private, multi-disciplinary medical practice, the Fleet St. Clinic has specialised in vaccines for three decades, delivering hundreds of thousands of doses. Through the pandemic, most of our doctors and nurses volunteered to deliver Covid-19 vaccines in the NHS. We are especially pleased that being vaccinated against Covid-19 can now be a matter of choice for individuals and businesses alike, no longer restricted to those in the most vulnerable groups.”
Pre-Book Your Covid Vaccine
Covid vaccination will become available in March, but you can pre-book your own Covid vaccine or a Workplace vaccination programme, from today. Fill in our online form and we will be in touch with more information.
Pre-book your private covid vaccination programme here.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Full Respiratory Panel PCR Test
What to do if you think your child has measles and when to keep them off school.
Measles cases are increasing throughout England, particularly among children. This highly contagious infection can lead to severe complications for some individuals.
Since there is no specific medical treatment for measles, obtaining vaccination is crucial for the best defence against serious illness. The measles, mumps, and rubella (MMR) vaccine is part of routine childhood vaccinations, meaning most children are already immunised against measles.
If your child has received both doses of the vaccine, it is unlikely that they will contract the virus.
Here, we’ll provide everything you need to know about measles, from ensuring your child’s vaccination to knowing when to keep them away from school.
What are the symptoms of measles?
Measles usually starts with cold-like symptoms, followed by a rash a few days later. Some people may also get small spots in their mouth.
Symptoms of measles usually start to appear 7-14 days after you become infected, which include:
- Runny/blocked nose
- Sneezing
- High temperature
- Sore, red eyes that may be sensitive to light
- Sore throat
- White spots inside the mouth
What does a measles rash look like?
Measles usually begins as flat red spots that appear on the face at the hairline and spread downward to the neck, body, arms, legs, and feet. Small, raised bumps may also appear on top of the flat red spots. The spots may become joined together as they spread from the head to the rest of the body.
What should you do if you think your child has measles?
If you suspect that you or your child might have measles, it’s important to request an immediate GP appointment or seek assistance from NHS 111.
Before visiting the GP or any healthcare facility, make sure to call ahead for guidance.
In the event of a measles diagnosis for your child by a doctor, it is advisable for them to refrain from attending nursery or school for a minimum of 4 days from the onset of the rash. Additionally, they should steer clear of close interactions with infants and individuals who are pregnant or have compromised immune systems.
What is the best way to protect against measles?
The best protection against measles for children and adults is to get both doses of the MMR vaccine.
MMR vaccination is available at Fleet Street Clinic for children and adults who would like catch-up on doses. If you or your child haven’t been vaccinated yet, or have an unfinished course of vaccines, either book an appointment online or contact our reception team on +44 20 7353 5678 to book an appointment.
We can usually accommodate same day appointments.
Alternatively, children receive the vaccine at no cost on the NHS at 12 months and then a second dose at 3 years and 4 months. You may find the NHS vaccination service has a longer wait time that us.
If you prefer a version of the MMR vaccine without pork products, please get in touch, explaining your preference and we will do our best to accommodate. It’s important to note that we would be ordering this product specially for you, so there may be a longer wait time for delivery and prepayment will be required. Either call our reception team on +44 20 7353 5678 or email info@fleetstreetclinic.com
Cold-like symptoms can be an early sign of measles. Should you still send your child to school?
If your child has been vaccinated, it’s very unlikely that they have measles. Check if they have a high temperature or a fever, and if not, we’d advise it’s fine to send your child to school.
Keep an eye on their symptoms and adapt accordingly if they worsen.
When should you keep your child off school or nursery and how long for?
If your child has measles, they should stay off nursery or school for at least 4 days from when the rash first appears and avoid close contact with babies and anyone who is pregnant or has a weakened immune system.
The school will let you know if your child has been in contact with someone who has measles and advise what you need to do.
They may advise people who are more susceptible to contracting the virus, such as unvaccinated siblings to stay away from school for the incubation period to be on the safe side.
The incubation period is the length of time it can take to develop the illness after being in contact with someone with measles. For measles, the incubation period can be up to 21 days.
Anyone, child or adult, who has been vaccinated is unlikely to be considered susceptible.
If you’re not sure whether your child is due a vaccination or has missed a vaccination, you can check their Red Book or contact your registered GP practice for confirmation.
If your child has missed their first or second dose of the MMR vaccine, we’d advise you book an appointment for catch up vaccines. You can book an appointment online.
Should you keep your child off school if another pupil has been diagnosed with measles?
Most children will be protected against measles and there is no need to keep your child off school if they have had both their MMR vaccinations.
Your school will let you know if your child has been in contact with someone with confirmed measles and will advise what the next steps are.
Can I still get my child vaccinated even if they’re older?
Yes. The MMR vaccine is suitable for adults and children, therefore, anyone who has not had 2 doses of the MMR vaccine can book an appointment for catch up vaccinations.
It’s best to have vaccines on time, but you can still catch up on most vaccines if you miss them. Two doses of the vaccine are needed to ensure full protection.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Related Blogs:
Measles outbreak & isolation warning
UTIs can strike unexpectedly, casting a shadow over an otherwise fantastic holiday.
Whether you’re a seasoned traveller or embarking on your first adventure, the risk of urinary tract infections (UTIs) is real and more likely to occur during travel, especially in hot countries.
This blog compiles expert advice and practical tips to empower you to minimise the chances of developing a troublesome UTI during your travels.
1. Stay hydrated
One of the simplest yet most effective ways to prevent UTIs is to stay well-hydrated. Proper hydration helps flush bacteria out of your urinary system, reducing the likelihood of infection.
Aim to drink at least eight glasses of water a day, and avoid excessive consumption of caffeinated and alcoholic beverages, as they can contribute to dehydration.
Bring a reusable water bottle and make a habit of refilling it throughout the day, ensuring you have access to clean and safe drinking water wherever you are.
2. Don’t delay going to the toilet
It can be tempting to “hold it in” during long journeys, delayed or remote travel but putting off going to the bathroom can cause UTIs.
Holding your bladder for too long can contribute to the growth of bacteria in your urinary tract. Since urination flushes bad bacteria out of the bladder before they get a chance to multiply to dangerous levels, going to the toilet as soon as you can means less bacteria are left to sit in your bladder for longer than necessary, reducing your risk of a painful infection.
Remember, maintaining good personal hygiene is crucial in preventing gynaecological infections, particularly UTIs and cystitis. When travelling, it’s essential to prioritise cleanliness. Carry antibacterial wipes to clean your hands before and after using public toilets.
3. Choose comfortable clothing
Believe it or not, your choice of clothing can impact your risk of developing UTIs. Tight-fitting clothes, especially in the pelvic area, can trap moisture and create an environment conducive to bacterial growth.
Opt for loose-fitting, breathable fabrics to allow proper air circulation. Additionally, change out of wet bathing suits promptly to prevent the proliferation of bacteria.
By paying attention to your wardrobe choices, you can significantly reduce the risk of developing uncomfortable infections during your travels.
4. Treat constipation
Exploring new cuisines can lead to various challenges for travellers. While some may grapple with traveller’s diarrhoea, others might experience constipation due to altered eating patterns, dehydration, increased alcohol consumption, and a more sedentary lifestyle.
Unfortunately, constipation increases your risk of contracting a UTI. To mitigate this risk, aim to eat a diet rich in fibre, stay active, and drink plenty of water.
5. Carry a female health kit with you whilst you travel
If you experience any symptoms of a UTI or gynaecological infection, it’s crucial to have medications on hand so you can continue your holiday or travel unaffected.
Carrying a female health kit with you whilst you travel means you can detect and treat your UTI symptoms whilst on-the-go. It contains urine test strips which can confirm if you have a urine infection as well as antibiotics and cystitis relief sachets to alleviate symptoms of inflammation.
Symptoms of a UTI may include frequent and painful urination, lower abdominal discomfort, blood in your urine, a high temperature or lower back pain.
Take our free online consultation to see if you can buy a female health kit online.
Remember, in addition to self-treatment, it’s crucial to seek prompt medical attention, especially if symptoms worsen.
Your travel experience should be memorable for all the right reasons, not marred by the discomfort of a urinary tract infection.
By following these essential tips – from prompt bathroom breaks, to arming yourself with the right travel medicine – you can significantly reduce the risk of encountering a UTI while abroad.
Our female health kits are designed for travel and contain everything you would need to treat and alleviate symptoms for a urinary or gynaecological infection. Begin by completing our free online consultation today.
Whether you’re prone to urinary tract infections, or have never experienced one before, it’s a good idea to buy a female health kit before any trip or holiday and arm yourself against the discomfort and misery of a UTI while abroad.
Fleet St. Clinic is here to support your well-being whilst you travel.
Stay healthy, stay informed, and make the most of your travels!
Related services available at Fleet Street Clinic
Blue Monday happens every year on the third Monday of January. It is supposedly the most depressing day of the entire year, based on a crude calculation of bad weather, long nights, back to work dread and post-Christmas debt.
It does sound very plausible perhaps because we so familiar with the term “January Blues” but Blue Monday is in fact, a myth!
The phrase “Blue Monday” was coined by Sky Travel back in 2005 as a way to encourage people to book their next holiday as something to look forward too. They highlighted all the seasonal negatives to reinforce the benefits of booking a holiday – a clever marketing trick.
But can we really pinpoint the most depressing day of the year?
There is no actual scientific studies that have ever backed up any claims about Blue Monday being true or that there could even be a “most depressing day of the year”. This does make sense because this would be different for each and every one of us based on personal circumstances and the variables are extensive. It did, however, get use thinking about our mood, mental health and overall wellbeing at this time of year.
January is cold, often wet and everyone is trying to shake off the Christmas comedown and get excited about the new year ahead, but the January blues can creep in.
Remember you are not alone, and many people experience a dip in mood this time of year but it is important to identify when the January blues are actually symptoms of depression.
Depression is more than simply feeling unhappy, fed up or low for a few days. It can be long lasting and the symptoms range from mild to severe. Once accessed by a doctor, they will conclude the severity of your depression.
A simplified description follows:
Mild depression will have some impact on your daily life.
Moderate depression has a significant impact on your life.
Severe depression makes it almost impossible to get through daily life.
Sometimes there’s a trigger for depression. Life-changing events, such as bereavement, losing your job or giving birth, can bring it on. Other times, it can be linked with family history; people with family members who have depression are more likely to experience it themselves. But you can also become depressed for no obvious reason. It is quite complex and each person is unique.
There are many symptoms of depression and the combination is unpredictable.
They can be categorised at physiological, physical and social symptoms.
Some examples of psychological symptoms of depression include:
- continuous low mood or sadness
- feeling hopeless and helpless
- having low self-esteem
- feeling tearful
- feeling irritable and intolerant of others
- having no motivation or interest in things
- finding it difficult to make decisions
- not getting any enjoyment out of life
- feeling anxious or worried
- having suicidal thoughts or thoughts of harming yourself
Some examples of physical symptoms of depression include:
- moving or speaking slower than usual
- changes in appetite or weight (usually decreased, but sometimes increased)
- constipation
- unexplained aches and pains
- lack of energy
- low sex drive
- changes to your menstrual cycle
- disturbed sleep – for example, finding it difficult to fall asleep at night or waking up very early in the morning
Some examples of social symptoms of depression include:
- avoiding contact with friends and taking part in fewer social activities
- neglecting your hobbies and interests
- having difficulties in your home, work or family life
The most common symptoms of depression tend to be a low mood, feelings of hopelessness, low self-esteem, lack of energy, problems with sleep and a loss of interest in things you used to enjoy but it can be any number of symptoms listed above.
It’s important to seek help from a GP if you think you may be depressed. The sooner you see a doctor, the sooner you can be on the way to recovery.
For more information on GP services at Fleet Street Clinic, click here.
With every change of season comes a host of different medical issues, and winter can be one of the worst. With colder temperatures, shorter days, and seasonal illnesses circulating, it is one of the harder seasons to keep fit and healthy. There are certain conditions which are known to worsen in the colder months and so it is important to be aware of them and how you can best prepare yourself to keep healthy throughout winter.
These conditions include:
- Asthma
- COPD
- Circulatory disorders, such as claudication, Raynaud’s disease, and chilblains
- Ischaemic heart disease
- Hypothyroidism (if untreated)
- Osteoarthritis and any joint disorder to include rheumatoid arthritis
- Seasonal Affective disorder
- Allergic rhinitis
To reduce the increased risk associated with the above conditions, it is important to have a check up with your GP, ideally in the early Autumn before the Winter months. This will give you the best chance of getting ahead and allowing you to prepare for the coming season. But, if for whatever reason, you were unable to have a check up in Autumn, it is still beneficial to have a check up during the Winter months.
During a check up for asthma and COPD it’s advised to have a peak flow and lung function check. Asthma and COPD are worse in the dry, cold weather, so it is important to make sure you have plenty of your prescribed inhalers. It is best to be prepared rather than be taken unawares by an attack of wheezing. It is extremely important to see a doctor if you develop winter wheezing and are short of breath, especially during the night as this is when asthma and COPD attacks are most dangerous.
Circulatory disorders are worse in the cold weather as lower temperatures constrict blood vessels, increasing the likelihood of pain due to claudication (pain in the calves after walking a certain distance), Reynaud’s (discolouration of the fingertips due to constriction of the blood vessels) and chilblains (small, itchy, red patches on the skin). You can prepare for all of these conditions by obtaining prescriptions for treatment but most importantly, by keeping warm and preparing for the cold.
Ischaemic heart disease is also worse in the cold weather due to the effect of constricting blood vessels. It is important to have a cardiac check to include blood pressure, and if you suffer from angina, to ensure you have the medication to treat this painful condition which is likely to be much worse in the cold weather. Avoiding the extreme cold and wearing thermal clothing may also mitigate against the likelihood of a heart attack or myocardial infarction if you do suffer from Ischaemic heart disease.
If you suffer from Hypothyroidism, it is a good idea to have an annual blood test. Left untreated, hypothyroidism can cause increased sensitivity to cold, which can be particularly unpleasant in winter.
For those with arthritis of any kind, the best way to avoid pain and stiffness in the joints is to keep warm and keep the joints moving. Find more information on Arthritis in Winter here.
If your mood tends to be lower in the winter months, each year, you should have a check up with your GP to discuss Seasonal Affective Disorder (SAD). If you are diagnosed with SAD, consider CBT (Cognitive Behavioural Therapy) rather than medication if you can, and invest in a daylight lamp as these do help.
Allergic rhinitis is another ailment that tends to crop up a lot around winter time. This is diagnosed when you have a persistent nasal discharge. This can occur either as a result of pine or autumnal tree leaf mould, or due to house dust or mould which is often exacerbated by central heating. In this instance, nasal sprays and antihistamines are often required.
Finally, the Norovirus peaks in November until April. This is a really unpleasant vomiting virus which is picked up from contaminated surfaces or foods. To help avoid this nasty bug, always wash hands when handling food and make sure food is washed thoroughly before cooking or eating raw.
If you know or suspect that you might suffer from any of these conditions, please do visit your GP to help you keep prepared. Similarly, if anything new arises you should see your GP as soon as you can; the earlier a health condition is addressed, the easier it is to treat.
In general, an annual medical is a good way to give you a full-body overview of your health, as well as monitor the progression of any existing health conditions. A varied, balanced diet and regular exercise will also be crucial in keeping you generally fit and healthy throughout winter.
For more information on our GP Services.
Book a GP Appointment or an Annual Medical.
Arthritis is a common condition that causes pain and inflammation in joints. It is not a single disease but an informal way of referring to joint pain or joint disease. There are more than 100 types of arthritis and related conditions. There are thought to be 10 million people with some form of arthritis in the UK. It is the most common cause of disability in the UK and can affect people of all ages but it does occur more frequently as people get older.
Common arthritis joint symptoms include swelling, pain, stiffness and decreased range of motion. Symptoms can range dramatically from person to person, with some experiencing mild symptoms with occasional flare ups to those who experience constant debilitating pain everyday. The sad truth is that there is no cure for arthritis, so it is all about pain management and how to best reduce flare ups.
The impact of the weather on the symptoms of arthritis has been debated for many years and people tend to report more arthritis flare-ups in the winter, but the reason why is not specifically known.
Quite often sufferers will state that their symptoms get worse when the weather is damp and cold and some state they are able to tell when the weather is about to change based on their arteritis symptoms worsening.
Even if there is currently nothing to support this scientifically, this doesn’t remove the pain felt by sufferers and so rather than comment on where this is true or not, let’s look at ways to reduce flare ups in winter.
Our top 4 tips:
1. Stay warm
When the temperature drops both inside and outside, dress warmly. Make sure all arthritis prone areas are kept warm.
2. Stay hydrated
Drink plenty of water throughout the day. Even mild dehydration might make you more sensitive to pain.
3. Take warm baths
A warm bath or visiting a heated swimming pool will ease joint pain and comfort you. If you visit a heated swimming pool, gentle exercise will also help your mobility.
4. Stay active
It is now clear that active people experience less joint pain than those who are sedentary. If you are experiencing an arthritic flare then reduce your usual activity (but don’t stop altogether) and use simple anti-inflammatory medication such as ibuprofen if it is safe for you to do so.
Enjoy winter while taking the above precautions for Arthritis.
If you are facing extreme discomfort and pain in your joints due to arthritis, book an appointment with a GP to discuss your options.
In the months since its release in the UK, we have seen a huge demand for the new Dengue vaccine, Qdenga.
For those with experience of the disease, the news of its licensing has been much anticipated and we are proud to be one of the first clinics in the UK to offer the vaccine.
What is Dengue Fever?
Dengue is a viral infection that is spread through the bite of an infected aedes mosquito, a species easily recognisable by its striped legs. It occurs in over 120 countries worldwide, mainly in the tropics and sub-tropics, and is the second most common cause of fever in the returning traveller.
The most seriously impacted regions are the Americas, South-East Asia, and Western Pacific, with Asia accounting for around 70% of the world’s disease burden.
It is also spreading to new areas, including Europe, where outbreaks have been increasing in recent years. Read more about this in our recent blog, Dengue Fever in Europe: Temperature Risk.
Since it is transmitted from person to person, via the mosquito vector, it is of particular concern in populated, urban areas.
What are the symptoms of Dengue Fever?
Whilst most cases are asymptomatic, some will develop a severe flu like illness that can require hospitalisation. In rare cases, this will be life threatening.
Common symptoms include;
a high fever,
severe headache,
pain behind the eyes,
muscle ache,
joint pains,
nausea,
vomiting and rash.
There are four serotypes of Dengue virus; for those infected by one type, a subsequent infection is more likely to be life threatening. The severe type of Dengue usually starts a few days after the initial symptoms began. After feeling a bit better, symptoms suddenly return and can include severe abdominal pain, persistent vomiting and bleeding.
Approximately 1 in 20 patients with Dengue will progress into the severe form of the disease.
Dengue Fever Vaccination
Historically, the only protection we could provide was advice surrounding mosquito bite avoidance. With the arrival of Qdenga, we now have the option of a vaccination which provides safe and effective protection.
Studies have shown Qdenga to offer 80% protection from the first dose, with long term immunity achieved after the second.
Who should get vaccinated?
Qdenga can be safely given to those who have previously had the disease, and it is especially important for this group. We would also encourage frequent or long stay travellers to consider the vaccine. The vaccine is licensed for the prevention of Dengue in individuals from 4 years of age and requires two doses, to be given three months apart.
It is a live vaccine, so it’s not suitable for everyone. To discuss your suitability with one of our specialist travel nurses, please book a travel consultation online, or call our reception team on +44 20 7353 5678.
We can usually accommodate same day bookings and suitable vaccinations can be given within the same appointment.
Related services available at Fleet Street Clinic
Travellers’ Diarrhoea Online Consultation
For further reading
In September 2021, Public Health England released new rules surrounding the timing of BCG vaccination, increasing the minimum age of vaccination to 28 days. This has been implemented in line with a pilot disease screening programme that tests eligible newborns for Severe Combined Immunodeficiency (SCID), the outcome of which becomes available by the time the baby is 6 weeks old. It is important that we wait for the result of this test before giving the BCG vaccine.
What is SCID screening?
All newborn babies in the UK are currently offered blood spot screening (heel prick test) that looks for 9 rare diseases, including sickle cell and cystic fibrosis. The NHS is considering introducing an additional test for Severe Immunodeficiency (SCID), a name given to a group of rare, inherited disorders that cause major abnormalities in the immune system. Affected infants have an increased risk of life-threatening infections and will normally become severely unwell in the first few months of life. Without treatment they will rarely live past their first birthday. About 14 babies a year are born in England with SCID.
The evaluation of this testing, which began on 6th September 2021, is taking place in 6 areas across England and will cover around 60% of new born babies. It is running alongside the existing blood spot screening and the intention is to roll it out nationally once the 2 year evaluation has been made.
Why does this affect the BCG vaccination?
Bacillus Calmette-Guérin (BCG) is a live attenuated vaccine that can cause problems if given to an immunocompromised person. Treatment for SCID is more complicated if the child has received the BCG vaccine, so it is important that if your child has been tested. We wait for a negative result before vaccinating.
What we need from you:
If your child was included in the SCID programme, you will need to provide a letter that confirms the negative result of screening.
If your child was born outside of the programme areas and therefore, not included in the SCID programme, we will need to see a letter confirming this.
In either case, please bring the letter with you to your appointment, as well as your child’s vaccination book.
Nb. If your child was born before 1st September 2021, before the programme was introduced, no letter will be needed.
For more information on:
Other Childhood Vaccinations
RSV is a common and highly contagious respiratory virus that is a leading cause of lung disease. RSV is seasonal, and like other respiratory viruses, its peak incidence is during the winter months each year. It spreads from person to person via droplets, or from infected surfaces or objects. RSV is a virus, so antibiotics are not effective.
Arexvy is a new vaccination designed to protect against lower respiratory tract disease caused by respiratory syncytial virus (RSV). It is an important advance, because no specific treatment for RSV is available, and infection is often severe.
Older adults, and those with underlying medical conditions such as diabetes, heart disease and lung diseases such as asthma and COPD are at the greatest risk of the infection. RSV can exacerbate these underlying conditions and lead to pneumonia.
In the UK, RSV causes more hospitalisations and deaths than flu in those over the age of 60. It is estimated that RSV causes14,000 hospitalisations and an estimated 8,000 deaths in adults 60 years of age and older each year.
Arexvy is a recombinant adjuvanted vaccine for the prevention of RSV is adults 60 years of age and above. It is the only licensed vaccination in the UK that has been authorised for use by the Medicines and Healthcare products Regulatory Agency, meaning at risk adults are now able to be vaccinated against the disease.
Arexvy is as in inactive vaccination and only requires single dose for protection. It can be administered at the same time as other vaccinations including flu, pneumococcal, and COVID.
We are among the first practices in the UK to offer it to adults needing protection.
Step into the realm of Movember, where the Chevron, the Dali, or the Handlebar becomes more than just a style statement – it’s a symbol of men’s health awareness.
Are you ready to join the Mo-gang and make a statement this Movember?
Movember transcends mere facial hair growth; it’s a global movement dedicated to transforming the landscape of men’s health. This renowned charity, a beacon of hope and change, addresses critical issues like prostate cancer, testicular cancer, and mental health and suicide prevention.
In the heart of London, at Fleet St. Clinic, we’re not just embracing the ‘Mo’ spirit; we’re championing the cause of male health. As the statistics reveal, one man succumbs to prostate cancer every 45 minutes in the UK. It’s time to take charge of your well-being and be part of a movement that’s making a difference.
Prostate Cancer –
Our clinic offers a comprehensive Prostate Cancer check, with an experienced doctor committed to your health journey. This thorough examination includes a detailed health discussion covering lifestyle and family history, an internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Early detection is the key, and we’re here to guide you every step of the way.
Testicular Cancer –
Testicular cancer, the most common cancer among young men in the UK, demands attention. Knowledge is power, and understanding the symptoms can be a lifesaver. A lump or swelling, a heavy scrotum, or discomfort in the testicle or scrotum are health signals not to be ignored. At Fleet St. Clinic, we emphasise the importance of awareness and early detection.
Mental Health –
Let’s break the silence surrounding mental health. The Movember Foundation has spearheaded programs globally, fostering resilience and mental well-being in men. It’s not just about growing a mustache; it’s about cultivating conversations that matter.
Now, let’s talk about your health journey with Fleet Street Clinic’s essential men’s health screenings and medicals.
Medical Health Check (From £425) –
Essential
Review your health with one of our experienced GPs. Benefit from a thorough physical examination and carefully selected health checks and blood tests, including thyroid function.
1 hour appointment with a GP – £425
book online
Executive
Check your health from top to toe, with our more enhanced Executive medical, including an audiometry test to assess your hearing, spirometry tests to assess your lung function, and cancer checks and markers.
1.5 hour appointment with a GP – £675
Executive+
For maximum reassurance and peace of mind, consider our most advanced medical. Benefit from advanced health screenings including a sophisticated cardiac (CaRi-Heart) scan, and a bone density DEXA scan.
3 hour appointment with a GP – £3,950
View our medical health checks in more detail and book online.
Prostate Cancer Check (£175)
Prostate cancer is the most commonly diagnosed cancer in men in the UK. Early diagnosis is crucial.
Our prostate cancer check is carried out by an experienced male GP, who’ll conduct a detailed health discussion, internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Swift courier services ensure timely analysis at our nearby pathology laboratory. Our GP will provide you with full support throughout the process and provide aftercare services and referrals if required.
In a world where ‘strong, silent men’ are rewriting their narrative, Movember beckons. Join us at Fleet St. Clinic, where your health is not just a checkup; it’s a commitment to a longer, healthier life.
Book your Appointment now, and let your Mo make a statement for men’s health in London.
We are delighted to announce that Fleet Street Clinic, together with our optical practice, Whitby & Co. have achieved ISO 27001:2022 accreditation for excellent security practice across our business.
ISO 27001 is the ultimate benchmark for businesses to establish, implement, and maintain a strong information security management system.
With ever growing concern around data and cyber security, this achievement gives an additional layer of assurance to our patients and business partners alike, that our data security practices meet independently-assessed world-class quality standards.
ISO 27001 is the globally recognised standard for information security management, and we are proud of our team’s accomplishments.
‘The ISO 27001 certification gives reassurance to our current and future patients and business partners that information and data security has been, and continues to be, of the highest importance – I am proud of the entire team for this wonderful achievement.’
Dr Richard Dawood – Medical Director & Founder
Fleet Street Clinic and Whitby & Co. went through a rigorous audit, addressing risk factors across the business, and ensuring robust cyber security levels and business continuity were in place. This accreditation demonstrates our continuing commitment to risk management, cyber-resilience, digital defence and operational excellence.
Click to view our accreditation certificate.
More information on ISO 27001 accreditation
ISO 27001 accreditation details the requirements for businesses to securely manage information assets and data to an internationally recognised standard. It provides a robust approach for managing assets such as employee details, patient information, intellectual property, financial information and third-party data.
The accreditation requires the business to assess their information security risks, put in place robust security controls and processes, and embed information security management across the organisation.
Achieving accredited ISO 27001 certification demonstrates that a company is dedicated to following the best practices of information security. Additionally, ISO 27001 certification provides an expert evaluation of whether an organisation’s information is adequately protected.
Click to view our private patient services or our workplace healthcare services.
If you have a heart condition you have a greater risk of becoming more seriously ill from flu (seasonal influenza) than the general population. In addition, having the flu can exacerbate pre-existing conditions like diabetes or asthma.
According to the NHS, “every year over 11,000 people in England die from complications caused by the flu virus. Many of these deaths could have been prevented by having the flu vaccination.”
Preventing the flu in the first place is the best option.
The best protection is to have a Flu Vaccine each winter.
What is the flu?
Many people think having influenza, also known as the flu, is like having a bad cold, but in reality flu is a nasty respiratory virus that can make you very unwell. Influenza causes inflammation in the body and can be very serious – sometimes leading to hospitalisation or even death.
There is evidence that heart attacks happen more often during or immediately after an acute inflammatory illness, such as flu.
A flu jab is the best protection against flu.
In general, the flu causes stress and inflammation on the body, increasing blood pressure, heart rate and heart function. This is not good for someone with heart or circulatory problems.
Flu vaccination is strongly recommended for anyone who has ever had a heart attack, stroke or has underlying heart disease. A previous diagnosis of heart or circulatory diseases is considered a high risk factor for complications or even another heart attack, for anyone who becomes ill with flu.
Does flu affect heart medication?
If you take warfarin, flu symptoms can affect your blood clotting rate (INR). You should speak to your doctor if this happens so they can monitor your situation closely. It does also mean if you do become unwell, it may take you longer to recover than the average person.
In addition, some over-the-counter flu medicines can’t be used when taking medicines for heart conditions, so contact your doctor before taking things like painkillers and cough medicines. It is better to check before beginning any new medications.
When is the best time to get the flu jab?
Flu vaccinations become available from mid to late September, and through the season until February. It’s best to get your flu vaccine in September or October. The peak time for catching flu runs from Christmas to Easter. The aim is to be vaccinated before flu transmission starts, and to allow at least a couple of weeks post-vaccination, for maximum immunity to develop. The sooner you have the vaccination, the sooner you will be protected.
You can book your flu jab online.
We have a range of flu vaccinations available, including the premium recombinant vaccine, cell-based vaccine, FluAd (for those aged 65 year and older), kids nasal spray and the standard flu jab.
It is important to have a flu jab every year because the flu virus can change. There are many strains of flu already and some are more dominant than others. Each year strains are analysed to determine which strains are likely to be the prevalent strains circulating that year. They can vary year to year so relying on a past vaccination for protection is risky. The previous year’s vaccine may not offer you the right protection against the strains in circulation this year.
In addition, immunity to flu decreases over time. Exposure to the flu virus strengthens the immune response and offers natural protection. With less flu circulating over the past few years due to covid restriction measures, natural immunity in the general population will have decreased.
A flu vaccine will boost immunity.
With most workers now returned to the office and social distancing restrictions long gone, there is a greater chance of the flu spreading and more people falling ill this winter. With both illnesses circulating around it is highly recommended to reduce the risk by getting the flu jab.
Protect yourself against the flu.
You can find more information on the types of flu vaccines available.
For more information on the premium recombinant flu jab.
_____________
Wanting to book a Workplace Flu Vaccination Programme?
Flujabs.org is part of Fleet Street Clinic and has been providing workplace flu vaccinations to UK businesses for many years.
Fill out the online form and one of our flu coordinators will get back to you with current availability and costs.
Some infections can harm your baby if you catch them during pregnancy. Research suggests that the flu, in particular strains such as H1N1 (swine flu), can significantly increase the risk of complications to expecting mothers and their unborn babies.
Vaccinating expecting mothers against flu or before pregnancy can provide the newborn baby with significant ‘passive’ protection – which can last several weeks after birth. This is important because babies cannot be vaccinated themselves until they are 6 months old. So, a mother’s vaccination is strongly advised.
Fleet Street Clinic are urging all the mums-to-be to have the vaccine. The Quadrivalent Flu Jab can be safely given at any point during pregnancy.
Pregnant women are less able to fight off infections and therefore more likely to be seriously ill if they contract the flu virus. Pregnant women are at risk of complications from the flu at any stage of pregnancy. So therefore, it is important for those expecting to get their flu jab as early as possible.
If you are currently planning your pregnancy, it would be sensible to consider getting your flu jab prior to becoming pregnant.
The flu vaccine can safely be given to pregnant women at the same time as the whooping cough vaccine. You can have the whooping cough vaccine from 16 weeks onwards.
The vaccine is inactivated, and cannot cause flu itself.
Having the flu vaccine is the best protection.
If you are interested in booking flu vaccinations for your staff, visit flujabs.org for more information and to get a quote.
