Category: Cancer
Step into the realm of Movember, where the Chevron, the Dali, or the Handlebar becomes more than just a style statement – it’s a symbol of men’s health awareness.
Are you ready to join the Mo-gang and make a statement this Movember?
Movember transcends mere facial hair growth; it’s a global movement dedicated to transforming the landscape of men’s health. This renowned charity, a beacon of hope and change, addresses critical issues like prostate cancer, testicular cancer, and mental health and suicide prevention.
In the heart of London, at Fleet St. Clinic, we’re not just embracing the ‘Mo’ spirit; we’re championing the cause of male health. As the statistics reveal, one man succumbs to prostate cancer every 45 minutes in the UK. It’s time to take charge of your well-being and be part of a movement that’s making a difference.
Prostate Cancer –
Our clinic offers a comprehensive Prostate Cancer check, with an experienced doctor committed to your health journey. This thorough examination includes a detailed health discussion covering lifestyle and family history, an internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Early detection is the key, and we’re here to guide you every step of the way.
Testicular Cancer –
Testicular cancer, the most common cancer among young men in the UK, demands attention. Knowledge is power, and understanding the symptoms can be a lifesaver. A lump or swelling, a heavy scrotum, or discomfort in the testicle or scrotum are health signals not to be ignored. At Fleet St. Clinic, we emphasise the importance of awareness and early detection.
Mental Health –
Let’s break the silence surrounding mental health. The Movember Foundation has spearheaded programs globally, fostering resilience and mental well-being in men. It’s not just about growing a mustache; it’s about cultivating conversations that matter.
Now, let’s talk about your health journey with Fleet Street Clinic’s essential men’s health screenings and medicals.
Medical Health Check (From £425) –
Essential
Review your health with one of our experienced GPs. Benefit from a thorough physical examination and carefully selected health checks and blood tests, including thyroid function.
1 hour appointment with a GP – £425
book online
Executive
Check your health from top to toe, with our more enhanced Executive medical, including an audiometry test to assess your hearing, spirometry tests to assess your lung function, and cancer checks and markers.
1.5 hour appointment with a GP – £675
Executive+
For maximum reassurance and peace of mind, consider our most advanced medical. Benefit from advanced health screenings including a sophisticated cardiac (CaRi-Heart) scan, and a bone density DEXA scan.
3 hour appointment with a GP – £3,950
View our medical health checks in more detail and book online.
Prostate Cancer Check (£175)
Prostate cancer is the most commonly diagnosed cancer in men in the UK. Early diagnosis is crucial.
Our prostate cancer check is carried out by an experienced male GP, who’ll conduct a detailed health discussion, internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Swift courier services ensure timely analysis at our nearby pathology laboratory. Our GP will provide you with full support throughout the process and provide aftercare services and referrals if required.
In a world where ‘strong, silent men’ are rewriting their narrative, Movember beckons. Join us at Fleet St. Clinic, where your health is not just a checkup; it’s a commitment to a longer, healthier life.
Book your Appointment now, and let your Mo make a statement for men’s health in London.
According to Prostate Cancer UK, 1 in 8 men will get prostate cancer in their lifetime and it is the most common cancer in men in the UK.
In 2021, around 52,000 men were diagnosed with prostate cancer in the UK alone and the risk of developing it increases with age, as most cases are diagnosed aged 65 and over.
It’s not uncommon for men find out by complete chance, and often it can be too late when the diagnosis is less treatable. For that reason, it’s essential to understand the symptoms, available tests, and the importance of early detection.
What is the Prostate?
The prostate gland is a small, walnut-sized gland located below the bladder and in front of the rectum in males. It plays a key role in the male reproductive system by producing seminal fluid, which nourishes and helps transport sperm during ejaculation.
As men age, the prostate can undergo changes, including enlargement (benign prostatic hyperplasia) or other conditions, such as prostatitis (inflammation) and prostate cancer.
Regular check-ups and awareness of symptoms are important for prostate health.
What is Prostate Cancer?
Prostate cancer occurs when cells in the prostate gland grow uncontrollably.
An enlarged prostate is very common in men over the age of about 50, but having an enlarged prostate is not the same as having prostate cancer.
Having an enlarged prostate doesn’t increase your risk of getting prostate cancer. But it’s possible to have an enlarged prostate and prostate cancer at the same time.
While many men with prostate cancer may not experience symptoms, early detection is vital for effective treatment.
