Category: GP Service
In today’s fast paced world, finding the time to visit a doctor can be challenging. Whether you are juggling a busy work schedule, looking after family, facing mobility issues, or travelling, accessing quality healthcare shouldn’t be difficult. This is where a home visit GP service in London can make all the difference. Fleet Street Clinic offers private GP home visits, ensuring that expert medical care comes directly to you, whenever and wherever you need it.
Why Home Visits Are Essential in London
1. Convenience at Your Doorstep
Navigating London’s traffic and packed public transport can make a short trip to the doctor extremely stressful. A GP home visit removes travel time, allowing you to receive expert medical care in the comfort of your home, office, or hotel.
2. Same-Day Appointments for Immediate Care
Waiting for a GP appointment at a busy surgery can take days, if not weeks. Often, NHS appointments require a registration process that can take several days. With same-day GP home visits in London, Fleet Street Clinic ensures you receive prompt medical attention when you need it most.
3. Personalised and Unhurried Care
Unlike traditional 15- or 30-minute clinic visits that may feel rushed, a private GP home visit allows for a more in-depth consultation. Your doctor can assess your condition in a familiar environment and provide tailored treatment plans suited to your lifestyle.
4. Ideal for Families, Elderly Patients, Busy Professionals, and Travellers
- Parents with young children can avoid exposing them to germs in waiting rooms.
- Elderly patients or those with mobility issues benefit from receiving care without the challenge of travelling.
- Professionals with demanding schedules can fit a GP consultation into their day without taking time off work.
- People travelling into London may need urgent medical attention before flights back home; home visits can also take place in hotels, airbnbs, or any other third party location.
5. Comprehensive Medical Services at Home
Fleet Street Clinic’s private doctor home visits cover a wide range of medical services, including:
- Diagnosis and treatment of illnesses. Prescriptions and medication advice.
- Vaccinations, including flu and travel vaccines. Health check-ups and screenings.
- Chronic disease management.
- Medical certificates and sick notes.
- Wide range of services including blood tests, urine samples, swabs, and more.
Book a GP Home Visit in London Today
If you need a home visit GP in London, Fleet Street Clinic is here to help. We provide professional, same-day medical care wherever you are, ensuring your health remains a priority without the hassle of travel.
Call us now at +44 207 353 5678 to book your appointment or schedule a home visit directly on our website. Take control of your health with the convenience of private GP home visits in London.
Step into the realm of Movember, where the Chevron, the Dali, or the Handlebar becomes more than just a style statement – it’s a symbol of men’s health awareness.
Are you ready to join the Mo-gang and make a statement this Movember?
Movember transcends mere facial hair growth; it’s a global movement dedicated to transforming the landscape of men’s health. This renowned charity, a beacon of hope and change, addresses critical issues like prostate cancer, testicular cancer, and mental health and suicide prevention.
In the heart of London, at Fleet St. Clinic, we’re not just embracing the ‘Mo’ spirit; we’re championing the cause of male health. As the statistics reveal, one man succumbs to prostate cancer every 45 minutes in the UK. It’s time to take charge of your well-being and be part of a movement that’s making a difference.
Prostate Cancer –
Our clinic offers a comprehensive Prostate Cancer check, with an experienced doctor committed to your health journey. This thorough examination includes a detailed health discussion covering lifestyle and family history, an internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Early detection is the key, and we’re here to guide you every step of the way.
Testicular Cancer –
Testicular cancer, the most common cancer among young men in the UK, demands attention. Knowledge is power, and understanding the symptoms can be a lifesaver. A lump or swelling, a heavy scrotum, or discomfort in the testicle or scrotum are health signals not to be ignored. At Fleet St. Clinic, we emphasise the importance of awareness and early detection.
Mental Health –
Let’s break the silence surrounding mental health. The Movember Foundation has spearheaded programs globally, fostering resilience and mental well-being in men. It’s not just about growing a mustache; it’s about cultivating conversations that matter.
Now, let’s talk about your health journey with Fleet Street Clinic’s essential men’s health screenings and medicals.
Medical Health Check (From £425) –
Essential
Review your health with one of our experienced GPs. Benefit from a thorough physical examination and carefully selected health checks and blood tests, including thyroid function.
1 hour appointment with a GP – £425
book online
Executive
Check your health from top to toe, with our more enhanced Executive medical, including an audiometry test to assess your hearing, spirometry tests to assess your lung function, and cancer checks and markers.
1.5 hour appointment with a GP – £675
Executive+
For maximum reassurance and peace of mind, consider our most advanced medical. Benefit from advanced health screenings including a sophisticated cardiac (CaRi-Heart) scan, and a bone density DEXA scan.
3 hour appointment with a GP – £3,950
View our medical health checks in more detail and book online.
Prostate Cancer Check (£175)
Prostate cancer is the most commonly diagnosed cancer in men in the UK. Early diagnosis is crucial.
Our prostate cancer check is carried out by an experienced male GP, who’ll conduct a detailed health discussion, internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Swift courier services ensure timely analysis at our nearby pathology laboratory. Our GP will provide you with full support throughout the process and provide aftercare services and referrals if required.
In a world where ‘strong, silent men’ are rewriting their narrative, Movember beckons. Join us at Fleet St. Clinic, where your health is not just a checkup; it’s a commitment to a longer, healthier life.
Book your Appointment now, and let your Mo make a statement for men’s health in London.
According to Prostate Cancer UK, 1 in 8 men will get prostate cancer in their lifetime and it is the most common cancer in men in the UK.
In 2021, around 52,000 men were diagnosed with prostate cancer in the UK alone and the risk of developing it increases with age, as most cases are diagnosed aged 65 and over.
It’s not uncommon for men find out by complete chance, and often it can be too late when the diagnosis is less treatable. For that reason, it’s essential to understand the symptoms, available tests, and the importance of early detection.
What is the Prostate?
The prostate gland is a small, walnut-sized gland located below the bladder and in front of the rectum in males. It plays a key role in the male reproductive system by producing seminal fluid, which nourishes and helps transport sperm during ejaculation.
As men age, the prostate can undergo changes, including enlargement (benign prostatic hyperplasia) or other conditions, such as prostatitis (inflammation) and prostate cancer.
Regular check-ups and awareness of symptoms are important for prostate health.
What is Prostate Cancer?
Prostate cancer occurs when cells in the prostate gland grow uncontrollably.
An enlarged prostate is very common in men over the age of about 50, but having an enlarged prostate is not the same as having prostate cancer.
Having an enlarged prostate doesn’t increase your risk of getting prostate cancer. But it’s possible to have an enlarged prostate and prostate cancer at the same time.
While many men with prostate cancer may not experience symptoms, early detection is vital for effective treatment.
Symptoms of Prostate Cancer
In its early stages, prostate cancer may not cause noticeable symptoms. However, as the disease progresses, some common symptoms include:
- Needing to urinate more often than usual, especially at night
- Difficulty starting or stopping urination
- Weak or interrupted urine flow
- Painful urination or ejaculation
- A feeling that your bladder hasn’t emptied properly
If prostate cancer breaks out of the prostate (locally advanced prostate cancer) or spreads to other parts of the body (advanced prostate cancer), it can cause other symptoms, including:
- Persistent pain in the lower back, hips, or pelvis
- Unexplained weight loss or fatigue
- Blood in urine or semen
- Problems getting or keeping an erection
If you experience any of these symptoms, it’s crucial to consult a healthcare professional for evaluation.
All these symptoms are usually caused by other things that aren’t prostate cancer. But it’s still a good idea to tell your GP about any symptoms so they can find out what is causing them and make sure you get the right treatment, if you need it.
Who Should Consider a Prostate Screening?
- Men aged 50 and older: if you’re at average risk, starting at 50 is recommended.
- Men aged 45 and older: if you have a higher risk, such as a family history of prostate cancer.
Tests for Prostate Cancer at Fleet Street Clinic
Several tests can help confirm the presence of prostate cancer:
- Prostate-Specific Antigen (PSA) Test: This blood test measures the level of PSA, a substance produced by the prostate gland. Elevated PSA levels can indicate prostate cancer, but they can also be elevated due to benign conditions such as an enlarged prostate. A normal PSA indicates that the chance of a prostate cancer is very low.
- Digital Rectal Exam (DRE): During this exam, a doctor manually examines the prostate for any irregularities or lumps. While this test can help identify abnormalities, it is typically used in conjunction with the PSA test.
Consider booking a GP appointment for either of these Prostate Cancer tests, or for a more comprehensive assessment, opt for our Prostate Cancer Check, which includes both tests.
Factors That Can Cause the PSA to be Falsely Raised
Several factors can cause a false elevation in Prostate-Specific Antigen (PSA) levels, potentially leading to misleading test results. Here are common causes:
- Recent Ejaculation: Sexual activity, especially ejaculation, can elevate PSA levels temporarily. Avoid sexual activity for 24–48 hours before a PSA test.
- Prostate Manipulation: Any recent procedures or physical manipulation, such as a digital rectal exam (DRE) or catheter insertion, can elevate PSA levels. Let your doctor know if you’ve had any recent prostate exams or urological procedures.
- Vigorous Exercise: Activities that put pressure on the prostate, like cycling or horseback riding, can raise PSA levels temporarily. Avoid these activities for a f48 hours before the test.
- Prostate Infections or Urinary Tract Infections (UTIs): These infections can cause inflammation and increase PSA levels. Treat infections and allow recovery before testing.
- Benign Prostatic Hyperplasia (BPH): An enlarged prostate from BPH can raise PSA levels even though it’s not cancerous. Make sure your doctor considers this in the interpretation.
- Certain Medications: Some drugs, like testosterone, can increase PSA levels, while others like finasteride (for hair loss or BPH) can decrease it. Inform your doctor of any medications you’re taking.
Avoiding or managing these factors before a PSA test can help improve the accuracy of the results. Always discuss any concerns with your doctor.
You may need additional tests, as listed below, if your PSA is raised or if there is concern from the examination. We can refer you to specialists who may be available for same-day consultations to provide further evaluation.
- Imaging Tests: Additional imaging tests, such as an MRI or CT scan, may be conducted to visualise the prostate gland.
- Biopsy: If initial tests indicate potential cancer, a biopsy is often performed to confirm the diagnosis. During this procedure, a small sample of prostate tissue is removed and examined under a microscope for cancer cells.
Movember, an organisation focused on raising awareness of men’s health issues, including prostate cancer, emphasises the importance of regular check-ups and understanding one’s own health risks. Their campaigns encourage men to talk openly about health issues, promoting early detection and treatment.
Prostate cancer is a serious health concern for men, but awareness and early detection can lead to better outcomes. Regular check-ups and understanding the symptoms are essential steps in addressing this disease.
If you have concerns about prostate cancer or related symptoms, don’t hesitate to seek medical advice by booking a GP appointment. Early action can make a significant difference in your health and well-being.
Related services at Fleet Street Clinic
Prostate Cancer Check
Private GP Appointments
Annual Medical
Blood Tests
October is Breast Cancer Awareness Month
You may notice an increased amount of pink during this month, especially iconic pink ribbons, and it’s for a good reason: October is Breast Cancer Awareness Month.
This annual campaign aims to increase the awareness of the disease and to raise funds for research into its cause, prevention, diagnosis and treatment. With the hope that in the not too distant future, a cure will be found!
Breast Cancer is the most common cancer in the UK. 1 in 8 women in the UK will be diagnosed at some point in their lives.
In the UK, over 55,000 women each year are diagnosed with Breast Cancer which is the most common cancer. Thanks to research, more people are surviving breast cancer than ever before, yet there are still nearly 1,000 women who’ll die of breast cancer each month. Breast cancer is often thought of as something that only affects women, but men can get it in rare cases. It is important for males (especially those over 75 years with a high BMI) to check breast tissue for abnormalities as well.
We will be sharing important information on symptoms, causes and lifestyle alteration you can make to reduce your risk.