STUDENTS URGED TO GET VACCINATED BEFORE UNIVERSITY
The UK Health Security Agency (UKHSA), formerly known as Public Health England, is encouraging students to get vaccinated before they start/ return to University to protect themselves against a range of life-threatening illnesses.
Starting university and attending Fresher’s Week exposes students to a host of viruses and bacteria – some of which for the first time.
First year or returning students can be at increased risk of serious diseases such as meningitis, septicaemia and measles as they mix with large numbers of other students from around the country and overseas.
We strongly advise the following 3 vaccinations at a minimum for students:
Meningococcal ACWY (MenACWY)
– Protects against 4 common strains causing meningitis and septicaemia
Measles, Mumps and Rubella (MMR)
– Protects against measles, mumps, rubella
Human Papillomavirus (HPV)
– Protects against HPV-related cancers including cervical, penile & throat cancers, alongside protection against genital warts. HPV vaccination is estimated to prevent up to 90% of HPV-related cancers.
Meningitis Vaccinations:
– Meningococcal ACWY (MenACWY)
– Meningococcal B (MenB)
UKHSA vaccine coverage data shows around 1 in 8 new students going to college and university this year remain unprotected against these 4 strains of meningococcal bacteria, each of which can cause long term disability, serious health complications and can be life threatening.
The MenACWY vaccine is given by a single injection into the upper arm and protects against four different strains of the meningococcal bacteria that cause meningitis and blood poisoning (septicaemia): A, C, W, and Y. You can book online.
The MenB vaccine is also given as an injection to the upper arm but is a 2-dose course for full protection. It protects agains the B-strain of the meningococcal bacteria. You can book online.
Cases of meningitis, particularly virulent strain Men W & Men B, have been rapidly rising amongst students since 2009.
What is Meningitis W?
Meningitis is a bacterial infection of the protective membranes surrounding the brain and spinal cord. Meningococcal meningitis (Men W) is a highly serious form of bacterial meningitis that can lead to septicaemia. It is spread by droplets that come from a person who is infected with the bacteria.
Although the strain is most likely to affect babies, statistics reveal that older children, teenagers, and adults are also at risk. In recent times, cases amongst normally healthy teenagers have spiked and the fatality percentage is higher with Meningitis W than it is with the most common strains, Meningitis B and C.
Meningitis can progress quickly leading to blood poisoning (sepsis), which can kill within 24 hours. So, it is important to know the signs and symptoms of meningitis and septicaemia (sepsis).
Early symptoms of Meningitis include:
- headache
- a high temperature (fever)
- being sick (vomiting)
- a rash that does not fade when a glass is rolled over it (but a rash will not always develop)
- a stiff neck
- a dislike of bright lights
- cold feet and hands
- or muscular pain
Sepsis is a life-threatening reaction to an infection. It happens when your immune system overreacts to an infection and starts to damage your body’s own tissues and organs. Symptoms can be vague but include:
- acting confused, slurred speech or not making sense
- blue, pale or blotchy skin, lips or tongue
- a rash that does not fade when you roll a glass over it, the same as meningitis
- difficulty breathing, breathlessness or breathing very fast
Many people confuse the symptoms with just a hangover or freshers’ flu, which is one of the theories as to why students are so high-risk. So, check-in on your friends who are unwell. Symptoms can progress rapidly so urgent action in getting medical attention is critical – call NHS 111 straight away
Protection against this strain of Meningitis W is provided through the Meningitis ACWY vaccine. Only one dose is required.
We also carry an excellent stock of the Meningitis B vaccine and can provide both vaccinations at the same time should you require it.
Book your MenACWY & MenB vaccination appointment online
Measles, Mumps and Rubella (MMR) Vaccination
Mumps is a highly contagious viral infection which is spread in the same way as the flu. Coughing, sneezing and kissing can rapidly spread the infection, especially in the close quarters of student accommodation.
Measles is a very infectious viral infection which is also spread by coughing and sneezing. There have been multiple outbreaks of Measles around the world including the UK this year, so it’s important to make sure you are protected as you socialise with new peers.
Both Mumps and Measles can be prevented by safe and effective vaccination, MMR.
Book your MMR vaccination appointment online
Human Papillomavirus (HPV) Vaccination
HPV is a common virus that is passed on via genital contact. There are more than 100 HPV types which infect genital areas. Sometimes they cause no harm and the infection can go away on its own. However, the virus can persist and cause cells to change which can lead to some forms of cancers; cervical, head, neck & throat or genital warts. More information on HPV can be found here.
The HPV vaccine is offered at our clinic for girls and boys to protect against HPV-related cancers and genital warts. Book your HPV vaccination appointment online
Other vaccinations that we recommend for students starting/ returning to University are:
Fresher’s Flu:
Every year different flu strains circulate and infect millions of people. Being exposed to a new pool of infections in University accommodation can increase the risk of catching the flu. Having the flu jab before you go to University will help protect you against the flu and stop you getting sick.
Flu jabs become available from 3rd September and can be booked online.
BCG:
If you are from outside the UK, you should be vaccinated against tuberculosis (TB) before you enter the UK. A weakened strain of tuberculosis, the BCG Vaccine, is injected to protect against the infection. Those unsure of their immunity can have a simple Mantoux test to confirm.
Book your BCG vaccination or Mantoux Test appointment online
Tetanus:
Tetanus is a rare condition caused by bacteria entering a wound. We recommend making sure you are up to date with your DTP vaccinations and boosters before leaving for university. This vaccine protects against tetanus as well as Diptheria and Polio. Don’t let a cut or burn ruin your freshers week.
Book your Tetanus vaccination appointment online
Wellness VACCINATIONS AT FLEET STREET CLINIC
Fleet Street Clinic offers a friendly environment and a team of experienced medics to administer all wellness vaccinations. We meet rigorous quality management standards to ensure we offer you the highest standards of clinical care: you can feel confident you are in safe hands.
Secure your peace of mind by ensuring you are protected. Get your vaccines before university starts to receive protection in time.
Book your vaccination appointment today
_____________
For the full The UK Health Security Agency (UKHSA) statement, click here.
Recombinant Flu Jab – The Most Advanced Protection from Influenza
In a world constantly battling the threat of infectious diseases, the importance of vaccinations cannot be underestimated. Influenza – the flu – is a year-round, global respiratory threat that remains a constant concern, owing to the ability of flu viruses to mutate rapidly and cause seasonal epidemics.
As science advances, so does our ability to protect ourselves from flu. Applying recombinant technology to flu vaccines is a remarkable breakthrough that has created a new generation of premium vaccines, capable of delivering enhanced protection.
Why are recombinant flu vaccines the premium offering in comparison to other flu vaccines?
Traditional flu vaccines are created by growing influenza viruses in chicken eggs, allowing the viruses to replicate, and then inactivating or weakening them for use as vaccines. This process, while effective, presents several challenges, including the potential for the virus to mutate during replication in eggs.
Recombinant flu vaccines offer an innovative alternative to these traditional methods. Instead of using live viruses, these vaccines utilise genetic engineering techniques to produce specific proteins found on the surface of the influenza virus. These proteins are then harvested and used as the key components in the vaccine.
Notably, recombinant flu vaccines eliminate the need for egg-based production, thus addressing concerns related to egg allergies and the risk of viral mutations.
Key benefits
Precise Targeting: Recombinant flu vaccines consist only of precise copies of the surface antigen proteins that flu viruses use to enter our cells. This enables the immune system to recognise and remember them, ensuring the most robust immune response possible whenever flu viruses are encountered.
Enhanced Effectiveness: The genetic engineering process in recombinant vaccines ensures a high degree of consistency and purity in the vaccine components. This consistency translates to enhanced vaccine effectiveness, reducing the risk of a mismatch between the vaccine strains and the circulating flu viruses.
Reduced Allergic Reactions: Individuals with egg allergies often face a dilemma when considering traditional flu vaccines, as these vaccines are cultivated in eggs. Recombinant flu vaccines eliminate this concern, providing a safe option for those with egg allergies.
Forward-Thinking Defence: The adaptability of the flu virus demands a vaccination strategy that can keep up with its mutations. Recombinant vaccines, designed with a focus on the virus’s evolutionary genetics offers a forward-thinking defence by stimulating immunity against a broader range of potential viral strains.
Broader Accessibility: Traditional flu vaccine production is dependent on the availability of fertile chicken eggs and a lengthy production process. Recombinant vaccines overcome these limitations, allowing for more rapid production and distribution, even in situations where egg supplies are compromised.
So, why choose a recombinant flu jab over a traditional standard fu jab?
In the fight against influenza, staying ahead of the mutating virus requires cutting-edge solutions. Recombinant flu vaccinations represent a quantum leap in our approach to flu protection, offering a targeted, effective, and forward-looking defence against the ever-changing flu strains.
As technology continues to evolve, these vaccines hold the promise of becoming the gold standard in flu protection, providing individuals with a safer, more reliable shield against this seasonal threat.
So, when the flu season comes around, consider the power of recombinant flu vaccinations—the premium offering for your ultimate flu protection.
Private Patients
For more information on our flu vaccinations and pricing.
Workplace Flu Vaccination Programmes
Fill out the form below for a quote for flu jabs for your employees.
______________
RELATED SERVICES AVAILABLE AT FLEET STREET CLINIC
In today’s health-conscious era, prioritising well-being has become a central focus in our lives. However, understanding just how fit we truly are requires a comprehensive approach.
A medical check-up is the optimal method for obtaining a holistic view of your overall health. Familiarising yourself with essential health indicators can play a pivotal role in preventing potential illnesses and diseases.
Here’s a breakdown of key health numbers that can provide valuable insights into your well-being:
- Body Mass Index (BMI):
- BMI, frequently mentioned in the media, is a straightforward index of weight-for-height. It classifies individuals as underweight, overweight, or obese based on the ratio of their weight to the square of their height in meters.
- Resting Heart Rate:
- Your resting heart rate serves as an indicator of your basic fitness level and is a reliable predictor of cardiovascular health. Monitoring this metric can offer valuable insights into your overall well-being.
- Waist to Hip Ratio:
- The distribution of body fat, especially around the abdominal area, can impact health significantly. Research suggests that fat stored in this region may contribute to heart disease, obesity, and diabetes. Understanding your waist-to-hip ratio is crucial for assessing this risk.
- Cholesterol:
- Surprisingly, over half of all UK adults have elevated cholesterol levels, and a cholesterol test is the only definitive way to ascertain if you are affected. High cholesterol is linked to heart disease, a prevalent cause of mortality in the UK.
- Blood Pressure:
- Elevated blood pressure places additional strain on your arteries and heart, potentially leading to severe health issues such as heart attacks, strokes, kidney disease, or dementia. Regular blood pressure tests are essential for early detection and preventive measures.
- Blood Sugars:
- Monitoring your blood sugar levels is critical for identifying diabetes or the risk of developing it. For type 2 diabetes, often associated with lifestyle factors, early detection allows for dietary adjustments that may prevent the need for medication and even avert the onset of the disease.
- Bone Density:
- Bone density testing, a non-invasive procedure known as bone densitometry or a bone mineral density scan (BMD), provides insights into the strength of your bones. This assessment can reveal potential risks of osteoporosis, guiding proactive measures for bone health.
- Mammogram/Prostate Check:
- Depending on age, routine checks like mammograms for women and prostate checks for men are advised by healthcare professionals. These screenings are crucial for early detection of tumors or cancerous cells, significantly improving the chances of successful intervention.
If you’re interested in discovering your health numbers, consider booking a comprehensive medical check-up or consulting your GP to determine which medical is best suited for you.
Prioritising these assessments can empower you to take control of your well-being and make informed decisions about your lifestyle.
Hajj and Umrah are religious pilgrimages to Mecca, Saudi Arabia. Hajj is a mandatory Pilgrimage for every Muslim to take once in their lifetime, given that the individual is physically and financially able.
It takes place in the last month of the Islamic calendar and is taken annually by 2.5 million Muslims worldwide pre-pandemic. Whereas, Umrah is a shorter pilgrimage to Mecca taken any time of the year.
Muslims from all over the world gather annually in Mecca in a display of unity, faith and solidarity. Due to the large number of participants performing the pilgrimage there are some health risks you should be aware of.
There are also health requirements set by the Health Ministry of Saudi Arabia that you could affect your VISA. It is good to be aware of those requirements before travelling.
COVID-19 Requirements:
Ministry of Health KSA states that in order to perform Hajj pilgrims, one must have the proof for the following:
- A full course of COVID-19 vaccinations (second dose of a two dose vaccine or received a single dose vaccine) approved by the Saudi Ministry of Health. The approved vaccines’ list can be found here – Ministry of Health Approved Vaccines.
- There is no longer a requirement for PCR testing to perform Hajj or to enter KSA.
Vaccine Requirements:
A pre-travel consultation should be scheduled at least 4 weeks before your trip.
Any mandatory or advised vaccinations will be discussed with a nurse and can be given in the appointment. Follow up doses can also be arranged in the appointment.
Before travelling to Hajj or Umrah, it is recommended that pilgrims be up-to-date with all of their wellness vaccinations.
– Meningitis
All British citizens travellers performing Umrah or Hajj are required to submit a valid Meningitis ACWY vaccination certificate in order to obtain a visa. The MenACWY vaccine protects against meningitis (strains A, C, W & Y) and sepsis. Adults and children over the age of 2 are required to have the vaccine and provide evidence of immunisation no less than 10 days before you plan to arrive in Saudi Arabia. This requirement also applies to seasonal workers in Hajj areas.
You may also want to consider Meningitis B vaccine – this is not a mandatory VISA requirement.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Covid-19
All travellers must be vaccinated against Covid-19 to perform Hajj Pilgrim. The vaccines that are approved by the Ministry of Health KSA can be found here – Ministry of Health Approved Vaccines.
– Polio
Travellers from countries reporting positive environmental sources samples of circulating vaccine derived polio virus 2 (cVDPV2), including the UK, are recommended to be vaccinated with at least one dose of IPV within the previous 12 months and at least four weeks prior to arrival, however there is no polio vaccination certificate requirement.
A polio certificate requirement will only apply to UK pilgrims if they are travelling to KSA via a country reporting WPV1, cVDPV1 or cases of cVDPV2 or Acute Flaccid Paralysis, and not if they are travelling directly to KSA from the UK.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Flu Vaccine
Since both Hajj and Umrah both pose crowded conditions and close contact, seasonal flu vaccination is advised, especially for those who are more vulnerable to severe influenza diseases. This precautionary measure will help reduce the potential spread of the flu.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Hepatitis B
Hep B is spread by contaminated blood and bodily fluid. Pilgrims who intend to shave their heads as one of the rites of Hajj should consider taking the vaccination. Although licensed barbers performing head shaving are obliged to use a new blade for each pilgrim, unlicensed barbers may not adhere to this practice. Vaccinations require 3 injections to be given over a 3 week period and can be given from birth.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Rabies
Rabies is spread through the bite of an infected animal such as cats, dogs, monkeys and bats. Saudi Arabia is classified as a high-risk country for rabies. Full protection is achieved with 3 doses – 3 vaccinations usually given over a 3 week period, however, we do offer a rapid course which can achieve full protection in 7-days. The rabies vaccine can be given from birth.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
TRAVELLERS’ DIARRHOEA
Travellers’ diarrhoea can occur in up to 60% of travellers. Although most cases are mild, taking sensible precautions with food and water can reduce the risk. Carrying medicines for self-treatments is useful such as antibiotics – take our Online Travellers’ Diarrhoea Consultation to see if it is suitable for us to prescribe you standby Travellers’ Diarrhoea treatment.
The best protection are preventative measures such as drinking bottled or purified water, washing your hands thoroughly and frequently and eating well-cooked, hot food.
Fore more information on Travellers’ Diarrhoea.
CLIMATE HEALTH
Saudi Arabia has had some of the hottest temperatures on record this year. Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes which can cause rapid dehydration. This can result in heat exhaustion or heat stroke which can be life threatening if not dealt with promptly.
Heat related illness can be avoided by the following:
- Seek shelter and shade during the middle of the day (11am-3pm) when temperatures are the hottest
- If you are outside, ensure you protect your skin against the sun with high factor sun cream
- Wear loose fitting, lightweight and light colour clothing
- Keep hydrated by drinking plenty of fluids
- Ensure you are taking sufficient salt in your diet (sweating leads to electrolyte and salt depletion)
- Avoid caffeine and alcohol, which can worsen heat related illnesses
GENERAL HEALTH:
Both Hajj and Umrah pilgrimages require strenuous effort, it is worth considering having a full body medical check up before you travel to ensure you are in good health. To prepare for the miles of walking, try increasing your physical activities to improve mobility and movement. In case of unforeseen circumstances, remember to pack a first aid kit and extra supplies of any prescribed medication you are currently taking. We have an onsite pharmacy if you’d like to purchase any of these items during your appointment, speak with your GP or nurse whilst at the clinic.
DENGUE AND MALARIA:
Dengue is spread by day-biting mosquitoes and Malaria by mosquitoes that are active at night. You can reduce your risk of insect bites by using effective insect repellents and protective clothing. You can also sleep under a mosquito net that is impregnated with insecticide to have a peaceful sleep.
If you require complete protection from bugs and mosquitoes, you can check out our ultimate bug kit here.
Delaying your period:
If you decide you would like to delay your period for pilgrimage, you can do so by taking hormonal medication. In advance of your trip, book an appointment with a GP to discuss your options as soon as possible.
When you get home:
If you return home unwell it is important to book an appointment with a GP to determine the cause. If your symptoms worsen or becoming life-threatening do not wait to see a doctor, go straight to A&E for urgent medical care.
If you return with a stomach bug or persistent travellers’ diarrhoea, you may want to consider booking a Gastrointestinal (GI) Panel PCR test – it looks for any microbes (bacteria, viruses & parasites) that may be causing your symptoms and can quickly identify the exact cause. Results can be provided in as little as 1-hour, so that accurate and effective treatment can begin straight away. Firstly, you need to book a GP appointment, express your interest in a GI PCR test and they will advise whether you are suitable or not.
Dengue Fever has been in the news following two cases linked to travel to the Spanish island of Ibiza. This has sparked concerns about the spread of mosquito-borne illnesses in Europe, which is especially unusual for this time of year.
Dengue fever is a viral infection transmitted by the Aedes mosquito, which is found in tropical and subtropical regions worldwide. With rising temperatures and changing climates, there is a risk of mosquitoes and other disease vectors spreading to new areas, potentially causing outbreaks of diseases such as dengue fever.
The two cases of dengue fever in Ibiza were reported by the Spanish Ministry of Health and were both in residents of Germany who had visited the island before becoming ill. Each case was accompanied by two family members who were also suspected to have had dengue fever.
The risk of dengue fever in Spain is highest between the months of May and November, when mosquitoes are most active so to have cases at this time of year is uncommon.
So, why are we seeing cases outside of the usual infection months?
The reason is multi-facetted.
Our medical director and travel health specialist, Dr Richard Dawood explains:
“Firstly, there is the introduction or spread of mosquitoes to “pastures new” – places that might have been previously inhospitable, perhaps through temperature; or alternatively, that offer an environment with plenty of suitable breeding sites that they are suddenly able to take advantage of. These mosquitoes can bring disease with them, or can spread it around if there is a reservoir in the local population.
Secondly, there is the possibility of introducing disease to a vector population that is already established, ready and waiting. This is exactly the (long-standing) concern with yellow fever. There are mosquito species in Asia, for example, that are easily capable of spreading yellow fever were it to be introduced by an infected traveller – which is why Asian countries are so careful to insist on proof of yellow fever vaccination from travellers arriving from the endemic zones of Africa and South America. Asia is yellow fever-free, and wants to remain so. However, this type of introduction has already recently happened in Australia, where Japanese encephalitis (a virus infection that can cause rare but serious complications in humans) has recently established a reservoir of infection in farm animals, that may be impossible to reverse. It is also happening with Lyme disease spreading gradually into parts of Europe (and the UK) with a susceptible tick population.
Similar concerns apply to Zika – there is very large potentially susceptible mosquito population that could spread the virus in many tropical countries, if introduced; dengue fever; and also potentially malaria, in parts of the world that have been the target of successful elimination campaigns, but where mosquito populations could still spread it, were it to be reintroduced, if control measures are neglected or ceased.
With changing climates, a valid concern about global warming is that it could create conditions in which populations of mosquitoes and other vectors thrive and spread – hence the crucial importance of vigilance, surveillance, and early action if needed.”
How can you protect yourself from Dengue Fever?
QDENGA, Dengue Fever Vaccination
Relatively new to the UK, QDenga is a new travel vaccine that can prevent dengue fever.
The course consists of two doses, given three months apart, and provides long lasting protection.
Learn more about QDENGA, Dengue Fever Vaccination
Book a travel consultation for your Qdenga vaccination.
Avoid Mosquito Bites
In addition to vaccination, the best way to protect yourself against dengue fever is to take measures to avoid mosquito bites. This includes wearing protective clothing, using mosquito repellent, and staying in places with air conditioning or screens on windows and doors.
If you develop a high fever during or after travelling to an affected area, seek medical advice as soon as possible and provide details of your recent travel history. Dengue is often also accompanied by a rash and joint or muscle pain.
In conclusion, rising temperatures and changing climates have the potential to create conditions in which populations of mosquitoes and other disease vectors thrive and spread. It is crucial for public health authorities to remain vigilant and take early action if needed to prevent the spread of diseases such as dengue fever.
By receiving the Qdenga vaccine and implementing effective measures to prevent mosquito bites, travellers can lower their personal risk of contracting Dengue Fever, along with other insect-borne diseases.
If you’re considering Qdenga before your next trip, book a travel consultation with one of our specialist travel nurses.
Related services available at Fleet Street Clinic
QDENGA, Dengue Fever Vaccination
Suitable Medical Kits available to buy online
Related Online Consultations
Female Travel Health Kit: Start Consultation
HIV (Human Immunodeficiency Virus) is a viral infection that damages cells in your immune system. As a result, it weakens the body’s ability to fight off everyday infections such as the common cold. If you have HIV and get sick with a cold, you are much more likely to experience complications, such as developing pneumonia.
HIV is found in the body fluids of an infected person, such as semen, vaginal and anal fluids, blood and breast milk. It is not found in sweat, urine or saliva. Meaning HIV is typically spread by unprotected sex, the sharing of injecting equipment such as needles, and/ or passed from mother to baby either through birth or breastfeeding.
About National HIV Testing Week
National HIV Testing Week #HIVTestWeek aims to raise awareness of HIV and AIDS. It is an annual national campaign to encourage people to get tested for HIV regularly to reduce the number of people who are diagnosed late or remain undiagnosed.
Out of the 106,890 people in the UK with HIV, 1 in 20 of those do not realise they are HIV positive. Which is why it is so important to make sure everyone gets tested to know their status.
Data from 2019, revealed that 42% of people were diagnosed late. A late diagnosis significantly increases the risk of the virus seriously damaging your health, not to mention the fact that you are more likely to pass the virus on during the period when you are unaware of a positive diagnosis. The only means to address this issue is to increase awareness of the importance of HIV testing.
If you have HIV for a long time without knowing, it can damage your health and shorten your life expectancy. It’s a good idea to test at least once a year (or more if you have unprotected sex with more than one partner). Early detection can give you a better quality of life and reduce the spread of the disease.
While there is no ‘cure’ for HIV, thankfully there are now very effective treatments available that allow those who are HIV positive to live a healthy life and have a normal life expectancy. There is also emergency treatment available if you have been exposed to HIV within the last 72 hours (PEP). Additionally, there is medication available to prevent contracting HIV (PrEP) and even a tablet that will prevent you passing the virus on to anyone else. Access to these treatments is available to anyone HIV positive but the only way to know your HIV status is to get tested.
Know Your Status
At Fleet Street Clinic, we have two types of HIV tests available: an instant test and a blood test. An instant HIV test can provide you with results within a 15 minute nurse appointment. The test is a simple blood test done via a needle prick to the finger and is suitable for use 90 days post-exposure. It is a very simple process with extremely accurate results.
For HIV testing week we’re promoting our ‘So quick you can do whilst grabbing a coffee’ campaign to highlight just how quick an HIV test can be. We want to encourage all to make time to find out their HIV status.
Get Tested
We offer a number of HIV Tests, some of which can be performed in the clinic in just 15 minutes. You can be tested for HIV from as early as 28 days post-contact with a blood test, but don’t worry, during your appointment the clinician will let you know which test they recommend based on your history. Following an HIV test, we are on hand to offer guidance and referrals, should they be required.
Your privacy will be strictly protected.
You can book an HIV Test Online.
For more information on HIV you can visit our HIV page or HIV Prevention England.
Statins are a widely prescribed class of drugs used to lower cholesterol levels and prevent cardiovascular events such as heart disease and strokes. The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
This decision was made after the independent committee updating the NICE guideline on cardiovascular disease (CVD) risk assessment and reduction considered new evidence on the safety and side effects of statins, meaning more people could be given them.
The draft guideline recommends that doctors should consider statins for people who haven’t had a CVD event (called ‘primary prevention’) with a 10-year CVD risk score of less than 10%. The committee agreed that if more people took statins there would be a greater reduction in the incidence of heart disease and strokes.
In addition to being prescribed by National Health Service GP’s, statins can also be prescribed by private healthcare providers, such as us, Fleet Street Clinic. In fact, private GP’s can play an important role in the management of cardiovascular disease risk by offering statins as part of a comprehensive treatment plan for patients at high risk.
People can be at risk from CVD because of factors they cannot change including their age, sex, ethnicity and family history but it’s important to note that certain lifestyle changes can reduce the risk. These include stopping smoking, reducing alcohol consumption, introducing or increasing exercise and eating a healthy diet.
Therefore, the decision to take a statin should be made in consultation with a healthcare professional and should take into account the individual’s values and priorities as well as the potential risks and benefits of treatment.
With the British Heart Foundation noting that “there are around 7.6 million people living with heart and circulatory diseases in the UK” and that they “estimate that in the UK more than half of us will get a heart or circulatory condition in our lifetime” this is likely to be an impactful change in the landscape of CVD and statins.
To conclude, Paul Chrisp, director of the Centre for Guidelines at NICE, said:
“What we’re saying is that, for people with a less than 10% risk over 10 years of a first heart attack or stroke, the decision to take a statin should be left to individual patients after an informed discussion of benefits and risks.
“The evidence is clear, in our view, that for people with a risk of 10% or less over 10 years, statins are an appropriate choice to reduce that risk.
“We are not advocating that statins are used alone. The draft guideline continues to say that it is only if lifestyle changes on their own are not sufficient, and that other risk factors such as hypertension are also managed, that people who are still at risk can be offered the opportunity to use a statin, if they want to. They don’t have to, and their decision should be informed by an understanding of the risks and tailored to their values and priorities.”
Reference Source: https://www.nice.org.uk/guidance/indevelopment/gid-ng10178/documents
Related services available at Fleet Street Clinic:
Sleep plays a crucial role in maintaining overall health and well-being, and recent research has revealed a strong link between sleep and cardiovascular health. A study conducted by the University of Warwick in the UK found that individuals who get 7-9 hours of sleep per night have a lower risk of cardiovascular disease (CVD) and mortality compared to those who sleep less or more than the recommended range.
The study, published in the Journal of the American College of Cardiology, analysed data from over 116,000 participants in the UK Biobank study and found that those who slept less than 6 hours or more than 9 hours had a higher risk of CVD and mortality. These findings add to the growing body of evidence that suggests a link between sleep duration and cardiovascular health.
The exact mechanisms by which sleep affects cardiovascular health are not fully understood, but researchers suggest that it may be related to the impact of sleep on cardiovascular regulation, inflammation, and metabolic function.
It is important to prioritize sleep and aim for the recommended range of 7-9 hours to maintain cardiovascular health.
It’s worth noting that these findings are observational, and more research is needed to fully understand the relationship between sleep and cardiovascular health, but it’s a good indication that sleep plays a vital role in maintaining a healthy cardiovascular system.
To read the full study, continue reading here:
medscape.co.uk – Does sleep duration influence cvd and mortality risk?
Related services available at Fleet Street Clinic:
Travelling can have a significant positive impact on one’s physical and mental health, according to a study published in the Journal of Travel & Health. The study surveyed over 1,000 adults who had recently returned from a trip and found that the majority of them reported improvements in overall well-being, including increased energy and reduced stress levels.
One of the key reasons for these self-rated health benefits is that travelling allows individuals to step out of their daily routine and experience new environments and cultures. This can lead to increased physical activity, as travellers may be more likely to walk or bike instead of drive which may also expose them to different types of food, leading to a healthier diet.
Additionally, travelling can have a positive impact on mental health as well. The study found that the majority of participants reported feeling more relaxed and less stressed after their trip. This is likely because travelling can provide a sense of excitement and adventure, as well as a break from the demands and responsibilities of everyday life.
Another benefit of travelling is that it allows individuals to build new social connections, which can be important for mental health. Meeting new people and forming new friendships can provide a sense of belonging and can also help to reduce feelings of loneliness and isolation.
In conclusion, the study suggests that travelling can be good for one’s physical and mental health. It can help to increase energy levels, reduce stress and improve overall well-being. So, next time you are planning a trip, remember it’s not only good for your soul but also for your body.
To read the full study, continue reading here: https://www.sciencedirect.com/science/article/pii/S2214140522002079?via%3Dihub
Related services available at Fleet Street Clinic:
- Travel Vaccinations
- Jet Lag Calculator
- Travellers’ Diarrhoea Online Consultation
- Antimalarials
- DVT Rick Calculator
Chinese New Year is a festival celebrated annually by Chinese communities across the world to bring good luck and prosperity into the New Year. Every year corresponds with one of the 12 animals in the Chinese Zodiac, with 2023 being the Year of the Rabbit. Celebrations for Chinese New Year kick off on the 22nd Jan, continuing until the 5th February where the festivities culminate with the Chinese Lantern Festival. Every year, thousands of people travel to China to enjoy the celebrations. So, if you are one of those people who are planning to travel to China to join in with the festivities, please ensure you follow these tips to stay healthy whilst abroad.
Firstly, you may want to check the entry requirements for China in terms of required covid-19 testing. If you travel to China after 8th Jan, you would require a negative Covid-19 test and submit your negative result by filling a Health Declaration Form via China Custom Website or their app or WeChat account. You would also need a pre-departure Covid -19 test when coming back to England from China. If you are still travelling to China you can view what covid-19 testing entry rules are currently in place here: GOV.UK WEBSITE. You can find more information on our rt-PCR Testing service here and our Lateral Flow Testing here.
Covid aside, check your vaccination history. All travellers need to ensure they are up-to-date with their childhood vaccines, most importantly, Hepatitis A, Typhoid, Measles, Mumps and Rubella (MMR), and Diphtheria, Tetanus and Polio (DTP).
More information on our wellness vaccinations can be found here.
It is worth noting that it is still influenza season in the northern hemisphere and transmission can occur well into spring. Those travellers who haven’t received their annual flu vaccination to protect them against the most common strains for 2022-23, should ensure they receive it before travelling to China. You can still book your annual flu vaccine, here.
Travellers who are planning extended stays, and more remote and rural travel may also wish to consider vaccinations against Rabies and Hepatitis B.
More information on our travel vaccinations can be found here.
Those who are heading further south to rural areas where the weather is warmer may wish to consider vaccination against Japanese Encephalitis (JE), which is spread via the culex mosquito. You can also purchase our ‘Ultimate Bug Kit’ which will help protect you from mosquito bites.
There have been recent cases of Avian Influenza (bird flu) in both the UK and China. Bird flu is a very unpleasant illness which can cause people to fall quite unwell. It is passed on via contact with infected birds. Travellers can minimise risk by avoiding contact with any birds (dead or alive): avoid touching dead or dying birds, and steer well clear of ‘wet markets’ (marketplaces that sell meat, fish, and often live animals including birds).