Symptoms of Prostate Cancer
In its early stages, prostate cancer may not cause noticeable symptoms. However, as the disease progresses, some common symptoms include:
- Needing to urinate more often than usual, especially at night
- Difficulty starting or stopping urination
- Weak or interrupted urine flow
- Painful urination or ejaculation
- A feeling that your bladder hasn’t emptied properly
If prostate cancer breaks out of the prostate (locally advanced prostate cancer) or spreads to other parts of the body (advanced prostate cancer), it can cause other symptoms, including:
- Persistent pain in the lower back, hips, or pelvis
- Unexplained weight loss or fatigue
- Blood in urine or semen
- Problems getting or keeping an erection
If you experience any of these symptoms, it’s crucial to consult a healthcare professional for evaluation.
All these symptoms are usually caused by other things that aren’t prostate cancer. But it’s still a good idea to tell your GP about any symptoms so they can find out what is causing them and make sure you get the right treatment, if you need it.
Who Should Consider a Prostate Screening?
- Men aged 50 and older: if you’re at average risk, starting at 50 is recommended.
- Men aged 45 and older: if you have a higher risk, such as a family history of prostate cancer.
Tests for Prostate Cancer at Fleet Street Clinic
Several tests can help confirm the presence of prostate cancer:
- Prostate-Specific Antigen (PSA) Test: This blood test measures the level of PSA, a substance produced by the prostate gland. Elevated PSA levels can indicate prostate cancer, but they can also be elevated due to benign conditions such as an enlarged prostate. A normal PSA indicates that the chance of a prostate cancer is very low.
- Digital Rectal Exam (DRE): During this exam, a doctor manually examines the prostate for any irregularities or lumps. While this test can help identify abnormalities, it is typically used in conjunction with the PSA test.
Consider booking a GP appointment for either of these Prostate Cancer tests, or for a more comprehensive assessment, opt for our Prostate Cancer Check, which includes both tests.
Factors That Can Cause the PSA to be Falsely Raised
Several factors can cause a false elevation in Prostate-Specific Antigen (PSA) levels, potentially leading to misleading test results. Here are common causes:
- Recent Ejaculation: Sexual activity, especially ejaculation, can elevate PSA levels temporarily. Avoid sexual activity for 24–48 hours before a PSA test.
- Prostate Manipulation: Any recent procedures or physical manipulation, such as a digital rectal exam (DRE) or catheter insertion, can elevate PSA levels. Let your doctor know if you’ve had any recent prostate exams or urological procedures.
- Vigorous Exercise: Activities that put pressure on the prostate, like cycling or horseback riding, can raise PSA levels temporarily. Avoid these activities for a f48 hours before the test.
- Prostate Infections or Urinary Tract Infections (UTIs): These infections can cause inflammation and increase PSA levels. Treat infections and allow recovery before testing.
- Benign Prostatic Hyperplasia (BPH): An enlarged prostate from BPH can raise PSA levels even though it’s not cancerous. Make sure your doctor considers this in the interpretation.
- Certain Medications: Some drugs, like testosterone, can increase PSA levels, while others like finasteride (for hair loss or BPH) can decrease it. Inform your doctor of any medications you’re taking.
Avoiding or managing these factors before a PSA test can help improve the accuracy of the results. Always discuss any concerns with your doctor.
You may need additional tests, as listed below, if your PSA is raised or if there is concern from the examination. We can refer you to specialists who may be available for same-day consultations to provide further evaluation.
- Imaging Tests: Additional imaging tests, such as an MRI or CT scan, may be conducted to visualise the prostate gland.
- Biopsy: If initial tests indicate potential cancer, a biopsy is often performed to confirm the diagnosis. During this procedure, a small sample of prostate tissue is removed and examined under a microscope for cancer cells.
Movember, an organisation focused on raising awareness of men’s health issues, including prostate cancer, emphasises the importance of regular check-ups and understanding one’s own health risks. Their campaigns encourage men to talk openly about health issues, promoting early detection and treatment.
Prostate cancer is a serious health concern for men, but awareness and early detection can lead to better outcomes. Regular check-ups and understanding the symptoms are essential steps in addressing this disease.
If you have concerns about prostate cancer or related symptoms, don’t hesitate to seek medical advice by booking a GP appointment. Early action can make a significant difference in your health and well-being.
Related services at Fleet Street Clinic
Prostate Cancer Check
Private GP Appointments
Annual Medical
Blood Tests
October is Breast Cancer Awareness Month
You may notice an increased amount of pink during this month, especially iconic pink ribbons, and it’s for a good reason: October is Breast Cancer Awareness Month.