We are urging everyone, especially women, to check their breasts regularly and get checked out by a professional if something seems unusual for you.
REMEMBER: The earlier breast cancer is diagnosed, the easier it is to treat and the better the chance of successful treatment.
BREAST CANCER SYMPTOMS TO LOOK OUT FOR:
- a new lump or thickening in your breast, upper chest area or armpit
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
- Unexplained pain in your breast or armpit that’s there all or almost all the time
How to check your breasts
Checking your breasts yourself means you’ll get to know what is “normal” for you. As a society we are probably not that familiar with how our body currently is and so that makes it difficult to know what subtle changes happen. It’s most likely that unless a dramatic change has occurred a subtle change will go unnoticed.
So, how do you check your breasts?
There is no special technique and you don’t need any training to start checking your breasts. It may feel like you’re unsure what you’re doing but get to know your body and any breast check is better than no breast check.
The easiest and most accurate way is to divide the breasts into four quadrants; the upper outer quadrant, outer lower quadrant, inner lower quadrant and inner upper quadrant. Examine each quadrant with the flat of your hand. It is important to do this regularly so that you are familiar with what each breast feels like normally. That way, should you notice any changes, (hopefully not), you will pick them up straight away and changes won’t go unnoticed. It is important to remember to check your armpits as well. It is surprising how many breast lumps are discovered after an “axillary” or armpit lymph node is found and checked.
Breast Cancer Now advises the TLC method – “touch, look and check”.
Touch: Can you feel anything new or unusual?
Look: Does anything look different?
Check: Any changes with your GP
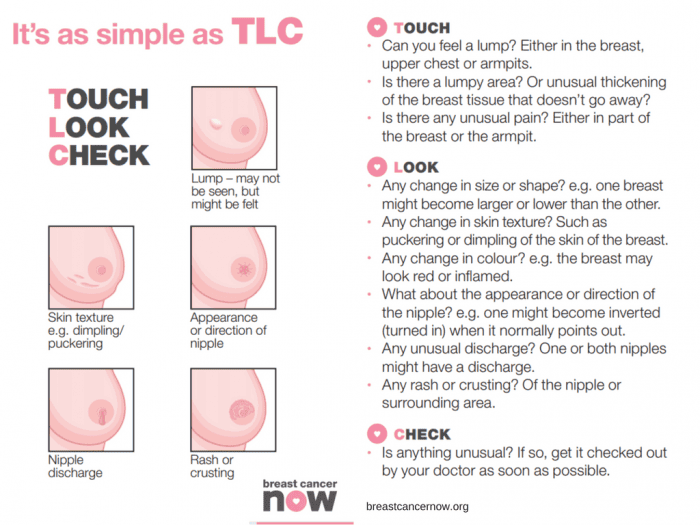
You should check your breasts Regularly
Get to know your “normal” by checking your breasts regularly. Get in the habit of checking your breasts at least every month. It can be easier whilst in the bath or shower.
Your breasts can change throughout your life for many reasons – like the menopause, pregnancy and breastfeeding, or puberty. So, if you check them regularly, you’ll be able to spot any new or unusual changes that should be checked out by a GP.
For young and pre-menopausal women it is advised to check mid-cycle (a week after their period finishes) if there are any changes this requires checking with your GP.
As older women are of a higher risk of breast cancer, due to age, it is advised they check even more frequently. Older women should check on a monthly basis without exception. It is advised for men to check also.
Any lump requires attention and checking with your GP immediately.
In addition to regular self-checks, it is important to never miss a mammogram appointment. They may be painful and momentarily uncomfortable, but a mammogram can save your life. If you have a long wait for a mammogram, are unable to access an appointment or just want an additional check, contact the Fleet Street Clinic and we should be pleased to help.
What are the causes of breast cancer?
There are several factors that contribute to increasing your risk of developing breast cancer. There is no single cause, and has to do with our lifestyle, environment and genetics. There are factors which we simply cannot control such as getting older, family history, inherited genes, dense breast tissue, hormones and age at which period started and stopped. However, there are some lifestyle choices that if altered can reduce your risk of breast cancer.
Lifestyle change that will reduce your risk of breast cancer
1. Your weight
Being overweight or obese has a high risk of breast cancer in both men and women (especially after menopause). You can work out your ideal weight using a BMI (Body Mass Index) calculator, this checks your height and weight to see if you are at a healthy weight. For the majority of adults an ideal BMI ranges from 18.5 to 24.9. A BMI between 25 – 30 means overweight. Obesity means a BMI of 30 and above.
2. How much alcohol you drink
Alcohol consumption increases the risk of breast cancer. The risk is greater with each extra unit per day, the latest UK guidelines state no more than 14 units a week.
3. How much exercise you do
Being inactive contributes to a small increased risk of breast cancer, this qualifies as doing less than 150min of moderate activity on a weekly basis. This does not necessarily mean sport and exercise, anything that makes you warmer and out of breath counts.
Throughout October we’ll be highlighting the reasons to support this campaign across our social media platforms. We will be sharing inspirational stories from those who have survived the disease and those who are currently battling. We will also hear from those who have supported a suffering loved one during treatment. Sharing these stories humanises the disease and can provide support/tips for those who may be struggling with a current diagnosis. We will be sharing ways of checking for early warning signs. We’ll also be encouraging all to undertake a Well-Woman or Well-Man health checks. Both of which contain a breast examination.
At Fleet Street Clinic, we specialise in women’s health and have four female GPs on-site to facilitate well-woman health checks. Our Executive Well Woman medical is focused on protecting your well-being and involves a full examination including breast examinations and cervical screen tests. Our comprehensive medical is designed to screen for health problems at the earliest possible stage.
Book Your Well Woman Medical Online. Or if you notice any changes to your breast or have any concerns, you should book a GP appointment as soon as possible.
_______________
To find out more from Breast Cancer Now, visit breastcancernow.org
Women between the ages of 25 and 64 are invited for regular cervical screenings where a healthcare professional looks at the health of the cervix to detect any cell changes or abnormalities. However, in 2022-2023, the number of women who attended their cervical screen fell. Nearly a third of the women invited to do their cervical screen didn’t attend their appointments, this is around 4.6 million women, a deeply concerning number, as over 3000 women are diagnosed with cervical cancer each year and 99.8% of those cases are preventable. Prevention is better than curing, and the earlier you are aware of any cell changes, the easier it is to treat.
Why do some women not attend their cervical screenings?
One of our general practitioners, Dr Belinda Griffiths, has found that in her experience women don’t attend their cervical screenings for a number of reasons including: difficulties with taking time off work for a GP appointment, fear of embarrassment, and fear of the process being uncomfortable or painful.
However, to combat these concerns, the NHS has launched at-home HPV kits. Dr Griffiths explains how they work – “The HPV test is highly sensitive so it separates out those who are HPV-positive and HPV-negative. Those who are HPV-negative will be considered ‘low risk’ for cervical cancer and will be asked to do a future test. Those who are HPV-positive will be deemed ‘high risk’ and be asked to attend for follow-up with a clinician whereby they will conduct a cervical screening to check the health of their cervix and investigate if any abnormal cells are present.”
These new tests are the same process as at-home STI tests whereby a simple swab collects the sample from the vagina. Having the option of this sort of test at home removes the fear some women may have surrounding the slightly more intrusive cervical screen.
What is HPV?
HPV (human papillomavirus) is a common virus passed on via skin-to-skin contact, usually through genital contact. There are many types of HPV, most of which are harmless, don’t usually cause any symptoms and the infection will go away on its own. However, others are deemed ‘high risk’ as they can persist and cause cell changes which can lead to cancer. It is thought that these ‘high risk’ HPV strains are responsible for around 80% of cervical cancer cases, making the detection of HPV all the more important.
How can you prevent HPV?
You can be protected from certain HPV strains through vaccination. There are two HPV vaccines currently available in the UK: Gardasil which protects against 4 strains of HPV used in the NHS and the vaccine used here at the Fleet Street Clinic, Gardasil-9, which protects against 9 of the high-risk HPV strains.
When can you be vaccinated against HPV?
The NHS now routinely offers the Gardasil vaccine to girls and boys around age 12/13, before the age people generally become sexually active. However, the vaccination programme only came into full force in 2019, meaning many people are currently unvaccinated. It should be pointed out that adults can get vaccinated at any age and even if you have already been exposed to HPV, the vaccine can still offer protection against other strains to which you have not yet been exposed.
It is a particularly good idea for people to get vaccinated before they attend university or before they go travelling on a ‘gap year’, as these are typically times where young people are more sexually active and therefore more likely to be exposed to HPV.
It is important to note that getting the HPV vaccination most certainly doesn’t mean missing or not participating in HPV tests or cervical screenings. A combination of these preventative measures gives you the highest possible chance of preventing cervical cancer.
Book your Cervical Screen or HPV vaccine online today.
What to do if you think your child has measles and when to keep them off school.
Measles cases are increasing throughout England, particularly among children. This highly contagious infection can lead to severe complications for some individuals.
Since there is no specific medical treatment for measles, obtaining vaccination is crucial for the best defence against serious illness. The measles, mumps, and rubella (MMR) vaccine is part of routine childhood vaccinations, meaning most children are already immunised against measles.
If your child has received both doses of the vaccine, it is unlikely that they will contract the virus.
Here, we’ll provide everything you need to know about measles, from ensuring your child’s vaccination to knowing when to keep them away from school.
What are the symptoms of measles?
Measles usually starts with cold-like symptoms, followed by a rash a few days later. Some people may also get small spots in their mouth.
Symptoms of measles usually start to appear 7-14 days after you become infected, which include:
- Runny/blocked nose
- Sneezing
- High temperature
- Sore, red eyes that may be sensitive to light
- Sore throat
- White spots inside the mouth
What does a measles rash look like?
Measles usually begins as flat red spots that appear on the face at the hairline and spread downward to the neck, body, arms, legs, and feet. Small, raised bumps may also appear on top of the flat red spots. The spots may become joined together as they spread from the head to the rest of the body.
What should you do if you think your child has measles?
If you suspect that you or your child might have measles, it’s important to request an immediate GP appointment or seek assistance from NHS 111.
Before visiting the GP or any healthcare facility, make sure to call ahead for guidance.
In the event of a measles diagnosis for your child by a doctor, it is advisable for them to refrain from attending nursery or school for a minimum of 4 days from the onset of the rash. Additionally, they should steer clear of close interactions with infants and individuals who are pregnant or have compromised immune systems.
What is the best way to protect against measles?
The best protection against measles for children and adults is to get both doses of the MMR vaccine.
MMR vaccination is available at Fleet Street Clinic for children and adults who would like catch-up on doses. If you or your child haven’t been vaccinated yet, or have an unfinished course of vaccines, either book an appointment online or contact our reception team on +44 20 7353 5678 to book an appointment.
We can usually accommodate same day appointments.
Alternatively, children receive the vaccine at no cost on the NHS at 12 months and then a second dose at 3 years and 4 months. You may find the NHS vaccination service has a longer wait time that us.
If you prefer a version of the MMR vaccine without pork products, please get in touch, explaining your preference and we will do our best to accommodate. It’s important to note that we would be ordering this product specially for you, so there may be a longer wait time for delivery and prepayment will be required. Either call our reception team on +44 20 7353 5678 or email info@fleetstreetclinic.com
Cold-like symptoms can be an early sign of measles. Should you still send your child to school?
If your child has been vaccinated, it’s very unlikely that they have measles. Check if they have a high temperature or a fever, and if not, we’d advise it’s fine to send your child to school.
Keep an eye on their symptoms and adapt accordingly if they worsen.
When should you keep your child off school or nursery and how long for?
If your child has measles, they should stay off nursery or school for at least 4 days from when the rash first appears and avoid close contact with babies and anyone who is pregnant or has a weakened immune system.
The school will let you know if your child has been in contact with someone who has measles and advise what you need to do.
They may advise people who are more susceptible to contracting the virus, such as unvaccinated siblings to stay away from school for the incubation period to be on the safe side.