Chinese New Year is heavily focused on food, with items such as fish, fruit and dumplings symbolising luck, wealth and prosperity. Travellers should ensure that they maintain good food and water practises to avoid tummy trouble whilst away. You should avoid tap water and ice made from tap water, instead stick to bottled water. Ensure you wash your hands thoroughly before eating and after using the toilet. Ensure all food that you eat is cooked thoroughly and served straight to you. And lastly, consider taking medicines for self-treatments with you, such as antibiotics – take our Online Travellers’ Diarrhoea Consultation to see if it is suitable for us to prescribe you standby Travellers’ Diarrhoea treatment.
By following these guidelines and ensuring you are generally sensible and hygienic, you will be able to relax and enjoy the sheer joys of travel and seeing the world.
Happy Chinese New Year!
You can book online for a travel consultation appointment here.
Or for more information on all of our travel vaccinations, wellness vaccinations or travellers’ diarrhoea.
Dry January grows in popularity year on year.
The campaign by Alcohol Change UK, encourages participants to give up alcohol for the entire month of January.
The dry January one-month booze-free challenge can have a significantly positive impact on your health.
Alcohol has proven to increase the risk of developing a range of health problems (including cancers of the mouth, throat and breast) and that risk increases the more you drink on a regular basis.
Ruth Kander, our dietitian, looks at what is considered a safe amount of alcohol consumption.
The UK Chief Medical Officers’ (CMOs) guideline for keeping health risks from alcohol to a low level for both men and women states that:
- It is safest not to drink more than 14 units a week on a regular basis.
- Regularly drinking as much as 14 units per week, it’s best to spread your drinking evenly over three or more days.
– If you have one or two heavy drinking episodes a week, you increase your risk of death from long-term illness and injuries. - Cutting down the amount you drink, a smart way to help achieve this is to have several drink-free days a week.
A useful website for more information about alcohol is www.drinkaware.co.uk
What is a unit of alcohol?

How long does alcohol stay in your body?
On average, it takes about one hour for your body to break down one unit of alcohol, however, this can vary, depending on:
- Your weight
- Whether you’re male or female
- Your age
- Your metabolism – how quickly or slowly your body turns food into energy
- How much food you have eaten
- The type and strength of the alcohol you have consumed
- Whether you’re taking medication and, if so, what type
- It can also take longer if your liver isn’t functioning normally
If I am on medicines can I drink alcohol?
People taking sedative drugs (like diazepam/valium) or antidepressants (like fluoxetine/Prozac) should avoid alcohol altogether.
There are some antibiotics; metronidazole and tinidazole which just do not mix with alcohol – drinking with these will make you sick. But for most commonly prescribed antibiotics, drinking is unlikely to cause problems so long as it is within the low-risk alcohol unit guidelines.
People taking long-term medications should be careful about drinking, as alcohol can make some drugs less effective and long-term conditions could get worse. Examples of long-term medications include drugs for epilepsy, diabetes, or drugs like warfarin to thin the blood.
(From www.drinkaware.co.uk)
What are the consequences of drinking too much alcohol?
- Low mood/mood swings
- Liver problems
- Heart problems
- Cancers (mouth, tongue, throat, oesophagus)
- Weight gain
- Poor sleep
- Blood pressure instability
By Ruth Kander BSc(Hons)RD | Dietitian
If you wish to discuss ways to maintain a healthy diet and reduce your alcohol consumption, Ruth holds a virtual clinic every Friday from 9am-2pm. Please call our reception team on 020 7353 5678 if you would like to request a face-to-face appointment
Flu cases in the UK have increased earlier this winter than usual, perhaps by over a month.
Other unpleasant respiratory infections such as RSV are also on the rise.
Information from around the world can help us predict what might type of flu season might be heading our way.
- Australia has just come to the end of a bad flu season, with a dramatic increase in flu cases and hospitalisations relative to the mild season it experienced last year, in a pattern likely to be replicated in the UK.
- In the USA, by the end of November 2022 there had already been more than 6.2 million flu cases, with 53,000 hospitalisations, and 2,900 deaths from flu.
- Across Europe as a whole, the flu season has commenced earlier than in the 4 previous seasons, and the proportion of positive tests from sentinel locations has exceeded the technical threshold for consideration as an epidemic.
Meanwhile, UK vaccination rates have so far been low: by the end of November, when the flu vaccination campaign should be largely complete, fewer than 40% of “at risk” adults under 65 had been vaccinated, fewer than 25% of healthy adults aged 50 to 64, and fewer than 30% of pregnant women.
So this winter’s flu season is likely to be more severe, and not enough people will be protected.
What can you do to keep well this winter?
Get Vaccinated . Get Tested . Get Treatment
Get Vaccinated
The good news is that circulating flu strains have so far been a good match with this year’s flu vaccines. It is not too late to be vaccinated. Vaccines are still available. At this point in the season, our preferred vaccine for adults is our premium recombinant vaccine, Supemtek, which is known to be highly immunogenic.
Flu cases in children are rising but the nasal spray vaccine has so far been in restricted supply. If your child has not yet been able to obtain the flu spray, injected flu vaccines are at least as effective and should be given without further delay.
You can easily book your flu jabs online.
For family or groups bookings, it may be more convenient for you to book by phone or email.
Get Tested
At the Fleet Street Clinic, we can test quickly and accurately for a full panel of respiratory viruses in our own laboratory. It is helpful to know whether you are suffering from flu, covid, or another circulating virus such as RSV or metapneumovirus. We can tailor treatment to the result, help you know how long symptoms will last, and can help you prevent spreading it to others – especially important over the Christmas period when socialising in high at work and amongst family and friends.
Get Treatment
Flu is treatable with anti-viral drugs, which reduce symptoms and speed recovery. Preventive treatment for close contacts and other members of your family is also something we can help with, available from our GPs. Knowing for certain that you have a viral infection can also help avoid unnecessary antibiotic treatment.
___________________________
For more information on Flu Jabs available at Fleet Street Clinic.
Other recommended winter vaccinations are the shingles vaccine & the pneumonia vaccine.
We can also provide onsite Workplace Flu Vaccinations for companies in the UK – for more information.
Complete the below form for a quote:
A good night’s sleep is essential to your health, and an important part of your overall well-being. People spend about a third of their lives in bed, so it’s vitally important to get it right when it comes to back health. Back pain can significantly affect a person’s ability to get the quality and amount of sleep they need. Furthermore, poor bed posture can worsen or even be the cause of backache in the first place. This is because certain positions can place unnecessary pressure on the neck, hips, and back.
This blog will provide an in-depth review of different sleeping positions and types of beds and the impact both have on your quality of sleep.
Sleeping positions
Before looking at the positions to sleep better, it is important to address a few crucial things. First and foremost, you should be comfortable. For a good night’s sleep, waking up feeling properly rested and not in pain is the most important thing. If any of these positions cause issues, don’t hesitate in letting me (or another osteopath) know so that alternative suggestions can be made and you find something else that works for you.
Secondly, I know it’s not always possible to control what position you get into once you’ve fallen asleep. However, this is where perseverance comes in, if you keep trying, your body can adapt in a week or two. Pillows are always a good ally, to stop you rolling one way or the other.
Here are some positional tips that can help you get a better night’s sleep:
1. The Classic: Lying on your back.
Lying on the back is probably the best all-around sleeping position for a healthy back. It ensures good spinal alignment from the head and cervical vertebrae, through the thoracic and lumbar, all the way down to the pelvis. Because the back is the body’s largest area, weight is most widely distributed in this position, minimising pressure hot spots. This doesn’t suit everyone though, some people don’t feel as ‘nested’ as in other positions so, they struggle to get to sleep on their backs. Also, snorers may find that this position exacerbates the problem.
For people who like back sleeping, it’s definitely worth adding a pillow under your knees. It loosens the hamstrings a little and takes some pressure off the lumbar lordosis.
2. The Foetal Position: Lying on your side with your knees up a little.
This is a fairly intuitive position to get into if you have lumbar disc issues as it slightly flexes the low back and opens up the gaps in the facet joints.
Again, a good tip in this position is to use a pillow, however, this time put it in between your knees. This stops your top leg dropping forward and rotating the low back. It also aligns your hips and pelvis better, and feels more comfortable on the upper knee.
Try to swap sides from time to time if you’re lying in the foetal position.
3. Face Down: Lying on your stomach.
I normally ask people to avoid this position, it’s usually quite problematic for the neck as well as the low back. Unfortunately, for a lot of people, it’s the only position they can fall asleep in, or any other position makes them snore. If you’re one of them, reach for that extra pillow again and put it under your low stomach and upper pelvis to take the pressure off the low back. This is a good idea if you’re having a massage too. Front lying needs a much flatter pillow (or even no pillow) under the head too.
If you’re someone who falls asleep on their back or side, then rolls over in their sleep and wakes up on their stomach, try hugging a large pillow against your chest and stomach to keep you in position. Another reason sleeping on the front is considered bad is because the head is usually turned to one side. This twists the spine and places additional stress on the neck, shoulders, and back. To avoid this, you can try lying face down. Place a small firm pillow or tightly rolled-up towel under the forehead, or better still a face pillow, allowing room to breathe. In this position, you should still place a pillow under the stomach.
4. Reclined Sleeping.
If all else fails, you can try sleeping in a reclined position. People with spondylolisthesis, for instance, may resort to this after finding it comfortable falling asleep in a recliner chair. There are beds available that can be sat up slightly. So, this is worth investigating.
What about the perfect bed for sleep?
There are so many different opinions about beds that I don’t even know where to start, nonetheless here’s mine.
Spend some time and effort (and dare I say money) choosing a bed and mattress. People seem happy to spend thirty times or more on a car than a mattress, but remember, a third of your life is spent in bed!
It’s really difficult to choose a mattress on a twenty minute trip to the bed store, so really take your time, spend an afternoon there, take your shoes off, try different sleeping positions, not just lying on your back! Do your research before you go, but make sure the review sites you look at aren’t secretly run by a bed company, or affiliated to one.
Firmness
Try not to be seduced by softness. Lots of people jot down the name of a mattress they’ve found comfortable in a hotel, and while this can sometimes be a good indicator, you should know that hotels buy mattresses to give you a couple of nights feeling like you were sleeping on a cloud, but these mattresses are usually not supportive enough to be using full time, especially if you have low back issues, which can be aggravated over weeks and months. Often the mattress in a big hotel chain is not available to buy for the public as they are specifically manufactured for different hotels’ standards.
A fairly firm mattress is usually a good idea, perhaps with a shallow in-built topper. This can give you the support you need for your low back while the topper takes the pressure off bony prominences and allows shoulders and hips of side sleepers to sink in a little. I suggested a built in topper as they are usually better segmented and don’t allow stuffing to move around and bunch up as much. However, removable toppers give you more scope to adapt by removing it if needed, and also allow you to flip the mattress.
Mattresses that are fully stuffed as well as sprung are good and supportive. Price is a good indicator for a quality mattress. £1,500 for a king size mattress is not excessive. While we’re talking about price, beware of anything that seems too good to be true. The “Winning awards” mattresses need to be checked as to which award, and who’s giving it!
Memory Foam Mattress
Patients have different opinions about memory foam mattresses. While some patients swear by them, others do not get along with them. I’d like to reiterate the price, if you’re set on a memory foam mattress, find the one with better quality, so it doesn’t start to develop a permanent dip where you lie. It’s all about density which is measured in pounds of pressure per cubic square foot. More is normally more expensive and better quality, but at the same time is also more supportive and feels harder.
There can be a problem with memory foam mattresses feeling too hot. While many of the better brands have addressed this to an extent, many memory foam mattresses have become hybrids so, it’s not just 100% foam any more.
Platform Bases
Mattresses should be changed about every 8 years, but you can keep the same bed base, of course, as long as it’s not damaged. Divans have pretty thin wood tops that can crack or bow so, check it carefully.
In my opinion, a platform base is always the best. If the base is sprung, the whole mattress will start to fold which is usually not what they’re designed to do. A slatted base is slightly better than a fully sprung one, but still not as good as a solid base.
Pillows
Finally, I should mention pillows. Pillows are very subjective to the person, and especially to any neck/upper back/shoulder girdle conditions they may have.
As a rule of thumb (and this is painting with a very broad brush) people seem to usually have too much pillow depth more often than too little. One medium depth pillow is usually best if you don’t have any specific issues. I find feather works well as you can punch and mould it to the right height and shape, so there is some support under your neck but that’s very much a personal preference.
I rarely see anyone who gets on well with memory foam pillows (there are the odd one or two) or sprung pillows.
The price of a good feather pillow is probably about £50, but as I said right at the start, I want you to not only be in a good position, but also comfortable and pain-free during the night and the next day, so if a £5 pillow works for you then that’s absolutely fine. Don’t forget most pillows can be laundered regularly which may give (especially feather pillows) some of their volume back.
If you are experiencing neck pain though, get your neck examined and treated first and ask your osteopath what pillow they would suggest for you specifically going forward.
BE ‘BED FIT’
The healthier and stronger your back is, the better night’s sleep you will get and the better your back will be when you get up in the morning.
Core strengthening exercises will help support the back during the night and prevent back spasms. Gentle stretching before bed can increase flexibility and help to relax the body and reduce stress.
Take care getting in, and especially out, of bed. Take your time. When you wake up in the morning, allow a few minutes to get your muscles and joints moving fully instead of leaping out of bed at the alarm. Roll onto your side then use your arms to push you upright while your legs drop over the side, then sit there for a minute moving gently before slowly standing up.
Perhaps most importantly, if you do have a back or musculoskeletal issue, get it checked. A health professional can assess why you’re suffering and help treat the symptoms. They can suggest the correct investigations, treatment and exercises, as well as further helping you to choose that all important correct mattress.
Booking an appointment with an osteopath could be the start of ending your back pain for good!
Mental Health Awareness Week: What Is Stress?
Look around your office, do you know if anyone is struggling?
You may think those around you – fellow colleagues or your staff – are completely fine. But mental health affects us all and problems in the workplace are actually very common.
According to mental health charity Mind, at least one in six workers are experiencing common mental health problems, including anxiety and depression.
Nowadays, there is increasing recognition of stress and mental health problems, both within the workplace and in everyday life. Currently, following Stress Awareness Month in April, we are approaching Mental Health Awareness Week, which takes place from 13-19th May.
We thought it might be helpful to focus on some positive strategies to help, in terms of stress management and resilience. Whilst being particularly useful and relevant within the workplace, these can all be used in everyday life as well.
WHAT IS STRESS?
In its purest form, stress is the body’s reaction to something it perceives as dangerous or threatening. When we feel under attack, our bodies respond by producing a mixture of hormones such as adrenaline and cortisol. These prepare us for physical action by diverting blood away from our core and into our limbs. It also temporarily shuts down some less vital bodily functions such as digestion.
For immediate, short-term situations, stress can be beneficial to your health, by helping you cope with potentially serious situations.
Yet if your stress response continues, and stress levels stay elevated far longer than necessary, it can take a toll on your health.
WHY IS IT IMPORTANT TO TACKLE STRESS?
Chronic stress can cause a variety of symptoms, contribute to many health problems (such as high blood pressure, heart disease, obesity and diabetes, anxiety and depression) and affect your overall well-being.
Reducing stress can help prevent these harmful effects on both mind and body.
Looking after yourself and ensuring you have good mental health has many benefits – not just for you as an individual, but for the business too. Employees are generally more productive, passionate and motivated when in good health. Even if they’re experiencing mental health problems, knowing they are supported by their employer can help in the recovery process.
STRESS PREVENTION IS BETTER THAN STRESS MANAGEMENT
Ultimately, the best way to manage stress is through prevention rather than cure.
Research shows that those who are better informed about the practical ways in which they can lower their stress levels are far better able to tackle difficult situations with emotional resilience and determination.
Within the workplace, employers are encouraged to make promoting the wellbeing of their employees a core element of the company’s internal operations. Some examples of a proactive approach to stress-management might be:
- To invite people to take active breaks away from their desks
- Offering lunchtime yoga classes or mindfulness sessions
- Group walks in the fresh air.
So what can help you reduce stress? Continue reading our stress, with Our Top Tips For Reducing Stress.
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch. Or if you are an individual who needs help with stress management, you can book a GP appointment online.
Feeling stressed?
Everyone feels stressed from time to time. In small doses, stress can actually be quite useful; motivating us to achieve our goals. But for some, stress is chronic. Meaning it is debilitating and negatively impacts their mood, their health and wellbeing, their relationships and their work.
Experiencing a lot of stress over a long period of time can also lead to a feeling of physical, mental and emotional exhaustion, often called burnout. It is, therefore, easy to see why reducing stress across all areas of your life would be important. Stress management tips are a good place to start.
Learning how to manage your stress takes practice and time.
Here are our top 10 ways on managing and reducing stress.
10 TIPS TO REDUCE STRESS:
-
Prioritise your health
– make decisions which will benefit your physical, mental and emotional wellbeing. For example, go alcohol-free a few nights each week or allow yourself time for a hobby you enjoy. These small steps for a healthier lifestyle will help in reducing stress levels.
-
Get a good night’s sleep (regularly)
– research clearly shows that sleep deprivation amplifies the symptoms associated with stress. Aim for between 7-9 hours of good quality sleep every night.
-
Practice deep breathing
– when our bodies are stressed, the muscles that help us breathe tighten. By focussing on taking several deep breaths we can quickly and effectively relieve physical symptoms associated with feeling stressed or anxious. Try to do this regularly throughout the day.
-
Drink enough water
– being dehydrated (however mild) causes our cortisol levels to rise, which automatically makes us feel stressed. Your body is already dehydrated if you’re feeling thirsty. So try to avoid reaching this point by hydrating yourself regularly. Aim for 2-3 litres per day, more in hot weather or when exercising.
-
Eat a balanced diet
– dieticians stress how certain foods have stress-relieving properties. For example, dark chocolate is rich in antioxidants, whilst avocados and oily fish are high in omega-3 fatty acids (both of which are proven to help lower anxiety levels).
-
Exercise regularly
– physical activity causes our brains to release mood-improving chemicals called endorphins. These help us to cope with potentially challenging situations. Both Public Health England and the World Health Organisation recommend at least 150 minutes of moderate intensity physical activity each week, in bouts of 10 minutes or more. Choose activities you enjoy to achieve maximum benefit for the mind as well as the body.
-
Adopt a positive mindset
– research suggests that making a conscious effort to think positively can help protect us against a whole host of physical and mental issues, including stress.
-
Manage your time and tasks effectively
– by giving ourselves enough time in which to complete a given task, and by making sure that we don’t try and accomplish too many stressful things at once, we can reduce the likelihood of feeling overwhelmed.
-
Spend less time online
– many studies have found a strong positive correlation between internet usage and stress levels. Spending less time on our computers and phones is a simple way to practice self-care. Having screen-free time for at least an hour before bedtime has also been shown to improve sleep.
-
Learn to say no
– in a culture that demands we take on more and more responsibilities, having the confidence to say “no” will only become more important. This final tip takes us back to the start, by reiterating the importance of prioritising our health above unrealistic social pressures, and brings us onto developing an essential tool – resilience.
Continue reading about Resilience or read What is Stress?
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch.
Or if you are an individual who needs help managing stress, you can book a GP appointment online. Our doctors will be able to talk through your thoughts, symptoms and emotions and set you on the right path to diagnosis. They will also be able to recommend relevant support services for stress, if appropriate.
Mental Health Awareness Week: Resilience
WHAT IS RESILIENCE?
Resilience is the ability to recover from adversity, hardships, or significant sources of stress.
It means “bouncing back” from difficult experiences, feeling stronger and more capable to cope than before. With life becoming more stressful than ever, it is an important skill to develop which can make a big difference between surviving and thriving within work and general life.
HOW RESILIENT AM I?
Research has shown that resilience is ordinary, not extraordinary, and is not simply a trait we either have or do not have.
So here’s the good news! Resilience can be developed. It involves behaviours, thoughts and actions which can be learned and developed in anyone.
SO HOW CAN I DEVELOP RESILIENCE?
Many studies show that the primary factor in developing resilience is having caring and supportive relationships within and outside the family, including at work. Relationships fostering trust, provide role models and offer encouragement and reassurance help bolster resilience.
Several additional factors are associated with resilience, including:
- The capacity to make realistic plans and take steps to carry them out.
- A positive view of yourself and confidence in your strengths and abilities.
- Skills in communication and problem-solving.
- The capacity to manage strong feelings and impulses.
These are all factors you can develop in yourself, and which can be fostered within the work environment by employers taking an active interest in employees’ wellbeing.
TOP TIPS FOR DEVELOPING RESILIENCE
Here are a few things you could try, to develop your resilience.
Please don’t feel you need to tackle them all at once – trying one or two at a time may be enough to make a big difference!
1) Create connections
– good relationships with family, friends and colleagues are crucial. Accepting help and support from those who will listen to and care about you strengthens resilience. Assisting others in their time of need can benefit you in return.
2) Accept that change is fundamentally part of living
– accepting circumstances that cannot be changed can help you deal with these more effectively whilst focussing on circumstances that you can alter.
3) Avoid seeing stressful events as insurmountable problems
– try to look beyond the present towards how future circumstances may be a little better. Take note of any subtle ways in which you might already feel better as you deal with difficult situations – signs of good progress.
4) Take decisive action
– this can assist you in giving some control over your response to challenging situations
5) Pursue your goals
– making them small but achievable and most importantly realistic. Each day, ask yourself “What’s one thing I know I can accomplish today which will help me move in the direction I want to go? Take baby steps in the right direction!
6) Nurture a positive outlook
– developing confidence in your ability to solve problems and trusting your instincts helps build resilience.
7) Keep things in perspective
– retaining an optimistic outlook and visualising what you want, rather than worrying about what you don’t want, can all help the brain engage with this.
8) Practice mindfulness and meditation
– Mindfulness means paying more attention to the present moment – to your own thoughts and feelings, and to the world around you. Meditation involves the use of techniques such as mindfulness to train attention and awareness. Mindfulness and meditation are believed to relax and calm the brain, tackling sources of stress while improving clarity focus and even sleep. According to mentalhealth.org.uk, those practising mindfulness have shown increased activity in the area of the brain associated with positive emotions.
9) Take opportunities for self-discovery and personal growth
– by learning something about themselves, people may find that they have grown in some respect. Many people who have experienced tragedies and hardship have reported better relationships, a greater sense of strength even while feeling vulnerable, increased sense of self-worth, a more developed spirituality and heightened appreciation for life.
10) Take good care of yourself
– pay attention to your own needs and feelings. Engage in activities that you enjoy and find relaxing. Exercise regularly. Taking care of yourself helps to keep your mind and body primed to deal with situations requiring resilience.
If you would like further help and support in resilience training in your workplace, get in touch with our Corporate Health department.
Stress: Are we coping?
We all feel the effects of stress in daily life, whether it’s managing children or dealing with a problem at work. Stress is a normal response, in fact, in small doses, stress can be useful. The problems arise when you start to have a ‘fight or flight’ stress response to situations in everyday life. This can lead to illness, both mentally and physically.
The first step is to recognise symptoms of stress:
- Nail biting and fidgeting
- Over-eating or loss of appetite
- Irritability with other people
- Substance abuse, including alcohol and smoking
- Lack of concentration
- Increased and suppressed anger
- Feeling out of control
- Excessive emotion & crying
- Lack of interest in anything
- Permanently tired even after sleep
By identifying stress-related problems as early as possible, action can be taken to avoid any serious stress-related illness. For Mental Health Awareness week, which runs from 14-18 May, here are some tips to help manage your own personal stress:
- Be active – 30 minutes a day can reduce the emotions and let you take the time to think more clearly
- Take control – you are your own worst enemy, but you are also the key to empowerment!
- Find support – Connect with your family and friends, the more help the better the solutions
- Take time for yourself – remember to have time for yourself as well. Read, relax and get things done on your to do list that may be holding you back
- Create challenges for yourself – Setting achievable goals, little or big can help build confidence in your abilities
- Avoid unhealthy habits – Cut down on caffeine, smoking, and alcohol. These can enhance the feeling of stress in the long run
- Be positive – Instead of looking at problems negatively, try to see what you can get out of it to help you grow. Be grateful!
- Acceptance – Take ownership of mistakes, or acceptance of things you can’t control.
Our Occupational Health team at the Fleet Street Clinic are able to provide a full range of work health assessments to address the occupational health needs of your staff. Click here for more information.
To book an appointment with one of our friendly doctors, or for further details on what we can offer for our Occupational Health, call us today on 0207 353 5678 email info@fleetstreetclinic.com or book online now.

Cutting back on alcohol can be a really effective way to improve your health, boost your energy, loose weight and save money.
In 2016, the Chief Medical Officers in the UK reduced the recommended amount of alcohol you should consume a week due to concerns about the risk of cancer. New research confirmed that even drinking a small amount of alcohol per week can cause an increase in risk of cancer.
From then onwards, it has been recommended that men and women have the same weekly intake of units per week. According to the UK low risk drinking guidelines, you should drink no more than 14 units a week, make sure you have several drink-free days, and never binge drink.
What does 14 units of alcohol look like?
Because alcoholic drinks come in different strengths and sizes, units are a way to tell how strong your drink is. 14 units is equivalent to six pints of average strength beer or six medium (175ml) glasses of average strength wine.

It’s safest for both men and women to drink no more than 14 units a week, spread over three or more days with several drink-free days, and no bingeing.
Your risk of death from long term illness, accident or injury, is increased if you ‘binge drink’ 1 or more times a week.
How long does alcohol stay in your body:
On average, it takes about one hour for your body to break down one unit of alcohol. However, this can vary, depending on:
- Your weight
- Whether you’re male or female
- Your age
- How quickly or slowly your body turns food into energy (your metabolism)
- How much food you have eaten
What are the consequences of drinking too much alcohol:
- Low mood/mood swings
- Liver problems
- Heart problems
- Cancers (mouth, tongue, throat, oesophagus)
- Weight gain
- Poor sleep
- Blood pressure instability
What are the benefits to cutting down on alcohol?
Short-term benefits:
- waking up in a better mood
- being less tired and more energetic throughout the day
- healthier looking skin
- saving some money
Long-term benefits:
- lower your blood pressure
- lower the risk of diseases including cancer, stroke, hypertension and liver disease
- lower your cholesterol levels
- your memory will improve
- better quality of sleep
- help with weight management*
* Did you know? Alcoholic drinks are high in calories, so cutting back on the amount you drink can really help to reduce your calorie intake.
According to our GP & Occupation Health Physician, Dr Claire Braham;
“When you drink alcohol, you lose around 4 times as much fluid as you drink.
It is therefore easy to understand why dehydration often occurs. Dehydration symptoms are much like your classic hangover symptoms and will include headache, nausea and fatigue. These symptoms will become present when you are about 2-percent dehydrated, which is about when you start to feel thirst.
Avoiding alcohol means better hydration and sleep which will reduce hangovers and headaches, reduce tiredness, reduce sickness, increase your concentration and improve your overall control over emotions and behaviour. This leads to more productivity, better decision making and overall less accidents, regrets and more enjoyment.
It is not advised to drink more than 14 units a week, which is the equivalent of 6 pints of beer. That converts to 1,092 calories in total and would need 109 minutes of running to burn off those additional consumed calories. Abstinence is an easy way to avoid festivity weight gain.
Nowadays it is very easy to cut down or cut out alcohol. There is a wide variety of alcohol-free beer, wine, prosecco, gin, vodka, whisky and other spirits available on the market. These include some which are vegan and gluten-free as well as often free from sugar and artificial sweeteners. So you can still enjoy a ‘drink’, without the alcohol and high-sugar but with health benefits.”
For further detail of how alcohol can have a negative impact on your health, head to drinkaware.co.uk for more information and advice on drinking.
If you have concerns about the amount of alcohol you are drinking or about your health you should speak to a GP. You can book an appointment online.
More information on our GP service can be found here.
How walking can help Chronic pain
Firstly, what is chronic pain?
Chronic or persistent pain can be explained as pain that carries on for longer than 12 weeks despite medication or treatment.
The root cause can vary person-to-person, with it sometimes due to illness or an injury. In other cases it can be due to being overweight, having years of poor posture or improper lifting of heavy weights. It can be debilitating but movement is known to help.
As an osteopath, the conversation I seem to have at least once-a-day is; how much exercise should someone who is in pain be doing?
As you can imagine every case is different, and exercise advice varies hugely from person to person and condition to condition. There is a big difference between chronic pain and recovery from injury pain. I am focusing on exercises for people with chronic pain conditions, specifically walking.
Many people with chronic pain are afraid that movement, including walking, will worsen pain. But as many have subsequently discovered, the opposite is very often true. Using your muscles and joints less can often cause pain to becomes worse. Gentle exercise like walking can really help to bring those pain levels down, as well as many other benefits like improving your circulation, strengthening your bones and of course helping to keep those extra pounds off.
Here are tips before you start:
1. Talk to your healthcare professional first
You should always take the advice of a health professional before starting any exercise. They can ensure it is safe for you to start, and guide you with the types of exercises you should begin with. They will also help you understand your limits and outline suitable goals. As a rule of thumb, if you are in pain, stop!
I, or another osteopath, can check your posture and gait and give you tips on engaging the correct muscles.
2. Get the right shoes
A good pair of supportive trainers will prove invaluable. Walking boots that protect the ankle are only really required if you’re planning to walk on loose surfaces or heading off into the mountains. Otherwise, walking trainers will suffice. To find out more about choosing the right footwear, read our blog on How To Avoid Running Injuries.
3. Start slow
What we’re aiming for is about half an hour to an hour of physical activity five days a week, but this may take some time to achieve. There’s no rush! A good indicator that you are at the right intensity level is that even though your heart rate is up a little, you are still able to carry on a conversation while walking. When starting your walk don’t go full speed immediately. Allow your muscles and joints to warm up for the first few minutes before getting up to speed. This will help prevent damage and injuries.
4. Keep hydrated
You may need to carry a bottle of water, especially for walking in hot weather. If the weather is hot, make sure you also take sunscreen and a hat to stop sunburn.
5. Finally, try to enjoy it!
The more you enjoy it, the easier it becomes. Find somewhere nice to walk, even if that means
driving somewhere. Listen to music/ podcasts/ audiobooks, or even better get a walking buddy to join you for a chit chat along the route.
For more information on osteopathy services, visit the main page.
___________________________________
OSTEOPATHY AT FLEET STREET CLINIC
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC).
Book an appointment with him if you have any musculoskeletal injuries by calling +44 20 7353 5678, email info@fleetstreetclinic.com or book an appointment online.
Urgent polio boosters advised for London children
UK Health Security Agency (UKHSA) has announced that all children aged 1-9 years regardless of previous immunisation status are recommended a polio vaccine booster from all London boroughs.
The virus, which can cause paralysis, has been found 116 times in London’s waste water between February and July this year.
In the UK, the overall risk of paralytic polio is considered low because most people are protected from this by vaccination. However, due to the recent discovery of type 2 vaccine-derived poliovirus in sewage in multiple locations in London, the Joint Committee on Vaccination and Immunisation (JCVI) have advised that booster vaccinations in all children aged 1-9 years is an appropriate course of action.
The UKHSA says most of the samples detected are the safe vaccine form of polio, but “a few” have mutated enough to be considered dangerous.
Parents should seek the polio vaccine booster as soon as possible – even if their child is up-to-date with their childhood vaccinations.
The aim is two-fold; to ensure a high level of protection from polio paralysis and help reduce further spread of the polio virus across London and beyond.
