Month: May 2019
Parents are being urged to get their children vaccinated for measles, mumps and rubella following outbreaks of measles across Europe:
Anyone who is eligible to get vaccinated should get the MMR vaccine.
A measles outbreak across Europe has left UK officials urging parents to get their children vaccinated for measles, mumps and rubella. As measles is highly infectious, anyone who has not received 2 doses of the MMR vaccine is at risk. Particularly those unvaccinated people travelling to countries where there are currently large outbreaks of measles.
In the first three months of this year, there have been 231 confirmed cases of measles and 795 of mumps. While Public Health England (PHE) figures showed while measles cases were lower than the 265 reported during the same period last year, they had more than doubled compared to the 97 reported between October and December. The number of mumps cases has nearly tripled compared to the 275 cases during the first three months of 2018. No new cases of rubella have been reported.
PHE has now appealed to parents to make sure their children receive the MMR vaccine when it’s offered, or to get a GP appointment booked if they missed it. Officials have also warned that not only is measles highly contagious, but it can also kill a child if they are not vaccinated. Anyone who has not received two doses of MMR vaccine is at risk of measles as it is highly contagious.
There have been 3,789 cases of measles in Europe during the first three months of this year, according to the European Centre for Disease Prevention and Control. The highest numbers were in Romania, France, Poland and Lithuania.
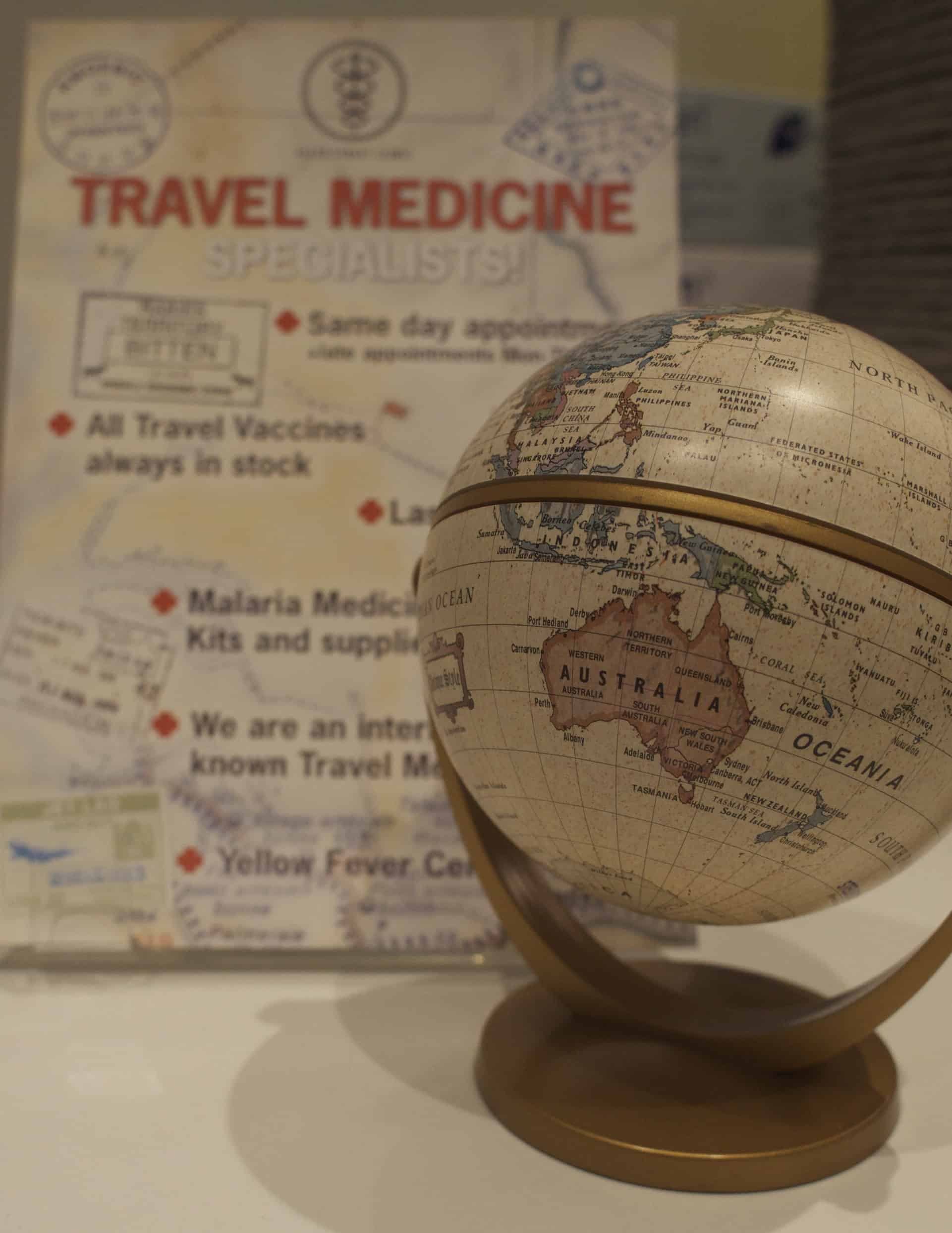
Advice for travellers
For all those planning to travel to Europe, make sure you are up-to-date with all currently recommended UK vaccines. This includes two doses of the MMR vaccine for protection against measles, mumps and rubella.