The incubation period is the length of time it can take to develop the illness after being in contact with someone with measles. For measles, the incubation period can be up to 21 days.
Anyone, child or adult, who has been vaccinated is unlikely to be considered susceptible.
If you’re not sure whether your child is due a vaccination or has missed a vaccination, you can check their Red Book or contact your registered GP practice for confirmation.
If your child has missed their first or second dose of the MMR vaccine, we’d advise you book an appointment for catch up vaccines. You can book an appointment online.
Should you keep your child off school if another pupil has been diagnosed with measles?
Most children will be protected against measles and there is no need to keep your child off school if they have had both their MMR vaccinations.
Your school will let you know if your child has been in contact with someone with confirmed measles and will advise what the next steps are.
Can I still get my child vaccinated even if they’re older?
Yes. The MMR vaccine is suitable for adults and children, therefore, anyone who has not had 2 doses of the MMR vaccine can book an appointment for catch up vaccinations.
It’s best to have vaccines on time, but you can still catch up on most vaccines if you miss them. Two doses of the vaccine are needed to ensure full protection.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Related Blogs:
Measles outbreak & isolation warning
Blue Monday happens every year on the third Monday of January. It is supposedly the most depressing day of the entire year, based on a crude calculation of bad weather, long nights, back to work dread and post-Christmas debt.
It does sound very plausible perhaps because we so familiar with the term “January Blues” but Blue Monday is in fact, a myth!
The phrase “Blue Monday” was coined by Sky Travel back in 2005 as a way to encourage people to book their next holiday as something to look forward too. They highlighted all the seasonal negatives to reinforce the benefits of booking a holiday – a clever marketing trick.
But can we really pinpoint the most depressing day of the year?
There is no actual scientific studies that have ever backed up any claims about Blue Monday being true or that there could even be a “most depressing day of the year”. This does make sense because this would be different for each and every one of us based on personal circumstances and the variables are extensive. It did, however, get use thinking about our mood, mental health and overall wellbeing at this time of year.
January is cold, often wet and everyone is trying to shake off the Christmas comedown and get excited about the new year ahead, but the January blues can creep in.
Remember you are not alone, and many people experience a dip in mood this time of year but it is important to identify when the January blues are actually symptoms of depression.
Depression is more than simply feeling unhappy, fed up or low for a few days. It can be long lasting and the symptoms range from mild to severe. Once accessed by a doctor, they will conclude the severity of your depression.
A simplified description follows:
Mild depression will have some impact on your daily life.
Moderate depression has a significant impact on your life.
Severe depression makes it almost impossible to get through daily life.
Sometimes there’s a trigger for depression. Life-changing events, such as bereavement, losing your job or giving birth, can bring it on. Other times, it can be linked with family history; people with family members who have depression are more likely to experience it themselves. But you can also become depressed for no obvious reason. It is quite complex and each person is unique.
There are many symptoms of depression and the combination is unpredictable.
They can be categorised at physiological, physical and social symptoms.
Some examples of psychological symptoms of depression include:
- continuous low mood or sadness
- feeling hopeless and helpless
- having low self-esteem
- feeling tearful
- feeling irritable and intolerant of others
- having no motivation or interest in things
- finding it difficult to make decisions
- not getting any enjoyment out of life
- feeling anxious or worried
- having suicidal thoughts or thoughts of harming yourself
Some examples of physical symptoms of depression include:
- moving or speaking slower than usual
- changes in appetite or weight (usually decreased, but sometimes increased)
- constipation
- unexplained aches and pains
- lack of energy
- low sex drive
- changes to your menstrual cycle
- disturbed sleep – for example, finding it difficult to fall asleep at night or waking up very early in the morning
Some examples of social symptoms of depression include:
- avoiding contact with friends and taking part in fewer social activities
- neglecting your hobbies and interests
- having difficulties in your home, work or family life
The most common symptoms of depression tend to be a low mood, feelings of hopelessness, low self-esteem, lack of energy, problems with sleep and a loss of interest in things you used to enjoy but it can be any number of symptoms listed above.
It’s important to seek help from a GP if you think you may be depressed. The sooner you see a doctor, the sooner you can be on the way to recovery.
For more information on GP services at Fleet Street Clinic, click here.
With every change of season comes a host of different medical issues, and winter can be one of the worst. With colder temperatures, shorter days, and seasonal illnesses circulating, it is one of the harder seasons to keep fit and healthy. There are certain conditions which are known to worsen in the colder months and so it is important to be aware of them and how you can best prepare yourself to keep healthy throughout winter.
These conditions include:
- Asthma
- COPD
- Circulatory disorders, such as claudication, Raynaud’s disease, and chilblains
- Ischaemic heart disease
- Hypothyroidism (if untreated)
- Osteoarthritis and any joint disorder to include rheumatoid arthritis
- Seasonal Affective disorder
- Allergic rhinitis
To reduce the increased risk associated with the above conditions, it is important to have a check up with your GP, ideally in the early Autumn before the Winter months. This will give you the best chance of getting ahead and allowing you to prepare for the coming season. But, if for whatever reason, you were unable to have a check up in Autumn, it is still beneficial to have a check up during the Winter months.
During a check up for asthma and COPD it’s advised to have a peak flow and lung function check. Asthma and COPD are worse in the dry, cold weather, so it is important to make sure you have plenty of your prescribed inhalers. It is best to be prepared rather than be taken unawares by an attack of wheezing. It is extremely important to see a doctor if you develop winter wheezing and are short of breath, especially during the night as this is when asthma and COPD attacks are most dangerous.
Circulatory disorders are worse in the cold weather as lower temperatures constrict blood vessels, increasing the likelihood of pain due to claudication (pain in the calves after walking a certain distance), Reynaud’s (discolouration of the fingertips due to constriction of the blood vessels) and chilblains (small, itchy, red patches on the skin). You can prepare for all of these conditions by obtaining prescriptions for treatment but most importantly, by keeping warm and preparing for the cold.
Ischaemic heart disease is also worse in the cold weather due to the effect of constricting blood vessels. It is important to have a cardiac check to include blood pressure, and if you suffer from angina, to ensure you have the medication to treat this painful condition which is likely to be much worse in the cold weather. Avoiding the extreme cold and wearing thermal clothing may also mitigate against the likelihood of a heart attack or myocardial infarction if you do suffer from Ischaemic heart disease.
If you suffer from Hypothyroidism, it is a good idea to have an annual blood test. Left untreated, hypothyroidism can cause increased sensitivity to cold, which can be particularly unpleasant in winter.
For those with arthritis of any kind, the best way to avoid pain and stiffness in the joints is to keep warm and keep the joints moving. Find more information on Arthritis in Winter here.
If your mood tends to be lower in the winter months, each year, you should have a check up with your GP to discuss Seasonal Affective Disorder (SAD). If you are diagnosed with SAD, consider CBT (Cognitive Behavioural Therapy) rather than medication if you can, and invest in a daylight lamp as these do help.
Allergic rhinitis is another ailment that tends to crop up a lot around winter time. This is diagnosed when you have a persistent nasal discharge. This can occur either as a result of pine or autumnal tree leaf mould, or due to house dust or mould which is often exacerbated by central heating. In this instance, nasal sprays and antihistamines are often required.
Finally, the Norovirus peaks in November until April. This is a really unpleasant vomiting virus which is picked up from contaminated surfaces or foods. To help avoid this nasty bug, always wash hands when handling food and make sure food is washed thoroughly before cooking or eating raw.
If you know or suspect that you might suffer from any of these conditions, please do visit your GP to help you keep prepared. Similarly, if anything new arises you should see your GP as soon as you can; the earlier a health condition is addressed, the easier it is to treat.
In general, an annual medical is a good way to give you a full-body overview of your health, as well as monitor the progression of any existing health conditions. A varied, balanced diet and regular exercise will also be crucial in keeping you generally fit and healthy throughout winter.
For more information on our GP Services.
Book a GP Appointment or an Annual Medical.
Arthritis is a common condition that causes pain and inflammation in joints. It is not a single disease but an informal way of referring to joint pain or joint disease. There are more than 100 types of arthritis and related conditions. There are thought to be 10 million people with some form of arthritis in the UK. It is the most common cause of disability in the UK and can affect people of all ages but it does occur more frequently as people get older.
Common arthritis joint symptoms include swelling, pain, stiffness and decreased range of motion. Symptoms can range dramatically from person to person, with some experiencing mild symptoms with occasional flare ups to those who experience constant debilitating pain everyday. The sad truth is that there is no cure for arthritis, so it is all about pain management and how to best reduce flare ups.
The impact of the weather on the symptoms of arthritis has been debated for many years and people tend to report more arthritis flare-ups in the winter, but the reason why is not specifically known.
Quite often sufferers will state that their symptoms get worse when the weather is damp and cold and some state they are able to tell when the weather is about to change based on their arteritis symptoms worsening.
Even if there is currently nothing to support this scientifically, this doesn’t remove the pain felt by sufferers and so rather than comment on where this is true or not, let’s look at ways to reduce flare ups in winter.
Our top 4 tips:
1. Stay warm
When the temperature drops both inside and outside, dress warmly. Make sure all arthritis prone areas are kept warm.
2. Stay hydrated
Drink plenty of water throughout the day. Even mild dehydration might make you more sensitive to pain.
3. Take warm baths
A warm bath or visiting a heated swimming pool will ease joint pain and comfort you. If you visit a heated swimming pool, gentle exercise will also help your mobility.
4. Stay active
It is now clear that active people experience less joint pain than those who are sedentary. If you are experiencing an arthritic flare then reduce your usual activity (but don’t stop altogether) and use simple anti-inflammatory medication such as ibuprofen if it is safe for you to do so.
Enjoy winter while taking the above precautions for Arthritis.
If you are facing extreme discomfort and pain in your joints due to arthritis, book an appointment with a GP to discuss your options.
RSV is a common and highly contagious respiratory virus that is a leading cause of lung disease. RSV is seasonal, and like other respiratory viruses, its peak incidence is during the winter months each year. It spreads from person to person via droplets, or from infected surfaces or objects. RSV is a virus, so antibiotics are not effective.
Arexvy is a new vaccination designed to protect against lower respiratory tract disease caused by respiratory syncytial virus (RSV). It is an important advance, because no specific treatment for RSV is available, and infection is often severe.
Older adults, and those with underlying medical conditions such as diabetes, heart disease and lung diseases such as asthma and COPD are at the greatest risk of the infection. RSV can exacerbate these underlying conditions and lead to pneumonia.
In the UK, RSV causes more hospitalisations and deaths than flu in those over the age of 60. It is estimated that RSV causes14,000 hospitalisations and an estimated 8,000 deaths in adults 60 years of age and older each year.
Arexvy is a recombinant adjuvanted vaccine for the prevention of RSV is adults 60 years of age and above. It is the only licensed vaccination in the UK that has been authorised for use by the Medicines and Healthcare products Regulatory Agency, meaning at risk adults are now able to be vaccinated against the disease.
Arexvy is as in inactive vaccination and only requires single dose for protection. It can be administered at the same time as other vaccinations including flu, pneumococcal, and COVID.
We are among the first practices in the UK to offer it to adults needing protection.
Ovarian cancer is a disease that affects thousands of women worldwide each year and is often referred to as the silent killer due to its silent symptoms, including bloating, abdominal pain, and changes in bowel habits, which are often mistaken for other conditions. Despite advances in treatment, the disease remains a major public health concern due to its high mortality rate. However, new data from a study funded by Cancer Research UK (CRUK) suggests that a seemingly unlikely tool – supermarket loyalty card surveillance – could help spot ovarian cancer early, when it is most treatable.
The study, which was published in JMIR Public Health and Surveillance, analysed data from supermarket loyalty card programs and found that changes in purchasing behaviour could be used to detect early signs of ovarian cancer.