This annual campaign aims to increase the awareness of the disease and to raise funds for research into its cause, prevention, diagnosis and treatment. With the hope that in the not too distant future, a cure will be found!
Breast Cancer is the most common cancer in the UK. 1 in 8 women in the UK will be diagnosed at some point in their lives.
In the UK, over 55,000 women each year are diagnosed with Breast Cancer which is the most common cancer. Thanks to research, more people are surviving breast cancer than ever before, yet there are still nearly 1,000 women who’ll die of breast cancer each month. Breast cancer is often thought of as something that only affects women, but men can get it in rare cases. It is important for males (especially those over 75 years with a high BMI) to check breast tissue for abnormalities as well.
We will be sharing important information on symptoms, causes and lifestyle alteration you can make to reduce your risk.
We are urging everyone, especially women, to check their breasts regularly and get checked out by a professional if something seems unusual for you.
REMEMBER: The earlier breast cancer is diagnosed, the easier it is to treat and the better the chance of successful treatment.
BREAST CANCER SYMPTOMS TO LOOK OUT FOR:
- a new lump or thickening in your breast, upper chest area or armpit
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
- Unexplained pain in your breast or armpit that’s there all or almost all the time
How to check your breasts
Checking your breasts yourself means you’ll get to know what is “normal” for you. As a society we are probably not that familiar with how our body currently is and so that makes it difficult to know what subtle changes happen. It’s most likely that unless a dramatic change has occurred a subtle change will go unnoticed.
So, how do you check your breasts?
There is no special technique and you don’t need any training to start checking your breasts. It may feel like you’re unsure what you’re doing but get to know your body and any breast check is better than no breast check.
The easiest and most accurate way is to divide the breasts into four quadrants; the upper outer quadrant, outer lower quadrant, inner lower quadrant and inner upper quadrant. Examine each quadrant with the flat of your hand. It is important to do this regularly so that you are familiar with what each breast feels like normally. That way, should you notice any changes, (hopefully not), you will pick them up straight away and changes won’t go unnoticed. It is important to remember to check your armpits as well. It is surprising how many breast lumps are discovered after an “axillary” or armpit lymph node is found and checked.
Breast Cancer Now advises the TLC method – “touch, look and check”.
Touch: Can you feel anything new or unusual?
Look: Does anything look different?
Check: Any changes with your GP
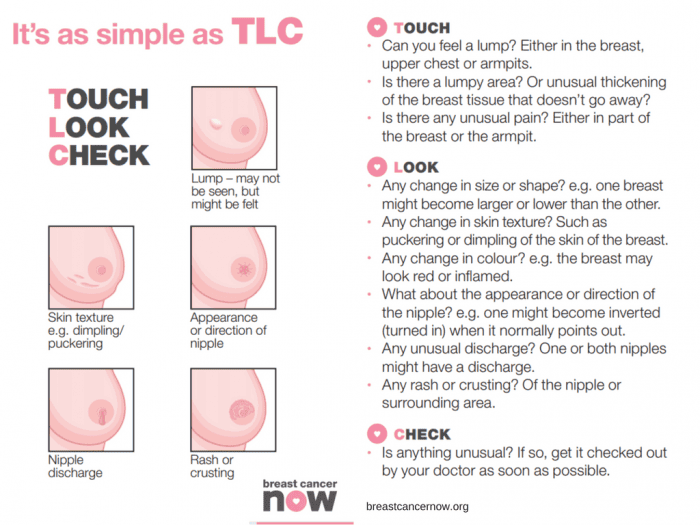
You should check your breasts Regularly
Get to know your “normal” by checking your breasts regularly. Get in the habit of checking your breasts at least every month. It can be easier whilst in the bath or shower.
Your breasts can change throughout your life for many reasons – like the menopause, pregnancy and breastfeeding, or puberty. So, if you check them regularly, you’ll be able to spot any new or unusual changes that should be checked out by a GP.
For young and pre-menopausal women it is advised to check mid-cycle (a week after their period finishes) if there are any changes this requires checking with your GP.
As older women are of a higher risk of breast cancer, due to age, it is advised they check even more frequently. Older women should check on a monthly basis without exception. It is advised for men to check also.
Any lump requires attention and checking with your GP immediately.
In addition to regular self-checks, it is important to never miss a mammogram appointment. They may be painful and momentarily uncomfortable, but a mammogram can save your life. If you have a long wait for a mammogram, are unable to access an appointment or just want an additional check, contact the Fleet Street Clinic and we should be pleased to help.
What are the causes of breast cancer?