Anyone who is not sure if they are protected should check with their GP practice. Vaccination is usually done within your childhood vaccinations. However, the MMR vaccine is available to all adults and children who have not had their two-dose course. In some cases, the MMR vaccine can be offered to babies from six months of age. Cases such as travelling to countries where measles is common, or during an outbreak situation. Book a travel consultation with our travel nurse for advice on the best option for your children before you travel.
Head of immunisation at PHE, Dr Mary Ramsay, warned with measles outbreaks across parts of Europe, families should make sure they are vaccinated before travelling. ‘There are measles outbreaks happening across Europe so if you are planning to travel, make sure you check with your GP and catch-up if needed.’
Herd immunity
Measles elimination can only be sustained by maintaining and improving coverage of MMR vaccine in children, and by using all opportunities to catch up older children and adults who missed getting the MMR vaccine.
To achieve herd immunity for measles at least 90 to 95 per cent of the population needs to be fully protected. PHE said 94.9 per cent of eligible children aged five received their first dose of MMR in quarter 4 of 2018. However, the second dose of protection falls to 87.4 per cent for children aged five.
Fleet Street Clinic’s medical director, Dr Richard Dawood explains, ‘When the rate of vaccination in the general population falls below 95%, outbreaks occur and can easily spread, with the highest impact on those most vulnerable populations, undermining years of hard work around the world to bring measles under control.’
Vaccination against Measles, Mumps & Rubella
One dose of the MMR vaccine is about 90 to 95 per cent effective at preventing measles. Protection rises to around 99 per cent after the second dose. Two doses of MMR in a lifetime are needed for a person to be considered fully protected.
The MMR vaccine schedule:
- Two doses, to be given at least 4 weeks apart.
- If the first dose is given before 12 months of age (due to the need for early protection), this should be discounted and the child should continue to receive 2 doses as per the normal schedule.
- The vaccine is also available to all adults and children who are not up-to-date with their 2 doses.
Anyone who is not sure if they are fully vaccinated should check with their GP.
You can book all vaccination appointments online.
Bolivia is famous for its salt flats and varied terrain spanning over the Andes Mountains, the Atacama Desert and Amazon Basin rainforest. Located in South America, the climate varies drastically from one eco-region to the other. Travelling around Bolivia you’ll experience different climatic extremes, such as humid tropical climates to subtropical climates to desert-polar climates. It is important to seek travel advice before travelling as medical advice can vary dependent on the area/s you plan to visit.
Our general advice includes:
Vaccines
Routine immunisations are a high priority; it is good to check that they are all up-to-date before travelling anywhere. Given the current worldwide outbreaks, we strongly recommend checking your immunity status to measles. A simple immunity test can confirm all those who are unable to source vaccine proof. The best protection against measles is having 2 doses of a measles-containing vaccination, such as the MMR.
Travel vaccinations for Bolivia vary depending on where you plan to travel, and what you plan to do. It is best to book a consultation with a travel nurse to discuss your upcoming adventure. They will assess what risks you will potentially be exposed to. From this, they can develop a bespoke treatment plan specifically for your holiday.