Researchers found that women with ovarian cancer often experience a decline in their appetite and energy levels, which can result in changes in their grocery shopping habits. By monitoring these changes in real-time, it may be possible to detect the disease early and improve the chances of successful treatment.
This is an exciting development in the fight against ovarian cancer, and one that has the potential to revolutionise the way we detect and treat the disease. By leveraging the vast amounts of data generated by supermarket card programs, healthcare providers and public health officials could identify women who may be at risk of ovarian cancer and encourage them to seek early medical attention. This could help to improve the outcomes of treatment and reduce the overall impact of the disease on society.
One of the key benefits of supermarket card surveillance is that it allows for continuous monitoring of women’s purchasing behaviour. This means that healthcare providers can receive real-time alerts when changes occur, allowing them to act quickly and effectively. This level of monitoring is not possible with traditional screening methods, which are typically performed only once or twice per year and may miss early signs of the disease.
Additionally, supermarket card surveillance is a cost-effective way to monitor the population for signs of ovarian cancer. Unlike other screening methods, it does not require specialised equipment or trained personnel, and the cost of monitoring is negligible compared to the cost of treatment. This could make it possible to implement large-scale screening programs, even in resource-limited settings, and reach a greater number of women who may be at risk of ovarian cancer.
Of course, it’s important to keep in mind that supermarket card surveillance is not a substitute for traditional screening methods, such as ultrasound or CA-125 tests, or for regular self-reporting and awareness of symptoms. However, it could be used as an adjunct to these methods, helping to improve the accuracy of screening and reduce the number of missed cases.
Another important consideration is the privacy of women whose purchasing behaviour is being monitored. While supermarket card surveillance has the potential to help detect ovarian cancer early, it is important to ensure that women’s privacy is protected and that the data collected is used only for medical purposes. Healthcare providers and public health officials should work together to ensure that any monitoring programs are transparent, secure, and in compliance with privacy regulations.
In conclusion, the findings of this study are a major step forward in the fight against ovarian cancer. By leveraging supermarket card surveillance, it may be possible to detect the disease early, when it is most treatable, and improve the outcomes of treatment for women around the world. However, it is important to carefully consider the privacy implications of monitoring purchasing behaviour and to ensure that any programs implemented are transparent, secure, and in compliance with privacy regulations. The early detection of ovarian cancer is a critical goal, and we hope that this research will help to pave the way for new and innovative approaches to screening and treatment. Additionally, women should be encouraged to seek medical attention if they notice any changes.
Reference Source: https://publichealth.jmir.org/2023/1/e41762
Related services available at Fleet Street Clinic:
Statins are a widely prescribed class of drugs used to lower cholesterol levels and prevent cardiovascular events such as heart disease and strokes. The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
This decision was made after the independent committee updating the NICE guideline on cardiovascular disease (CVD) risk assessment and reduction considered new evidence on the safety and side effects of statins, meaning more people could be given them.
The draft guideline recommends that doctors should consider statins for people who haven’t had a CVD event (called ‘primary prevention’) with a 10-year CVD risk score of less than 10%. The committee agreed that if more people took statins there would be a greater reduction in the incidence of heart disease and strokes.
In addition to being prescribed by National Health Service GP’s, statins can also be prescribed by private healthcare providers, such as us, Fleet Street Clinic. In fact, private GP’s can play an important role in the management of cardiovascular disease risk by offering statins as part of a comprehensive treatment plan for patients at high risk.
People can be at risk from CVD because of factors they cannot change including their age, sex, ethnicity and family history but it’s important to note that certain lifestyle changes can reduce the risk. These include stopping smoking, reducing alcohol consumption, introducing or increasing exercise and eating a healthy diet.
Therefore, the decision to take a statin should be made in consultation with a healthcare professional and should take into account the individual’s values and priorities as well as the potential risks and benefits of treatment.
With the British Heart Foundation noting that “there are around 7.6 million people living with heart and circulatory diseases in the UK” and that they “estimate that in the UK more than half of us will get a heart or circulatory condition in our lifetime” this is likely to be an impactful change in the landscape of CVD and statins.
To conclude, Paul Chrisp, director of the Centre for Guidelines at NICE, said:
“What we’re saying is that, for people with a less than 10% risk over 10 years of a first heart attack or stroke, the decision to take a statin should be left to individual patients after an informed discussion of benefits and risks.
“The evidence is clear, in our view, that for people with a risk of 10% or less over 10 years, statins are an appropriate choice to reduce that risk.
“We are not advocating that statins are used alone. The draft guideline continues to say that it is only if lifestyle changes on their own are not sufficient, and that other risk factors such as hypertension are also managed, that people who are still at risk can be offered the opportunity to use a statin, if they want to. They don’t have to, and their decision should be informed by an understanding of the risks and tailored to their values and priorities.”
Reference Source: https://www.nice.org.uk/guidance/indevelopment/gid-ng10178/documents
Related services available at Fleet Street Clinic:
Sleep plays a crucial role in maintaining overall health and well-being, and recent research has revealed a strong link between sleep and cardiovascular health. A study conducted by the University of Warwick in the UK found that individuals who get 7-9 hours of sleep per night have a lower risk of cardiovascular disease (CVD) and mortality compared to those who sleep less or more than the recommended range.
The study, published in the Journal of the American College of Cardiology, analysed data from over 116,000 participants in the UK Biobank study and found that those who slept less than 6 hours or more than 9 hours had a higher risk of CVD and mortality. These findings add to the growing body of evidence that suggests a link between sleep duration and cardiovascular health.
The exact mechanisms by which sleep affects cardiovascular health are not fully understood, but researchers suggest that it may be related to the impact of sleep on cardiovascular regulation, inflammation, and metabolic function.
It is important to prioritize sleep and aim for the recommended range of 7-9 hours to maintain cardiovascular health.
It’s worth noting that these findings are observational, and more research is needed to fully understand the relationship between sleep and cardiovascular health, but it’s a good indication that sleep plays a vital role in maintaining a healthy cardiovascular system.
To read the full study, continue reading here:
medscape.co.uk – Does sleep duration influence cvd and mortality risk?
Related services available at Fleet Street Clinic:
Mental Health Awareness Week: What Is Stress?
Look around your office, do you know if anyone is struggling?
You may think those around you – fellow colleagues or your staff – are completely fine. But mental health affects us all and problems in the workplace are actually very common.
According to mental health charity Mind, at least one in six workers are experiencing common mental health problems, including anxiety and depression.
Nowadays, there is increasing recognition of stress and mental health problems, both within the workplace and in everyday life. Currently, following Stress Awareness Month in April, we are approaching Mental Health Awareness Week, which takes place from 13-19th May.
We thought it might be helpful to focus on some positive strategies to help, in terms of stress management and resilience. Whilst being particularly useful and relevant within the workplace, these can all be used in everyday life as well.
WHAT IS STRESS?
In its purest form, stress is the body’s reaction to something it perceives as dangerous or threatening. When we feel under attack, our bodies respond by producing a mixture of hormones such as adrenaline and cortisol. These prepare us for physical action by diverting blood away from our core and into our limbs. It also temporarily shuts down some less vital bodily functions such as digestion.
For immediate, short-term situations, stress can be beneficial to your health, by helping you cope with potentially serious situations.
Yet if your stress response continues, and stress levels stay elevated far longer than necessary, it can take a toll on your health.
WHY IS IT IMPORTANT TO TACKLE STRESS?
Chronic stress can cause a variety of symptoms, contribute to many health problems (such as high blood pressure, heart disease, obesity and diabetes, anxiety and depression) and affect your overall well-being.
Reducing stress can help prevent these harmful effects on both mind and body.
Looking after yourself and ensuring you have good mental health has many benefits – not just for you as an individual, but for the business too. Employees are generally more productive, passionate and motivated when in good health. Even if they’re experiencing mental health problems, knowing they are supported by their employer can help in the recovery process.
STRESS PREVENTION IS BETTER THAN STRESS MANAGEMENT
Ultimately, the best way to manage stress is through prevention rather than cure.
Research shows that those who are better informed about the practical ways in which they can lower their stress levels are far better able to tackle difficult situations with emotional resilience and determination.
Within the workplace, employers are encouraged to make promoting the wellbeing of their employees a core element of the company’s internal operations. Some examples of a proactive approach to stress-management might be:
- To invite people to take active breaks away from their desks
- Offering lunchtime yoga classes or mindfulness sessions
- Group walks in the fresh air.
So what can help you reduce stress? Continue reading our stress, with Our Top Tips For Reducing Stress.
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch. Or if you are an individual who needs help with stress management, you can book a GP appointment online.
Feeling stressed?
Everyone feels stressed from time to time. In small doses, stress can actually be quite useful; motivating us to achieve our goals. But for some, stress is chronic. Meaning it is debilitating and negatively impacts their mood, their health and wellbeing, their relationships and their work.
Experiencing a lot of stress over a long period of time can also lead to a feeling of physical, mental and emotional exhaustion, often called burnout. It is, therefore, easy to see why reducing stress across all areas of your life would be important. Stress management tips are a good place to start.
Learning how to manage your stress takes practice and time.
Here are our top 10 ways on managing and reducing stress.
10 TIPS TO REDUCE STRESS:
-
Prioritise your health
– make decisions which will benefit your physical, mental and emotional wellbeing. For example, go alcohol-free a few nights each week or allow yourself time for a hobby you enjoy. These small steps for a healthier lifestyle will help in reducing stress levels.
-
Get a good night’s sleep (regularly)
– research clearly shows that sleep deprivation amplifies the symptoms associated with stress. Aim for between 7-9 hours of good quality sleep every night.
-
Practice deep breathing
– when our bodies are stressed, the muscles that help us breathe tighten. By focussing on taking several deep breaths we can quickly and effectively relieve physical symptoms associated with feeling stressed or anxious. Try to do this regularly throughout the day.
-
Drink enough water
– being dehydrated (however mild) causes our cortisol levels to rise, which automatically makes us feel stressed. Your body is already dehydrated if you’re feeling thirsty. So try to avoid reaching this point by hydrating yourself regularly. Aim for 2-3 litres per day, more in hot weather or when exercising.
-
Eat a balanced diet
– dieticians stress how certain foods have stress-relieving properties. For example, dark chocolate is rich in antioxidants, whilst avocados and oily fish are high in omega-3 fatty acids (both of which are proven to help lower anxiety levels).
-
Exercise regularly
– physical activity causes our brains to release mood-improving chemicals called endorphins. These help us to cope with potentially challenging situations. Both Public Health England and the World Health Organisation recommend at least 150 minutes of moderate intensity physical activity each week, in bouts of 10 minutes or more. Choose activities you enjoy to achieve maximum benefit for the mind as well as the body.
-
Adopt a positive mindset
– research suggests that making a conscious effort to think positively can help protect us against a whole host of physical and mental issues, including stress.
-
Manage your time and tasks effectively
– by giving ourselves enough time in which to complete a given task, and by making sure that we don’t try and accomplish too many stressful things at once, we can reduce the likelihood of feeling overwhelmed.
-
Spend less time online
– many studies have found a strong positive correlation between internet usage and stress levels. Spending less time on our computers and phones is a simple way to practice self-care. Having screen-free time for at least an hour before bedtime has also been shown to improve sleep.
-
Learn to say no
– in a culture that demands we take on more and more responsibilities, having the confidence to say “no” will only become more important. This final tip takes us back to the start, by reiterating the importance of prioritising our health above unrealistic social pressures, and brings us onto developing an essential tool – resilience.
Continue reading about Resilience or read What is Stress?
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch.
Or if you are an individual who needs help managing stress, you can book a GP appointment online. Our doctors will be able to talk through your thoughts, symptoms and emotions and set you on the right path to diagnosis. They will also be able to recommend relevant support services for stress, if appropriate.
Mental Health Awareness Week: Resilience
WHAT IS RESILIENCE?
Resilience is the ability to recover from adversity, hardships, or significant sources of stress.