Booster Polio Vaccinations at Fleet Street Clinic
We offer two vaccinations in-clinic that offer protection from Polio:
Revaxis Vaccine: Suitable for children from 6 years and above
Protects against: Diphtheria, Tetanus, Polio
Cost: £47 + £20 appointment fee
Call to book
Repevax Vaccine: Suitable for children from 3 years and above
Protects against: Diphtheria, Tetanus, Polio & Whooping Cough
Cost: £69 + £20 appointment fee
Call to book
Both of these vaccinations are inactivated, and given by injection. They are both licensed as booster doses, and are not intended for primary immunisation.
More information on the Polio vaccines available at Fleet Street Clinic, click here.
Primary Polio Vaccination
Unfortunately, we do not offer the infant/ baby vaccination for Polio – in the UK this would be the Infanrix-Hexa, the 6-in-1 vaccine. We have no suitable vaccination for children under the age of 3, or for those requiring their primary immunisation against Polio.
Please contact your NHS doctor or an alternative provider to see if they can help you further.
Dr Vanessa Saliba, Consultant Epidemiologist at UKHSA, said:
“It is vital parents ensure their children are fully vaccinated for their age. Following JCVI advice all children aged 1 to 9 years in London need to have a dose of polio vaccine now – whether it’s an extra booster dose or just to catch up with their routine vaccinations. It will ensure a high level of protection from paralysis. This may also help stop the virus spreading further.”
______________________
More information on Polio and the emerging London findings:
What is Polio?
Polio is a serious viral infection that is transmitted through the stool’s of an infected person through contaminated water, food or surfaces. It can cause unpleasant flu-like symptoms and in severe cases, cause paralysis.
What are the symptoms of Polio?
The majority of people with the infection have no symptoms but some feel as if they have the flu, with:
- high temperature
- sore throat
- headache
- abdominal pain
- sickness
In severe cases of polio, the virus can attack the nerves in the spine and brain which can cause paralysis. In some cases, it can cause persistent or lifelong difficulties and even be life-threatening.
Where has Polio been found?
According to the UKHSA statement, in addition to the findings earlier this year of type 2 poliovirus (PV2) collected from the Beckton sewage treatment works, further upstream sampling undertaken by the UK Health Security Agency (UKHSA) and the Medicines and Healthcare products Regulatory Agency (MHRA) has now identified at least one positive sample of the poliovirus, currently present in parts of the following boroughs:
- Barnet
- Brent
- Camden
- Enfield
- Hackney
- Haringey
- Islington
- Waltham Forest
The sampling has also detected the virus in lower concentrations and frequency in areas adjacent to the Beckton catchment area to the South (immediately below the Thames) and to the east of Beckton. However, it is not clear whether the virus has established itself in these areas or if the detections are due to people from the affected area visiting these neighbouring areas.
How many cases of Polio have been identified?
To date, again based on the UKHSA statement, ‘a total of 116 PV2 isolates have been identified in 19 sewage samples collected in London between 8 February and 5 July this year’.
A further 15 sites in London will start sewage sampling in mid-August, and 10 to 15 sites will be stood up nationally to determine if poliovirus is spreading outside of London.
To book your child’s Polio Booster Vaccination, call +44 20 7353 5678 today.
With (hopefully!) sunnier and longer days upon us, summer is a great time of year to get your running shoes on. As a keen runner myself, I understand the appeal; it’s pure, it’s meditative, and it gets your blood pumping like little else.
Unfortunately, for all its positives, running can be problematic for the body and it tends to bring out minor issues and turn them into major ones. These often include achilles tendonitis, shin splints, plantar fasciitis, ITB syndrome, stress fractures, hip and lower back issues, and more knee problems than I have time to list.
Many of the problems from running come from two areas. Firstly, heel strike which is where the heel hits the ground repeatedly and sends a shock through the whole skeleton which causes issues from the heel itself all the way up to the lower back. Secondly, gait – which is the way a person walks; the whole lower limb (especially the knee) is quite finely tuned to work in certain ways, and anything that affects that can begin to cause problems. A dropped arch, tight muscle, old injury, slight one-sidedness etc can bring these issues on.
What can be done to prevent these issues?
Like always, the number one rule is to get any symptoms you are experiencing looked at as soon as possible. Early diagnosis, advice and treatment is vital.
One thing that can really help heel strike and gait is by getting the right trainers. Here’s a few things to consider:
- Don’t confuse fashion and effectiveness. Good running trainers generally don’t look cool! Some of the bigger brands will advertise to you that they are great for sports but do your research. I would usually recommend Asics or Brooks.
- Replace your shoes regularly. The soles of most trainers are good for about 200-250 miles maximum. So, if you’re running 20 miles per week, you’ll probably need to replace them after 4-6 months.
The shoe may still look okay after that but there is an increased risk of injury. It is, therefore, important to ensure that you are replacing your trainers as regularly as required. - You don’t need to buy the most recent model. Many of the best running trainers are on their 20th/30th or so iteration. When a new model is released the price of the last couple of iterations will drop quite significantly, and will still be an excellent option.
- Good arch support. Trainers largely work on preventing pronation etc. by the way they flex. Many have little if any arch support, even with good ones you may need an additional orthotic insole made for your specific needs. This may also mean you need half a size bigger.
- Speak to the experts. A running machine in a shoe shop is useful, but remember the shop assistant has probably only had a brief introduction in what to look for, and no idea of your other contributing factors. Speak to a specialist – an osteopath, podiatrist, or physio.
_____________
OSTEOPATH AT FLEET STREET CLINIC
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC).
Book an appointment with him if you have any musculoskeletal injuries by calling +44 20 7353 5678, email info@fleetstreetclinic.com or book an appointment online.
WHAT IS DIABETES?
Diabetes is a lifelong condition that occurs when the body is unable to properly regulate the amount of glucose (sugar) in your blood. Poor control of diabetes can lead to high blood sugar levels and cause long term damage to your overall health and organs.
WHAT HEALTH PROBLEMS DOES IT CAUSE?
High blood sugar levels can cause a lot of damage to your body and if not managed correctly, may lead to many diabetic complications. This will cause long term health problems, especially if they go untreated.
HOW DOES DIABETES AFFECT OTHER PARTS OF YOUR BODY?
Eyes: Retinopathy is a complication of diabetes caused by high blood sugar levels damaging the retina, often leading to vision impairment. It is the leading cause of blindness among working-age adults in the UK. As a consequence of diabetic retinopathy, swelling can take place, called diabetic macular oedema. People with diabetes are also more prone to develop cataracts and glaucoma at an earlier age, contributing to vision reduction.
Feet: Foot health is often a neglected area anyway but high blood glucose levels can lead to insensitivity in the foot and lower limbs, which means you lose the ability to feel pain and distinguish hot or cold. It can also lead to less blood supply to your feet leading to poor circulation.
Loss of sensitivity means that you may not notice if you have a minor cut, sore or wound and poor circulation means if you do get a cut or sore, it will take longer to heal and open wounds are more likely to become infected. This combination is why there is an increase in risk of amputation for those who are diabetic. Regular podiatry appointments are the best way to look after your foot health.
Heart: High blood sugar levels can also cause problems to your blood vessels which can sometimes lead to serious problems such as heart attacks and strokes.
Kidneys: High blood sugar levels creates more difficulty for the kidneys to clear waste. This may lead to Diabetic Nephropathy, the deterioration of the kidneys.
HOW CAN DIABETES BE TREATED?
There is currently no cure for diabetes, therefore, the best way to deal with diabetes is to get it properly managed and controlled. If you are diagnosed with type 1 diabetes, you must either inject or pump insulin into body to treat your diabetes. If you have type 2 diabetes, you may also have to use insulin, however, it can be managed through diet and lifestyle changes.
HOW CAN YOU TEST FOR DIABETES?
An instant HbA1c test can confirm if you’re within the recommended range, or are considered pre-diabetic or confirm that you have diabetes. Using a small blood sample it will measure how well your blood sugar has been controlled over the last 3 months and provide a numerical reading.
As the HbA1c test provides 3-months insight, it is an important blood test for diagnosed diabetics. It provides a good indication of how well they are managing their diabetes..
Many people are more familiar with the glucose blood test – it measures the concentration of glucose molecules in your blood at a single point in time. The amount of glucose in your blood could also indicate whether you could be diabetic or not. People with diabetes can also use this test to manage their condition on a daily basis alongside regular HbA1C testing.
You can book an instant HbA1C test online at a cost of £54.50.
WHAT ARE THE SYMPTOMS?
When it comes to diabetes the symptoms are not always obvious and can often go unnoticed for long periods of time before being diagnosed.
The most common symptoms include:
- Feeling constantly thirsty or dehydrated
- Unintentional loss of weight and increased appetite (type 1)
- Vision begins to blur
- Numbness in your hands or feet (type 2)
- Fatigue
- Urinating more frequently
WHO IS AT RISK?
In the UK, type 2 diabetes is the most common type of diabetes, affecting over 90% of sufferers. The symptoms of diabetes are often mild, therefore, it’s important to be aware of the risk factors that could make you more susceptible to diabetes in the future.
According to Diabetes UK, type 2 diabetes is twice more likely in people of African descent in comparison to people of European descent and six times more likely in South Asian communities, making them a high risk category in developing diabetes. Additionally, people of African – Caribbean and South Asian descent are also at risk of type 2 diabetes much earlier, usually over the age of 25. On the other hand, for Europeans the risk increases when over the age of 40. Other factors contributing to diabetes include being overweight, high blood pressure and genetics.
Other general risk factors include:
- Having high blood pressure
- Carrying extra weight around your middle
- Smoking
- Polycystic Ovary Syndrome (PCOS) sufferers
- Those with a sedentary lifestyle
- Drinking too much alcohol
- Those with disturbed sleep – this includes those who do not get enough sleep and those whose sleep too much
If you have symptoms of diabetes or general concerns about your diabetic risk, you can book a GP appointment to discuss in more detail.
Alternatively, you can book in for an instant HbA1c test with a nurse.
From Sunday, June 12, 2022 at 12:01AM ET all COVID-19 testing entry requirements for international travellers to the United Stated were rescinded.
Arrivals no longer need to show proof of a negative Covid-19 test or documentation of recovery prior to boarding a flight to the U.S nor upon arrival.
The Centre For Disease Control (CDC) has reached the decision based on the high vaccine uptake and widespread population immunity.
In the statement they released, they explain; “The COVID-19 pandemic has now shifted to a new phase, due to the widespread uptake of highly effective COVID-19 vaccines, the availability of effective therapeutics, and the accrual of high rates of vaccine- and infection-induced immunity at the population level in the United States. Each of these measures has contributed to lower risk of severe disease and death across the United States. As a result, this requirement which was needed at an earlier stage in the pandemic may be withdrawn.”
Most countries, including the UK, have already abandoned testing requirements in a bid to return international travel to pre-Covid levels and it seems the CQC have decided it is now time for the U.S to do the same.
Does this mean that the COVID-19 pandemic has ended?
No, but it does signify a shift in the pandemic. As we see a worldwide reduction in covid cases and death rates, the CDC statement clarifies that whilst testing may not be necessary right now, they will continue to monitor the data and adapt accordingly.
They state; “CDC continues to evaluate the latest science and state of the pandemic and will reassess the need for a testing requirement if the situation changes”.
What about covid vaccinations…
Do I need to be vaccinated to travel to the U.S?
Yes, foreign travellers from outside of the U.S are required to be double vaccinated from COVID-19 to enter the country. But for people under the age of 18, U.S citizens/ nationals or lawful permanent residents will be exempt from vaccination requirements. Currently, the Covid Booster vaccination is not a requirement and there is no set expiry date on the first dose of vaccination.
Overall, the easing of the US Covid restrictions is welcome news to the travel and tourism industry and demonstrates the possibility of international travel returning back to its pre-covid levels.
However, the absence of masks, vaccines, or travel mandates does not mean that the risk of catching Covid-19 has gone away.
We strongly recommend:
- Having comprehensive travel health insurance for all travel to the USA – hospital care should you require treatment for Covid is very costly.
- Wearing a high filtration (N95 or FFP3) mask during your journey
- Practising all the usual hygiene recommendations during your journey (e.g. hand sanitisers, distancing where possible
- Having an early test and avoiding travel if you have even minor symptoms.
For more information on the covid testing services available at Fleet Street Clinic.
With monkeypox cases being recorded in over 20 countries across the globe, people are becoming increasingly concerned about its spread and transmission.
Following 2 years of the Covid-19 pandemic, this outbreak has reignited the public’s fear and uncertainty of infectious diseases.
Whilst the media coverage of the monkeypox outbreak is alarming, we would like to reassure our patients that as it stands, the risk is still very minimal and vaccination is not advised as a precautionary measure. Whilst vaccines will undoubtedly be a key part of containing the outbreak, for now, only people who may have been exposed are being offered vaccination.
Our Medical Director & Travel Medicine Specialist, Dr Richard Dawood explains;
“Lots of people have been getting in touch with us to ask about a monkeypox vaccination, but this is not available privately. It is currently only being offered to anyone identified as a direct, close contact of a confirmed case deemed to be at sufficient risk.
The current outbreak does, however, highlight the need to think about your vaccine protection more generally, whether for travel or simply to protect your health and well-being, taking advantage of the best vaccines currently available.”
In a more general sense, it is never too late to catch up on childhood vaccinations, incomplete vaccination courses or any required boosters.
Your immune system naturally decreases with age and certain diseases are also more prevalent in older adults so there may be new vaccinations which are now suitable for you to consider for preventable diseases. Some health conditions can also weaken the body’s immune response, making you more vulnerable to infectious diseases, complications and hospitalisation. Therefore, it is important to ask your GP which vaccinations would be suitable for keeping you healthy.
– For more information on wellness vaccinations.
If you are travelling soon and haven’t had a travel consultation with a travel nurse, perhaps it is time to consider one. Travel nurses are experts in travel health and will advise which travel vaccinations & medications you should consider based on the risk of where you are travelling to and your itinerary once there.
– For more information on travel consultations.
To conclude, we’d like to dismiss a couple of dangerous myths about monkeypox that are unnecessarily scaremongering the public:
Myth 1: Monkeypox is as contagious as COVID-19 or smallpox
Fact: Monkeypox is far less contagious compared to smallpox, measles, or COVID-19.Myth 2: Monkeypox is a new virus.
Fact: No, the monkeypox virus is not a novel virus. It’s a known virus and is generally seen in central and western African countries as localised outbreaks.In summary, we, like the rest of the medical field, will be keeping a close eye on the progression of the Monkeypox outbreak and should our advice change based on new information, we will update this statement accordingly.
For more information on Monkeypox.
Everyone lives such busy lives, so much so that stress now seems an inevitable part of daily life. Whether it be work, personal relationships or even keeping up hectic social schedules, there is often very little time to truly relax.
When stress is chronic it will affect the body in many different ways, interfering with normal body functions such as digestion, blood flow, your pain threshold and also your ability to sleep. Your risk for depression and anxiety, heart attack and heart disease, obesity, eating disorders, and several gut problems also increases.
Tension across the shoulders, headaches, short temperedness, insomnia, tiredness, aches and pains, digestive disorders or menstrual problems are all made worse when the body is stressed and chronic stress can often be the root of unexplained infertility.
Common effects of chronic stress could include the following.
- Upset stomach, diarrhoea, nausea, constipation, heartburn, or other gut issues
- Rapid heart rate or chest pain
- Trouble sleeping
- Loss of sexual desire or reduced sexual function
- More colds or seasonal illness than usual
- Clenched jaw or teeth grinding
- Sore, tense muscles, especially in the neck and shoulders
- Constant worry
- Always seeing the “worst case scenario”
- Racing thoughts
- Feeling frazzled and unfocused
- Disorganisation and forgetfulness
Can you spot any of your mental or physical symptoms in the list?
So how does stress impact the body?
When subject to a stressor, adrenaline floods the body and primes the muscles and senses ready for action. Whilst this is useful to escape from danger, to meet that important deadline or to win the 100m race, when this ‘fight-flight’ stress response is constantly switched on, prolonged muscle tension and poor circulation eventually take its toll on the body. Often resulting in poor health, fatigue and ultimately adrenal exhaustion and collapse.
Our acupuncture specialist, Diane Timewell runs our acupuncture clinic in London. She takes a particular interest in the effects of chronic stress and how acupuncture can help with switching the body from this ‘fight- flight’ response into the parasympathetic ‘rest and digest’ side of the nervous system. Acupuncture can help with controlling stress and anxiety, as it affects the part of your brain that regulates emotions, reducing stress naturally.
Medical acupuncture stimulates acupoints of the body to promote the release of ‘happy hormones’ such as endorphins. This reminds the body to relax, let go of daily stress and signals that you are safe and secure so the stress response can be turned off. In doing so, proper circulation is restored allowing our internal organs to work as they should unhindered by tension. This produces a vibrancy and vitality that can be felt both physically and mentally.
When it comes to acupuncture treatment for stress, there is no one-size-fits-all approach. Whilst there are many points that consistently improve stress, when acupuncture is used to treat stress, the treatment will be fully bespoke.
Stress affects everyone’s body individually and so Diane will work with you to pinpoint all your personal imbalances, treating your whole body based on your particular symptoms and pain areas.
You don’t need to feel unwell to benefit from acupuncture medicine. High achievers, Type A personalities, those who want to climb every mountain are very often sympathetic-dominant adrenal types. Adrenaline is the motivator of the body and so to some extent all successful people will benefit from a certain amount of stress. Learning how to switch it off after the target has been achieved is the key.
Acupuncture treatment is an essential tool for both physical and mental well-being. It can be an excellent way to learn how to take control of your health and switch off chronic stress.
At Diane’s acupuncture clinic, she creates a safe and peaceful environment where you can de-stress, reenergize and regain your natural well-being and vitality.
You can book an acupuncture appointment with Diane online.
Chronic kidney disease (CKD) is a long-term condition where the kidneys don’t work as well as they should. In some circumstances, the loss of kidney function can get progressively worse over time but CKD only reaches an advanced stage in a small proportion of people. Although the damage is irreparable, sometimes if changes are made, CKD can be halted with no further damage occurring.
Chronic Kidney disease (CKD) is divided into 5 stages.
Stage 1 is the earliest stage whereby tests have indicated some level of kidney damage. It is important not to ignore a stage 1 diagnosis as this is the time to take action and make lifestyle changes so that the condition does not worsen. With every increase in stage, more kidney damage has been detected up until the last stage, stage 5. Stage 5 means the kidneys have lost almost all their function and it will be time for thinking about dialysis or a transplant.
What to do if your recent blood test shows a reduced kidney function.
Don’t panic, absorb the diagnosis and understand this doesn’t definitively mean your kidneys will stop working altogether. CKD should not be ignored as it can get worse over time but with careful monitoring and management it can be maintained and you can live long fulfilling lives without being unduly affected by the condition.
It is important to review your lifestyle and in particular, your diet. With early stage CKD (stages 1-3) it is paramount to be as healthy as possible and have a healthy balanced diet.
What do I mean by a healthy balanced diet?
This includes:
- Consistently eating freshly cooked food for every meal
- Limiting your intake of processed foods and avoid highly-processed foods
- Reducing your daily salt intake
- Having considered balanced meals – your lunch and dinner meals should contain proteins, carbohydrates and vegetables. Your portion size will depend on your weight and if you have diabetes
- Ensuring you have a minimum of 2-3 portions of fruits and vegetables each and every day
- Increasing your intake of plant based proteins such as beans, lentils, tofu, soya, seitan
- Drinking lots of water to remain well hydrated (ensure your urine runs clear)
- Being as active as physically possible for you
- Avoiding non-steroidal medicines such as ibuprofen, naproxen etc.
What is a renal diet?
You may have heard of the term, renal diet. The term is used quite widely amongst those who have CKD, but personally, I am not a fan of this term. It doesn’t really mean much and can often be misused. People often think it means a diet of low protein, low salt, low potassium and low phosphate – which is pretty hard to do all at once and not always necessary.
People newly diagnosed with CKD in particular often restrict their diet in a panic unnecessarily and in combination with online resources not being clear enough, this can cause a lot of confusion.
My advice would be to seek guidance from someone like myself, a dietician who can look at your lifestyle and individual health and work out a personalised diet plan. This will be much more achievable and as well as not feeling so overwhelming, you’ll only have to limit the foods you absolutely need to.
How do you monitor CKD?
The best way to monitor CKD is to have regular tests, either blood or urine. How often you require testing will be dictated by the stage of CKD. Your GP will determine what is best for you and it is best to ask them any medical and testing questions rather than your dietician who will focus solely on your lifestyle and diet.
______________
Ruth Kander is a kidney-specialist dietitian, to book an appointment with her please click here.
Women today lead incredibly busy lives. They run and organise homes and build successful careers, usually all whilst taking on the majority share of caring for their children and often their older relatives. It is therefore not uncommon for women to have little or no time to look after themselves, their health included.
In addition to not making time to prioritise their health, it seems that when women do put their health first and seek medical advice, they are less likely to feel heard and supported in comparison to their male counterparts.
A recent survey by The Department of Health and Social Care found that “more than 4 in 5 (84%) women they surveyed had experienced times when they (or the woman they had in mind) were not listened to by healthcare professionals.”
Based on the data they collected, ‘not being listened to’ appears to be present at all stages of the healthcare pathway. Specifically, many women told them:
- their symptoms were not taken seriously and/or dismissed upon first contact with GPs and other health professionals
- they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years
- if they did secure a diagnosis, there were limited opportunities to discuss or ask questions about treatment options and their preferences were often ignored
Many women recalled their symptoms being dismissed upon first contact with GPs and other professionals; women felt they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years; and post-diagnosis, discussions about treatment options were often limited, and some said their preferences were ignored.
To make matters worse, there is some evidence that due to historical clinical trials being disproportionately male-orientated there is much less research into women-only health concerns and assumptions have been made that similar medical treatments will work for both sexes. The top reasons for the under-representation of women in trials were the belief that hormone fluctuations could influence results and concerns that fertility could be affected. A widely accepted negative repercussion, amongst others, being that women are much more likely to experience adverse side effects of medications because drug dosages have historically been based on clinical trials conducted on men.
A combination of these factors may explain why there is a gender gap in health outcomes, with women experiencing poorer health outcomes in comparison to men. We strongly believe in equality and ensuring health is a top priority for all.
Therefore, here are the top health symptoms women should never ignore:
1) Any change in bowel habit and/ or urination
This includes blood in the stools, unexplained persistent abdominal pain, weight loss, lumps around the anus, lack of appetite, blood in the urine or increased frequency of urination. These are all reasons for seeing your doctor ASAP as these symptoms could be due to bowel, bladder or ovarian cancer. All patients should have an annual faecal occult blood (FOB) test to exclude bowel cancer, which has increased in incidence in the UK for reasons unknown. Or if you are looking for a more in-depth investigation, you should request a colonoscopy which entails looking at the bowel with a colonoscopy. This is the gold standard, but an FOB is the next best thing and far less invasive as a first investigative option. It takes no time at all and is a good preventative check.
2) Any changes to the breast.
Any breast lumps, skin changes, nipple discharge, nipple changes or pain in the breast must be checked ASAP. Breast cancer is the most common type of cancer in the UK and often can present insidiously. Get to know what your breast feels like so that any subtle changes can be detected as early as possible.
3) Skin lesions that do not heal.
Any scab on the skin which does not heal, especially around the eyes, nose, ears and face should be checked. All these areas are the most sun-exposed, and, as such, are more at risk of skin cancer. If these lesions are picked up and treated early, scarring is minimal, but if left, then disfiguring scars and skin grafts may be necessary.
4) Bleeding after the menopause.
If you experience any bleeding after 1-year of your last menstrual period, you must visit your GP for further investigation. Bleeding after the menopause is not common and could be an indicator of cancer of the uterus, or the cervix. They will usually opt for a biopsy of the uterine lining to exclude both – don’t worry, this doesn’t hurt.
5) Always have regular cervical screens.
Most people don’t find cervical screens painful, although they can feel somewhat uncomfortable. If you are concerned about the pain or you have previously found the procedure painful with the NHS, you can opt to book a private appointment. It is important that you don’t miss your appointment.
6) Bleeding between periods.
At any age, you should never ignore bleeding between periods or after intercourse, as this can be a sign of cervical or uterine cancer. Whilst cervical cancer is monitored by regular screening, it is important to still get bleeding between periods checked out following a normal smear result. Cancer of the endometrium is becoming increasingly common in women who have not had children.
7) A persistent cough.
Regardless of gender, you should get a persistent cough checked out by your doctor, especially if you are coughing up discoloured sputum or blood.
8) Any unexplained changes to your body.
Any new indigestion, shortness of breath on exertion, neck or left arm pain requires follow up ASAP. Make sure a GP examines your chest and makes the appropriate investigations.
The same applies to calf pain or any pain in the chest. By taking a full history, examining you and doing quick and easy investigations, worrying conditions can be excluded, such as a pulmonary embolism or a heart attack.
Some recent examples of cases where other healthcare providers have failed our new female patients:
1) We saw a 36 year old who had not had a cervical screening for 5-years because the last one was so painful. The NHS advises a screening every 3-years but we advise yearly screenings to ensure any abnormalities are found as early as possible. 5-years is far too long!
2) We saw a woman who had a suspicious lump at her anal margin, which her usual GP had told her was part of her bladder. She wanted a second opinion because it had grown in size and was now painful. The patient was referred for an urgent assessment to exclude cancer.
3) We saw an 88 year old patient who was disfigured by a large basal cell carcinoma on her forehead, about which she was embarrassed. The patient had been seen by a dermatologist who had frightened her about having the lesion removed by saying she might not survive an anaesthetic. The patient wished that she had taken the risk and asked to be referred back, as the skin lesion was disfiguring and ruining her quality of life.
** The outcomes of these patients are yet unknown, but they are all certainly serious health concerns that should have been properly addressed long before now.
We want to encourage women to take ownership over their health and be assertive when they feel that something has changed from our normal. If they feel like they are not being taken seriously or not being heard, they should seek a second opinion.
If you cannot get an appointment with your usual GP or through the NHS, rather than waiting for weeks and worrying about what it could be, make an appointment with a private GP who can usually see you on the same day!
Put your mind at ease with private healthcare.
Fear of flying, otherwise known as aerophobia, is an excessive worry about air travel. It is one of the most common forms of phobia and according to YouGov, around 24% of Brits have some form of anxiety about getting on a plane.
People suffering from fear of flying experience extremely anxious thoughts which are often so powerful they become physical symptoms. These can include shallow breathing, experiencing chest tightening, sweaty palms, feeling nauseated or lightheaded and sometimes these even develop into a panic attack, meaning many opt to avoid air travel altogether.
For some, it will have been a lifelong problem that has meant never flying at all. For others, who have flown many miles in their lifetime, it is a problem that slowly creeps up on them over time. In both circumstances, the fear can be debilitating and symptoms often trickle into other areas of life.
Like all phobias, there is little logic to support the anxiety that it causes – travel is in fact the safest form of transport and you are much more likely to die from a car accident than in a plane crash. Knowing that fact does little to ease the flying-related anxiety of an aerophobic sufferer.
So, what can be done to overcome our fear of flying?
Understand the reason why you’re a nervous flyer
Fear of flying is usually caused by a combination of factors. Understanding the root cause of your own phobia is perhaps the first step in overcoming it. Is it a fear of heights? Claustrophobia? Was it that film you watched as a child? Or has a particular world event sparked the fear? Many people suddenly developed a fear of flying after 9/11 for example. Figuring this out will then allow you to tackle it in the right way and using the appropriate techniques.
Fight fear with knowledge
Some experts suggest the first strategy for everyone suffering from a fear of flying is learning about the aeroplane and the science behind flight. Our anxiety is fed by ‘what if?’ catastrophic thoughts. Once you become knowledgeable, your ‘what if’ thoughts will be limited by the facts. There are professionally designed courses that will explain aspects like air traffic control, anti-terrorism measures, and what happens during turbulence. Some courses use Virtual Reality (VR) to simulate a flight, explaining everything along the way with the aim of injecting logic into an illogical fear.
Seek medical help for anxiety, fear and panic
From here, a form of therapy may help to identify and break anxiety cycles. There are many different types of therapy and choosing the right one for you will depend on your own needs and goals. Hypnotherapy and cognitive behavioural (CBT) are some of the most commonly used, but there are countless more to choose from. Deciding which is the most appropriate form of therapy can be daunting, so it may be helpful to seek advice from your GP or a travel nurse.
For those who manage to make it onto the plane, there are quite a few, simple personal techniques that can be used to calm your nerves.
Deep breathing techniques
Making a conscious effort to breathe slowly and deeply can interrupt panic. Deep breathing is known to trigger a comfort response and will help prevent hyperventilation.
Distract yourself
Reading a book or listening to a good podcast can refocus your mind and attention.Distracting yourself from the fact that you are flying can be a great way to keep calm if you’re a nervous flyer.. Time tends to pass much more quickly when adequately distracted.
Tell the flight attendants
Alerting the flight attendants of a nervous flyer could also help – with their training and expertise, they are ideally placed to provide reassurance and will regularly check in on you during the flight.
Avoid coffee and wine
Nervous flyers in general should avoid drinking coffee and wine before and whilst flying. Both can leave you more dehydrated than normal. The extra caffeine in coffee can aggravate anxiety issues and the Dutch courage wine offers will pass leaving you more susceptible to jet lag. Stick with water where possible.
Tea really does help
It’s very British to recommend tea to make everything better, but there are many different herbal teas available which can help with relaxation, reducing stress and calming anxiety. Peppermint, camomile, lemon balm and lavender teas are the most commonly used.
We advise nervous flyers and people with aerophobia to seek further information and guidance from their GP who will be able to make a formal diagnosis and treatment options.
For more advice and information you can book a travel consultation appointment.
Ageing is an inevitable part of living. As we age, many physical and psychological changes affect our overall health and these vary from person to person.
The general myth is that as you age, you become more fragile and that this is unavoidable. This is most certainly not the case. There are always things we can do to help keep healthy in our older years and these changes can slow down or even prevent certain health conditions from developing.
The term “fragile” is defined as not “strong or sturdy; delicate and vulnerable” and is most often used to describe older ladies. One particular age-related health issue that supports this description would be osteoporosis.
Osteoporosis is a degenerative disease that weakens and thins the bones which makes them fragile and more likely to break and is becoming increasingly common. It is much more prevalent in women than men due to the menopause directly affecting hormone balances and this directly affects bone density. It is important to prevent osteoporosis as we age as 75% of fractures due to osteoporosis occur in people aged 65 and over.
There are several things you can do to help prevent osteoporosis:
1) Do regular, weight bearing physical activity.
The lack of regular exercise will result in loss of bone and muscle, so adults who are inactive are more likely to have a hip fracture than those who are more active. Adults should aim to do at least two and a half hours of moderate-intensity exercise every week. Weight bearing and resistance training are a particularly great way of improving bone density and helping to prevent osteoporosis.
2) Eat plenty of calcium and Vitamin D containing foods.
Your diet is very important and the nutrients we get from the food we consume will affect how strong our body is. Eat plenty of dairy, seeds, eggs, oily fish, protein, fruit and vegetables. Additionally, try to get at least 15-minutes of sun exposure per day to increase your Vitamin D intake. As we know in the UK, such sun exposure is not always possible during the winter months and, if this is the case, taking a daily Vitamin D supplement is advised.
3) Maintain a healthy weight.
As you get older, you start to lose lean body mass like muscle and bone density and this can start to happen yearly from the age of 30. Being underweight weakens your bones so it is important to keep your weight in a healthy range. A good indication, although not exact, is your BMI. For most adults, a healthy BMI range is between 18.5 and 24.9, so try not to let your BMI fall below 19.
Those who suffer from eating disorders such as anorexia and bulimia are at a higher risk of fragility due to the conditions causing further bone density loss. This can happen to anorexic and bulimic sufferers of all ages.
Older people should aim to consume a varied diet, consisting of enough calories for maintaining a healthy weight.
4) Limit your consumption of alcohol.