There are several factors that contribute to increasing your risk of developing breast cancer. There is no single cause, and has to do with our lifestyle, environment and genetics. There are factors which we simply cannot control such as getting older, family history, inherited genes, dense breast tissue, hormones and age at which period started and stopped. However, there are some lifestyle choices that if altered can reduce your risk of breast cancer.
Lifestyle change that will reduce your risk of breast cancer
1. Your weight
Being overweight or obese has a high risk of breast cancer in both men and women (especially after menopause). You can work out your ideal weight using a BMI (Body Mass Index) calculator, this checks your height and weight to see if you are at a healthy weight. For the majority of adults an ideal BMI ranges from 18.5 to 24.9. A BMI between 25 – 30 means overweight. Obesity means a BMI of 30 and above.
2. How much alcohol you drink
Alcohol consumption increases the risk of breast cancer. The risk is greater with each extra unit per day, the latest UK guidelines state no more than 14 units a week.
3. How much exercise you do
Being inactive contributes to a small increased risk of breast cancer, this qualifies as doing less than 150min of moderate activity on a weekly basis. This does not necessarily mean sport and exercise, anything that makes you warmer and out of breath counts.
Throughout October we’ll be highlighting the reasons to support this campaign across our social media platforms. We will be sharing inspirational stories from those who have survived the disease and those who are currently battling. We will also hear from those who have supported a suffering loved one during treatment. Sharing these stories humanises the disease and can provide support/tips for those who may be struggling with a current diagnosis. We will be sharing ways of checking for early warning signs. We’ll also be encouraging all to undertake a Well-Woman or Well-Man health checks. Both of which contain a breast examination.
At Fleet Street Clinic, we specialise in women’s health and have four female GPs on-site to facilitate well-woman health checks. Our Executive Well Woman medical is focused on protecting your well-being and involves a full examination including breast examinations and cervical screen tests. Our comprehensive medical is designed to screen for health problems at the earliest possible stage.
Book Your Well Woman Medical Online. Or if you notice any changes to your breast or have any concerns, you should book a GP appointment as soon as possible.
_______________
To find out more from Breast Cancer Now, visit breastcancernow.org
Women between the ages of 25 and 64 are invited for regular cervical screenings where a healthcare professional looks at the health of the cervix to detect any cell changes or abnormalities. However, in 2022-2023, the number of women who attended their cervical screen fell. Nearly a third of the women invited to do their cervical screen didn’t attend their appointments, this is around 4.6 million women, a deeply concerning number, as over 3000 women are diagnosed with cervical cancer each year and 99.8% of those cases are preventable. Prevention is better than curing, and the earlier you are aware of any cell changes, the easier it is to treat.
Why do some women not attend their cervical screenings?
One of our general practitioners, Dr Belinda Griffiths, has found that in her experience women don’t attend their cervical screenings for a number of reasons including: difficulties with taking time off work for a GP appointment, fear of embarrassment, and fear of the process being uncomfortable or painful.
However, to combat these concerns, the NHS has launched at-home HPV kits. Dr Griffiths explains how they work – “The HPV test is highly sensitive so it separates out those who are HPV-positive and HPV-negative. Those who are HPV-negative will be considered ‘low risk’ for cervical cancer and will be asked to do a future test. Those who are HPV-positive will be deemed ‘high risk’ and be asked to attend for follow-up with a clinician whereby they will conduct a cervical screening to check the health of their cervix and investigate if any abnormal cells are present.”
These new tests are the same process as at-home STI tests whereby a simple swab collects the sample from the vagina. Having the option of this sort of test at home removes the fear some women may have surrounding the slightly more intrusive cervical screen.
What is HPV?
HPV (human papillomavirus) is a common virus passed on via skin-to-skin contact, usually through genital contact. There are many types of HPV, most of which are harmless, don’t usually cause any symptoms and the infection will go away on its own. However, others are deemed ‘high risk’ as they can persist and cause cell changes which can lead to cancer. It is thought that these ‘high risk’ HPV strains are responsible for around 80% of cervical cancer cases, making the detection of HPV all the more important.
How can you prevent HPV?
You can be protected from certain HPV strains through vaccination. There are two HPV vaccines currently available in the UK: Gardasil which protects against 4 strains of HPV used in the NHS and the vaccine used here at the Fleet Street Clinic, Gardasil-9, which protects against 9 of the high-risk HPV strains.
When can you be vaccinated against HPV?