It means “bouncing back” from difficult experiences, feeling stronger and more capable to cope than before. With life becoming more stressful than ever, it is an important skill to develop which can make a big difference between surviving and thriving within work and general life.
HOW RESILIENT AM I?
Research has shown that resilience is ordinary, not extraordinary, and is not simply a trait we either have or do not have.
So here’s the good news! Resilience can be developed. It involves behaviours, thoughts and actions which can be learned and developed in anyone.
SO HOW CAN I DEVELOP RESILIENCE?
Many studies show that the primary factor in developing resilience is having caring and supportive relationships within and outside the family, including at work. Relationships fostering trust, provide role models and offer encouragement and reassurance help bolster resilience.
Several additional factors are associated with resilience, including:
- The capacity to make realistic plans and take steps to carry them out.
- A positive view of yourself and confidence in your strengths and abilities.
- Skills in communication and problem-solving.
- The capacity to manage strong feelings and impulses.
These are all factors you can develop in yourself, and which can be fostered within the work environment by employers taking an active interest in employees’ wellbeing.
TOP TIPS FOR DEVELOPING RESILIENCE
Here are a few things you could try, to develop your resilience.
Please don’t feel you need to tackle them all at once – trying one or two at a time may be enough to make a big difference!
1) Create connections
– good relationships with family, friends and colleagues are crucial. Accepting help and support from those who will listen to and care about you strengthens resilience. Assisting others in their time of need can benefit you in return.
2) Accept that change is fundamentally part of living
– accepting circumstances that cannot be changed can help you deal with these more effectively whilst focussing on circumstances that you can alter.
3) Avoid seeing stressful events as insurmountable problems
– try to look beyond the present towards how future circumstances may be a little better. Take note of any subtle ways in which you might already feel better as you deal with difficult situations – signs of good progress.
4) Take decisive action
– this can assist you in giving some control over your response to challenging situations
5) Pursue your goals
– making them small but achievable and most importantly realistic. Each day, ask yourself “What’s one thing I know I can accomplish today which will help me move in the direction I want to go? Take baby steps in the right direction!
6) Nurture a positive outlook
– developing confidence in your ability to solve problems and trusting your instincts helps build resilience.
7) Keep things in perspective
– retaining an optimistic outlook and visualising what you want, rather than worrying about what you don’t want, can all help the brain engage with this.
8) Practice mindfulness and meditation
– Mindfulness means paying more attention to the present moment – to your own thoughts and feelings, and to the world around you. Meditation involves the use of techniques such as mindfulness to train attention and awareness. Mindfulness and meditation are believed to relax and calm the brain, tackling sources of stress while improving clarity focus and even sleep. According to mentalhealth.org.uk, those practising mindfulness have shown increased activity in the area of the brain associated with positive emotions.
9) Take opportunities for self-discovery and personal growth
– by learning something about themselves, people may find that they have grown in some respect. Many people who have experienced tragedies and hardship have reported better relationships, a greater sense of strength even while feeling vulnerable, increased sense of self-worth, a more developed spirituality and heightened appreciation for life.
10) Take good care of yourself
– pay attention to your own needs and feelings. Engage in activities that you enjoy and find relaxing. Exercise regularly. Taking care of yourself helps to keep your mind and body primed to deal with situations requiring resilience.
If you would like further help and support in resilience training in your workplace, get in touch with our Corporate Health department.
Stress: Are we coping?
We all feel the effects of stress in daily life, whether it’s managing children or dealing with a problem at work. Stress is a normal response, in fact, in small doses, stress can be useful. The problems arise when you start to have a ‘fight or flight’ stress response to situations in everyday life. This can lead to illness, both mentally and physically.
The first step is to recognise symptoms of stress:
- Nail biting and fidgeting
- Over-eating or loss of appetite
- Irritability with other people
- Substance abuse, including alcohol and smoking
- Lack of concentration
- Increased and suppressed anger
- Feeling out of control
- Excessive emotion & crying
- Lack of interest in anything
- Permanently tired even after sleep
By identifying stress-related problems as early as possible, action can be taken to avoid any serious stress-related illness. For Mental Health Awareness week, which runs from 14-18 May, here are some tips to help manage your own personal stress:
- Be active – 30 minutes a day can reduce the emotions and let you take the time to think more clearly
- Take control – you are your own worst enemy, but you are also the key to empowerment!
- Find support – Connect with your family and friends, the more help the better the solutions
- Take time for yourself – remember to have time for yourself as well. Read, relax and get things done on your to do list that may be holding you back
- Create challenges for yourself – Setting achievable goals, little or big can help build confidence in your abilities
- Avoid unhealthy habits – Cut down on caffeine, smoking, and alcohol. These can enhance the feeling of stress in the long run
- Be positive – Instead of looking at problems negatively, try to see what you can get out of it to help you grow. Be grateful!
- Acceptance – Take ownership of mistakes, or acceptance of things you can’t control.
Our Occupational Health team at the Fleet Street Clinic are able to provide a full range of work health assessments to address the occupational health needs of your staff. Click here for more information.
To book an appointment with one of our friendly doctors, or for further details on what we can offer for our Occupational Health, call us today on 0207 353 5678 email info@fleetstreetclinic.com or book online now.

WHAT IS DIABETES?
Diabetes is a lifelong condition that occurs when the body is unable to properly regulate the amount of glucose (sugar) in your blood. Poor control of diabetes can lead to high blood sugar levels and cause long term damage to your overall health and organs.
WHAT HEALTH PROBLEMS DOES IT CAUSE?
High blood sugar levels can cause a lot of damage to your body and if not managed correctly, may lead to many diabetic complications. This will cause long term health problems, especially if they go untreated.
HOW DOES DIABETES AFFECT OTHER PARTS OF YOUR BODY?
Eyes: Retinopathy is a complication of diabetes caused by high blood sugar levels damaging the retina, often leading to vision impairment. It is the leading cause of blindness among working-age adults in the UK. As a consequence of diabetic retinopathy, swelling can take place, called diabetic macular oedema. People with diabetes are also more prone to develop cataracts and glaucoma at an earlier age, contributing to vision reduction.
Feet: Foot health is often a neglected area anyway but high blood glucose levels can lead to insensitivity in the foot and lower limbs, which means you lose the ability to feel pain and distinguish hot or cold. It can also lead to less blood supply to your feet leading to poor circulation.
Loss of sensitivity means that you may not notice if you have a minor cut, sore or wound and poor circulation means if you do get a cut or sore, it will take longer to heal and open wounds are more likely to become infected. This combination is why there is an increase in risk of amputation for those who are diabetic. Regular podiatry appointments are the best way to look after your foot health.
Heart: High blood sugar levels can also cause problems to your blood vessels which can sometimes lead to serious problems such as heart attacks and strokes.
Kidneys: High blood sugar levels creates more difficulty for the kidneys to clear waste. This may lead to Diabetic Nephropathy, the deterioration of the kidneys.
HOW CAN DIABETES BE TREATED?
There is currently no cure for diabetes, therefore, the best way to deal with diabetes is to get it properly managed and controlled. If you are diagnosed with type 1 diabetes, you must either inject or pump insulin into body to treat your diabetes. If you have type 2 diabetes, you may also have to use insulin, however, it can be managed through diet and lifestyle changes.
HOW CAN YOU TEST FOR DIABETES?
An instant HbA1c test can confirm if you’re within the recommended range, or are considered pre-diabetic or confirm that you have diabetes. Using a small blood sample it will measure how well your blood sugar has been controlled over the last 3 months and provide a numerical reading.
As the HbA1c test provides 3-months insight, it is an important blood test for diagnosed diabetics. It provides a good indication of how well they are managing their diabetes..
Many people are more familiar with the glucose blood test – it measures the concentration of glucose molecules in your blood at a single point in time. The amount of glucose in your blood could also indicate whether you could be diabetic or not. People with diabetes can also use this test to manage their condition on a daily basis alongside regular HbA1C testing.
You can book an instant HbA1C test online at a cost of £54.50.
WHAT ARE THE SYMPTOMS?
When it comes to diabetes the symptoms are not always obvious and can often go unnoticed for long periods of time before being diagnosed.
The most common symptoms include:
- Feeling constantly thirsty or dehydrated
- Unintentional loss of weight and increased appetite (type 1)
- Vision begins to blur
- Numbness in your hands or feet (type 2)
- Fatigue
- Urinating more frequently
WHO IS AT RISK?
In the UK, type 2 diabetes is the most common type of diabetes, affecting over 90% of sufferers. The symptoms of diabetes are often mild, therefore, it’s important to be aware of the risk factors that could make you more susceptible to diabetes in the future.
According to Diabetes UK, type 2 diabetes is twice more likely in people of African descent in comparison to people of European descent and six times more likely in South Asian communities, making them a high risk category in developing diabetes. Additionally, people of African – Caribbean and South Asian descent are also at risk of type 2 diabetes much earlier, usually over the age of 25. On the other hand, for Europeans the risk increases when over the age of 40. Other factors contributing to diabetes include being overweight, high blood pressure and genetics.
Other general risk factors include:
- Having high blood pressure
- Carrying extra weight around your middle
- Smoking
- Polycystic Ovary Syndrome (PCOS) sufferers
- Those with a sedentary lifestyle
- Drinking too much alcohol
- Those with disturbed sleep – this includes those who do not get enough sleep and those whose sleep too much
If you have symptoms of diabetes or general concerns about your diabetic risk, you can book a GP appointment to discuss in more detail.
Alternatively, you can book in for an instant HbA1c test with a nurse.
Women today lead incredibly busy lives. They run and organise homes and build successful careers, usually all whilst taking on the majority share of caring for their children and often their older relatives. It is therefore not uncommon for women to have little or no time to look after themselves, their health included.
In addition to not making time to prioritise their health, it seems that when women do put their health first and seek medical advice, they are less likely to feel heard and supported in comparison to their male counterparts.
A recent survey by The Department of Health and Social Care found that “more than 4 in 5 (84%) women they surveyed had experienced times when they (or the woman they had in mind) were not listened to by healthcare professionals.”
Based on the data they collected, ‘not being listened to’ appears to be present at all stages of the healthcare pathway. Specifically, many women told them:
- their symptoms were not taken seriously and/or dismissed upon first contact with GPs and other health professionals
- they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years
- if they did secure a diagnosis, there were limited opportunities to discuss or ask questions about treatment options and their preferences were often ignored
Many women recalled their symptoms being dismissed upon first contact with GPs and other professionals; women felt they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years; and post-diagnosis, discussions about treatment options were often limited, and some said their preferences were ignored.
To make matters worse, there is some evidence that due to historical clinical trials being disproportionately male-orientated there is much less research into women-only health concerns and assumptions have been made that similar medical treatments will work for both sexes. The top reasons for the under-representation of women in trials were the belief that hormone fluctuations could influence results and concerns that fertility could be affected. A widely accepted negative repercussion, amongst others, being that women are much more likely to experience adverse side effects of medications because drug dosages have historically been based on clinical trials conducted on men.
A combination of these factors may explain why there is a gender gap in health outcomes, with women experiencing poorer health outcomes in comparison to men. We strongly believe in equality and ensuring health is a top priority for all.
Therefore, here are the top health symptoms women should never ignore:
1) Any change in bowel habit and/ or urination
This includes blood in the stools, unexplained persistent abdominal pain, weight loss, lumps around the anus, lack of appetite, blood in the urine or increased frequency of urination. These are all reasons for seeing your doctor ASAP as these symptoms could be due to bowel, bladder or ovarian cancer. All patients should have an annual faecal occult blood (FOB) test to exclude bowel cancer, which has increased in incidence in the UK for reasons unknown. Or if you are looking for a more in-depth investigation, you should request a colonoscopy which entails looking at the bowel with a colonoscopy. This is the gold standard, but an FOB is the next best thing and far less invasive as a first investigative option. It takes no time at all and is a good preventative check.
2) Any changes to the breast.