We’d recommend that you drink no more than a maximum of 2 units of alcohol per day. Any more than this has been demonstrated to increase the risk of bone fracture. Alcohol abuse has detrimental effects on bone health and increases a person’s risk of developing osteoporosis.
5) Stop smoking and definitely don’t start!
Smoking is a known risk factor for osteoporosis as it increases bone mass loss. In fact, smoking doubles the risk of hip fracture.
Generally, being healthy is the key to avoiding fragility and in particular preventing osteoporosis as we age. Having an annual health medical can highlight any areas of concern. They can monitor the progression of any pre-existing health issues, as well as detect arising conditions in the early stages. You can book your annual medical online
In addition to making healthy lifestyle choices, it is also important to book a doctor’s appointment should you notice any changes to your health. The sooner a health concern is addressed, the easier it is to treat. You can book a GP appointment online.
At Whitby & Co. and the Fleet Street Clinic, we strongly believe in our duty to protect our colleagues and patients alike, independently of Government regulations. We have stayed open since the start of the pandemic, delivering key health services for our patients, face-to-face and without interruption, but with no compromise on safety.
Despite the recent changes to isolation legislation and access to testing, you can rely on the fact that we plan to keep regularly testing all our staff for the foreseeable future – using highly sensitive rt-PCR tests in our own onsite lab. The benefits of rt-PCR testing means the infection is detected much earlier, rather than at peak infection which is when lateral flow tests only turn positive. We will advise our employees to continue to isolate in the event of a positive test: we prefer to pay our staff to stay at home, rather than risk spreading Covid-19 among colleagues or to our patients.
Whilst we absolutely recognise that the Omicron variant is less severe than previous dominant strains of SARS-CoV-2, we are not willing to compromise the health and wellbeing of our employees or patients when the severity is so unpredictable person to person. For peace of mind and to protect those most vulnerable, we will continue to wear face masks and prevent infectious individuals from entering our premises.
Our internal strategy appears thus far to be successful: although a number of us have inevitably had Covid-19 over the course of the pandemic, there have certainly been no outbreaks among staff from workplace transmission.
Beyond this, you can rely on the fact that all our staff are fully vaccinated, and indeed (like all health workers) were prioritised for vaccination from the earliest opportunity.
Whatever your reason for coming to see us at 29 Fleet Street – whether for an eye examination, a GP appointment, travel vaccines, or to use any of our other services, you can be confident that we have all been vaccinated and have had a recent negative coronavirus test. And this extends to if any of us come and see you at your home, office or place of work, you can be completely assured that we have used all our resources to protect you, your family and your colleagues.
In theory, a hybrid working week is the best of both worlds for both the employee and the employer. It combines the best of pre-Covid collaborative office-based working with the flexibility of working from home. Allowing employees to be fully engaged with the company and their colleagues all whilst offering the opportunity for solo focus that comes with home working. It is thought that many companies will permanently adopt a ‘hybrid’ way of working.
With this being a long term model of working, many people have realised that their makeshift home office will not suffice without causing havoc on their bodies. Making sure that the physical and ergonomic set up of your home office is correct is imperative for avoiding any musculoskeletal problems.
A bad home office setup has the potential to cause you repetitive strain injury, lower back pain, increase your risk of carpal tunnel syndrome and could even be the cause of your headaches and migraines. It is worth taking the time to understand what a good home office set up is and work out the best way to adapt your setup to make a healthier home working space for you to work from.
Back to basics:
We always start at the basics. Even though they may seem obvious, time and time again it has been proven never to assume the basics are widely known. So, let’s go over them briefly:
- Choose the right chair: You should invest in a chair that offers adequate support. Try and get a chair that is fully adjustable – meaning you can alter the height, back position, and tilt to best suit you. This will be much more comfortable and will support your body when you’re sat for long periods of time.
- Support your back: You should adjust your chair so that your lower back is supported, this will reduce strain on your back. Your knees should be slightly lower than your hips.
- Arm position: Your elbows should be positioned by the side of your body so your arm forms a right-angled L-shape at the elbow joint.
- Screen level: Your screen should be directly in front of you with your monitor placed at about an arms length away, with the top of the screen roughly at eye level. You may need a screen monitor to achieve this.
- Keyboard and mouse position: Your keyboard should be placed in front of you with a 4-6 inch gap at the front of the desk to rest your wrists. You might consider a wrist rest. You should aim to position your mouse as close to you as possible. A mouse mat with a wrist pad can help.
Now for some suggestions a little more out the box:
L-shaped desks
It’s important to be fully facing whatever you’re doing. Trying to work while twisted, even a little, is going to cause problems. This often happens when someone needs to type at a screen, but also use a book, write, or use two monitors. A great solution is to set up your desk in an L shape (two desks perpendicular works). This allows you to swivel your chair to face whatever you’re doing at that moment.
Supplementary monitors
Plain monitors are cheaper than you’d think. Instead of hunching over a laptop, or piling books up to put a screen on, think about investing in an extra monitor, maybe with a bigger screen and a stand. If you need documents open, think about a second monitor, it will cut down on mouse usage of having to keep swapping between windows. It can also be used vertically to get whole pages on which means less scrolling. Equally, extra keyboards and mice are really quite cheap and ergonomically so much better. Lots of different mice for arm/shoulder complaints are available. You can have a full setup in place and simply plug in your laptop when you arrive.
Foot stools
If your desk isn’t height adjustable, chances are your chair is adjusted to match the desk, not you. This is ok, as long as your feet are still flat on the ground with knees at about 90 degrees. If not, you may find a footrest makes a great difference, taking pressure off the back of the thighs and preventing over extension of the lower back. If you’re too tall, leg extensions for the desk are a simple remedy.
If you’re looking at buying a new desk. I recommend adjustable ones. Costco stocks an electric one for under £200. This can allow you to spend part of the day working, standing.
Aesthetics
Creating an environment that is visually pleasing will do wonders for your mental wellbeing. This is equally as important as physical setup and will improve mood, lower levels of tension, and increase productivity. Try to utilise lots of natural light if you can. Position your desk where it feels airy and open. Choose light colours to surround your workspace. Add a couple of green leafy plants. Whatever little changes that make you feel happy!
Movement
Try to incorporate regular movement to your working day. If you can, get up every hour for 30 seconds and have a quick stretch. When working statically for long periods of time, the muscles fatigue.
This may all seem like a lot to consider for a workstation but these are simple changes that can easily be implemented. Optimising your work space can make a huge difference in both your comfort and productivity.
If you are experiencing any musculoskeletal problems, book an appointment online with our osteopath, Andrew Doody.
Or for more information on osteopathy, see here.
Throughout the pandemic we have supported many industries trying to navigate business-as-usual alongside managing the potential risk of coronavirus in the workplace.
Identifying covid-positive individuals as well as outbreaks is essential, but it is also important not to underestimate the peace of mind testing brings to employees who may be anxious about catching covid-19 in the work environment, especially those who have been in close contact with someone at work who has subsequently tested positive.
The creative arts industry has been particularly impacted by closures, and given the close-contact nature of the theatre and performing arts sector, outbreaks do occur. The speed at which those infected can be identified can make all the difference between a show going ahead or being cancelled.
We have supported Kenny Wax Productions for the last 2 years with crisis management and routine testing using our ultra-rapid covid-19 rt-PCR testing service.
Here’s how we supported the production of MAGIC GOES WRONG during their Christmas crisis:
At 15:18 on New Year’s Day (a Saturday), we received a text to say that the entire cast of MAGIC GOES WRONG was heading straight to Fleet Street, following a positive result from one of their actresses. The only way the evening performance could go ahead was to determine whether covid-19 had spread throughout their cast, or not.
We understood the urgency of this situation and quickly and calmly took samples from a cast of 21 against the clock. We ran them through our lab at the same time, which can be quite a challenge. Since we knew that there would not be enough time to re-run samples, this needed to be done with special care. For us to be able to give Kenny the “thumbs up” to go ahead with the evening show, it was imperative we got things right the first time.
One of the best things about our NeuMoDx lab equipment is that we can load each sample as soon as it is taken, rather than waiting for the complete batch. We started running samples immediately, the last of them had finished running by 18:10, when we were able to assure Kenny that it was safe for the cast to go on with the show.
We were able to go from initial text enquiry to sample-taking and final, confirmed results for the entire cast in just over 3 hours.
Kenny Wax, the Producer of MAGIC GOES WRONG explains:
“Our West End hit MAGIC GOES WRONG had managed to avoid shutdown. However, an actress who had been feeling a little unwell leading up to New Year and continuously tested negative on lateral flows, finally came through with a positive test on Saturday morning 31st December. Hearing this news, the rest of the cast became very anxious about continuing performances until they were confident that covid had not spread throughout the company.
As Producer of the show, I was made aware of this information at 1.45pm. There was due to be a matinee at 2.30pm and an evening show at 7:30pm. We had no other option than to cancel the matinee but in an attempt to save the evening performance (a Saturday Night), at very short notice we attempted to get the whole company of 21 people PCR tested in the afternoon. To achieve almost the impossible everyone set off for the Fleet Street Clinic and by 6.10pm, we received the good news that the rest of the company had tested negative on the PCR and we were able to continue with the evening performance and the following two
shows on the Sunday. This not only saved us another financial blow due to cancellations at the box office, but we were able to provide entertainment to 1,500 customers across those three performances.Dr Dawood’s staff at the Fleet Street Clinic are always polite, friendly and efficient. They fully understood the nuances of working with a West End theatre production company on a very tight deadline. I am very grateful for their continuing support and cannot recommend them highly enough.”
For more information on our corporate coronavirus testing services and other covid-19 support services.
Weight loss has become a thriving industry and we’re bombarded constantly with unhealthy FAD diets, weight loss programmes, influencers selling teas and pills all promising to help us lose weight. Many of these are promoting quick fixes which are not advised by doctors or dieticians. It can be really hard to know what information to trust. To help navigate the sea of information (and misinformation!) surrounding weight loss, we have asked one of our GPs, Dr Belinda Griffiths, and our dietitian, Ruth Kander, their advice on how to lose weight safely and successfully.
Firstly, it is important to note that weight loss should be consistent and gradual as it can be dangerous to lose too much weight too quickly. Dr Griffiths suggests that “a safe weight loss is 1-2 lbs or 0.5-1kg per week… Greater weight loss than this per week can lead to malnutrition, exhaustion, increased risk of gout and gallstones.” There is also an increased risk of developing an unhealthy relationship with food which, in extreme circumstances, could lead to eating disorders.
Ruth added, “Losing weight gradually and at a healthy rate is key.” Remember, it’s all about consistency! Perseverance will amount to healthy lifestyle changes which will allow you to achieve your weight loss goal.
Don’t underestimate diet
Both Dr Griffiths and Ruth agree that diet is the most important factor when it comes to weight loss. As Ruth explains; “having a healthy balanced diet that is lower in calories than our body uses is a good way to start the weight loss journey. If we don’t reduce calorie intake, one won’t lose weight:.” – this is known as being in a calorie deficit. The amount of calories that will result in weight loss will vary from person to person and depend on the amount of exercise the individual does. In order to lose weight, you will need to burn more calories than are consumed and therefore restricting your calorie intake is the simplest way of losing weight.
Foods to focus on
Ruth recommends that “people should focus on a variety of foods when trying to lose weight”. While Dr Griffiths suggests, “focusing on a range of lean proteins (including meat and fish), vegetables, high fibre foods (such as quinoa, bran flakes etc) and fruit in moderation”. Vegetarians can substitute in lentils, nuts, beans and tofu instead of meat and fish. In general, high calorie foods such as fried food, cakes, biscuits, chocolate and sugary drinks should be avoided.
Let’s get physical!
Although weight loss is still achievable without much exercise, incorporating exercise into your lifestyle will not only aid weight loss, but will generally improve your overall health. Any exercise is better than none whether it be tennis, swimming, or even walking, “whatever you are capable of, just do it!” is Dr Griffiths advice. Ideally, a combination of exercise is best for weight loss – this includes cardio / fat burning and resistance or weight training. Get those steps in! An easy way to incorporate more exercise into your daily routine is by aiming to walk at least 10,000 steps per day. This easy change can make a big difference and remember, as Dr Griffiths says “the more exercise you do, the greater calories are burned” – it’s as simple as that!
Don’t forget about NEAT movements!
NEAT (or Non-exercise activity thermogenesis) movement refers to the physical movement we do day-to-day that isn’t necessarily planned exercise and “encompasses the energy that we expend by simply living”.This includes the calories we burn breathing, eating, sleeping etc. Dr Griffiths suggests that “you can increase NEAT movement easily in your everyday life by making simple changes such as taking the stairs rather than the lift, by standing rather than sitting, by walking instead of taking the train/ bus/ tube or even by carrying bags rather than having items delivered”. It all adds up! These simple swaps will increase the number of calories you burn and help facilitate weight loss.
What to do when you plateau
The first stint of weight loss can make it seem a little too easy as you tend to lose weight more easily in the beginning, but a common issue lots of people face is when weight loss reaches a plateau. This is where you stop losing weight to the same extent you were before, or stop losing weight for a period of time. This can feel disheartening and more often than not, people tend to give up at this stage. Dr Griffiths states at this point “it is a case of persevering with calorie restriction and regular exercise and gradually weight loss will resume.” If it doesn’t, Ruth suggests “ looking at what you’re eating to see if anything has slipped”. She states “maybe you’re not taking into consideration extra calories here and there” but they all add up. See if there are any areas of your diet where you could be a little stricter, or consider starting or upping your exercise.
Sleep and Stress
A good night’s sleep and keeping your stress levels down will be your friend when it comes to weight loss. “In order to lose weight, you need to be in the correct frame of mind and life circumstances” says Ruth. Research has shown that you tend to eat more and make poorer food choices, including seeking comfort food, when you are sleep deprived. This is because not getting enough sleep “disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite” says Dr Griffiths.
Stress can also play a part in weight loss as Dr Griffiths explains that “stress increases cortisol levels which increases gastric acid output and makes you feel anxious and hungry”. Ruth adds “there is also a theory that being stressed can limit weight loss in terms of hormonal activity in the hypothalamic-pituitary axis which can lead to the release of hormones that can limit weight loss”. Keeping it simple, “to lose weight, good sleep and minimal stress would be ideal”.
Final thoughts
Trying to lose weight can seem complicated, confusing and difficult, but when you really break it down, the ingredients to losing weight successfully are actually very straightforward. If you stick to these simple rules and you are patient and consistent, the weight will come off and you will achieve your goals.
If you feel that you are doing everything right and you still aren’t losing weight, or are even putting weight on, there could be something else causing this. You may have an undiagnosed underlying medical condition and we’d advise you to visit your GP to make sure everything is well.
If you would like any extra support with your weight loss, why not book an appointment with Ruth. Or if you have any concerns over your health, please book an appointment with one of our GPs.
If you are feeling sad at the start of the year, don’t worry, you are not alone.
Although it comes around every year, we always seem to be caught off-guard by what has now commonly become known as “The January Blues”.
The January blues is another name for situational depression and is associated with the way we think and feel. Around this time of year, the weather is cold and gloomy, the days are shorter and the nights are longer, plus you may be experiencing post-Christmas exhaustion, debt and perhaps even dread going back to work.
Symptoms of the January blues are things such as low mood and sadness, lack of motivation, tiredness and low energy. These are all normal feelings, if temporary.
Most likely, your negative mood will be brought on by the anticlimax of reality after the exciting events of December & the New Year. Ever heard that old phrase, “don’t cry because it has ended, but smile because it happened”? Find comfort in knowing that you are absolutely not alone in feeling blue in January. In fact, many people in the UK feel especially down in January but the good news is that the January Blues are temporary and typically only last a couple of weeks. You don’t need to take any medication as your thoughts and feelings should naturally return to normal.
If it doesn’t and you are experiencing prolonged or worsening thoughts and feelings, you may actually have Seasonal Affective Disorder or SAD, which is different. SAD is clinical depression caused by a person’s biology. It is much longer-lasting, sometimes months on end and likely to occur every year in winter. You should see a doctor to discuss your symptoms as if you have SAD, a range of treatments are available to assist recovery. More information on SAD can be found here.
Remember, please be kind to yourself and know that you’re not alone.
For more information on our GP Services.
To book a GP appointment online, click here.
We no longer offer hypnotherapy at Fleet Street Clinic.
In 2021 we stopped providing hypnotherapy as a service to our patients. We do still offer other supporting services, which may be of interest and suitable for your needs:
If you are unsure, please contact us and we can assist you further.
For an overview of all other services available at Fleet Street Clinic, click here.
Most people experience fluctuations with their weight and it is common to gain weight naturally as we age. For the most part, diet changes, eating more or reducing exercise are the main causes for gaining weight. However, if a person gains weight in a short period of time for no reason, this could be the sign of an undiagnosed, underlying health condition. There are several conditions and circumstances that are known to cause weight gain, some of which can be serious and require medical attention.
Here are just some medical conditions which can cause sudden weight gain:
Polycystic ovary syndrome (PCOS)
This is a hormonal condition which affects the way a woman’s ovaries work. A common symptom of PCOS is weight gain, particularly around one’s middle. Weight gain is rarely the sole symptom, it is usually part of multiple symptoms including acne, excessive hair, irregular periods and/ or thinning hair. PCOS makes women less sensitive to insulin or cause insulin-resistance which can lead to weight gain and secondary conditions such as diabetes.
Hypothyroidism
A common cause of unexplained weight gain in men and women comes from having an underactive thyroid. This is because when a thyroid is underactive it doesn’t produce enough thyroid hormones, which in turn affects your metabolism, slowing it down. Hypothyroidism can be diagnosed with a thyroid function test and if diagnosed, it can be easily treated with a replacement hormonal tablets.
Cushing’s syndrome
This is a rare hormonal disorder which is caused by elevated levels of cortisol in the body. Cortisol is responsible for regulating metabolism and appetite, which means elevated levels can slow down your metabolism as well as increase hunger, both of which can cause weight gain.
Insomnia / chronic lack of sleep
Being sleep deprived can result in making poor food choices, including seeking unhealthy foods and eating more than usual. This is thought to be because a lack of sleep disrupts the hormones in the brain (Leptin and Ghrelin) that are responsible for appetite.
Medication
Certain medications affect metabolism which can cause weight gain and weight loss. Medications such as steroid medication can cause weight gain, bloating and swelling due to water retention.
Lipoedema
This is a problem caused by an issue with the lymphatic system that causes an abnormal build-up of fat in the legs and sometimes the arms. This usually results in the upper body being generally a much smaller size compared to the lower half of the body but typically affects both sides of the body equally. This condition can also be painful and cause tenderness or heaviness in the limbs. Lipoedema mainly affects women and it is rare in men.
Chronic stress, depression and/ or anxiety
Mental health issues can sometimes cause people to turn to food as a coping mechanism, often triggering compulsive eating behaviours. Additionally, higher cortisol levels are often found in people with depression which is known to increase appetite and the motivation to eat. Antidepressant medication can also increase hunger as they interfere with serotonin levels – a neurotransmitter that regulates appetite.
Menopause
Women going through the menopause often experience weight gain. Changing hormone levels affect the way the body stores fat and can cause women’s bodies to store, rather than burn, calories. Women also generally need less calories after the menopause, and so, if you do not adjust your calorie intake, you are likely to put on weight.
PMS
During PMS (premenstrual syndrome), progesterone levels surge and dip which are known to increase appetite (the cause of which are unknown). PMS can also cause weight gain as a result of water retention.
While many of these causes are rare, they are possible and anyone experiencing unexplained weight gain should visit their GP to rule out anything that may require medical care or treatment. It’s always best to be on the safe side! And if everything is normal, your GP can provide you with tips and advice on how to manage your weight gain.
If you are experiencing unexplained or sudden weight gain, or think you might be displaying symptoms of the conditions mentioned above, please book a GP appointment today.
Fleet Street Clinic receives UKAS ISO 15189 Accreditation for testing of SARS-CoV-2 (COVID-19)
Fleet Street Clinic has confirmed its UKAS ISO 15189 accreditation for the detection of the SARS-CoV-2 virus (COVID-19), granted on 8th December 2021.
UKAS is the National Accreditation Body for the United Kingdom and is appointed by the UK Government to access competence and accredit organisations that provide testing services. It is an internationally recognised accreditation body.
Fleet Street Clinic has been at the forefront of private Covid-19 testing since the start of the pandemic and is one of the very few private healthcare clinics in London who can deliver ultra-rapid testing to private patients and corporations.
Receiving the UKAS ISO 15189 accreditation confirms that Fleet Street Clinic has continuously met the standard of accuracy and safety for private covid-19 testing and offers quality assurance.
Our full scope of accreditation can be found here.
With almost 25 years of diagnostics experience, Fleet Street Clinic can be trusted with confidence to deliver private Covid-19 testing.
Have you thought about Corporate Flu Vaccinations?
The winter season can be problematic for businesses, as employees take time off due to sickness and annual leave. Illnesses such as flu are most likely to affect employees during the autumn and winter months.
If you are in charge of organising your company healthcare and wellbeing programmes, you may be unsure about whether to offer flu vaccines. The fact is, workplace flu vaccination can offer a significant return on investment in terms of reduced absenteeism and increased efficiency in the office, meaning there is one less thing to worry about.
We respond to some common questions about corporate flu programmes here:
WHAT TIME OF YEAR SHOULD I ORGANISE MY COMPANY’S corporate FLU VACCINATIONS?
Plan ahead and book the session as early as you feel able. This will ensure you’ll get the dates you want to suit your companies needs.
For best protection, the optimal timing for vaccination is between September and early December, before flu viruses begin to circulate. Each year, October and November prove a popular choice but we can vaccine up until February 2021.
WHY SHOULD I PROVIDE CORPORATE FLU VACCINATIONS FOR MY STAFF?
A flu outbreak in the workplace can cause an increase in absenteeism, which can result in a loss of productivity as well as increasing the workload of any staff that do not succumb to infection. For large and small organisations alike, this can have a massive impact on productivity and revenue. Furthermore, this year in particular, flu symptoms are extremely hard to distinguish between Covid-19. Getting the flu jab has become even more important than in previous years to eliminate potential confusion.
Workplace vaccinations are a great way of promoting health and wellbeing among your employees and demonstrating a caring ethos.
Benefits of the Flu Vaccine include:
- Flu vaccinations improve the wellbeing of your employees, promoting job satisfaction and a positive work atmosphere.
- Flu vaccinations reduce absenteeism.
- The greater the number of people who are vaccinated, the less potential there is for flu to spread through your workplace, among staff members families, and within the local community.
- Annual seasonal flu vaccination is the best way to reduce the chances of becoming ill with the flu.
HOW MANY PEOPLE TAKE UP THE FLU VACCINATION?
Workplace flu vaccination uptake can vary. Internal promotion and communication can make a big impact on likely numbers; motivation to avoid illness, and perception of current risk are also key factors. A good general guide, based on past years indicated an uptake of between 25%-45%. Due to more awareness of viral infections due to Covid-19, we anticipate this uptake to be higher this year and that given the option, most staff would probably choose to be vaccinated.
How Much Money Can You Save Your Company with a Flu Vaccine Programme?
Calculate the likely savings your company can make from a successful flu programme by visiting our corporate flu calculator here.
Fleet Street Clinic offers workplace flu vaccination programmes both on-site across the UK, and at our drop-in clinic in central London, via our flu vaccination programme, FluJabs.Org.
Get in touch and make an enquiry if you would like more information or a you can get quote for your company.
Sleep is one of our greatest allies when it comes to health and wellbeing. It is associated with a number of health benefits which can have a huge positive impact on our daily lives.
Conversely, a lack of sleep can be detrimental – research has even found that not getting enough sleep can negatively impact some aspects of brain function to a similar degree as alcohol intoxication!
Dr Belinda Griffiths discusses some of the mental and physical health benefits of getting a good night’s sleep.
Immune System
During sleep, your body releases cytokines, which are essential for the regulation of the immune system. Cytokines are required in increased amounts when you are attacked by a pathogen (when you’re ill) or under stress. The level of cytokines increases during sleep, and therefore lack of sleep hinders the body’s ability to fight infections. This is also the reason why the body tends to sleep more while suffering from an infection.
Weight Control
When you’re well-rested, you’re less hungry. Being sleep deprived disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite.
With those out of balance, your resistance to the temptation of unhealthy foods goes way down. And when you’re tired, you’re less likely to want to get up and move your body. Together, it’s a recipe for putting on the pounds!
Athletic Achievement
If your sport requires quick bursts of energy, like wrestling or weightlifting, sleep loss may not affect you as much as endurance sports like running, swimming, and biking. But you’re not doing yourself any favours. Besides robbing you of your energy and time for muscle repair, lack of sleep saps your motivation, which is what gets you across the finish line. You’ll face a harder mental and physical challenge – and see slower reaction times. Proper rest sets you up for your best performance.
Memory
When you’re tired, you can have difficulty recalling information. That’s because sleep plays a big part in both learning and memory. Without sufficient sleep, the brain finds it difficult to focus and take in new information in the first place and then doesn’t have enough time to properly store information as short-term memories. Sleep helps enable you to retain memories and store information.
Sleep also allows for your mind to rest, repair and rebuild, the same way it does for your body. As you sleep, your brain begins to organise and process all the information you’ve taken in during the day. It converts these short-term memories into long-term memories – this helps you to learn.
Concentration
Not sleeping properly can mean that both your body and brain don’t function properly the next day. It can impair your attention span, concentration, strategic thinking, risk assessment, reaction times and problem-solving skills. This is particularly important if you have a big decision to make, are driving, or are operating heavy machinery. So, getting plenty of sleep can help you stay sharp and focused all day long.
Mood
Another thing your brain does while you sleep is process your emotions. Your mind needs this time in order to recognise and react in the right way. When you cut that short, you tend to have more negative emotional reactions and fewer positive ones. Lack of sleep can cause bad temper and anxiety, so the better you sleep, the better your ability to stay calm, controlled and reasonable.
Chronic lack of sleep can also raise your chance of having a mood disorder. One large study found that people with insomnia were five times more likely to develop depression, and the odds of having anxiety or panic disorders are even greater.
A refreshing slumber helps you hit the reset button on a bad day, improve your outlook on life, and be better prepared to meet the challenges of the next day.
Heart Health
While you sleep, your blood pressure goes down giving your heart and blood vessels a bit of a rest. The less sleep you get, the longer your blood pressure stays up during a 24-hour cycle. High blood pressure can lead to heart disease and strokes. Therefore, it is important to keep your blood pressure down.
Pain Threshold
Poor sleep and pain mutually reinforce each other. Sleep deprivation increases pain sensitivity and reduces pain tolerance. Therefore, something will feel more painful when you’re tired.
It is clear that sleep is an essential part of helping us stay physically and mentally healthy. What better excuse to have a few extra hours of sleep a day!
If have any concerns about your health, book a GP appointment today.
SUMMER CYCLING
Summer is the perfect opportunity to dust off your bike and think about turning that commute into an opportunity to get fitter or shed a few pounds!
Cycling – a low impact sport
Compared to many sports, cycling is one with a relatively low injury rate. Crashes and collisions apart, cycling is impact free – good for your joints and muscles. In addition, if you select the correct gear to match the terrain, it means that you can avoid overloading your muscles and joints, keeping the cranks spinning rather than pushing a big gear.
Also important is that because your feet are fixed in place, spinning the cranks requires very little coordination, which also reduces the risk of injury due to poor technique, which is very common while running. Still, despite all these advantages, cyclists can, and regularly do, suffer overuse injuries.
Fix a good riding position:
One of the main issues is the set up of the bike itself. Here are a few pointers as to how to best achieve a good riding position:
SADDLE HEIGHT
This should be positioned so that when the pedal is at the bottom of the stroke and the ball of your foot is on the pedal, your knee should have a slight bend in it. If you want to get technical, saddle to pedal distance should be 109% of your inside leg measurement. Hips shouldn’t move sideways during crank rotation and you shouldn’t have to stretch at the bottom of the pedal stroke. Don’t be put off by feeling you have to come off the saddle to touch the floor.
SADDLE ANGLE
This should be in a horizontal position, parallel with the floor when viewed side on (but sometimes a very slight downwards tilt can be helpful for those who experience a lot of pressure in the perineum area. However, don’t do this just because it feels more comfortable, as this can cause lessen support and affect riding position).
POSITION OF THE SADDLE
With the pedals adjusted so that they are at the three o’clock and nine o’clock positions, a vertical line dropped from the kneecap of the forward knee should pass through the axle of the pedal.
HANDLEBAR POSITION
This is where opinion varies a little. Racers want the handlebars low to lower wind resistance, climbers want the handlebars low so they don’t feel too high when the bike’s angled up. The rest of us want them higher than this. A good rule of thumb is that you don’t want to be leaning on the handlebars too much, only holding them. If it feels like your upper bodyweight is being supported by the handlebars, try them up a little. Not all bikes are adjustable enough at the front but a stem raise is a cheap efficient way of remedying this. A bit more height in traffic is safer anyway.
And if you haven’t bought your bike yet, put a bit of research into what frame/wheel size you need before you do.
Cycling is a great way to get fit and works well with core stability, however, if any injuries do niggle don’t push through and do get them checked out!
Osteopath at Fleet Street Clinic
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC).
For more information on our osteopathy services, click here.
Book an appointment with him if you have any musculoskeletal injuries by calling on +44 20 7353 5678 , email info@fleetstreetclinic.com or book an appointment online.
With over 9 million employees put on the furlough scheme at the peak of the pandemic, and many still on the scheme 12 months later, it’s no wonder that there’s an increase in anxiety about returning back to the workplace.
With some employees seeming less than enthusiastic about returning to the workplace, it may be concerning for an employer about how they address this anxiety and what to do if faced with this situation.
From the many Occupational Health consultations we’ve had this past year, we’ve learnt first-hand and also through our clients about the transition back into the workplace for both employees and employers. We’ve been able to get a good picture of the main issues people have been facing and what the underlying cause for the anxiety can be.
As with any anxiety, the cause can be a singular concern or a combination of concerns and when investigating further, each person should be treated as an individual to fully understand their concerns.
A discussion with an empathetic leader is a great place to start. Sometimes, however, a review by an independent occupational health clinician from a SEQOHS-accredited clinic, like Fleet Street Clinic, is required to work out if the employee is fit to continue working, if any adaptations for working are suggested and some circumstances, what medical help is required.
Here are some of the main concerns and issues that have come up time and time again from both employee and employer and how these can be mitigated:
Lack of confidence:
Many furloughed returnees may come back wondering if they can still do their job as well as before, which can manifest into a lack of confidence. With not being at work for a long period of time, certain skill sets may have started to feel ‘rusty’. Worries and concerns about returning to full-time hours from the get go, and having to perform at the same level they were at before they went on furlough are just some examples.
What can help with this?
Early engagement between the employer and the returning employee is important to discuss any specific anxieties and to work out a ‘return plan’ which can really make a difference. ACAS advises employers to think about those returning from furlough as if they have been on maternity or long term sick leave. Using similar ‘check ins’ (as you would for maternity/ sick leave) prior to their return to work allows for real-time conversations to cover the practicalities, potentially a staggered return to build up confidence, as well as an opportunity to discuss any anxieties and concerns.
Concerns over workplace safety:
Two of the most common themes found in consultations with Fleet Street’s Occupational Health Department were employees worried about safety, and whether going back into the office ‘would be the same’.
What can help with this?
To help reduce such anxiety, employers have been encouraged to share with those returning their ‘Covid compliant workplace risk assessments’. HSE made these mandatory last year, although officially they do not have to publish their results internally unless there are over 50 employees. Sharing such information on an individual basis would allow the furloughed employee to see what changes and controls have been put in place, giving them reassurance and peace of mind. It also demonstrates to them that the employer is prioritising their health and safety.