The NHS now routinely offers the Gardasil vaccine to girls and boys around age 12/13, before the age people generally become sexually active. However, the vaccination programme only came into full force in 2019, meaning many people are currently unvaccinated. It should be pointed out that adults can get vaccinated at any age and even if you have already been exposed to HPV, the vaccine can still offer protection against other strains to which you have not yet been exposed.
It is a particularly good idea for people to get vaccinated before they attend university or before they go travelling on a ‘gap year’, as these are typically times where young people are more sexually active and therefore more likely to be exposed to HPV.
It is important to note that getting the HPV vaccination most certainly doesn’t mean missing or not participating in HPV tests or cervical screenings. A combination of these preventative measures gives you the highest possible chance of preventing cervical cancer.
Book your Cervical Screen or HPV vaccine online today.
Ovarian cancer is a disease that affects thousands of women worldwide each year and is often referred to as the silent killer due to its silent symptoms, including bloating, abdominal pain, and changes in bowel habits, which are often mistaken for other conditions. Despite advances in treatment, the disease remains a major public health concern due to its high mortality rate. However, new data from a study funded by Cancer Research UK (CRUK) suggests that a seemingly unlikely tool – supermarket loyalty card surveillance – could help spot ovarian cancer early, when it is most treatable.
The study, which was published in JMIR Public Health and Surveillance, analysed data from supermarket loyalty card programs and found that changes in purchasing behaviour could be used to detect early signs of ovarian cancer.
Researchers found that women with ovarian cancer often experience a decline in their appetite and energy levels, which can result in changes in their grocery shopping habits. By monitoring these changes in real-time, it may be possible to detect the disease early and improve the chances of successful treatment.
This is an exciting development in the fight against ovarian cancer, and one that has the potential to revolutionise the way we detect and treat the disease. By leveraging the vast amounts of data generated by supermarket card programs, healthcare providers and public health officials could identify women who may be at risk of ovarian cancer and encourage them to seek early medical attention. This could help to improve the outcomes of treatment and reduce the overall impact of the disease on society.
One of the key benefits of supermarket card surveillance is that it allows for continuous monitoring of women’s purchasing behaviour. This means that healthcare providers can receive real-time alerts when changes occur, allowing them to act quickly and effectively. This level of monitoring is not possible with traditional screening methods, which are typically performed only once or twice per year and may miss early signs of the disease.
Additionally, supermarket card surveillance is a cost-effective way to monitor the population for signs of ovarian cancer. Unlike other screening methods, it does not require specialised equipment or trained personnel, and the cost of monitoring is negligible compared to the cost of treatment. This could make it possible to implement large-scale screening programs, even in resource-limited settings, and reach a greater number of women who may be at risk of ovarian cancer.
Of course, it’s important to keep in mind that supermarket card surveillance is not a substitute for traditional screening methods, such as ultrasound or CA-125 tests, or for regular self-reporting and awareness of symptoms. However, it could be used as an adjunct to these methods, helping to improve the accuracy of screening and reduce the number of missed cases.
Another important consideration is the privacy of women whose purchasing behaviour is being monitored. While supermarket card surveillance has the potential to help detect ovarian cancer early, it is important to ensure that women’s privacy is protected and that the data collected is used only for medical purposes. Healthcare providers and public health officials should work together to ensure that any monitoring programs are transparent, secure, and in compliance with privacy regulations.
In conclusion, the findings of this study are a major step forward in the fight against ovarian cancer. By leveraging supermarket card surveillance, it may be possible to detect the disease early, when it is most treatable, and improve the outcomes of treatment for women around the world. However, it is important to carefully consider the privacy implications of monitoring purchasing behaviour and to ensure that any programs implemented are transparent, secure, and in compliance with privacy regulations. The early detection of ovarian cancer is a critical goal, and we hope that this research will help to pave the way for new and innovative approaches to screening and treatment. Additionally, women should be encouraged to seek medical attention if they notice any changes.
Reference Source: https://publichealth.jmir.org/2023/1/e41762
Related services available at Fleet Street Clinic:
How much would you pay to prevent bowel cancer?
£1,000? £500? £200? £100? Or just £45?
Everyone knows a friend or relative who has suffered from or unfortunately, died of bowel cancer. Also known as colorectal cancer, bowel cancer is the fourth most common cancer in the UK but the second biggest killer. More than 16,000 people die from bowel cancer in the UK every year. Similar to other types of cancer, bowel cancer is treatable and curable especially if diagnosed early.
The earlier it is detected, the greater the chance of survival.