Any breast lumps, skin changes, nipple discharge, nipple changes or pain in the breast must be checked ASAP. Breast cancer is the most common type of cancer in the UK and often can present insidiously. Get to know what your breast feels like so that any subtle changes can be detected as early as possible.
3) Skin lesions that do not heal.
Any scab on the skin which does not heal, especially around the eyes, nose, ears and face should be checked. All these areas are the most sun-exposed, and, as such, are more at risk of skin cancer. If these lesions are picked up and treated early, scarring is minimal, but if left, then disfiguring scars and skin grafts may be necessary.
4) Bleeding after the menopause.
If you experience any bleeding after 1-year of your last menstrual period, you must visit your GP for further investigation. Bleeding after the menopause is not common and could be an indicator of cancer of the uterus, or the cervix. They will usually opt for a biopsy of the uterine lining to exclude both – don’t worry, this doesn’t hurt.
5) Always have regular cervical screens.
Most people don’t find cervical screens painful, although they can feel somewhat uncomfortable. If you are concerned about the pain or you have previously found the procedure painful with the NHS, you can opt to book a private appointment. It is important that you don’t miss your appointment.
6) Bleeding between periods.
At any age, you should never ignore bleeding between periods or after intercourse, as this can be a sign of cervical or uterine cancer. Whilst cervical cancer is monitored by regular screening, it is important to still get bleeding between periods checked out following a normal smear result. Cancer of the endometrium is becoming increasingly common in women who have not had children.
7) A persistent cough.
Regardless of gender, you should get a persistent cough checked out by your doctor, especially if you are coughing up discoloured sputum or blood.
8) Any unexplained changes to your body.
Any new indigestion, shortness of breath on exertion, neck or left arm pain requires follow up ASAP. Make sure a GP examines your chest and makes the appropriate investigations.
The same applies to calf pain or any pain in the chest. By taking a full history, examining you and doing quick and easy investigations, worrying conditions can be excluded, such as a pulmonary embolism or a heart attack.
Some recent examples of cases where other healthcare providers have failed our new female patients:
1) We saw a 36 year old who had not had a cervical screening for 5-years because the last one was so painful. The NHS advises a screening every 3-years but we advise yearly screenings to ensure any abnormalities are found as early as possible. 5-years is far too long!
2) We saw a woman who had a suspicious lump at her anal margin, which her usual GP had told her was part of her bladder. She wanted a second opinion because it had grown in size and was now painful. The patient was referred for an urgent assessment to exclude cancer.
3) We saw an 88 year old patient who was disfigured by a large basal cell carcinoma on her forehead, about which she was embarrassed. The patient had been seen by a dermatologist who had frightened her about having the lesion removed by saying she might not survive an anaesthetic. The patient wished that she had taken the risk and asked to be referred back, as the skin lesion was disfiguring and ruining her quality of life.
** The outcomes of these patients are yet unknown, but they are all certainly serious health concerns that should have been properly addressed long before now.
We want to encourage women to take ownership over their health and be assertive when they feel that something has changed from our normal. If they feel like they are not being taken seriously or not being heard, they should seek a second opinion.
If you cannot get an appointment with your usual GP or through the NHS, rather than waiting for weeks and worrying about what it could be, make an appointment with a private GP who can usually see you on the same day!
Put your mind at ease with private healthcare.
Ageing is an inevitable part of living. As we age, many physical and psychological changes affect our overall health and these vary from person to person.
The general myth is that as you age, you become more fragile and that this is unavoidable. This is most certainly not the case. There are always things we can do to help keep healthy in our older years and these changes can slow down or even prevent certain health conditions from developing.
The term “fragile” is defined as not “strong or sturdy; delicate and vulnerable” and is most often used to describe older ladies. One particular age-related health issue that supports this description would be osteoporosis.
Osteoporosis is a degenerative disease that weakens and thins the bones which makes them fragile and more likely to break and is becoming increasingly common. It is much more prevalent in women than men due to the menopause directly affecting hormone balances and this directly affects bone density. It is important to prevent osteoporosis as we age as 75% of fractures due to osteoporosis occur in people aged 65 and over.
There are several things you can do to help prevent osteoporosis:
1) Do regular, weight bearing physical activity.
The lack of regular exercise will result in loss of bone and muscle, so adults who are inactive are more likely to have a hip fracture than those who are more active. Adults should aim to do at least two and a half hours of moderate-intensity exercise every week. Weight bearing and resistance training are a particularly great way of improving bone density and helping to prevent osteoporosis.
2) Eat plenty of calcium and Vitamin D containing foods.
Your diet is very important and the nutrients we get from the food we consume will affect how strong our body is. Eat plenty of dairy, seeds, eggs, oily fish, protein, fruit and vegetables. Additionally, try to get at least 15-minutes of sun exposure per day to increase your Vitamin D intake. As we know in the UK, such sun exposure is not always possible during the winter months and, if this is the case, taking a daily Vitamin D supplement is advised.
3) Maintain a healthy weight.
As you get older, you start to lose lean body mass like muscle and bone density and this can start to happen yearly from the age of 30. Being underweight weakens your bones so it is important to keep your weight in a healthy range. A good indication, although not exact, is your BMI. For most adults, a healthy BMI range is between 18.5 and 24.9, so try not to let your BMI fall below 19.
Those who suffer from eating disorders such as anorexia and bulimia are at a higher risk of fragility due to the conditions causing further bone density loss. This can happen to anorexic and bulimic sufferers of all ages.
Older people should aim to consume a varied diet, consisting of enough calories for maintaining a healthy weight.
4) Limit your consumption of alcohol.
We’d recommend that you drink no more than a maximum of 2 units of alcohol per day. Any more than this has been demonstrated to increase the risk of bone fracture. Alcohol abuse has detrimental effects on bone health and increases a person’s risk of developing osteoporosis.
5) Stop smoking and definitely don’t start!
Smoking is a known risk factor for osteoporosis as it increases bone mass loss. In fact, smoking doubles the risk of hip fracture.
Generally, being healthy is the key to avoiding fragility and in particular preventing osteoporosis as we age. Having an annual health medical can highlight any areas of concern. They can monitor the progression of any pre-existing health issues, as well as detect arising conditions in the early stages. You can book your annual medical online
In addition to making healthy lifestyle choices, it is also important to book a doctor’s appointment should you notice any changes to your health. The sooner a health concern is addressed, the easier it is to treat. You can book a GP appointment online.
If you are feeling sad at the start of the year, don’t worry, you are not alone.
Although it comes around every year, we always seem to be caught off-guard by what has now commonly become known as “The January Blues”.
The January blues is another name for situational depression and is associated with the way we think and feel. Around this time of year, the weather is cold and gloomy, the days are shorter and the nights are longer, plus you may be experiencing post-Christmas exhaustion, debt and perhaps even dread going back to work.
Symptoms of the January blues are things such as low mood and sadness, lack of motivation, tiredness and low energy. These are all normal feelings, if temporary.
Most likely, your negative mood will be brought on by the anticlimax of reality after the exciting events of December & the New Year. Ever heard that old phrase, “don’t cry because it has ended, but smile because it happened”? Find comfort in knowing that you are absolutely not alone in feeling blue in January. In fact, many people in the UK feel especially down in January but the good news is that the January Blues are temporary and typically only last a couple of weeks. You don’t need to take any medication as your thoughts and feelings should naturally return to normal.
If it doesn’t and you are experiencing prolonged or worsening thoughts and feelings, you may actually have Seasonal Affective Disorder or SAD, which is different. SAD is clinical depression caused by a person’s biology. It is much longer-lasting, sometimes months on end and likely to occur every year in winter. You should see a doctor to discuss your symptoms as if you have SAD, a range of treatments are available to assist recovery. More information on SAD can be found here.
Remember, please be kind to yourself and know that you’re not alone.
For more information on our GP Services.
To book a GP appointment online, click here.
Sleep is one of our greatest allies when it comes to health and wellbeing. It is associated with a number of health benefits which can have a huge positive impact on our daily lives.
Conversely, a lack of sleep can be detrimental – research has even found that not getting enough sleep can negatively impact some aspects of brain function to a similar degree as alcohol intoxication!
Dr Belinda Griffiths discusses some of the mental and physical health benefits of getting a good night’s sleep.
Immune System
During sleep, your body releases cytokines, which are essential for the regulation of the immune system. Cytokines are required in increased amounts when you are attacked by a pathogen (when you’re ill) or under stress. The level of cytokines increases during sleep, and therefore lack of sleep hinders the body’s ability to fight infections. This is also the reason why the body tends to sleep more while suffering from an infection.
Weight Control
When you’re well-rested, you’re less hungry. Being sleep deprived disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite.
With those out of balance, your resistance to the temptation of unhealthy foods goes way down. And when you’re tired, you’re less likely to want to get up and move your body. Together, it’s a recipe for putting on the pounds!
Athletic Achievement
If your sport requires quick bursts of energy, like wrestling or weightlifting, sleep loss may not affect you as much as endurance sports like running, swimming, and biking. But you’re not doing yourself any favours. Besides robbing you of your energy and time for muscle repair, lack of sleep saps your motivation, which is what gets you across the finish line. You’ll face a harder mental and physical challenge – and see slower reaction times. Proper rest sets you up for your best performance.
Memory
When you’re tired, you can have difficulty recalling information. That’s because sleep plays a big part in both learning and memory. Without sufficient sleep, the brain finds it difficult to focus and take in new information in the first place and then doesn’t have enough time to properly store information as short-term memories. Sleep helps enable you to retain memories and store information.
Sleep also allows for your mind to rest, repair and rebuild, the same way it does for your body. As you sleep, your brain begins to organise and process all the information you’ve taken in during the day. It converts these short-term memories into long-term memories – this helps you to learn.
Concentration
Not sleeping properly can mean that both your body and brain don’t function properly the next day. It can impair your attention span, concentration, strategic thinking, risk assessment, reaction times and problem-solving skills. This is particularly important if you have a big decision to make, are driving, or are operating heavy machinery. So, getting plenty of sleep can help you stay sharp and focused all day long.
Mood
Another thing your brain does while you sleep is process your emotions. Your mind needs this time in order to recognise and react in the right way. When you cut that short, you tend to have more negative emotional reactions and fewer positive ones. Lack of sleep can cause bad temper and anxiety, so the better you sleep, the better your ability to stay calm, controlled and reasonable.
Chronic lack of sleep can also raise your chance of having a mood disorder. One large study found that people with insomnia were five times more likely to develop depression, and the odds of having anxiety or panic disorders are even greater.
A refreshing slumber helps you hit the reset button on a bad day, improve your outlook on life, and be better prepared to meet the challenges of the next day.
Heart Health
While you sleep, your blood pressure goes down giving your heart and blood vessels a bit of a rest. The less sleep you get, the longer your blood pressure stays up during a 24-hour cycle. High blood pressure can lead to heart disease and strokes. Therefore, it is important to keep your blood pressure down.
Pain Threshold
Poor sleep and pain mutually reinforce each other. Sleep deprivation increases pain sensitivity and reduces pain tolerance. Therefore, something will feel more painful when you’re tired.
It is clear that sleep is an essential part of helping us stay physically and mentally healthy. What better excuse to have a few extra hours of sleep a day!
If have any concerns about your health, book a GP appointment today.
How much would you pay to prevent bowel cancer?
£1,000? £500? £200? £100? Or just £45?
Everyone knows a friend or relative who has suffered from or unfortunately, died of bowel cancer. Also known as colorectal cancer, bowel cancer is the fourth most common cancer in the UK but the second biggest killer. More than 16,000 people die from bowel cancer in the UK every year. Similar to other types of cancer, bowel cancer is treatable and curable especially if diagnosed early.
The earlier it is detected, the greater the chance of survival.
However, the survival rate drops significantly as the disease develops. The optimal test for bowel cancer is a colonoscopy, but it is an invasive test which checks the lining of the bowel for cancer. Due to the invasive nature of this test, it usually happens following a positive screening result or if a person has multiple symptoms so as not to cause unnecessary discomfort is symptoms are say. related to another health issue.