Employers should also consider setting up a ‘virtual tour’ of the amended workplace, to enable those returning to see and understand what their new workplace will look like. Changes such as one-way pathways around the building, socially distanced workstations, extra cleaning of communal areas and bathrooms are just some of the more visual changes. Employers should also take the time to discuss changes in policies such as obligatory wearing of masks, flexible office/home working (if feasible) and other benefits that may have been introduced. Logistical concerns about childcare is one of the major blockers for those returning, and this is another example of how the employer can have open discussion with the returnee to formulate a reasonable solution, preferably weeks ahead of the return to work date.
Concerns over leaving the home:
Returning employees may have concerns about leaving the home and what impact this may have on their health. Other factors employers had to think about were those who were shielding (classified as extremely vulnerable by the Government) and for those living in a household with someone shielding.
What can help with this?
To mitigate this, employers may have chosen to use Occupational Health to contact the employees returning to identify any risk factors or health concerns. Although any medical information would be classified as strictly confidential, the employee and Occupational Health professional discuss the outcome of the assessment which is then simply fed back to HR as ‘fit to return into the office workplace with no adjustments, or with adjustments (then outlined). In the rare circumstance of an employee being assessed as not fit to return to work, a management referral would be indicated. Fleet Street Occupational Health did this for various businesses, and found that many of the employees contacted were appreciative of having been asked about their health in relation to Covid. In a small number of cases, simple and feasible adjustments were recommended – mostly around avoiding a busy commute (flexible working hours were recommended in this instance). Employers fed back confirming the transition for those returning were certainly smoothened by this process.
Mental Health:
Mental health may have been affected for all employees for many different reasons, these include bereavement, stress from being at home with home schooling, fear of uncertainty etc. It is important that employers recognise this decline in mental health and look to support their employers.
What can help with this?
Employers should consider making sure that all employees are aware of what counselling services are available, or to train up ‘mental health first aiders’ to carry out weekly group check ins or a ‘return to work’ support group. If the employer would like independent advice from an Occupational Health clinician about where the employee is fit to work, then you may want to consider a management referral. They are primarily designed to support the referring manager in their decision making when dealing with an employee’s health-related issue and to determine the employee’s ongoing fitness to work, this includes mental health concerns.
How can the employer support the return back to the office in general?
Employers might consider a ‘phased return to work’ plan, to allow the furloughed employee to steadily get back into work. Both the employer and the employee want the same thing – to be at their best at work, and so allowing a gradual step up in days and hours (again as if returning from long term sick leave as an example) would be one way of enabling this.
Another thing that might help smoothen the transition back for those returning is a ‘buddy’ system. This is where a returnee is matched up with an employee who has not been on furlough to have them work together for the first few weeks. Not only would this help the returnee to navigate any new changes in the workplace, but it can enable collaborative working and remove the ‘grass is greener’ syndrome from both sides. Some examples of known sentiments include furloughed employees wondering if they’ll have a job to go back to, what it will be like, and a vulnerability about losing their skills etc. Those who remained at work may feel that those on furlough had the ‘easier option’ or feel resentment at not having been given the same option to go on furlough. These are just two sentiments raised from employees during our conducted Occupational Health consultations.
Our list of examples and scenarios outlined are not exhaustive; and we understand that as people we all have specific needs which may be different to others.
We hope that you found the suggestions we have outlined useful, especially in ensuring a smooth transition for those returning, and ultimately an emphatic and supportive working environment for all.
If you require support from our Occupational Health department, you can find more information here.
Alternatively, fill out the form below and we’ll propose suitable services for your consideration.
Our new, in-Clinic PCR laboratory is now open: Introducing Fleet Street Laboratory.
Our historic Grade II listed premises have been adapted to accommodate one of the latest and most technically advanced robotic PCR systems anywhere, enabling us to carry out more tests simultaneously, accurately, and delivering the fastest results. Our lab upgrade means we will also continue to meet the highest quality and safety standards.
PCR technology is not new, but until recently hasn’t needed the space, complexity and resources of a full-scale clinical laboratory. Our upgrades mean samples can be processed in large batches rather than individually run.
In 2017, we embraced the challenge of bringing PCR closer to the consulting room: a pioneering colleague in the US had begun to use PCR at “point-of-care”, and I’d seen the benefits to patients first-hand. The Fleet Street Clinic became one of the first practices in the UK to apply this to respiratory infections, and also to gastrointestinal infections in returning travellers at our busy Travel Medicine practice. This enabled us to confirm a diagnosis and start treatment all at the same initial visit.
PCR stands for “polymerase chain reaction”.
It is a laboratory technique that exponentially amplifies the tiniest traces of any genetic material – DNA and RNA – that exactly matches the infection or disease under test. Instead of hunting with microscopes, or incubating cultures for days at a time, viruses, bacteria and parasites can be found quickly and reliably. They can be sought individually, or in “syndromic panels”: a respiratory panel, for example, can screen a sample for an array of 22 different organisms at the same time, each capable of causing respiratory symptoms, detectable from a nasal swab.
By the time SARS-CoV-2 reached the UK at the beginning of 2020, we were onto our second generation of PCR systems. We had just added two faster and more efficient machines, adding a panel of sexually transmitted infections to the repertoire (and capable of delivering a full sexual health screen in a couple of hours rather than the 2 to 3-day turnaround that our outside lab was offering). Both were quickly “upgraded” to be able to detect coronavirus infection – and when I contracted a mild version at the beginning of March 2020, my sample was our first in-house positive case. Within a couple of weeks, demand for consumables overwhelmed supplies, and we were left with equipment that was impossible to use.
One year on, we have dramatically expanded our capacity and capabilities. We have four sophisticated PCR systems, each with different strengths and capabilities, to which our newest system will now be added. We have been able to support some of the most challenging requirements: from clinical diagnosis (including support for the NHS) to facilitating international travel; and workplace screening for critical industries and complex projects – including major film production in the UK and abroad. Our focus has been on combining high quality service with the fastest possible turnaround. We have built expertise, developed our team, and are very excited about our new lab.
Come and see it next time you come to the Fleet Street Clinic!
Or if you need a PCR test, you can book online.
Flu jabs are a necessary part of Flu prevention… even after Covid-19
Flu vaccinations become available mid-September each year. They offer the best protection against the flu and are designed to be had prior to exposure to the flu virus. Like all vaccinations, immunity can take up to 2-weeks following vaccination to become effective so the earlier you get vaccinated the better.
Flu is still something we should be vaccinated again as it can be serious and lead to complications that can prove fatal. Vaccination offer protect for you, your family, your work colleagues and also those most vulnerable in your community.
The successful Covid-19 vaccination campaign has clearly demonstrated how vaccinations can protect the vulnerable and limit outbreaks. I hope everyone will learn from this and take full advantage of flu vaccination next time it is offered.
What is the next flu season expected to be like?
We don’t really know what to expect. There was very little circulating flu virus during the 2020/21 season, which means that there will be less immunity within the general population and more people will be susceptible. To make things worse, if there has been less flu around – globally – it becomes harder to predict exactly which flu strains will be coming our way, and so more difficult to pick the best strains to include in next winter’s vaccines. It is dangerous to assume flu has disappeared due to the pandemic and Covid restrictions that are currently in place.
Booking your flu jab:
Private vaccination is available from September until February the following year. Due to coronavirus, we operate a booking system so we can manage the flow of patients being vaccinated in a safe way.
Opening Hours: Monday – Friday: 9am-5pm
Address: Fleet Street Clinic, 29 Fleet Street, London, EC4Y 1AA
How much would you pay to prevent bowel cancer?
£1,000? £500? £200? £100? Or just £45?
Everyone knows a friend or relative who has suffered from or unfortunately, died of bowel cancer. Also known as colorectal cancer, bowel cancer is the fourth most common cancer in the UK but the second biggest killer. More than 16,000 people die from bowel cancer in the UK every year. Similar to other types of cancer, bowel cancer is treatable and curable especially if diagnosed early.
The earlier it is detected, the greater the chance of survival.
However, the survival rate drops significantly as the disease develops. The optimal test for bowel cancer is a colonoscopy, but it is an invasive test which checks the lining of the bowel for cancer. Due to the invasive nature of this test, it usually happens following a positive screening result or if a person has multiple symptoms so as not to cause unnecessary discomfort is symptoms are say. related to another health issue.
As bowel cancer symptoms are also indicators for a wide range of gastroenterological (digestive system) disorders, a simpler, non-invasive FIT stool test (faecal immunochemical test) can be the first step for patients with concerns and/or symptoms such as lower abdominal symptoms such as abdominal pain, rectal bleeding and/or a change in bowel habits prior to a colonoscopy.
For those who are healthy with no symptoms, FIT screening is an important way of testing healthy people to see if they show any early signs of cancer.
Bowel Cancer Screening
It can be challenging to differentiate between patients with serious bowel disease such as bowel cancer, from those with benign functional or diet-related conditions, such as IBS – irritable bowel syndrome, and minor colorectal diseases such as haemorrhoids.
A FIT test or faecal immunochemical test, looks for blood in the stool, an early sign of bowel cancer. It is a simple and effective non-invasive test.
If there is blood present, this can indicate the presence of abnormalities in the bowel, which over time may develop into cancer. Patients with a positive FIT result are then referred for further investigation by colonoscopy.
A FIT test does not diagnose bowel cancer, but it’s a simple way to find out if you need further tests. Introducing regular bowel cancer screening into your health checks will reduce the risk of dying from bowel cancer.
Are all FIT Tests the same?
The short answer, no.
The sensitivity of a FIT test to detect blood in stools can be adjusted to be more or less accurate. The lower the threshold, the more sensitive the test is to blood in the stools meaning the earlier abnormalities can be identified.
Where you live in the UK dictates the FIT tests available to you, see below:
NHS Scotland:
Age range: 50-74 years – Automatic invite for screenings every 2 years / 75+ done on request
Blood sensitivity threshold: 80ug per g of stool
NHS England & Wales:
Age range: 60-74 years – Automatic invite for screenings every 2 years / 75+ done on request
Blood sensitivity threshold: 120ug per g of stool
Fleet Street Clinic:
Age range: Screening recommended from 40 years onwards. Available from 20 years if symptoms are present and for individuals with a family history of bowel cancer of one or more first-degree relatives (sibling, parent or child).
Blood sensitivity threshold: 20ug per g of stool.
A big difference!
Why is this so important?
If early detection is a matter of life and death when it comes to bowel cancer then the optimum FIT test has to have the lowest sensitivity threshold to provide the most accurate diagnosis. The more sensitive the FIT screening, the more cancer and precancerous polyps can be detected, especially at an early stage of abnormality.
At Fleet Street Clinic, we are more likely to pick up blood in the stool by a factor of 4 compared to NHS Scotland and by a factor of 6 in comparison to NHS England & Wales, all without the rigid age limitations.
Bowel Cancer Screening at Fleet Street Clinic
The FIT test at Fleet Street Clinic has the lowest sensitivity threshold on the market right now. It is an easy, quick test which costs just ££70* with results within a week.
Surely it is worth it?
If by any chance your test is positive, we provide a letter of referral which can be given to your GP (Private or NHS) or used at one of the referral centres we recommend for private colonoscopy. The choice is yours.
Tell your friends about this life-saving test and save a life – It could be your own.
If you’re concerned about bowel cancer, then it’s important to book a 15-minute GP appointment to speak to a doctor – you can book online.
* A 15-minute GP appointment costing £98 is required in addition to the cost of the FIT test.
Following the confirmation of the new variant of coronavirus found in the UK, we have taken many enquiries regarding our PCR testing technology at Fleet Street Clinic and its ability to detect this new variant.
Please feel assured that our suite of Covid-19 rt-PCR detection equipment can confirm the presence of this new variant alongside the previously known strain.
We understand identifying this new variant of SARS-CoV-2 may cause concern due to its higher rate of infection compared to the previous known strain. However, rest assured, there is no evidence to suggest it causes more serious illness or would disrupt the effectiveness of the Covid-19 vaccine.
Prof Calum Semple, a member of the Scientific Advisory Group for Emergencies (Sage) which advises the UK government, said the new strain is likely to become the dominant global strain and it is therefore important our equipment is able to adapt to change to identify mutations to the SARS-CoV-2 virus.
At Fleet Street Clinic, we have developed a comprehensive portfolio of COVID-19 diagnostic testing solutions including multiplex rt-PCR detection and antibody testing and are able to provide rapid test results for diagnosis and travel purposes. This positioning hasn’t changed since this new strain has emerged. We pride ourselves on constantly adapting to meet the challenges of the Covid-19 pandemic and will continue to do so should any further genetic variations be identified on the SARS-CoV-2 genome.
For more information about our Covid-19 testing options, click here.
Covid-19 Statistics:
UK: Public Health England
Worldwide: The Johns Hopkins Center
Coronavirus Testing:
Covid-19 testing is available at Fleet Street Clinic, including PCR testing for active infection, antibody testing for confirmation of past infection and PCR testing for travel purposes including travel certificate.
Samples can be collected in-clinic, during a home from the nurse or using a self-sample home testing kit.
For more information:
Alternatively, please call our reception team on +44 20 7353 5678 to see which option is most appropriate for your current circumstance.
Virtual GP Appointments:
If you have symptoms of coronavirus (a high temperature or a new, continuous cough), please do not leave your home. That includes coming into the clinic, any other GP surgery, a pharmacy or a hospital.
We’d suggest you can book a virtual GP appointment with one of our doctors. You can discuss your health concerns and symptoms by telephone or video call.
Alternatively, you can use the NHS 111 online coronavirus service. If you are experiencing life-threatening symptoms, always call 999 for an ambulance.
If you have symptoms you should self-isolate for 7 days. If you live with someone who has symptoms, you’ll need to self-isolate for 14 days from the day their symptoms started. This is because it can take 14 days for symptoms to appear. More details about self-isolation can be found here.
For further information about coronavirus (COVID-19) or read answers to common questions about it.
How to stop the spread of Coronavirus:
- Wash your hands with soap and water often – do this for at least 20 seconds
- Use hand sanitiser gel if soap and water are not available
- Wash your hands as soon as you get back home
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when you cough or sneeze
- Put used tissues in the bin immediately and wash your hands afterwards
- Do not touch your eyes, nose or mouth if your hands are not clean
Recommended information sources:
Gov.uk: For the latest guidance about coronavirus (COVID-19) for health professionals, businesses, schools and other organisations.
Public Health England: For the latest information about the situation in the UK, along with guidance for what to do if you think you’re at risk. You can sign up for email alerts from PHE concerning coronavirus updates here.
NaTHNaC: For travel health advice for travellers to countries/areas affected by COVID-19
World Health Organization (WHO)
__________________________
Our Medical Director and Travel Specialist Dr Richard Dawood, has been at the forefront of the conversation, sharing insight and opinions as the pandemic unfolds:
2021:
The Telegraph: Vaccine passports for travellers ‘unavoidable’
The Guardian: Vaccine passports ‘essential’ for resumption of international travel
The Sun: Covid vaccine questions answered – from when you can hug again to delaying 2nd dose
2020:
Times letters: Strategy for combating the coronavirus
The Telegraph: Staycations to face masks – 5 ways coronavirus could change the way we travel
The Telegraph: Why flying can make you ill – and how to stay healthy on board a plane
CNN Travel: Travel and the coronavirus pandemic: Everything you need to know
CNN Health: 7 of your latest coronavirus questions, answered
Express: Coronavirus: When will it end? Experts reveal if virus could die off in warmer weather
Express: Coronavirus protection: Best way to prevent the deadly virus spreading through the eyes
2019:
Mirror: Everything you need to know about flu jabs and why you should get one before Christmas
Please note: All information stated is correct at time of posting.
We are hoping you and your family are keeping safe and healthy.
We want to reassure you that we are committed to looking after your health during these trying times.
We have every intention of remaining open so you can access all of our services, however, we have had to make some necessary changes to adapt to the current circumstance.
Temporary Opening Hours:
We have made the difficult decision to temporarily adjust our opening hours. Starting Monday 23rd March, for the foreseeable future, the clinic will be open 9:00am – 5:30pm for face-to-face appointments – we may be able to facilitate virtual clinic appointments outside of these hours.
Virtual Clinic Offerings:
With many of you now working from home outside of London, it makes sense to adapt our services to meet your new needs.
You’ll be able to access a lot of our services through our virtual clinic from Monday 23rd March:
- GP appointments
- Travel consultation for health advice only
- Repeat prescriptions
We are confident that this will not affect the quality of service that we will continue to supply to you.
Reduced Services:
We are running a reduce service for optical appointments. We advise you call our front of house team on +44 20 7353 5678 to make any appointments or alterations.
Booking An Appointment:
To protect the health and wellness of our patients and our team, we’ve decided to turn off online bookings for the time being. Rest assured you can still book appointments, however, this now needs to be done through our friendly reception team on +44 20 7353 5678 to determine if a face-to-face appointment or virtual consultation is required. Due to reduced availability, a deposit is required for all appointments.
Getting in touch:
Due to these unprecedented circumstances, we’re experiencing an increase in phone calls so you may have noticed our call waiting times have been slightly longer than usual. Our reception team are working at full capacity to offer reassurance and to book your appointments, however, please do not hesitate to email us if the phone line is too busy. We will answer all enquiries we receive.
Prescriptions for Medicines & Contact Lenses:
Please note, you can place orders for repeat prescriptions and contact lenses in advance via email here.
Outline your medicine needs and/ or your contact lens prescription and you can either pick your prescription up from the clinic or we can dispense these directly to you via the post.
Feeling unwell?
We would kindly like to remind you that you must not come to the clinic if you are suffering from any of the symptoms below:
- Coughing
- Sneezing
- Running nose
- Sore throat
- High temperature
- Shortness of breath
We are not offering testing for COVID-19 at our clinic but will be sure to keep you informed if this is to change.
Our commitment to our patient’s health and well-being remains our primary focus and we will continue to work safely and strategically during these unprecedented times. If there are any developments that impact these arrangements, we will notify you at the earliest possible opportunity.
Thank you for your support in keeping one another safe.
On Friday 14th December 2019, The Fleet Street Clinic, along with thousands of people up and down the UK will embrace their craziest & tackiest Christmas jumpers in celebration of Christmas Jumper Day, to raise money for Save the Children.
Save the children, are a fantastic charity who help some of the world’s most vulnerable people, which is why we choose to support them every year.
Save The Children began Christmas Jumper Day with the aim of “making the world better with a sweater”. While it’s an undoubtedly fun and light-hearted occasion, the main focus of the day is to highlight the lifesaving work the charity does. They help bring essential food, healthcare & education to many children who are, for many reasons, currently missing out.
Save the Children aims to create a world where every child survives, learns and is protected. Child poverty, hunger, education and health are just a few of the charities key aims which help children who live in some of the toughest places in the world.
As a healthcare provider, ensuring all children throughout the world have access to health care is extremely important to us. There is a danger that children are being left behind because they are poor, because they are girls or because of their ethnicity.
Last year, Save the Children helped 10.6 million children through their health and nutrition work. This year they plan to help many, many more!
___________________
How can you get involved?
The simplest way of getting involved with Christmas Jumper Day is to join in!
Wear your most eye-catching Christmas jumper and donate some money towards Save the Children.
Make a difference this Christmas!
The Philippines is a fascinating archipelago, made up of thousands of islands where you can explore stunning beaches and enjoy superb surfing and diving.
Ensure you follow our top travel tips to stay healthy.
7,641 islands, of these islands, only 2,000 are inhabited.
The Philippine archipelago is divided into three island groups: Luzon, Visayas, and Mindanao.
Vaccinations
If you are heading to the Philippines you should ensure that you are up to date with your routine immunisations. There have been outbreaks of measles and polio this year in the country so all travellers should ensure they have received 2 doses of the MMR vaccination and a full course of diphtheria, tetanus and polio (DTP) vaccinations.
In addition, it is advised that vaccinations against hepatitis and typhoid are given. Other vaccinations that can be considered are hepatitis b, rabies and Japanese encephalitis. Find out more about our wellness and travel vaccinations.
Rabies
Rabies is an especially high risk in the Philippines. It is a virus found in the saliva and bodily fluids of mammals. It is transmitted to humans by the bite, scratch or lick to open skin. Once the virus enters the body and the nervous system, it is fatal. There is a large number of stray animals in the Philippines so extra care should be taken to avoid contact with animals. Pre-travel rabies vaccinations are strongly recommended for travellers to the Philippines. There have been reports of falsified rabies vaccinations and immunoglobulin circulating in the country meaning anyone exposed to the virus seeking medical treatment in-country may not receive the proper treatment.
Malaria
The majority of the Philippines is low to no risk of malaria. Palawan, Tawi Tawi, Zambales and Zamboanga del Norte present a higher risk of malaria. Most travellers will not require anti-malarial medication providing they are careful not to get bitten by mosquitoes. The malaria mosquitoes are most active during the evening, so if you plan to visit a high-risk area, ensure you are cautious between the hours of dusk and dawn and aim to sleep under a mosquito net to prevent bites whilst you sleep.
Insects
The Philippines has a risk of several non-vaccine preventable viruses that can be spread by mosquitoes. Dengue fever, chikungunya and zika virus are the main culprits. These viruses are spread by mosquitoes that predominantly bite in the day. As there is no vaccination nor medication that will prevent this illness, strict precautions must be taken to prevent their bites. Wear long loose clothing and cover up as much as possible, particularly between dawn and dusk. Wear a good insect repellent with a minimum of 50% DEET in it, and treat clothes with the insecticide permethrin for added protection.
The Philippines Department of Health (DoH) declared a national dengue epidemic on 6 August 2019. Continue to follow NaTHNaC advice and take precautions to avoid being bitten by mosquitoes
See our ultimate bug kit.
Water sports
The Philippines is made up of over 7000 islands and the main way of reaching them is by boat. If you are prone to travel sickness you may want to ensure you pack some medication to prevent this so not to interrupt your experience. There is an abundance of pristine coral reefs throughout the archipelago making the country perfect for water sports. Whether you are snorkelling, surfing or scuba diving, if you plan to take the plunge you need to be careful to avoid coral cuts and abrasions. Extra care needs to be taken with coral cuts to prevent them from becoming infected. Packing a small first aid kit with tweezers, waterproof dressings and antiseptic is a sensible idea.
The availability of medical care varies across the Philippines, and may not meet the standards of care in the UK. Although adequate in major cities, medical care is limited in more remote areas.
Book your travel appointment today
By Anna Chapman | Travel Nurse | November 2019
Myanmar is becoming an increasingly popular destination to visit in South-East Asia.
The golden pagodas of Yangon and the stupors of Bagan are top on most travellers itineraries, alongside a trip down the Irrawaddy river to Inle Lake.
The more adventurous may head to the islands on the Myiek archipelago or hike the hill station of Kalaw. Whatever the itinerary, it is essential to ensure you have sought pre-travel advice to ensure you stay healthy whilst abroad.
Vaccines
Travellers should ensure they are up-to-date with their routine immunisations. All travellers should ensure that they have received a vaccination against diphtheria, tetanus and polio (DTP) in the last 10 years. Other vaccinations that all travellers should ensure they are up-to-date with are Hepatitis A and Typhoid. Some travellers may wish to consider vaccination against hepatitis b, rabies, cholera and Japanese encephalitis. It is best to book a travel consultation with a travel nurse to discuss your route and your plans to ensure you are protected for all circumstances.
For more information on our vaccines, please visit our travel and wellness vaccination pages.
Malaria
The cities of Yangon and Mandalay have no risk of malaria. The majority of areas that travellers visit such as Bago, Inle Lake, Kyaikto Padoga and Bagan have a low risk of malaria and anti-malarial medication is not usually advised. The states of Chin, Kachin, Kayah, Rakhine and Sagaing have a high risk of malaria. Travellers visiting these areas are advised to take anti-malarial for this part of their trip. The malaria mosquitoes are most active during the evening. So, if you plan to visit a high-risk area, ensure you are cautious between the hours of dusk and dawn. Aim to sleep under a mosquito net to prevent bites whilst you sleep.
Insects
Myanmar has a risk of several non-vaccine preventable viruses that can be spread by mosquitoes. Dengue fever, chikungunya and Zika virus are the main culprits. These viruses are spread by mosquitoes that predominantly bite in the day. As there is no vaccination or medication that will prevent these illnesses, strict precautions must be taken to prevent being bitten. Wear long loose clothing and cover up as much as possible. Particularly between dawn and dusk. Wear a good insect relevant with a minimum of 50% DEET in it. Treat clothes with the insecticide permethrin for added protection. For short adventures, this can be done before your trip.
See our Ultimate Bug Kit.
Fancy a dip in Lake Inle?
Think again. Temperatures in Myanmar can reach 40 degrees and a quick dip in the lake may sound like a good way to cool off. However, there have been recent outbreaks of schistosomiasis infection in Myanmar. Schistosomiasis is a parasitic blood fluke. The fluke lives in freshwater snails and enters through the skin when an unsuspecting person takes a dip. The fluke causes infection of the liver, bladder and bowels and can lead to long term damage. The best way to avoid this is to avoid swimming or bathing in freshwater. The detection of schistosomiasis can take up to 8-weeks. You should visit a GP for a health assessment 2 months after your suspected exposure date, even if you haven’t yet returned to the UK.
First Aid
Some areas of Myanmar are remote. The further in-country you travel, the harder it will be to access medication and first aid supplies. In some areas, access will be non-existent. Packing a good basic first aid kit is essential to help treat minor injuries and illnesses. Include items such as dressings, plasters and antiseptic cream. They can help with minor cuts, scrapes and blisters. It is useful to pack items that can alleviate pain and treat upset stomachs, as these are common traveller’s health problems. Another medical kit you may want to consider is a worldwide gastro kit. Other items you may want to consider are anti-histamines for any mild allergic reactions.
If you take prescription medication to ensure you pack sufficient for your trip and carry a record of the medication with you.
Book your travel appointment today
By Anna Chapman | Travel Nurse | November 2019
How to Stay Healthy This Winter
When the temperature drops outside, it’s tempting to reach for comforting, high-calorie food and avoid exercise. Feeling cold, along with short days and weight gain can lead to the onset of Seasonal Affective Disorder or depression in the winter months.
Fleet Street Clinic’s Consultant Dietitian, Ruth Kander BSc (Hons) gives some practical advice on what you can do to avoid the winter blues.
Consume a Variety of Foods
By eating foods from all the food groups, you will have all the nutrients you need to stay healthy and keep winter germs at bay whilst maintaining your energy levels.
Eat Plenty of Fruits and Vegetables
These will give you vitamins and minerals to help your body fight winter bugs. Vitamin C is especially beneficial in the fight against colds and sore throats. Avoid taking supplements which contain high concentrations of vitamins which can lead to medical problems. Fruit and vegetables high in vitamin C include kiwi, citrus fruits, spinach, pumpkin and sweet potato. Zinc is also a good mineral to help fight winter infections and boost the immune system. Foods containing zinc include fish, oysters, poultry, eggs, milk, unprocessed grains and cereals. If you’re short on time, using a blender to create a vegetable and fruit drink is a great way to pack your diet full of vitamins. Try combining lettuce, cucumber, spinach, ginger, berries and a dash of orange juice and water for a zingy, low-sugar start to the day.
Keep the Pantry Cupboard Well Stocked
Good foods to store include:
- Tinned beans and lentils
- Tinned tomatoes
- Whole-wheat pasta
- Brown rice
- Couscous and noodles
- Wholegrain cereals – for example, Porridge and Weetabix
Plan Your Meals
Make soups and casseroles in advance and freeze. That way you can come home to a nutritious meal in the evenings. Simply take out of the freezer in the morning so that they are ready to heat up after work.
Watch Portion Sizes
To avoid eating too many carbohydrates, try eating your meals at the table with the TV turned off, use smaller plates and reserve half your dinner plate for vegetables. If you want more after your first serving, have some soup or more hot vegetables.
Stay Active
It’s tempting to reduce your exercise regime in the colder months. But small efforts can go a long way to help stave off winter weight gain. Going for a regular, brisk walk or using an exercise video at home can be enough to maintain your weight and stay healthy over the winter.
Drink Plenty of Fluids
Try to avoid getting dehydrated. This can make you feel overly tired and unnecessarily run down. Drink plenty of fluids throughout the day that are either low calorie or calorie-free – aim for 2 litres a day. Be aware that your daily hot drink from the coffee shop can contain 360 calories or more!
Looking for an alternative to still water? Try green tea, regular tea, herbal teas, regular coffee, hot no added sugar cordial or lemon water.
Consult Fleet Street Clinic
Ruth Kander holds a virtual clinic every Friday from 9am-2pm for individual dietitian consultations and ongoing weight management courses. Please call our reception team on +44 20 7353 5678 if you would like to request a face-to-face appointment
WINTER FEET – LOOKING AFTER YOUR FEET IN COLD WEATHER
ADVICE FROM OUR PODIATRIST, George Hill
Staying warm when it’s cold outside can be a challenge. Especially when it affects our body’s circulation; our feet and hands can suffer especially. In cold weather, it is a natural response to prioritise the heating of our vital organs. This is so they remain at their optimal temperature for full functionality. This means having cold feet is normal when the temperature drops. Nail growth slows down and skin will often become drier because nutrition to these tissues is affected.
In response to this temperature change, small blood vessels temporarily constrict. As a result, you may see a change in the colour of your skin, which could look pale, blanched and waxy at first, before becoming bluish. This is because the oxygen in the blood has been used up by the tissues. The skin is also cool to touch. Returning to warm conditions usually remedies this and the skin becomes pink and warm again.
However, in some individuals, this response is exaggerated and prolonged. This condition is known as Raynaud’s phenomenon and can be inherited. The same response will occur but much more readily and will last longer. Meaning the colour changes are much more obvious. When the skin is deprived of oxygen for long periods of time, some injury occurs to the soft tissues. This can make fingers and toes numb while they remain cold. When the blood vessels do finally relax and blood returns to the area, fingers and toes can throb and burn, turning bright red with inflammation. Eventually, things return to normal but repeated episodes of this can lead to dry, devitalised skin and changes in nail shape and texture.
Chilblains occur for much the same reason. These are painful, itchy swellings that often occur on the tops of small toe joints but can occur in other bony areas too, such as the back of the heel. Tightly fitting footwear can add to the misery by constricting blood flow further and rubbing on the painful skin. Chilblains are not caused by using hot water bottles, as commonly thought, they are a cold injury to Winter Feet, The attempt to relieve the intense itch by scratching merely worsens the problem, often causing further damage. Itching tends to break the skin and causes sores which can sometimes lead to infections.
Preventative action should reduce the likelihood of chilblains developing, but if they do, an antipruritic (anti-itching) cream or ointment can be obtained from pharmacies, and menthol-based products can also be very soothing.
If the skin becomes broken, antiseptic creams such as Savlon help the skin to heal and prevent infection. Cover with a gauze pad after applying, which can be secured with finger bandage or held in place with a cotton sock.
In the aftermath of chilblains, the affected skin is often dry, thin and rough, so use a moisturising cream to restore normal texture.
Cold feet at night can keep you awake or disrupt sleep.
What can be done to help? If you are susceptible to cold extremities, it is important to keep yourself generally warm. Listen to the temperature forecasts and dress accordingly. As well as suitable outer clothing, trousers, tights or socks will help to keep the whole limb warm. Fibres such as wool or bamboo are good insulators and several light layers, rather than one thick layer, traps more air and heat. Remember to wear roomier footwear to allow for thicker socks without compressing the skin.
Footwear should have a good rubber or composite material sole, to insulate against cold pavements – adding insoles of cork or lambswool can improve insulation and comfort. The sole should have good grip for traction on slippery pavements.
Keep active – this improves circulation, and have plenty of hot drinks and food throughout the day.