However, the survival rate drops significantly as the disease develops. The optimal test for bowel cancer is a colonoscopy, but it is an invasive test which checks the lining of the bowel for cancer. Due to the invasive nature of this test, it usually happens following a positive screening result or if a person has multiple symptoms so as not to cause unnecessary discomfort is symptoms are say. related to another health issue.
As bowel cancer symptoms are also indicators for a wide range of gastroenterological (digestive system) disorders, a simpler, non-invasive FIT stool test (faecal immunochemical test) can be the first step for patients with concerns and/or symptoms such as lower abdominal symptoms such as abdominal pain, rectal bleeding and/or a change in bowel habits prior to a colonoscopy.
For those who are healthy with no symptoms, FIT screening is an important way of testing healthy people to see if they show any early signs of cancer.
Bowel Cancer Screening
It can be challenging to differentiate between patients with serious bowel disease such as bowel cancer, from those with benign functional or diet-related conditions, such as IBS – irritable bowel syndrome, and minor colorectal diseases such as haemorrhoids.
A FIT test or faecal immunochemical test, looks for blood in the stool, an early sign of bowel cancer. It is a simple and effective non-invasive test.
If there is blood present, this can indicate the presence of abnormalities in the bowel, which over time may develop into cancer. Patients with a positive FIT result are then referred for further investigation by colonoscopy.
A FIT test does not diagnose bowel cancer, but it’s a simple way to find out if you need further tests. Introducing regular bowel cancer screening into your health checks will reduce the risk of dying from bowel cancer.
Are all FIT Tests the same?
The short answer, no.
The sensitivity of a FIT test to detect blood in stools can be adjusted to be more or less accurate. The lower the threshold, the more sensitive the test is to blood in the stools meaning the earlier abnormalities can be identified.
Where you live in the UK dictates the FIT tests available to you, see below:
NHS Scotland:
Age range: 50-74 years – Automatic invite for screenings every 2 years / 75+ done on request
Blood sensitivity threshold: 80ug per g of stool
NHS England & Wales:
Age range: 60-74 years – Automatic invite for screenings every 2 years / 75+ done on request
Blood sensitivity threshold: 120ug per g of stool
Fleet Street Clinic:
Age range: Screening recommended from 40 years onwards. Available from 20 years if symptoms are present and for individuals with a family history of bowel cancer of one or more first-degree relatives (sibling, parent or child).
Blood sensitivity threshold: 20ug per g of stool.
A big difference!
Why is this so important?
If early detection is a matter of life and death when it comes to bowel cancer then the optimum FIT test has to have the lowest sensitivity threshold to provide the most accurate diagnosis. The more sensitive the FIT screening, the more cancer and precancerous polyps can be detected, especially at an early stage of abnormality.
At Fleet Street Clinic, we are more likely to pick up blood in the stool by a factor of 4 compared to NHS Scotland and by a factor of 6 in comparison to NHS England & Wales, all without the rigid age limitations.
Bowel Cancer Screening at Fleet Street Clinic
The FIT test at Fleet Street Clinic has the lowest sensitivity threshold on the market right now. It is an easy, quick test which costs just ££70* with results within a week.
Surely it is worth it?
If by any chance your test is positive, we provide a letter of referral which can be given to your GP (Private or NHS) or used at one of the referral centres we recommend for private colonoscopy. The choice is yours.
Tell your friends about this life-saving test and save a life – It could be your own.
If you’re concerned about bowel cancer, then it’s important to book a 15-minute GP appointment to speak to a doctor – you can book online.
* A 15-minute GP appointment costing £108 is required in addition to the cost of the FIT test.
MARCH IS OVARIAN CANCER AWARENESS MONTH
A vital month raising awareness of ovarian cancer to improve early diagnosis to save lives.
More women died from ovarian cancer in the UK (4,227) than from all other gynaecological cancers combined in 2016, according to Cancer Research UK. However, worryingly one in five women in the UK (22%) mistakenly believe that a smear test (cervical screening) can detect ovarian cancer, according to research Target Ovarian Cancer carried out with YouGov.
We are committed to raising awareness of the disease.
Speak to one of our female GP’s about any concerns you may have about your gynaecological history and your families medical history. During your consultation, we will also conduct a breast check and pelvic examination.
“In the UK a woman dies every two hours from ovarian cancer, but the earlier the diagnosis the better the chances are”
Professor Hani Gabra – Director of Ovarian Cancer Action Research Centre
What is ovarian cancer?
Ovarian cancer is when abnormal cells in the ovary begin to grow and divide in an uncontrolled way and eventually form a growth (tumour). Every year 7,300 women in the UK are diagnosed with ovarian cancer.