As bowel cancer symptoms are also indicators for a wide range of gastroenterological (digestive system) disorders, a simpler, non-invasive FIT stool test (faecal immunochemical test) can be the first step for patients with concerns and/or symptoms such as lower abdominal symptoms such as abdominal pain, rectal bleeding and/or a change in bowel habits prior to a colonoscopy.
For those who are healthy with no symptoms, FIT screening is an important way of testing healthy people to see if they show any early signs of cancer.
Bowel Cancer Screening
It can be challenging to differentiate between patients with serious bowel disease such as bowel cancer, from those with benign functional or diet-related conditions, such as IBS – irritable bowel syndrome, and minor colorectal diseases such as haemorrhoids.
A FIT test or faecal immunochemical test, looks for blood in the stool, an early sign of bowel cancer. It is a simple and effective non-invasive test.
If there is blood present, this can indicate the presence of abnormalities in the bowel, which over time may develop into cancer. Patients with a positive FIT result are then referred for further investigation by colonoscopy.
A FIT test does not diagnose bowel cancer, but it’s a simple way to find out if you need further tests. Introducing regular bowel cancer screening into your health checks will reduce the risk of dying from bowel cancer.
Are all FIT Tests the same?
The short answer, no.
The sensitivity of a FIT test to detect blood in stools can be adjusted to be more or less accurate. The lower the threshold, the more sensitive the test is to blood in the stools meaning the earlier abnormalities can be identified.
Where you live in the UK dictates the FIT tests available to you, see below:
NHS Scotland:
Age range: 50-74 years – Automatic invite for screenings every 2 years / 75+ done on request
Blood sensitivity threshold: 80ug per g of stool
NHS England & Wales:
Age range: 60-74 years – Automatic invite for screenings every 2 years / 75+ done on request
Blood sensitivity threshold: 120ug per g of stool
Fleet Street Clinic:
Age range: Screening recommended from 40 years onwards. Available from 20 years if symptoms are present and for individuals with a family history of bowel cancer of one or more first-degree relatives (sibling, parent or child).
Blood sensitivity threshold: 20ug per g of stool.
A big difference!
Why is this so important?
If early detection is a matter of life and death when it comes to bowel cancer then the optimum FIT test has to have the lowest sensitivity threshold to provide the most accurate diagnosis. The more sensitive the FIT screening, the more cancer and precancerous polyps can be detected, especially at an early stage of abnormality.
At Fleet Street Clinic, we are more likely to pick up blood in the stool by a factor of 4 compared to NHS Scotland and by a factor of 6 in comparison to NHS England & Wales, all without the rigid age limitations.
Bowel Cancer Screening at Fleet Street Clinic
The FIT test at Fleet Street Clinic has the lowest sensitivity threshold on the market right now. It is an easy, quick test which costs just ££70* with results within a week.
Surely it is worth it?
If by any chance your test is positive, we provide a letter of referral which can be given to your GP (Private or NHS) or used at one of the referral centres we recommend for private colonoscopy. The choice is yours.
Tell your friends about this life-saving test and save a life – It could be your own.
If you’re concerned about bowel cancer, then it’s important to book a 15-minute GP appointment to speak to a doctor – you can book online.
* A 15-minute GP appointment costing £108 is required in addition to the cost of the FIT test.
THE WORLD HEALTH ORGANISATION (WHO), HAS REPORTED THAT POPULATION EXPOSURE TO HEAT IS INCREASING DUE TO CLIMATE CHANGE.
The WHO states, ‘global temperatures and the frequency and intensity of heatwaves will rise in the 21st century as a result of climate change’. Extended periods of heat exposure during the day and night time can increase the amount of physiological stress on the human body.’
The stress caused by heat exposure exacerbates the top causes of death globally. This includes respiratory and cardiovascular diseases, diabetes mellitus and renal disease.
They go on to state, ‘Exposure to excessive heat has wide-ranging physiological impacts for all humans, often amplifying existing conditions and resulting in premature death and disability.’
With the temperature said to continue rising, the WHO also states, ‘Awareness remains insufficient of the health risks posed by heatwaves and prolonged exposure to increased temperatures.’
So, who is most affected by heat exposure and how will it impact your health?
Who is affected?
Rising temperatures affect the whole population. However, some populations are more vulnerable to exposure to excessive heat. Those include:
- Elderly people
- Infants and children
- Pregnant women
- Outdoor and manual workers
- Athletes
- Poorer communities
How does heat impact health?
With rapid increases in external temperatures, the body will struggle to regulate our internal temperatures. The knock-on effect of this can result in a number of heat-related illnesses such as heat cramps, heat exhaustion, heatstroke, and hyperthermia. Reported small differences in the seasonal changes have been reported to have increased the number of heat-related illness and even death. Rising temperatures can also worsen chronic conditions such as cardiovascular, respiratory, and cerebrovascular disease and diabetes-related conditions.
What actions can you take to stay cool?
- Aim to keep your living space cool. WHO suggests ‘below 32 °C during the day and 24 °C during the night’
- If it is safe, open your windows at night time to cool your living space.
- Stay out of the heat by staying in the shade and avoiding going outside during the hottest part of the day.
- Take cool showers and wear loose-fitting clothing.
- Drink regularly and avoid alcohol and caffeine.
- Check on vulnerable family members who may be affected by the heat.
What to do if someone shows signs of a heat emergency?
It is extremely important to know what to do when someone is showing signs of heat illness. Everyone should know how to respond to heat emergencies, this can be learnt in first aid courses.
If one of your family members or someone you assist is showing signs of hot dry skin and delirium, convulsions and/or unconsciousness, call a doctor/ambulance immediately.
Whilst you are waiting for help to arrive place them in a cool place in a horizontal position and elevate their legs. It is now important to initiate external cooling.
This can be done by:
- Removing clothing
- Placing cold packs on the neck and groin
- Spraying cool water on their skin
- Fanning them
- If they are unconscious, place them on their side
If you or someone you are with is displaying mild signs of heat illness that is not considered an emergency, you might want to consider a same-day GP appointment. You can book an appointment online.
MARCH IS OVARIAN CANCER AWARENESS MONTH
A vital month raising awareness of ovarian cancer to improve early diagnosis to save lives.
More women died from ovarian cancer in the UK (4,227) than from all other gynaecological cancers combined in 2016, according to Cancer Research UK. However, worryingly one in five women in the UK (22%) mistakenly believe that a smear test (cervical screening) can detect ovarian cancer, according to research Target Ovarian Cancer carried out with YouGov.
We are committed to raising awareness of the disease.
Speak to one of our female GP’s about any concerns you may have about your gynaecological history and your families medical history. During your consultation, we will also conduct a breast check and pelvic examination.
“In the UK a woman dies every two hours from ovarian cancer, but the earlier the diagnosis the better the chances are”
Professor Hani Gabra – Director of Ovarian Cancer Action Research Centre
What is ovarian cancer?
Ovarian cancer is when abnormal cells in the ovary begin to grow and divide in an uncontrolled way and eventually form a growth (tumour). Every year 7,300 women in the UK are diagnosed with ovarian cancer.
Who can get ovarian cancer?
The risk of developing ovarian cancer increases as you get older. The most common type of ovarian cancer is epithelial ovarian cancer, this usually occurs in women older than 50 years old. We don’t know exactly what causes epithelial ovarian cancer. But some factors may increase or reduce the risk.
Factors that increase the risk include:
- getting older
- inherited faulty genes
- having breast cancer before
Factors that may reduce the risk include:
- taking the contraceptive pill
- having children
- breastfeeding
Ovarian Cancer is notoriously difficult to spot.
With non-specific symptoms in the early stages. It is hoped that this new method of early diagnosis could help save lives.
How to recognise the symptoms of Ovarian Cancer:
Early Ovarian Cancer symptoms can be similar to those of other conditions, these some to watch out for:
- Persistent bloating – not bloating that comes and goes
- Pain in the lower stomach and pelvis
- Difficulty Eating and feeling full quickly
- Back pain
- Fatigue
- Change in bowel habits
What should you do if you’re worried?
It is important to contact your GP as soon as possible if you spot any symptoms that are abnormal for you.
We understand talking about your concerns and having an examination can be quite worrying and for some, embarrassing, therefore, to make you as comfortable as possible, all our well woman services are booked with a female GP.
There is an Ovarian Cancer Blood Test – CA 125 available
Levels of protein CA125 in the blood are recognised as a marker for ovarian cancer. This simple and effective blood test will detect early stages of ovarian cancer. You can either have this as a stand-alone blood test or add it on to your medical for an additional cost. Please inquire for prices..
Links:
Target Ovarian Cancer
Cancer Research UK
For more information about Fleet Street Clinic’s Women’s Health Services.
You can also book a GP appointment online.
This week is Cervical Cancer Prevention Week (#CCPW) and we’d like to remind all our patients that cervical cancer can be fatal – It is the most common cancer in women aged 35 and under.
Current UK statistics state:
> 2 women lose their lives to the disease every day
> 9 women are diagnosed with cervical cancer every day
> 75% of cervical cancers can be prevented by a smear test
Thousands of lives can be saved every year with better awareness and understanding of the symptoms of cervical cancer. Regular smear tests and having the HPV vaccine can dramatically decrease your chances of developing cervical cancer and will also assist in early detection.
Smear tests are extremely important and a major contributing factor to lowering the number of cervical cancer cases seen each year. On average, cervical screening helps save the lives of approximately 4,500 women in England every year, however, 1 in 4 women still don’t attend their smear test.

Smear tests are a method of detecting abnormal cells on the cervix, (the entrance to the womb). The detection and removal of abnormal cells can prevent cervical cancer from developing. As with all cancers, the earlier a problem is detected, the better the patient’s outcome.
Information on Cervical Cancer
Cervical cancer is not thought to be hereditary.
Cervical screening is not a test for cancer as screening programmes help to prevent cancer by detecting early abnormalities in the cervix, so they can be treated. If these abnormalities are left untreated they can lead to cancer of the cervix (the neck of the womb).
Symptoms:

For more information: www.jostrust.org.uk
November is Mouth Cancer Awareness Month, and Fleet Street Clinic has collaborated with the charity campaign MouthCancer.org to help raise awareness of the disease.
For more information about Mouth Cancer, you can read the Q&A’s below.
What is Mouth cancer?
Mouth cancer relates to cancer found in the lips, tongue, cheek and throat.
There are, on average, almost 7,800 new cases of mouth cancer diagnosed in the UK each year. The number of new cases of mouth cancer is on the increase, and in the UK has increased by over half in the last decade alone.
Who is at risk?
Mouth cancer is twice as common in men than in women, though an increasing number of women are being diagnosed with the disease. Age is a factor, with people over the age of 40 more likely to be diagnosed, though more young people are now being affected than previously.
People with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer. Prognosis is good if the disease is caught early.
What can cause mouth cancer?
Although mouth cancer can affect anybody, around 91% of all diagnoses are linked to lifestyle. This means that by amending our lifestyle choices, we can help cut the chances of developing mouth cancer.
There are many known contributors to mouth cancer:
- Tobacco
- Alcohol
Many cases of mouth cancer are linked to tobacco and alcohol.
If tobacco and alcohol are consumed together the risk is even greater.
- Over-exposure to sunlight can also increase the risk of cancer of the lips.
- Poor diet is linked to a third of all cancer cases. Book a Dietitian Consultation
- Experts suggest the Human Papilloma Virus (HPV), transmitted through oral sex, could overtake tobacco and alcohol as the main risk factor within the coming decade. Book Your HPV Vaccine
What is the link between HPV and cancer?
There’s growing evidence that an increasing proportion of cancer is caused by HPV infection in the mouth. Around 1 in 4 mouth cancers and 1 in 3 throat cancers are HPV-related, but in younger patients, most throat cancers are now HPV-related.