At home, a warm (not hot) foot-bath will help. Dry with a rough towel and apply a cream or lotion with a massaging action. Some preparations include ingredients such as capsaicin or ginger, to stimulate circulation. Afterwards, put on loosely-fitting, warm socks or slippers to maintain the effect. If the feet are warm before going to bed, they are likely to stay warm. Bed socks in wool or cashmere can be very helpful. Water bottles or gel pads should not be over-heated, as sensation can be unreliable in cold feet.
People who suffer from eczema will find that cold weather tends to make the skin even drier and more cracked. Use plenty of ointment to keep the skin well hydrated and wear hose to help trap moisture and warmth. Silk is a good choice of material and is thin enough to wear under a thicker, outer sock.
In severe cold weather, you may find you get recurrent problems in your feet. Consult your GP who may advise a prescription drug to relax the constricted vessels and thus improve blood flow to the extremities.
Book Your Winter Feet Podiatry Appointment
For more information about podiatry at Fleet Street Clinic
Botswana is one of the greatest safari destinations.
The Okavango Delta offers exceptional opportunities to view wild creatures and birdlife. Elephants roam freely and herds of buffalo crowd around the winding waterways the river. The stark and desolate landscape of the Kalahari desert can be found in the south with the longest unbroken stretch of sand there is. Whatever your itinerary, ensure you follow our top travel tips.
Vaccines
All travellers should ensure they are up-to-date with their routine vaccinations including measles, hepatitis A, typhoid, diphtheria-tetanus and polio (DTP). You may want to consider getting vaccinations for rabies and hepatitis B as well. Both these diseases are classed as high-risk in Botswana. We would advise you to speak with a travel nurse ideally 4-6 weeks before travel. At this appointment, you can discuss where you’re going and what you plan to do. They can then advise you of all the recommended vaccinations you should consider.
Find out more information about our travel and wellness vaccinations.
Malaria
There is a high risk of malaria throughout the year in the northern areas of Botswana including the Okavango Delta, Chobe and Moremi. There is a low risk of malaria in the rest of the country including the central Kalahari, Gaborone and Gemsbok. Individuals travelling to hight risk regions are advised to take anti-malarial medications to prevent the disease. As well as taking precautions against mosquito bites. The mosquitoes that spread malaria predominantly bite at night. For that reason, it is essential you sleep under a mosquito net.
Insect prevention
All travellers need to take extra precautions against insect bites. Mosquitoes, ticks, mites and lice are able to spread diseases such as African tick bite fever, dengue fever, filariasis and myiasis. Travellers should wear good insect repellent with at least 50% DEET and try to cover up with long loose clothes. You can add extra protection to your clothes by treating them with an insecticide. We would recommend using a permethrin spray.
See our Ultimate Bug Kit.
What about Yellow Fever?
The is no risk of Yellow Fever in Botswana. It is therefore not recommended that travellers get vaccinated. Travellers may require a valid Yellow Fever Certificate if they are entering Botswana from a country that has yellow fever, or who have transited through a country with a risk of yellow fever.
First Aid Supplies
Areas of Botswana can be remote, and access to medication and first aid supplies can be limited. Packing a good basic first aid kit is a good idea to help treat minor injuries and illnesses. Basic items such as anti-histamines, pain relief and medicines to treat upset stomachs are useful. Likewise, pack small dressings, plasters and antiseptic cream to treat minor scrapes and scratches. If you take prescription medication to ensure you pack sufficient for your trip and carry a record of the medication with you.
Book your travel appointment today
By Anna Chapman | Travel Nurse | October 2019
Exercise More – Get Outdoors
Today is National Fitness Day. September is a great time to redress the balance after summer holidays and make a new exercise plan. Time to get out and get moving!
Regular exercise has many benefits – a healthier heart, increased well-being, and a better quality of life. Research shows that if you exercise with friends, you are more likely to continue to keep fit, as the social environment encourages positive associations with the activity.
Exercising outdoors can contribute to this feeling of wellbeing. Organised outdoor exercise groups have grown in popularity recently, with a wide range of community-based activities across the country. A few of the more popular outdoor exercise activities are detailed here:
Park Run – Over 1 million Britons have taken part in Park Run – the Saturday morning 5k run in local parks across the country.
Project Awesome – A free community exercise group based in London, Bristol and Edinburgh, Project Awesome is based on high-energy, early morning exercise classes designed to kick-start your day.
Good Gym – For those who’d like to combine voluntary work with exercise, Good Gym enables you to meet like-minded people to run and work together on community projects in your local area.
British Military Fitness – Operating in parks across the UK, British military fitness classes are run by serving or former members of the armed forces with recognised fitness training qualifications. Classes are graded by ability group and are for members of the public. They are designed for all abilities, from those just starting to exercise who want to lose weight, to the already very fit.
Open Air Swimming – If you’re a keen swimmer, have you ever tried swimming outdoors? There are many reported benefits to open-air swimming, which can be enjoyed all year round even in the UK, with or without wetsuits. Check Wild Swim for your nearest open-air swimming site.
Getting Fit with Fleet Street Clinic
Our podiatrists can offer advice on appropriate footwear for exercise and our dietician and osteopath can work with you to support your exercise regime, ensuring a holistic approach to achieving a long-term, healthier you.
Albania, located in Southeastern Europe, is a tourist haven this time of year.
Albania has much to offer, from stunning mountain scenes to crumbling castles to picture-perfect beaches all with easy-going charm and a friendly atmosphere. Right now the tales of its beauty haven’t quite reached the masses, but we have a feeling this is likely to change in the not too distant future.
If you plan on staying in Albania‘s capital, Tirana, be sure to see the rotating restaurant/ bars for spectacular city views. Or take to the countryside and seashores to take in the ubiquitous sight of the abandoned concrete bunkers of Albania. Fearing invasion during the Cold War, Albania’s leader Enver Hoxha forced his country to build tens of thousands of bunkers throughout the country. These days you’ll see most in a state of slow decay but some have been given a new lease of life as a hotel, home or museum.
Visit Berat, to see the ‘town of a thousand windows’. This fascinating city dates back to the Ottoman Empire. The most striking feature of Ottoman architecture is the collection of whitewashed houses and towering minarets which adorn the hill to its castle. It is easily a highlight of visiting Albania. If, however, you prefer the great outdoors scale the peaks and troughs of the Accursed Mountains and take in the captivating castles of Gjirokastra.
Whatever your plan to do, be sure to follow our top travel tips to stay healthy in Albania.
Routine Vaccinations
All travellers to Albania are advised to be in-date with their routine immunisations. These include diphtheria-tetanus and polio and measles, mumps and rubella. Europe has seen huge outbreaks of measles in recent years. Therefore, all travellers should make sure they have received at least two doses of the vaccination, MMR.
If you’re unsure of your immunity, you can have a simple blood test to find out. Some travellers may wish to consider vaccinations for Hepatitis A and Hepatitis B, Rabies, and Tick-Borne Encephalitis. It is best to book a pre-travel consultation with a travel nurse to discuss your holiday plans. Together you can discuss what vaccines you’ll need.
Trekking and Ticks
The dramatic peaks of the Accursed Mountains spread their spoil between Kosovo, Albania and Montenegro. Those who plan to take advantage of the great outdoors should strongly consider vaccination against tick-borne encephalitis (TBE). TBE is a bacterial infection spread via tick bites or the consumption of unpasteurised dairy produce (between spring to autumn). Contracting the illness causes a fever with neurological complications.
TBE is vaccine-preventable and consists of 2 doses of the vaccination being given at least 2 weeks apart. A third dose is given 5-12 months later to give longer-term protection. Travellers should also avoid ticks by wearing long trousers and socks, and using DEET insect repellant. If you spot a tick on you, it needs to be removed promptly with some flat tweezers or a tick remover and cleaned with alcohol to reduce the risk of infection.
Rabies
Rabies is a fatal virus found in the saliva of infected mammals. Travellers can be exposed to it through a bite, scratch or a lick to an open area of skin. Therefore, you should avoid contact with animals, especially wild and stray animals. The vaccination against rabies means that treatment can be given easily and in the country should a risk of rabies occur.
You will require a series of 3 vaccinations to be given over a 3 week period. Or over 1 week if a rapid course is needed. Travellers at greater risk are those who plan to do outdoor activities such as hiking, trekking, cycling or caving.
For more information on our vaccines, please visit our, travel and wellness vaccination pages.
First Aid Kit
For those trekking in the hills, packing good basic first aid kit is essential. The availability of health care and first aid supplies are very limited in rural areas, particularly outside Tirana. Therefore, you should make sure you bring your own adequate basic provisions. These include pain relief, plasters and medication to treat an upset stomach, such as loperamide and oral rehydration salts. Cuts, scapes blisters and even a twisted ankle can occur, so take blister pads, some waterproof dressings and a bandage to deal with any minor injuries whilst you are there.
Access to safe water may be limited. You should consider packing chlorine dioxide tablets to purify your own water. Alternatively, you can purchase a water-to-go bottle which has a built-in filter. If you take regular prescription medication, be sure you pack enough to last your entire journey. And, remember to carry the prescription with you just in case.
Book your travel appointment today
By Anna Chapman | Travel Nurse | September 2019
It’s now coming to the end of summer and many of us have spent plenty of time around pools and on the beach. Which can be wonderful, of course. However, bacteria and viruses can thrive in these locations causing foot infections.
George, our podiatrist talks about one in particular: the pesky verruca.
Verrucae are commonly found on the foot and are relatively harmless. However, there is the possibility they have other more sinister properties. Some can become malignant and/ or grow and spread across the foot causing a host of uncomfortable or potentially dangerous problems.
Verruca or Verrucae are caused by the Human Papilloma Virus (HPV). There are hundreds of different types of HPV and different strains infect the body differently. Some types infect the skin, causing verrucae. Even if you come into contact with the virus that causes warts, the risk of becoming infected and developing a wart is small.
Common warts and plantar warts are not usually a serious health concern. These viral warts have not been shown to play an aetiological role in wider known high-risk HPV-linked diseases* such as cervical cancer and Bower’s disease. This is due to HPV presenting as different strains. Having one does not mean you have the other.
*For additional information on HPV’s link to cervical cancer and HPV’s link to Bowen’s disease, we recommend Macmillan’s website.
Contrary to what the old wives tale would have you believe, warts are not caught from touching a toad. Viral plantar warts are in-fact contracted via skin to skin contact or surface to skin contact; among other suggested routes. While common warts are usually painless, plantar warts can be painful because they press inward when you stand on your feet.
In appearance, these lesions are lumps that are generally circular in shape and appear slightly raised and can be callused over with thicker skin. Some will present with small black/deep-red specks, often noted as the capillary heads and others can be clustered into groups. If you have any small areas of skin you are concerned about then it is important to have these reviewed by your Podiatrist immediately.

For many, a verruca will disappear in a few weeks to months. However, if they do not it is likely you will require treatment to remove them before they grow or spread. Although one small verruca can be pain-free but unsightly, a large cluster can be quite painful to walk on. Adjusting your walk to relieve the pain can lead to further foot complications. So, it is best to take action as soon as possible.
Over the counter treatment options may work for some people. However, stubborn, persistent verruca will require more appropriate specialist treatment and observation. A medical professional should review all lesions. This is very important so to rule out more serious health concerns.
Specialised treatment is often provided with minimal pain with great results. High strength acid paste or cryotherapy using true liquid nitrogen can be the most appropriate methods for nearly all strains of verrucae. Your podiatrist will advise you on the best course of action based on the verruca presentation, your lifestyle and detailed medical history.
We advised you do not begin treatment without consulting a medical practitioner first. Your Podiatrist should be the first port of call when dealing with these pesky verrucae.
For more information about our podiatry service, our foot health check-up, cryotherapy and medical pedicures.
By George Hill | Podiatrist | September 2019
Yellow Fever Update:
Recent news reports have raised concerns about yellow fever vaccine safety. It is important to understand the risks and benefits.
For decades, the yellow fever vaccine was considered to be extremely safe. More recently, however, we have become aware of a low rate of serious adverse effects occurring when older travellers are vaccinated for the first time. The two main types of adverse effects are called YEL-AVD and YEL-AND – the first involves damage to organs such as the liver, and the second damages the nervous system. Yellow fever vaccines contain live viruses that do not harm people with a normally functioning immune system but do seem to cause harm in a tiny proportion of people with an ageing immune system, as well as those with reduced immunity from other causes.
In one of the largest medical studies of yellow fever vaccine safety, the rate of YEL-AND in people aged 60-69 was 2.5 per 100,000 people vaccinated, and in over 70s was 1.6 per 100,000. For YEL-AND, the rates were zero and 4.0 per 100,000 respectively.
According to the US Centers for Disease Control, in the absence of a yellow fever outbreak, the “background” risk of yellow fever occurring in unvaccinated travellers on a 2-week trip to a zone where yellow fever is present is calculated to be:
- West Africa: 50 cases per 100,000, with 10 deaths per 100,000
- South America: 5 cases per 100,000, with 1 death per 100,000
Yellow fever vaccinating centres normally explain these risks to everyone they vaccinate, and in particular to travellers aged over 60. Vaccination for personal protection is recommended where benefit outweighs the risks, and a medical waiver is given when it is not safe for the vaccine to be used. Age alone is not a reason for issuing a waiver.
Other factors that complicate the picture include the following:
- There are active outbreaks of yellow fever in several parts of the world, notably at present in Brazil as well as in several African countries, so the risk to travellers is often much higher than that quoted above.
- Vaccination is the only way to prevent and control yellow fever and is often the only possible public health measure for entire populations.
- Many countries therefore rigorously enforce vaccine requirements as a condition of entry.
- Yellow fever vaccine shortages are common – there is currently a serious shortage in the USA, and the vaccine is not always available when needed.
- Awareness of vaccine risks has come with a stricter approach to recommending vaccine only when travellers are definitely going to be at risk; however, an unintended consequence of this has been to delay the opportunity to vaccinate travellers for the first time until they are older and at greater risk of adverse effects.
The World Health Organization now considers vaccine protection to be life-long, though border officials in several countries do not always recognise this. A small number of recent cases of yellow fever in Brazil among people who had been vaccinated previously has raised further doubt about this policy, and Brazil currently recommends revaccination every 10 years. Revaccination has not been linked to adverse effects.
There is currently extensive UK press coverage (that has also been picked up in the US) of YF vaccine adverse effects – one death occurred shortly after vaccination in a distinguished cancer researcher, and a psychotic reaction in a former BBC journalist vaccinated in Greece. Both cases were attributed to the vaccine because of the timing. Further clinical details are not available, so we can’t yet be certain of a direct link, but this news will undoubtedly have a considerable impact on public perception of the vaccine.
Written by: Richard Dawood, Medical Director and specialist in travel medicine
Book your yellow fever vaccination today.
Links:
- Cancer pioneer Martin Gore’s sudden death from routine jab – Source: The Times
- I had a yellow fever jab, then the voices told me: ‘Kill! Kill! Kill!” – Source: The Times
Bosnia is where East meets West.
It is a country on the Balkan Peninsula in southeastern Europe and has become somewhat a destination for adventurous travellers.
Beautiful Ottoman architecture, rugged mountains, captivating castles, raft-able rivers, and humble hiking trails are all reasons why travellers are choosing Bosnia as their next travel destination. The unveiling of the Via Dinarica mega hiking trail means the number of tourists to the Balkan country of Bosnia Hercegovina is expected to rise steeply. The 1930km trail provides a corridor linking traditional cultures between the former Yugoslavian nations. So whether you plan to mill about the city of Mostar, stroll the streets of Sarajevo, or take a hike in the hillside, ensure you follow our top travel tips to stay healthy.
Vaccinations
All travellers are advised to be in date with their routine immunisations, including diphtheria, tetanus and polio (DTP) and measles, mumps and rubella (MMR). Europe has seen huge outbreaks of measles this year alone, so all travellers should make sure they have received at least two doses of the measles-containing vaccination. A simple blood test can be done for all those who are unsure about their immunity. Some travellers may wish to consider vaccinations for Hepatitis A and Hepatitis B, rabies and tick-borne encephalitis. The activities you plan to do whilst travelling will determine which vaccines would be required. If you have any doubts or concerns, we also suggest booking a pre-travel consultation with a specialist travel nurse to discuss your options.
Find out more about our travel and wellness vaccinations.
Trekking and Ticks
Bosnia offers a wealth of outdoor activities. Those who plan to take advantage of the great outdoors should strongly consider vaccination against tick-borne encephalitis (TBE). TBE is a bacterial infection. Usually, it is spread through an infected tick bite. However, during Spring to Autumn, the consumption of unpasteurised dairy produce also carries a risk. Contracting the illness causes a fever with neurological complications. It is vaccine-preventable. Protection requires 2 doses of the vaccination, given at least 2-weeks apart. A third dose is given 5-12 months later to give longterm protection. You should also avoid ticks by wearing long trousers and socks. Using DEET insect repellant should also repel them.
If you spot a tick on you, it needs to be removed promptly. Use some flat tweezers or a tick remover and clean the bite with alcohol to reduce the risk of infection.
See our Ultimate Bug Kit.
Rabies
Rabies is a fatal virus that can be found in the saliva of an infected mammal. Most commonly a wild dog. Exposure can happen through a bite, scratch or a lick to an open area of the skin. You cannot catch rabies from another person and it cannot spread through unbroken skin. You should, where possible avoid contact with animals when travelling, especially wild or stay animals.
Rabies is almost always fatal once symptoms appear, but treatment before this is very effective. Pre-travel rabies vaccination offers great protection. And means that in the unlikely event you come into contact with the rabies virus, fast and effective treatment can be given easily and in the country of the incident.
Pre-travel rabies protection requires a series of 3 vaccinations given as injections into your upper arm. Your vaccines will be given over a 3-week period, or over 1 week if an accelerated course is needed, prior to travel. Travellers at greater risk are those who plan to do outdoor activities such as hiking, trekking, cycling or caving. You should consider a rabies vaccine if you plan to do any of these activities whilst visiting Bosnia.
First Aid Kit
For those trekking in the hills, packing good basic first aid kit is essential. When travelling in rural areas, access to healthcare can be limited. Travelling with a medical kit will give you access to basic provisions needed to treat minor injuries and pains.
Basic provisions include pain relief, plasters and medication to treat an upset stomach, such as loperamide and oral rehydration salts. If access to safe water may be limited, consider packing chlorine dioxide tablets. Cuts, scapes blisters and even a twisted ankle can occur, so take blister pads, some waterproof dressings and a bandage to deal with any minor injuries whilst you are there. If you take regular prescription medication, ensure you pack enough for the duration of your trip and carry the prescription with you.
Book your travel appointment today
By Anna Chapman | Travel Nurse | August 2019
Tanzania is the perfect haven for adventurous travellers. Not only does it boast three of Africa’s Seven Natural Wonders, but it is home to the ancient nomadic stewards, the iconic, Maasai people. It is also the perfect place for an African safari adventure, with it’s 16 national parks accounting for more than 30% of the country.
Tanzania is blessed with the highest peak in Africa. Mount Kilimanjaro beckons visitors from all over the world. It is the world’s highest free-standing volcano and gets an estimated 30,000 travellers attempting to summit the peak each year. Climbers by the thousands venture here to challenge themselves on its muddy slopes, rocky trails and slippery scree.
It’s crowning jewel is the island, Zanzibar. The island is famous for its mix of exotic white sand beaches, dense palm trees and coral seas. A true paradise. It hosts famous spice plantations and is rich with diverse culture. Unguja (the main island in Zanzibar) is also home to many endangered species including the red colobus monkey and green turtle.
Whether you are visiting for an action-packed safari, challenging yourself to reach the peak of Mt. Kilimanjaro or relaxing on the island of Zanzibar, ensure you follow our top travel tips to stay healthy in Tanzania.
Vaccines
All travellers should ensure they are in date with all their routine immunisations, including diphtheria, tetanus and polio (DTP), and measles, mumps and rubella (MMR).
You should consider specialist travel vaccinations prior to travel. Hepatitis A and Typhoid are highly recommended. Furthermore, some travellers may also wish to be vaccinated against Rabies, Hepatitis B and Cholera for extra precautions. Especially if travelling to more rural areas.
For more information on our vaccines, please visit our travel and wellness vaccination pages.
Yellow Fever
In Tanzania, there is no risk of yellow fever. If you are only travelling directly from the UK and back, it generally isn’t advised to have yellow fever vaccine. There is, however, a requirement for travellers to have a certificate of vaccination if they enter Tanzania from another country that has Yellow Fever. Bordering countries such as Kenya, Uganda, Rwanda, Burundi & DRC would all require a certificate. In this instance, a vaccination or a waiver certificate may be advised. It is best to speak with a specialist travel nurse, who will look at your route and access what vaccinations and certificates you would require.
Prevent Malaria
Whether you plan to visit Zanzibar or the mainland, all areas of Tanzania have a risk of malaria. Therefore, you should take anti-malarial medication. Malaria is spread by mosquitoes that are most active between dusk and dawn. A common question is whether or not you need to take them if you plan to trek Mount Kilimanjaro. Even though the risk of malaria is low in areas above 2,500m, the start and finish of the trek take you well below this altitude. In short, you should take medication to prevent it. You should take precautions to reduce the risk of being bitten in the first place.
Precautions include:
- Wear long, loose clothing
- Wear plenty of mosquito repellent with a minimum of 50% DEET
- Use clothes spray containing permethrin – you can spray before you travel for short-duration trips
- Sleep under a mosquito net
See our Ultimate Bug Kit for everything you need to keep the mosquitos at bay.
Climbing Kilimanjaro
If you are trekking Kilimanjaro, make sure your pre-travel plans take this into account. Trekking is physically demanding and exposes you to the risk of altitude sickness. The summit of the peak is 5,895m and treks can take anything from 5-9 days. Altitude sickness is unpleasant. Not only this but it can develop into something more serious and become life-threatening. Take time to acclimatise. This will reduce your risk of developing altitude sickness. Ideally, choose a longer trek. A slower ascent over more days will reduce your risk considerably. Alternatively, you can get a prescription of acetazolamide (Diamox) to aid the process. Speak to a specialist travel nurse about this at your pre-travel consultation. Don’t let altitude sickness ruin your trip.
Book your travel appointment today
By Anna Chapman | Travel Nurse | August 2019
Osteopathic manipulation, or HVT (high-velocity thrust) as it is more technically known, is the “click” that many people associate with osteopathic treatment.
It is by no means always used by an osteopath, but when it is, it can prove to be a quick, efficient, and pain-free way of restoring function to a joint.
Many patients’ conditions may not be suitable for HVT, and many may not be keen to have it done anyway. In these cases, the osteopath will treat with a whole collection of other highly effective ways. HVT should be seen as a useful tool in some circumstances, but not a be-all and end-all of osteopathy.
So how does it work?
HVT is placing a short sharp tug though a joint, most often a spinal facet (which is what we will concentrate on here), a click may or may not be heard. The noise itself is a bit of a by-product. What it is has been disputed a little but the generally accepted explanation is that when the joint is stretched, the synovial fluid inside the joint itself physically does not stretch, so gas is forced out of solution causing gas bubbles that allow the joint to gap slightly, causing the clicking noise. This also explains why another click cannot be produced for a little while until the gas has been reabsorbed.
The gapping of the joint is the key to the effectiveness of HVT.
What I must point out at this point though is that the click is not a relocation of a joint.
Barely a day goes past that someone doesn’t tell me their osteopath “clicked something back in” often assuming it was a disc. As much as it can feel miraculous like this sometimes, and a patient can often feel and be quite a bit straighter following treatment, the HVT is about restoring function to the joint, not putting it back in place. Discs especially do not just “pop back in”.
So what does the gapping achieve?
Well, here we have to get a little technical. There are three predominant effects caused by HVT as far as we can tell.
Firstly, post-contractile sensory discharge or PCSD.
Imagine that the brain keeps many muscles at a gentle tension, this allows you to hold your posture. When an area is identified as problematic (painful or inflamed etc), the brain may choose to cause the muscles around the area to spasm, often to protect the area. The spasm itself may cause further pain. This then becomes a vicious circle and dysfunction.
Tension in the muscles is controlled by spindle fibres. This is what detects the short sharp tug of the muscles in HVT. Imagine the short sharp tug as a reset for these fibres. The brain then has to determine the level of muscle tension required and often can reset to the original tension, immediately bringing the joint out of spasm.
Massage of muscles, slow stretching over a longer period, has a similar effect but unfortunately can’t be performed on the small, deep muscles directly around and holding the joint.
Secondly, pain gate theory.
Even when nerves are reporting pain in a certain area, it is important that the body can still detect a soft touch in the same area. To achieve this soft touch and position detecting nerves override deep pain detecting ones. Where you ever told to rub your knee or elbow after you bumped it and it hurt? That’s pain gate, the soft-touch overrides the deep pain. It won’t stop it completely of course but even a little relief will make it feel better. In turn, this may again stop the brain causing the area to spasm.
HVT moves the joint quickly and sharply. This causes the positional detectors to immediately report this to the brain, inhibiting the deep pain.
Thirdly, meniscoid theory.
In a joint, smooth cartilaginous surfaces rub together, but they may not be quite as smooth as we used to think. Small pieces of cartilage appear to be in the joint. Possibly to fill small gaps; craters on a moonscape is a good way to think of it. It has been suggested that when the joint spasms, these small bits of cartilage, which are attached to the capsule around the joint can become trapped out of place. Gapping the joint allows the tethers to the capsule to quickly pull them back into place.
It’s possibly worth pointing out before I finish, that although I said earlier that the click is an unnecessary by-product, I do wonder if it could be argued that the psychological effect of hearing the click could be put forward as a fourth effect. Hearing a click and knowing that it may have relieved a painful joint does often make a patient immediately relax. This may itself be part of the healing process.
Osteopathic manipulation is often a quick efficient way of relieving dysfunction of a joint. It is not a miracle cure. Many other things have to be taken into account for the osteopath to treat fully and effectively.
HVT will not immediately heal damaged tissue or disperse inflammation, but it often is a good way to kick start the process.
Book an osteopathy appointment
By Andrew Doody | Osteopath | August 2019
What is Cyclospora?
Cyclospora is a tiny, single-celled parasite, spread by contaminated food. It can cause diarrhoea, abdominal cramps, nausea, loss of appetite, bloating, gas, fatigue, mild fever, and weight loss.
Why is it in the news?
There’s been an outbreak in travellers to Mexico, with at least 204 reported cases in returning holidaymakers since June. However, it is difficult to detect using standard tests. Because it is uncommon in the UK, most labs don’t look for it and may miss the diagnosis. So the true number is probably much higher.
What’s the most reliable way of detecting it?
The best way is called a rapid PCR test, which detects the parasite’s DNA. The test also looks for DNA and genetic material from 21 other diarrhoea-causing parasites, bacteria and viruses at the same time – so there is a very high probability of finding the right cause. As you’d expect, the test is available at the Fleet Street Clinic. Importantly, we can have a result within an hour or so of receiving a sample.
How can I prevent it?
Outbreaks have been linked to eating fresh uncooked berries/unpeeled fruit and salad items that have not been washed in safe water. Sticking to foods that have been freshly and thoroughly cooked, when you travel, is the safest option.
How is it treated?
Confirmed cases can be treated with an antibiotic called co-trimoxazole. Some of the more commonly-used antibiotics for travellers’ diarrhoea may not be effective.
If you have any concerns about cyclospora and other parasites, our PCR test service can help detect the exact cause of any issue you might have. What this allows is proper diagnosis and treatment. Usually, guess-work on what bug a patient is carrying or general prescriptions to tackle the illness might be given by medical professionals. The PCR test offers accuracy like nothing else.
You can book an appointment online.
Imagine you’re holidaying in a tropical paradise, walking barefoot on the beach. Would you consider this a health risk? What if this simple, carefree activity could turn your trip into a nightmare?
Unfortunately, this is what happened to a Canadian couple in the Dominican Republic, who contracted hookworm in Punta Cana after walking on the beach without shoes.
Fleet Street Clinic’s medical director, Dr Richard Dawood, is Telegraph Travel’s medical expert and shared his medical opinion on the case in a recent article.
The article details the story of the couple, who shared their plight on social media to raise awareness of the parasitic worm infection.
Hookworm can infect humans if soil contaminated with their larva comes into contact with bare skin. Most commonly, hookworm infection can occur in Africa, the Americas, China and south-east Asia, according to the NHS.
Dr Dawood explained to the Telegraph how you can spot a hookworm infection:
“Typically there is a linear rash that follows the track of the migrating larva. It can become almost unbearable itchy, much worse than an insect bite, which is an important clue. There’s a local allergic reaction, which can then blister, making the line pattern harder to spot.”
And how to treat: “There are a number of different anti-parasitic treatments that work, either taken as tablets, or made into a cream and applied locally. The larvae can sometimes also be killed using cryotherapy to freeze them. Blisters or scratching can easily lead to infection, necessitating antibiotic treatment.”
To avoid hookworm, avoid coming into contact with soil or sand that could be contaminated. If walking on the beach, it’s advisable to wear shoes at all times!
Dr Richard Dawood at Fleet Street Clinic
Dr Richard Dawood is founder of Fleet Street Clinic in London and has practiced for over 35 years. He was one of the first doctors in the UK to establish Travel Medicine as a distinct speciality. Richard is the most senior UK travel medicine specialist working exclusively in a private setting.
You can book a travel consultation appointment online.
UPDATED RECOMMENDATIONS FOR Yellow Fever VACCINATION: Nigeria
The World Health Organization recently updated the yellow fever recommendations and requirements for residents and travellers to Nigeria.
As of 1 July 2019, the yellow fever certificate requirement for travellers to Nigeria changed. All travellers aged 9 months or over are now required to travel with a yellow fever vaccination certificate along with a valid visa. Failure to provide a valid certificate where required could deny entry to that country, or result in quarantine.
Previously a certificate was only required for those arriving from risk areas countries. However, an on-going outbreak of yellow fever, which started in September 2017, is continuing therefore a revised classification has been made. Between January and April 2019, a total of 930 suspected cases were reported in 447 Local Government Areas.
Advice for travellers
The Fleet Street Clinic would like to remind all travellers from the United Kingdom that there is a risk of yellow fever transmission throughout Nigeria.
We are a Certified Yellow Fever Centre with availability throughout the week and are usually able to accommodate same day appointments requests.
What is Yellow Fever?
Yellow Fever is an acute viral haemorrhagic disease transmitted by infected mosquitoes and has the potential to spread rapidly and cause serious public health impact. There is no specific treatment, although the disease is preventable using a single dose of yellow fever vaccine, which provides immunity for life.
For more information about Yellow Fever & the Vaccine.
Anyone travelling to Nigeria should book a Pre-Travel Consultation. One of our specialist Travel Nurses will access if a Yellow Fever vaccine is suitable for you.
Links:
World Health Organization
Japan is hosting the biggest Rugby event of the year in September.
Starting 20th September, across 12 Japanese cities, 48 matches will be played to determine the winner of Rugby World Cup 2019. Millions of people from around the world are expected to travel to Japan to attend this amazing sporting event. Much like any other reason for travelling, it does come with some health risks.
Big sporting events, like the Rugby World Cup, attract huge numbers of people which increases the risk of getting sick and spreading diseases. Venues are sometimes described as giant Petri dishes, where viruses and bacteria can flourish and spread.
But how can you prepare yourself so you remain healthy throughout your holiday?
Be prepared…
Get Vaccinated
It is advised that individuals are up-to-date with routine immunisations including diphtheria, tetanus and polio (DTP).
If you plan to venture outside of the major cities and explore Japan whilst you are there, you may need to consider some travel vaccines, such as Rabies and Hepatitis A or Hepatitis B. If those plans include visiting more rural areas, Japanese Encephalitis could be considered. For those trekking, hiking or camping, a vaccination against tick-borne encephalitis will provide protection against the disease.
MMR is a must
Ensure you are immune to measles before you travel. Japan has had multiple large outbreaks of measles this year and it is a highly contagious disease.