Who can get ovarian cancer?
The risk of developing ovarian cancer increases as you get older. The most common type of ovarian cancer is epithelial ovarian cancer, this usually occurs in women older than 50 years old. We don’t know exactly what causes epithelial ovarian cancer. But some factors may increase or reduce the risk.
Factors that increase the risk include:
- getting older
- inherited faulty genes
- having breast cancer before
Factors that may reduce the risk include:
- taking the contraceptive pill
- having children
- breastfeeding
Ovarian Cancer is notoriously difficult to spot.
With non-specific symptoms in the early stages. It is hoped that this new method of early diagnosis could help save lives.
How to recognise the symptoms of Ovarian Cancer:
Early Ovarian Cancer symptoms can be similar to those of other conditions, these some to watch out for:
- Persistent bloating – not bloating that comes and goes
- Pain in the lower stomach and pelvis
- Difficulty Eating and feeling full quickly
- Back pain
- Fatigue
- Change in bowel habits
What should you do if you’re worried?
It is important to contact your GP as soon as possible if you spot any symptoms that are abnormal for you.
We understand talking about your concerns and having an examination can be quite worrying and for some, embarrassing, therefore, to make you as comfortable as possible, all our well woman services are booked with a female GP.
There is an Ovarian Cancer Blood Test – CA 125 available
Levels of protein CA125 in the blood are recognised as a marker for ovarian cancer. This simple and effective blood test will detect early stages of ovarian cancer. You can either have this as a stand-alone blood test or add it on to your medical for an additional cost. Please inquire for prices..
Links:
Target Ovarian Cancer
Cancer Research UK
For more information about Fleet Street Clinic’s Women’s Health Services.
You can also book a GP appointment online.
This week is Cervical Cancer Prevention Week (#CCPW) and we’d like to remind all our patients that cervical cancer can be fatal – It is the most common cancer in women aged 35 and under.
Current UK statistics state:
> 2 women lose their lives to the disease every day
> 9 women are diagnosed with cervical cancer every day
> 75% of cervical cancers can be prevented by a smear test
Thousands of lives can be saved every year with better awareness and understanding of the symptoms of cervical cancer. Regular smear tests and having the HPV vaccine can dramatically decrease your chances of developing cervical cancer and will also assist in early detection.
Smear tests are extremely important and a major contributing factor to lowering the number of cervical cancer cases seen each year. On average, cervical screening helps save the lives of approximately 4,500 women in England every year, however, 1 in 4 women still don’t attend their smear test.

Smear tests are a method of detecting abnormal cells on the cervix, (the entrance to the womb). The detection and removal of abnormal cells can prevent cervical cancer from developing. As with all cancers, the earlier a problem is detected, the better the patient’s outcome.
Information on Cervical Cancer
Cervical cancer is not thought to be hereditary.
Cervical screening is not a test for cancer as screening programmes help to prevent cancer by detecting early abnormalities in the cervix, so they can be treated. If these abnormalities are left untreated they can lead to cancer of the cervix (the neck of the womb).
Symptoms:

For more information: www.jostrust.org.uk
November is Mouth Cancer Awareness Month, and Fleet Street Clinic has collaborated with the charity campaign MouthCancer.org to help raise awareness of the disease.
For more information about Mouth Cancer, you can read the Q&A’s below.
What is Mouth cancer?
Mouth cancer relates to cancer found in the lips, tongue, cheek and throat.
There are, on average, almost 7,800 new cases of mouth cancer diagnosed in the UK each year. The number of new cases of mouth cancer is on the increase, and in the UK has increased by over half in the last decade alone.
Who is at risk?
Mouth cancer is twice as common in men than in women, though an increasing number of women are being diagnosed with the disease. Age is a factor, with people over the age of 40 more likely to be diagnosed, though more young people are now being affected than previously.
People with mouth cancer are more likely to die than those having cervical cancer or melanoma skin cancer. Prognosis is good if the disease is caught early.
What can cause mouth cancer?
Although mouth cancer can affect anybody, around 91% of all diagnoses are linked to lifestyle. This means that by amending our lifestyle choices, we can help cut the chances of developing mouth cancer.
There are many known contributors to mouth cancer:
- Tobacco
- Alcohol
Many cases of mouth cancer are linked to tobacco and alcohol.
If tobacco and alcohol are consumed together the risk is even greater.
- Over-exposure to sunlight can also increase the risk of cancer of the lips.