HPV doesn’t directly give you cancer, but it causes changes in the cells it’s infected (for example, in the throat or cervix) and these cells can then become cancerous.
The HPV vaccine, Gardasil 9 is available at Fleet Street Clinic for both girls and boys. The vaccine was developed to fight cervical cancer, but it is likely that it’ll also help to reduce the rates of mouth cancer.
It is advisable to give the HPV vaccine before sexual activity starts to get the best protection. The underlying principle being there has been no exposure to any HPV strains yet. You can, however, receive the vaccination later on in life, this is down to personal choice. We’d recommend a GP consultation to discuss the HPV vaccine prior to booking.
More information on Gardasil 9.
What are the signs of mouth cancer?
Mouth cancer can appear in different forms and can affect all parts of the mouth, tongue and lips. Symptoms of mouth cancer include:
- A painless mouth ulcer that does not heal normally
- White or red patch in the mouth or on the tongue
- Any unusual lumps or swellings that linger
- 1 or more mouth ulcers that don’t heal after 3 weeks
- Pain when swallowing
- A feeling as though something’s stuck in your throat
Be mouth aware and look for changes in the mouth:
It is important to visit your dentist or your GP if these areas do not heal within three weeks.
How can mouth cancer be detected early?
Mouth cancer can often be spotted in its early stages by your dentist during a thorough mouth examination. If mouth cancer is recognised early, then the chances of a cure are good.
It is also advised to self-check regularly for any noticeable changes in your mouth, the inside of your cheeks, the front and sides of your neck, colour and texture changes of your tongue, changes to your lips and finally, lumps and swellings on your head and neck.
How can I keep my mouth healthy?
- It is important to visit your dentist regularly, as often as they recommend, even if you wear dentures. This is especially important if you smoke and drink alcohol.
- When brushing your teeth, look out for any changes in your mouth, and report any red or white patches, or ulcers, that have not cleared up within three weeks.
- When exposed to the sun, be sure to use a good protective sun cream, and put the correct type of barrier cream on your lips.
- A good diet, rich in vitamins A, C and E, provides protection against the development of mouth cancer. Plenty of fruit and vegetables help the body to protect itself, in general, from most cancers.
- Cut down on your smoking and drinking.
If you have any concerns about mouth cancer, you can book a GP appointment or a dental appointment with Temple Dental.
With thanks to mouthcancerawareness.org
Statistics via Mouth Cancer Foundation Org
Breast Cancer Now’s ‘Wear it Pink’ day is one of the biggest fundraising events in the UK.
Thousands of amazing people will ‘Wear It Pink’ in their communities, schools or workplaces for the UK’s largest breast cancer charity, Breast Cancer Now. This Friday 19th October the staff of Fleet Street will show off their best pink garments to raise awareness and show solidarity for such a great charity.
‘’This year, 55,000 women will hear the words “it’s breast cancer”
Breast Cancer Now supports nearly 450 of the world’s best researchers across the UK and Ireland. Working together to help prevent breast cancer, help improve the lives of those dealing with it now and most importantly stop people from dying from the disease. Research holds the key to a future where all that changes. Ensuring women get to enjoy their best life whether that be watching their children grow up or travelling the globe. It’s about making sure women are always able to create a lifetime of memories with the people they love.
The Fleet Street Clinic is championing Breast Cancer Now’s goal, that by 2050, everyone who develops breast cancer will live – and live well. By our staff wearing pink, raising awareness and donating we can help get there and make life-saving research happen.
Well Woman Services
We have four female GPs specialising in women’s health. Women’s health is a focus for us, and one of our highest priorities.
Our Well Woman health checks are focused on protecting your well-being and meeting your exact needs. Each comprehensive medical is tailored to your circumstances and designed to screen for health problems at the earliest possible stage.
Well-woman health checks include:
- Recording your height, weight and body mass index (BMI)
- Blood pressure
- Breast examination (and instruction on breast self-examination)
- Cervical smear test
- Pelvic examination
- Urine test
- Blood tests
Some viruses thrive in the winter and are easily spread during cold weather. The lack of sunlight also means there is less Vitamin D in your body during winter, which can lower your immune system. This makes it harder for the body to fight off infections, resulting in a higher chance of sickness, even amongst the healthy.
If you’re planning on avoiding the flu this year, going on holiday, starting University, having a child or just living a healthy lifestyle in general, then there are a number of extremely important vaccines you should know about.
1. Flu Vaccine:
Now is the perfect time to have your flu jab, to ensure protection for the entire winter. Our adult flu vaccines are already in stock including Quadrivalent, FluAd and egg-free. Due to distribution delays, needle-free Quadrivalent vaccines for kids will be arriving soon.
– Find out more about the Flu Vaccine
2. MMR – Measles, Mumps and Rubella:
Many people who are now adults have never been vaccinated against measles, mumps or rubella, either from concerns over misinformation during the 1990s or because they simply missed out on getting protected. As a result, there has been an alarming rise in cases and outbreaks, with several deaths. Unfortunately, this year the UK also lost its ‘Measles Free’ status. Two doses are needed for protection, and it is never too late to be vaccinated!
– Find out more about the MMR Vaccine
3. Chickenpox:
There’s no need for any child to go through the misery of the chickenpox. It is entirely preventable with a vaccine that is still not yet available on the NHS, Varicella. This vaccine can be given to children over the age of one year. 2 doses are recommended for full protection.
– Find out more about the Chickenpox Vaccine
4. Shingles:
Shingles is a horrible reactivation of the chickenpox virus in adults who have had chickenpox during childhood. It consists of a painful, blistering rash. The pain can linger for months or years but it is also preventable. Shingrix is a relatively new vaccine which provides the best protection against Shingles. It offers up to 90% immunity. Supplies worldwide are limited but The Fleet Street Clinic is one of the first medical practices in the UK to make it consistently available.
– Find out more about the Shingles Vaccine, Shingrix
5. HPV (Human Papilloma Virus) Vaccine:
HPV is the leading cause of cervical cancer but also causes other genital, head & neck cancers. The national programme offers all 12- and 13-year-olds in school the Gardasil HPV vaccine. HPV-4 protects against 4 types of HPV. There is no “catch-up” programme for older children and adolescents.
At Fleet Street Clinic, we offer Gardasil 9. It offers greater protection against 5 additional types of HPV. In our opinion, if you have not received the HPV vaccine yet, you are better to get the HPV- Gardasil 9 vaccine to benefit from the extra protection it offers.
– Find out more about the HPV Vaccine, Gardasil 9
6. Whooping Cough:
Childhood vaccination does not give lifelong protection, and newborns are especially vulnerable. Vaccination is recommended during pregnancy, and may also be advisable if you have a close family member who is pregnant, or if you’re likely to be in close contact with their newborn baby.
– Find out more about Whooping Cough
7. Meningitis:
We offer Meningitis ACWY and Meningitis B vaccines. This vaccine is recommended to all those who fall outside the age groups currently targeted by the NHS or have an important deadline for protection.
– Find out more about Meningitis ACWY and Meningitis B vaccines
8. Hepatitis B:
Hepatitis B is spread by blood and body fluids. In most other developed countries, it has been a standard part of the childhood vaccination schedule for many years, but in the UK it has only just been added to the schedule at birth and infancy. There is no “catch-up” programme for older children and adolescents. We strongly believe this vaccine should be offered more widely – all young, sexually active adults ought to be protected.
– Find out more about Hepatitis B
9. Pneumonia:
We strongly recommend the Prevenar pneumonia vaccine for those aged 65 and over. Pneumonia can affect people of any age, but it’s more common and can be more serious, in certain groups of people, such as the very young or the elderly. Anyone with a past history of pneumonia, asthma or lung disease should also consider this vaccine. Anyone can get a pneumococcal infection, but not everyone is offered the pneumococcal vaccine on the NHS. Prevenar pneumonia vaccine protects against 13 of the most common strains of Streptococcus pneumoniae bacteria.
– Find out more about the Pneumonia Vaccine
10. Rabies:
At the Fleet Street Clinic, we are well known for offering the full range of travel vaccines, always in stock. But if I had to pick just one vaccine I would never want to be without, it would be rabies. Protection is cheap, easy, safe and long-lasting – but expensive and hard to find if you are ever unlucky enough to be bitten abroad. I was once attacked by a dog in a remote part of Peru, and have had to look after dozens of travellers who have been in similar situations.
– Find out more about the Rabies Vaccine
Get in touch…
If you would like more information or require any of these vaccinations, please give us a call to arrange an appointment or book your appointment online today
HPV vaccine unavailable to boys on the NHS
The HPV vaccine is now offered to girls aged 12-18 years in the UK for free by the NHS.
Since its introduction in 2008, it has already shown to be very effective in reducing the cases of cervical cancer in females*. But the HPV virus doesn’t only cause cervical cancer, it can lead to other cancers such as anal, head, neck and throat cancers. Men are as much at risk of these cancers as women, so why are boys ineligible to receive the HPV vaccine as part of the NHS vaccination schedule?
The BBC has reported the case of Jamie Rae today, to highlight the issue. Mr Rae is campaigning for the HPV vaccine to be introduced, after undergoing radiotherapy for his throat cancer which he believes could have been prevented if an HPV vaccine had been available.
The article also reports that Professor Francis Vaz, a head and neck surgeon at University College London Hospital, paid privately to vaccinate his three sons, to protect them from certain cancers like anus, penis, mouth and throat. He said he saw on a daily basis that cancers driven by the HPV virus had been increasing in the past decade.
“I regularly see the bad end of that spectrum, so I thought the vaccination would be suitable for my sons,”
– he said.
“It’s just unfortunate it wasn’t available for them on the NHS. I was happy to pay for it because I think it’s a good vaccine.”
Why boys should receive the HPV vaccine
- About 15% of UK girls eligible for vaccination are currently not receiving both doses, a figure which is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries with no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high – treating anogenital warts alone in the UK is estimated to cost £58m a year, while the additional cost of vaccinating boys has been estimated at about £20m a year
Source: HPV Action
Our HPV vaccine page explains how get an HPV vaccine at Fleet Street Clinic.
FLEET STREET CLINIC – SPECIALIST VACCINE CLINIC
Fleet Street Clinic is a specialist vaccination clinic offering all vaccinations from travel jabs, to childhood immunisations to flu vaccinations programmes.
TO BOOK
You can book an appointment online.
Meningitis Now Offers Advice for World Meningitis Day, to spread the word about meningitis, how to spot it and what causes it, as well as the importance of vaccines.
The theme for World Meningitis Day 2018 is #AllMeningitisMatters.
There are several different causes of meningitis and vaccines can help protect against certain strains of bacterial and viral meningitis.
The key messages for this year are:
- Meningitis is a potentially deadly disease that can kill within 24 hours.
- Bacterial meningitis can be caused by many different types of bacteria.
- There are safe and effective vaccines that protect against the most common causes of bacterial and viral meningitis.
- Not all strains of meningitis are vaccine preventable, so being able to recognise the symptoms is crucial.
The HPV Vaccine, Gardasil 9, is back in stock at Fleet Street Clinic.
The vaccine is available to men and women. It protects against a range of cancers including cervical, head and neck cancer and other HPV-related diseases including genital warts.
5 facts about the HPV (Human papillomavirus) :
- Nearly all cases of cervical and anal cancer and 70% of oropharyngeal cancers are related to HPV.
- HPV is one of the most common sexually-transmitted diseases, so common in fact that most sexually active men and women will have HPV at some point in their life.
- There are different strains of the virus and they can be categorised into low-risk and high-risk HPV.
- There is no cure for HPV; some people fight off the virus without any knowledge of having been infected, whilst the virus can lie dormant in others, remaining undetected for many years.
- The virus can eventually cause abnormal cell growth – cervical abnormalities in women, which is why regular cervical screening is so important.
In order to protect against the virus, the HPV vaccine is strongly recommended. For more information, visit our HPV Vaccine page.
BOOKING A Vaccination APPOINTMENT
You can book an HPV appointment online.