The best protection against measles is to ensure you have received 2 doses of the MMR vaccine. You may not have received the full course during your childhood vaccines which means you’re not fully immune. A simple blood test can determine immunity if you are unsure.
Beware of Flu Season
Flu season for the Northern Hemisphere begins in Autumn, which coincides with the start of the Rugby World Cup. It’s possible people could pick up the flu virus at these events as the Flu is a highly contagious viral disease. Transmission of the flu is always amplified when large groups of people congregate in enclosed space. People travelling to and from mass gatherings can also spread flu to other communities and to family members when they get home. An infected person can transmit the virus before even realising they are sick.
Getting a flu vaccine every year is the best way to avoid getting seasonal flu.
Those travelling from mid-September onwards should consider getting the flu jab as soon as it becomes available.
Find out more about our travel and wellness vaccinations.
Minimize Your Risk
Besides the flu vaccine, here are a few tips on how to minimize your risk of contracting an illness at the Rugby World Cup:
- Keep a distance from people coughing and sneezing – droplets from coughs or sneezes containing flu virus can travel at least 3 feet, so keeping this distance from sick people can help lower your chance of becoming ill.
- Wash your hands often, before eating or after contact with sick people, public places and bathrooms to limit your chances of contact with the virus.
- Carry hand sanitizer to use when hand washing is inconvenient or not available. Ensure it has a minimum of 60% alcohol content to be most effective.
- Avoid touching your mouth, nose and eyes with your hands.
- Use clean, disposable tissues to wipe your mouth or blow your nose. Throw away used tissue immediately after use.
- Avoid getting overly cold and wet by wearing appropriate clothing.
- if you are already sick, wear a face mask to help lower the chance of spreading your illness to others.
First Aid
Despite having a good reputation for health care, it’s worth being prepared for minor illnesses and injuries when travelling abroad. Pack an essential First Aid Kit for your travels and include some basic items such as pain relief, plasters, antiseptic creams and something to treat minor wounds. Being able to treat minor accidents whilst abroad means less time hunting down a pharmacy or time wasted visiting a doctor should you need it.
For convenience, we sell a ready to go Essential First Aid Kit, available online.
You can book a pre-travel consultation online.
Greenland is home to truly magnificent mountainscapes and glaciers.
Jakobshavn Glacier, the world’s fastest-moving glacier in the Northern Hemisphere can be found here.
In the Winter, tourist travel to this wonderland to potentially see the wondrous the Northern Lights. Things are quite different in the Summer.
Chasing the Midnight Sun
Summer in Greenland is an image not often associated with the country. Summertime offers eternal light in the land of ‘The Midnight Sun’ whereby the day has neither a beginning nor an end. Those wanting to experience this time-shifting experience must travel north or the Arctic Circle. The low-lying sun makes the surrounding scenery appear almost dreamlike; icebergs and hilltops are bathed in a surreal palette of pink, purple, yellow and red. Travellers to Greenland have options of hiking the land or sailing the fjords between icebergs.
If you plan to travel to Greenland this summer follow our top travel tips to ensure you stay healthy.
Vaccinations
Even though Greenland resides in the Arctic Circle, travellers should still ensure they receive appropriate pre-travel vaccinations. This includes being up-to-date with Measles, diphtheria-tetanus and polio. Greenland has a high risk of Rabies, a virus spread through the infected bite of a mammal. Travellers who plan to trek inland may wish to consider this vaccination before they travel to reduce the risk.
Suncare
Despite Greenland having long, dark winters, the summer months provide almost constant light. Bright sun, combined with the effects of lights reflection from snow and water can increase the risk of sun damage from UV light. Despite temperatures remaining cold, travellers still need to be sun smart. Ensure you wear a high factor SPF, and use lip balm to prevent cracking. Polarised sunglasses that wrap around will prevent the UV rays causing damage to your eyes.
Sea Sickness
Many activities in Greenland involve taking to the water and visiting the infamous Disko Bay in search of Icebergs. Sometimes the seas can be rough which can make for a miserable time if you are prone to travel sickness.
Sea Sickness can be reduced by:
-
Sit in the centre of the boat where the motion will be less aggressive
-
Close your eyes or focus on a point on the horizon, this can help your inner ear balance.
-
Avoid alcohol and large heavy meals, instead, keep hydrated on water and eat smaller lighter meals
-
Sucking on a mint or ginger sweet can help with nausea
-
Seas Sickness medication tablets
-
Patches that can be used to prevent sea-sickness
Trekking
Parts of Greenland can be remote so taking a good First aid kit with you is essential. Basic provisions include pain relief, plasters and medication to treat an upset stomach, such as loperamide and oral rehydration salts. If you take prescription medication to ensure you pack enough and carry the prescription with you. If you plan on trekking the hinterland, pack additional items such as blister dressings and plasters.
Book your travel appointment today
By Anna Chapman | Travel Nurse | July 2019
June to September is the best months to trek to Machu Picchu, although you can visit all year round. The weather is at its driest and coolest with gloriously sunny days. Trekking to the roof of the Andes is a rewarding experience that many travellers to Peru sign up for. Travellers who are trail-blazing their way on the Inca road to catch a glimpse of the forgotten city should follow our top travel tips to ensure they stay healthy on the road.
Vaccinations
All travellers to Peru should ensure that they are up-to-date with measles, diphtheria, tetanus and polio (DTP), and have received vaccinations against Hepatitis A and Typhoid. There is a risk of Rabies and Hepatitis B in Peru, and all travellers attempting the Inca Trail should consider vaccinations against these.
There is no risk of Yellow Fever on the Inca Trail or Cusco. However, the vaccination may be recommended to travellers who are doing further travel in Peru, such as the Amazon rainforest. Those planning to extend their trip to South America may require the Yellow Fever vaccination for personal protection. Additionally, you may require a valid yellow fever certificate to enter some other countries. It is best to book in a travel consultation with our specialist travel nurses to discuss your route.
Altitude Sickness
The highest altitude of the Inca trail is 4,215m, a whopping 1,800m higher than Machu Picchu itself! Most people start the hike from Cusco which lies at 3,400m, meaning trekking this wonder of the world poses a real risk of altitude sickness. Altitude sickness is unpleasant and can develop into something serious and become life-threatening. It is best avoided by taking time to acclimatise. Ideally, if you are arriving from sea level, spend a few days in Cusco before your trek begins to adjust to the different altitude. Choose a longer trek, a slower ascent over more days will reduce your risk considerably. Alternatively, you can get a prescription of acetazolamide (Diamox) to aid the process. Speak to a specialist travel nurse about this at your pre-travel consultation. Don’t let altitude sickness ruin your trip.
Stay Hydrated
Treks on the Inca trail usually last around 5 days, meaning that an average trekker will probably consume at least 15 litres of water over the course of their trek. Unclean and unsafe drinking water can lead to sickness and diarrhoea so it is important that travellers have access to safe water. Carrying 15 litres of water on the trail is a near impossibility so travellers should ensure that they have a way to make water safe to drink. Carrying water purification tablets, or a bottle with a filter can ensure you have access to safe drinking water throughout.
Travellers Diarrhoea
Travellers diarrhoea and other common gastrointestinal infections can put a dampener on any adventure but especially when hiking. Access to toilets is likely to be limited throughout your journey so it is important to stay healthy. Ensure all food you eat is thoroughly cooked. Pack an alcohol hand gel so you can keep your hand clean before you eat and after using the toilet. It is wise to carry medication with you, so, if you do become unwell you have doctor-approved medication available to take. We recommend packing one of our Worldwide Gastro Kits. Inside there is medicine to prevent and treat travellers diarrhoea, dehydration, mild infections, nausea and vomiting. Hopefully, you won’t have to use this kit, however, for peace of mind, it is better to be safe than sorry.
Foot Health
The Inca trail typically consists of between 6-9 hours of walking a day, with shared tent accommodation. Hiking the Inca Trail through the Sacred Valley to Machu Picchu is both arduous and awe-inspiring. Make sure you have good walking boots that are broken in before you start. Book an appointment with a podiatrist and osteopath if you have any niggles or pain before setting off. Take care of your feet throughout your adventure – keep them clean and dry to avoid problems. Any blisters should be cleaned and covered with a dressing to prevent pain and infection. Pack your own first aid kit with some basic medications for pain, allergies and upset stomachs in case you do become unwell. Access to medical supplies will not be until Aguas Calientes at the end of the trek. You can buy a Fleet Street Clinic Essential First Aid Kit online to save you the hassle of assembling yourself. We would recommend considering a medical pedicure upon your return. Treat our feet a little bit of TLC for taking you on an adventure of a lifetime.
We would encourage all those taking on the Inca trail adventure to consider booking a travel consultation with either myself or another of our specialist travel nurses. We all have extensive knowledge on what vaccines and health precautions you should take on an individual basis to remain healthy throughout your adventure. Chances are at least one of us has done a similar adventure so we can give you some first-hand experience on what to expect too!
Book your travel appointment today
By Anna Chapman | Travel Nurse | July 2019
The health of both our planet and its people is, without doubt, one of the most important issues of our time. Maintaining healthy wellbeing has been in the public eye for some time now, particularly the topic of how to achieve good mental health. Chinese medical thought and acupuncture treatment can help us understand what we can do to help ourselves to achieve and maintain good health. Its teachings encourage us to inhabit our body, to connect to and to nourish our physical self and the physical world around us. This physical basis provides the root of our mental and emotional well-being.
A holistic treatment
Where Western Scientific Medicine has gone down the microscope to discover the minutiae workings of the human body (cells, biochemicals, genes), the understandings of Chinese Medicine, developed over thousands of years, have focused on how the body systems work together. It observes a person in their environment, their lifestyle, their posture… to understand the causes of ill-health, and the symptoms that arise to alert us to this. The whole body-mind is considered, and treated, to bring us back to good health and well-being.
A leap of faith for our Western minds
Acupuncture is a leap of faith for our Western minds. The concepts on which it is based do not exist in Western thought. You can’t cut open the body and find the meridians which form the energetic framework of the human body, or the Qi (pronounced ‘chee’, meaning energy) which flows through this network to motivate our physiological processes. Similarly, you can’t cut open a light bulb and find electricity. Likewise, you cannot cut open a computer and find cyberspace. It doesn’t mean that these things don’t exist. Proof of their existence lies in their application and the same is true of acupuncture treatment. Only through experiencing acupuncture for yourself will you be able to judge its true value.
Acupuncture helps reduce stress
Acupuncture is often described as incredibly relaxing, regardless of what a person seeks treatment for. Furthermore, most patients report an improvement in energy levels, sleep and a feeling of general well-being.
Acupuncture helps calm the nervous system. As a result, it helps switch off the ‘Fight-Flight’ stress response. Fuelled by adrenaline to keep us alert and primed for action, the stress response helps us to achieve. It is a useful tool for success. If the stress reaction is prolonged and not switched off, problems start to arise.
Heart rate increases, breathing quickens, muscles tighten, blood pressure rises .. it is perhaps not surprising that stress-related ailments are estimated to account for 75-90% of all doctor’s visits. By calming the body and promoting parasympathetic activity, Acupuncture helps improve circulation and reduce general muscle tension. This enhances all body functions not concerned with immediate survival – immunity, digestion, fertility, rest, recovery, repair. Generally speaking, the results note an overall feeling of relaxation and well-being.
Acupuncture helps manage day-to-day ailments
Our Acupuncturist, Diane, has 25 years experience in Chinese Medicine. She treats a wide variety of day-to-day ailments. Including headaches, IBS, anxiety, infertility. As well as the musculoskeletal pain, which acupuncture is most famous for. Why not book an appointment today to see how acupuncture can help you improve your health and well-being?
If you think you could benefit from acupuncture, you can book your appointment online.
By Diane Timewell | Acupuncturist | July 2019
The Southern African nation, Mozambique is gaining popularity amongst the adventure traveller community. Often referred to as ‘The Pearl of the Indian Ocean’, it is well off the usual tourist trail of Africa. Mozambique offers rustic beaches, delightful architecture, superb national parks, and plenty of diving opportunities.
Many choose to start their adventure exploring the capital city, Maputo. It is easy to understand why. It is rich in culture with beautifully preserved Portuguese colonial architecture. You could easily spend a week enjoying the hospitality of the friendly locals, eating the delicious food and partying the night away. Maputo is a largely-underestimated African capital city.
Mozambique is also known for having some of the most pristine dive sites in the world. Tofo is arguably one of the greatest places on Earth to see megafauna marine life. Crystal clear water provides perfect visibility to view the abundant marine life. The beautiful tropical Islands of the Bazaruto and Quirimbas Archipelagos are some of the most romantic and secluded beach destinations in the world – ideal for honeymooners.
Whatever your holiday entails, ensure you read out top travel tips to stay healthy in Mozambique.
Vaccinations
Travellers should ensure they are up-to-date with their routine immunisations including measles, mumps and rubella (MMR) and diphtheria-tetanus and polio (DTP). Additional travel vaccinations are advised including hepatitis A, typhoid, rabies and hepatitis B. It’s best to speak with a travel nurse about any specific travel vaccinations you may need in a pre-travel consultation.
For more information on our vaccines, please visit our, travel and wellness vaccination pages.
…What about Yellow Fever?
Yellow Fever is a viral haemorrhagic illness spread from the infected bite of the Aedes mosquito. Whilst it can occur in parts of Africa, there is no risk of Yellow Fever in Mozambique. Therefore, travellers do not need to be vaccinated.
The only exception to this will be for travellers who are entering Mozambique from a country which does have a risk of the illness. In this case, it is best to speak to a travel nurse to see if you require the vaccine. If you do, you will need to be in possession of a Yellow Fever Vaccination certificate as a condition of entry. Ask your travel health specialist for advice.
…And Polio?
Polio is a viral infection. As it is contagious, you can get polio from contact with an infected person. In addition, consuming food or water that has been contaminated by a person with poliovirus also puts you at risk. There has been a worldwide effort to eliminate polio, which is proving highly successful. However, Mozambique still remains at risk due to vaccinate-derived circulating strains. All travellers should ensure they are up-to-date with their polio immunisation. The polio vaccine is a combination vaccination, given with diphtheria and tetanus. It provides protection for 10 years.
If you plan to stay for longer than 4 consecutive weeks, it’s advised that your polio vaccine be administered within the last 12-months. You should also have the dose recorded on an International certificate of vaccination prophylaxis card as proof of immunisation. Furthermore, long-term travellers to Mozambique may be required to show this when they leave the country, as proof they have been immunised.
Malaria
All of Mozambique has a risk of malaria. Malaria is an infection spread by the Anopheles mosquitoes which are most active during dusk till dawn. You should take strict precautions against mosquito bites. This includes wearing long loose clothing and using an insect repellent with a minimum of 50% DEET. You can reduce the risk of indoor mosquito activity with the use of plug-in vaporisers. Plus, sleeping under a mosquito net can help reduce night-time bites.
We recommend taking antimalarial medication for the duration of your trip. As there are different options available, it’s best to speak to a travel nurse to find the best option for you and your family.
See our Ultimate Bug Kit.
Special precautions post-Cyclone Idai
Cyclone Idai battered the coast of Mozambique on the 9th March 2019. The storms brought heavy rains, winds and flooding. As a result of the initial impact alone, there were hundreds of fatalities. The storm created many serious health risks. Firstly, like most natural disasters, the storm has displaced a huge number of local people. Which as a result, will increase the risk of diseases spreading. Secondly, it has placed a strain on the countries structural and health infrastructure. Which as a result, and can lead to further flooding and increases the risk of water-borne infections such as cholera. Thirdly, the increase of water has led to an increase in breeding sites for mosquitoes. Therefore, there is an increased risk of malaria and other mosquito-transferred diseases.
Although the risk for tourists will be much lower than that of the local population, extra precautions to avoid infectious diseases should be taken. You should pay extra attention to the food and water hygiene you consume. This will minimise the risk of you getting a diarrhoeal illness.
If you are travelling to an area with a known outbreak, the Cholera vaccine can be considered. Similarly, those undertaking humanitarian work or those with inadequate access to safe water and sanitation should also consider the vaccine.
Book your travel appointment today
By Anna Chapman | Travel Nurse | July 2019
THE WORLD HEALTH ORGANISATION (WHO), HAS REPORTED THAT POPULATION EXPOSURE TO HEAT IS INCREASING DUE TO CLIMATE CHANGE.
The WHO states, ‘global temperatures and the frequency and intensity of heatwaves will rise in the 21st century as a result of climate change’. Extended periods of heat exposure during the day and night time can increase the amount of physiological stress on the human body.’
The stress caused by heat exposure exacerbates the top causes of death globally. This includes respiratory and cardiovascular diseases, diabetes mellitus and renal disease.
They go on to state, ‘Exposure to excessive heat has wide-ranging physiological impacts for all humans, often amplifying existing conditions and resulting in premature death and disability.’
With the temperature said to continue rising, the WHO also states, ‘Awareness remains insufficient of the health risks posed by heatwaves and prolonged exposure to increased temperatures.’
So, who is most affected by heat exposure and how will it impact your health?
Who is affected?
Rising temperatures affect the whole population. However, some populations are more vulnerable to exposure to excessive heat. Those include:
- Elderly people
- Infants and children
- Pregnant women
- Outdoor and manual workers
- Athletes
- Poorer communities
How does heat impact health?
With rapid increases in external temperatures, the body will struggle to regulate our internal temperatures. The knock-on effect of this can result in a number of heat-related illnesses such as heat cramps, heat exhaustion, heatstroke, and hyperthermia. Reported small differences in the seasonal changes have been reported to have increased the number of heat-related illness and even death. Rising temperatures can also worsen chronic conditions such as cardiovascular, respiratory, and cerebrovascular disease and diabetes-related conditions.
What actions can you take to stay cool?
- Aim to keep your living space cool. WHO suggests ‘below 32 °C during the day and 24 °C during the night’
- If it is safe, open your windows at night time to cool your living space.
- Stay out of the heat by staying in the shade and avoiding going outside during the hottest part of the day.
- Take cool showers and wear loose-fitting clothing.
- Drink regularly and avoid alcohol and caffeine.
- Check on vulnerable family members who may be affected by the heat.
What to do if someone shows signs of a heat emergency?
It is extremely important to know what to do when someone is showing signs of heat illness. Everyone should know how to respond to heat emergencies, this can be learnt in first aid courses.
If one of your family members or someone you assist is showing signs of hot dry skin and delirium, convulsions and/or unconsciousness, call a doctor/ambulance immediately.
Whilst you are waiting for help to arrive place them in a cool place in a horizontal position and elevate their legs. It is now important to initiate external cooling.
This can be done by:
- Removing clothing
- Placing cold packs on the neck and groin
- Spraying cool water on their skin
- Fanning them
- If they are unconscious, place them on their side
If you or someone you are with is displaying mild signs of heat illness that is not considered an emergency, you might want to consider a same-day GP appointment. You can book an appointment online.
Have you ever thought of applying sunscreen before taking a flight?
If not, you may want to reconsider.
A recent article in the Telegraph Travel with contribution from Fleet Street Clinic’s medical director, Dr Richard Dawood, has highlighted a study published in the Journal of the American Medical Association (JAMA) Dermatology. It reports that pilots flying for about 56 minutes at 30,000 feet were exposed to the same amount of carcinogenic UVA radiation as one would receive 20-minute session on a tanning bed.
The plane’s windshield blocked only about half of the UVA rays, dangerous enough to contribute to cancer risk.
However, applying this potential risk to all types of aircraft and to the cabin space outside the cockpit is “a bit speculative”, notes Dr Dawood. The aforementioned study was based on UV radiation measured from the cockpit of a Socata TBM850, a single turbo-prop private plane.
“Awareness of the issue is a good thing – especially for pilots; and for passengers, sensible use of window shades to avoid strong direct sunlight, which most people probably do anyway,”
– says Dr Richard Dawood.
For more travel advice, contact our expert travel team at Fleet Street Clinic – you can book an appointment online.

Planning a trip abroad?
Whether you’re travelling afar for business or pleasure, the long-haul travel involved can be a daunting prospect. But with a little preparation you can enjoy a comfortable journey, and prevent the health risks associated with travel.
At Fleet Street Clinic, we regularly see frequent travellers for travel health-related consultations and vaccinations. Our travel experts have compiled some tips to ensure you are in great shape throughout your travels, starting with a healthy outbound flight:
Deep Vein Thrombosis (DVT)
Travelling on long-haul flights with extended periods of immobility can leave you at an increased risk of DVT (blood clots), especially if you have any pre-existing conditions.
To prevent DVT during your flight:
- Wear loose comfortable clothes.
- Keep moving during the flight – get up regularly to walk around the cabin to aid circulation.
- Keep hydrated by drinking plenty of water- drink at least one cup of water for every hour spent in the air.
- Avoid alcoholic and caffeinated drinks.
- Wear compression socks which apply gentle pressure to the ankle to help with blood flow.
Dehydration
Air in the plane’s cabin is recirculated, which results in a loss of moisture. This can cause dry skin, lips, and eyes.
To prevent dehydration:
- Contact lens wearers should remove lenses prior to travel and wear spectacles to avoid dry eyes and prevent damage to the cornea.
- Dry skin should be moisturised, and if nasal irritation occurs, a saline spray can be used.
- Keep hydrated – don’t be afraid to ask cabin staff for water outside of mealtimes.
Travel / Motion Sickness
Motion sickness occurs when there is confusion between what the eyes see, and what the inner ear senses. With turbulence, cramped spaces and lack of fresh air, susceptible travellers can suffer.
To minimise the risk of travel sickness:
- Keep hydrated.
- Avoid large meals prior to and during the flight.
- Request a seat near the front wing – the most stable part of the plane.
- Use preventative medication such as Cinnarizine (to be taken 2 hours prior to boarding the aircraft).
Jet Lag
Flying can leave you feeling sleep deprived and jet lagged.
To reduce avoidable risks and arrive at your destination in good shape, here’s how you can prevent or combat the effects:
- Avoid night-time flights when possible – otherwise make sure you build a rest period into your schedule on arrival.
- Give your body clock clues as to your new time zone – adjust your watch, observe local mealtimes and bedtimes.
- Use melatonin and timed exposure to bright light – talk to your doctor or consult a specialist travel clinic about using medication to aid both sleeplessness and wakefulness.
- Use our Jet Lag Calculator – whether you’re using timed exposure to bright light, melatonin, both or none of these methods, our calculator can calculate timings based on your exact travel details.
Book An Appointment
If you’re taking a long-haul flight and need travel vaccines or advice, you can book an appointment online to ensure a smooth transit to your destination.
Approximately 1 in 4 people in the UK will experience a Mental Health problem.
Unfortunately, how we cope with mental health problems, in general, seems to be getting worse.
Leading to an increased number of self-harm and suicide victims. Spotting early warning signs in the workplace and helping those who may be experiencing workplace problems is an extremely important part in reducing the number of deaths by mental ill health each year.
Stress, anxiety and depression are the biggest cause of sickness absence in our society. At Fleet Street Clinic, we believe in creating safe, healthy workplaces where mental health and physical health of employees are valued equally. Therefore, we believe that investing in mental health first aid training, much like physical first aid training should be part of everyone’s corporate wellbeing strategy.
The Fleet Street Clinic will be running a two-day Mental Health First Aid course delivered by Leigh Mckay. This course is designed for all employees, line managers, HR professionals, OH workers and senior leaders alike who wish to become a qualified mental health first aider. By training your staff you’ll be joining a global movement of over 3 million trained Mental Health First Aiders across 25 countries.
Leigh is a quality assured MHFA instructor accredited by the Royal Society of Public Health. She has a particular interest in psychology and emotional resilience. Leigh has a wealth of experience in delivering the MHFA courses in corporate companies. Plus, she advocates that a workplace and community that promotes wellbeing can have a positive impact on everyone’s physical, mental and emotional health.
What is Mental Health First Aid?
Mental Health First Aid (MHFA) is an Internationally-recognised training course. It teaches people how to spot the signs and symptoms of mental ill health. MHFA won’t teach you to be a therapist, however, just like physical first aid training, it will teach you to listen, reassure and respond, even in a crisis.
A quality assured instructor will deliver the adult MHFA courses, which are for everyone aged 16 upwards. All instructors attend an Instructor Training programme accredited by the Royal Society for Public Health. Therefore, they are specifically trained to keep people safe and supported whilst they study this course.
What will I learn?
Learning will take place through a mix of group activities, presentations and discussions. Throughout the course, you will gain practical skills and awareness about mental health.
This includes:
- A deeper understanding of mental health and the factors that can affect people’s wellbeing, including your own
- Practical skills to spot the triggers and signs of mental health issues
- Confidence to step in, reassure and support a person in distress
- Enhanced interpersonal skills such as non-judgemental listening
- Knowledge to help someone recover their health by guiding them to appropriate support
How will attending an MHFA course help?
There are many benefits to taking part in an MHFA course. Firstly, research and evaluation have shown this course raises awareness of mental health literacy. The more understanding and knowledge about mental disorders lead to better recognition, management and prevention. Secondly, this reduces the stigma attached to ill mental health, especially in the workplace. Further, this course champions its students to increase their confidence in handling mental health issues. But, most importantly, it promotes early intervention. Above all, becoming a Mental Health First Aider can enable the recovery of a sufferer and even save lives.
Course Details:
Date: Thursday 26th & Friday 27th September, 2019
Location: 29 Fleet Street, London, EC4Y 1AA
Cost: £350 per person
Spaces are limited.
To book yourself and/or a colleague on to the Mental Health First Aid course, please email to our Corporate Manager, Caroline McKenzie here.
A safari in Namibia is a unique experience in Africa. It has the highest sand dunes on the continent, the world’s oldest and uninhabited deserts, the Skeleton Coast and a lush jungle to the north. Whatever you have planned on your trip, ensure you follow our top travel tips to stay healthy.
Vaccines
All travellers need to ensure they are up-to-date with Hepatitis A, Typhoid and Diphtheria, Tetanus and Polio (DTP). These are your basic traveller vaccine requirements. You may wish to consider further vaccinations against Rabies and Hepatitis B.
There is no risk of Yellow Fever in Namibia, however, travellers who will arrive in Namibia having transited from a country with a risk of Yellow Fever will be required to be in possession of a valid Yellow Fever Certificate.
Countries this would apply to include Kenya, Nigeria, Zambia, Ethiopia, Brazil, Peru and Bolivia. For the full list of countries with risk of yellow fever transmission as per the World Health Organisation.
For more information on our vaccines, please visit our travel and wellness vaccination pages.
Malaria
There is a risk of malaria in the northern areas of Namibia of the Kunene River, Caprivi and Kavango regions and Etosha National Park. Windhoek, Swakopmund and the Skeleton coast have a low risk of malaria. If you intend to visit malarial regions, ensure that you take the antimalarial medication with you. Mosquitoes that are responsible for the spread of malaria are most active between dusk and dawn, and therefore you need to be extra cautious during this time against mosquito bites.
Insects
Ticks, flies and mosquitoes all have the ability to transmit unpleasant disease in Namibia. The best prevention against these diseases is to avoid mosquito bites. Cover up as much as possible and apply a minimum concentration of 50% DEET to any areas of exposed skin. Clothes can be treated with permethrin before setting off to provide an extra level of protection. Sleep under a mosquito net especially if you plan to stay anywhere remote or rural.
See our Ultimate Bug Kit.
Food and water
Travellers should exercise caution with food and water when travelling to Namibia to avoid tummy troubles. Do not drink tap water in Namibia, stick to bottled water or water that has been boiled. If you are undertaking a self-drive trip and plan camping in remote areas it is a good idea to take either a water bottle with a filter or some chlorine dioxide tablets to make water safe to drink should you not be able to find a shop with bottled water. The Namib Desert is one of the aridest in the world so always ensure you pack extra water.
See our Worldwide Gastro Kit to help with any travellers tummy troubles.
Book your travel appointment online today.
By Anna Chapman | Travel Nurse | June 2019
How to Cope During a Heatwave
The UK is currently experiencing a heatwave with temperatures rising to 35 degrees in some parts of the country this week. While sunshine is welcome and the vitamin D is much needed, too much heat can lead to illness. To avoid any heat-related sickness, make sure you are well-prepared! Follow Fleet Street Clinic’s tips to help keep safe during the hot weather.
Risks During the Heat:
- Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes causing rapid dehydration. This can result in heat exhaustion or heatstroke which can be life threatening if not dealt with promptly.
- The highest risk groups are the elderly, babies, children and those with pre-existing medical conditions.
- If you engage in strenuous physical activity this will increase the risk of illness related to the heat.
Top 7 Tips For Beating the Heat
- Seek shelter and shade during the middle of the day (11am -3pm).
- If you are outside, ensure you protect your skin against the sun with a high factor sun cream, hat and sunglasses.
- Wear loose fitting, light-weight and light colour clothing.
- Keep hydrated by drinking plenty of fluids and eating food with a high water content (such as fruit).
- Ensure you are taking in sufficient salt in your diet (sweating leads to electrolyte and salt depletion).
- Avoid caffeine and alcohol, which can worsen heat-related illness.
- Heat stroke can be a life-threatening emergency and medical help should be sought.
About Fleet Street Clinic
Fleet Street Clinic is an independent healthcare practice in London. For more advice or to book an appointment with our expert medical team, you can book online.
Glastonbury has been going for over 50 years and is back this year following a fallow year last year.
Whether you are a festival first-timer or a seasoned Glastonbury veteran, make sure you follow our top tips on how to stay healthy during festival season.
First things first, facilities…
A major part of festival fun is the back to nature approach to living, so do expect basic living facilities. Facilities at festivals are confined to porta-loos, long drops and communal showers; a perfect breeding ground for bugs. Dodge the diarrhoea by following some simple rules. Wash your hands where possible, especially before eating and always after the toilet. If running water isn’t available, use hand wipes or hand sanitiser. Pack your own pocket-size alcohol hand gel for when you are on the go.
The Vaccines…
Don’t be fooled into thinking vaccinations are only for those far-flung destinations. Glastonbury is the largest greenfield festival in the world and over the course of a week, home to over 175,000 people. Crowded spaces and shared living areas increase the risk of infectious diseases spreading. Many of which are entirely vaccine preventable. Measles and mumps cases have been on the rise in the UK, so festival goers should check they have received at least 2 doses of the MMR vaccination to ensure they are protected. If there is any doubt you can get immunity tested to put your mind at ease. Young adults and children can also be particularly vulnerable to meningitis, so if you are in this group, make sure that you have also received the recommended Meningitis ACWY vaccination.
You can find more information on all our vaccinations here.
Eat, drink and be merry…
It is estimated that an average festival goer burns around 9,000 calories and walks over 15 miles. Make sure you fuel your festival by eating plenty, especially if you are drinking alcohol. Keep hydrated and ensure you drink plenty of water to prevent dehydration, especially on those (potentially) hot days.
Come rain or shine…
Glastonbury has seen it all: heatwaves, rain, floods, cloudless skies. The Great British weather is never predictable and exposure to extreme weather can cause anything from hypothermia to heat stroke. Be prepared for all eventualities. Take warm waterproof clothes that will dry quickly in case of wet weather. Pack cool, light coloured clothing to help you keep cool in the sun. Pack a hat and some good suncream and make sure you wear it! Shady areas are few and far between if you are centre stage for the day, and without sun protection you could end up with sunburn, or worse, heat stroke. You can lean more about staying safe in the heat here.
STI’s
Don’t run the risk of sexually transmitted infections if you decide to go beyond social intercourse. The best way to prevent infections such as chlamydia and gonorrhoea is to use condoms. Some STI’s can take several weeks to present themselves, and in some cases are asymptomatic (display no symptoms at all). It is quick and easy to get checked for STI’s, so if you have any concerns when the festival is over, make sure you get tested.
You can book appointments for all our services online.