- Poor diet is linked to a third of all cancer cases. Book a Dietitian Consultation
- Experts suggest the Human Papilloma Virus (HPV), transmitted through oral sex, could overtake tobacco and alcohol as the main risk factor within the coming decade. Book Your HPV Vaccine
What is the link between HPV and cancer?
There’s growing evidence that an increasing proportion of cancer is caused by HPV infection in the mouth. Around 1 in 4 mouth cancers and 1 in 3 throat cancers are HPV-related, but in younger patients, most throat cancers are now HPV-related.
HPV doesn’t directly give you cancer, but it causes changes in the cells it’s infected (for example, in the throat or cervix) and these cells can then become cancerous.
The HPV vaccine, Gardasil 9 is available at Fleet Street Clinic for both girls and boys. The vaccine was developed to fight cervical cancer, but it is likely that it’ll also help to reduce the rates of mouth cancer.
It is advisable to give the HPV vaccine before sexual activity starts to get the best protection. The underlying principle being there has been no exposure to any HPV strains yet. You can, however, receive the vaccination later on in life, this is down to personal choice. We’d recommend a GP consultation to discuss the HPV vaccine prior to booking.
More information on Gardasil 9.
What are the signs of mouth cancer?
Mouth cancer can appear in different forms and can affect all parts of the mouth, tongue and lips. Symptoms of mouth cancer include:
- A painless mouth ulcer that does not heal normally
- White or red patch in the mouth or on the tongue
- Any unusual lumps or swellings that linger
- 1 or more mouth ulcers that don’t heal after 3 weeks
- Pain when swallowing
- A feeling as though something’s stuck in your throat
Be mouth aware and look for changes in the mouth:
It is important to visit your dentist or your GP if these areas do not heal within three weeks.
How can mouth cancer be detected early?
Mouth cancer can often be spotted in its early stages by your dentist during a thorough mouth examination. If mouth cancer is recognised early, then the chances of a cure are good.
It is also advised to self-check regularly for any noticeable changes in your mouth, the inside of your cheeks, the front and sides of your neck, colour and texture changes of your tongue, changes to your lips and finally, lumps and swellings on your head and neck.
How can I keep my mouth healthy?
- It is important to visit your dentist regularly, as often as they recommend, even if you wear dentures. This is especially important if you smoke and drink alcohol.
- When brushing your teeth, look out for any changes in your mouth, and report any red or white patches, or ulcers, that have not cleared up within three weeks.
- When exposed to the sun, be sure to use a good protective sun cream, and put the correct type of barrier cream on your lips.
- A good diet, rich in vitamins A, C and E, provides protection against the development of mouth cancer. Plenty of fruit and vegetables help the body to protect itself, in general, from most cancers.
- Cut down on your smoking and drinking.
If you have any concerns about mouth cancer, you can book a GP appointment or a dental appointment with Temple Dental.
With thanks to mouthcancerawareness.org
Statistics via Mouth Cancer Foundation Org
Breast Cancer Now’s ‘Wear it Pink’ day is one of the biggest fundraising events in the UK.
Thousands of amazing people will ‘Wear It Pink’ in their communities, schools or workplaces for the UK’s largest breast cancer charity, Breast Cancer Now. This Friday 19th October the staff of Fleet Street will show off their best pink garments to raise awareness and show solidarity for such a great charity.
‘’This year, 55,000 women will hear the words “it’s breast cancer”
Breast Cancer Now supports nearly 450 of the world’s best researchers across the UK and Ireland. Working together to help prevent breast cancer, help improve the lives of those dealing with it now and most importantly stop people from dying from the disease. Research holds the key to a future where all that changes. Ensuring women get to enjoy their best life whether that be watching their children grow up or travelling the globe. It’s about making sure women are always able to create a lifetime of memories with the people they love.
The Fleet Street Clinic is championing Breast Cancer Now’s goal, that by 2050, everyone who develops breast cancer will live – and live well. By our staff wearing pink, raising awareness and donating we can help get there and make life-saving research happen.
Well Woman Services
We have four female GPs specialising in women’s health. Women’s health is a focus for us, and one of our highest priorities.
Our Well Woman health checks are focused on protecting your well-being and meeting your exact needs. Each comprehensive medical is tailored to your circumstances and designed to screen for health problems at the earliest possible stage.
Well-woman health checks include:
- Recording your height, weight and body mass index (BMI)
- Blood pressure
- Breast examination (and instruction on breast self-examination)
- Cervical smear test
- Pelvic examination
- Urine test
- Blood tests