As a minimum, travellers should be protected against Hepatitis A, and diphtheria, tetanus and polio. Certain travellers may consider vaccinations against typhoid, Rabies, Hepatitis B and Yellow Fever.
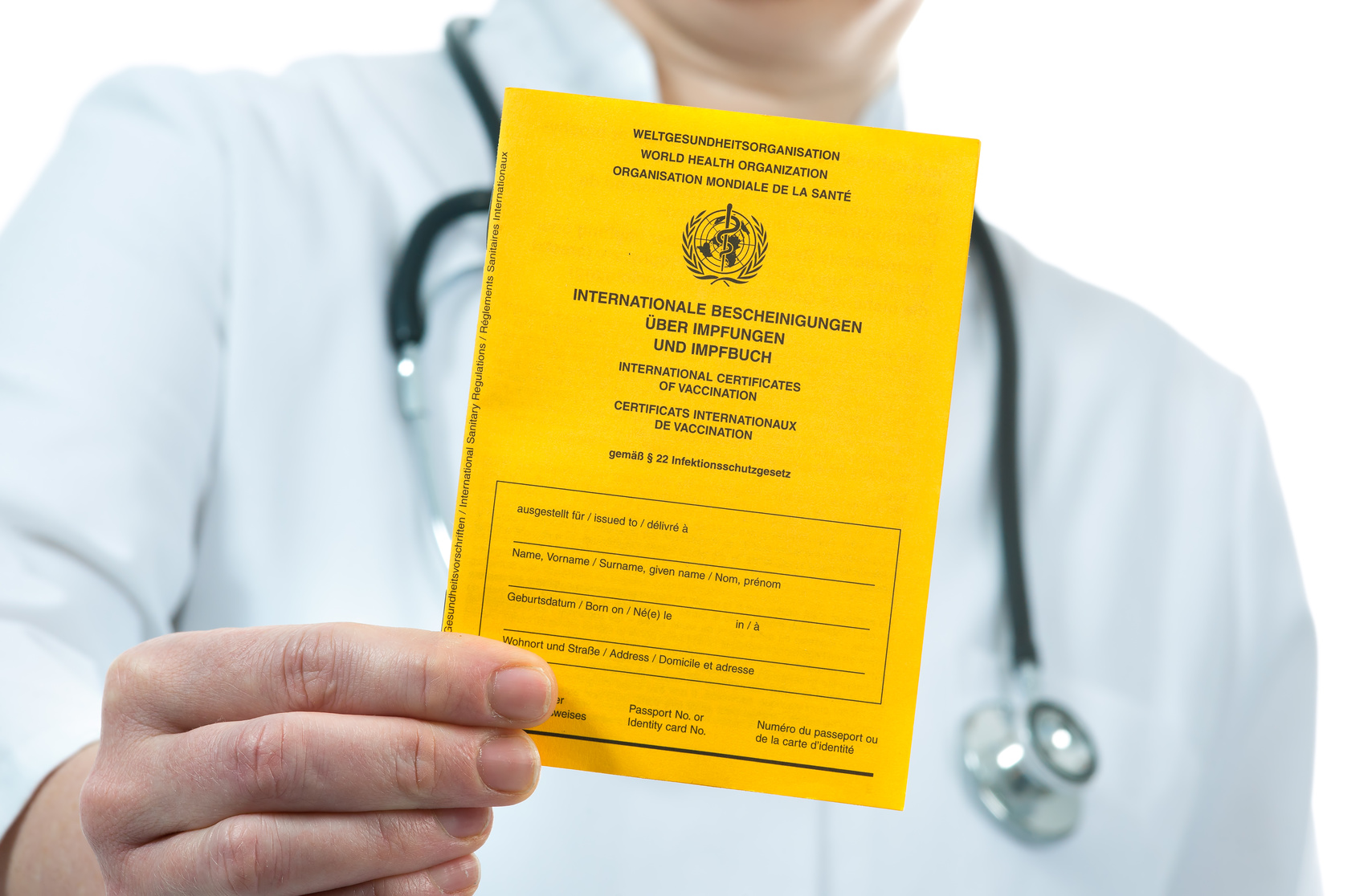
Yellow Fever
Yellow Fever is an unpleasant virus spread by the Aedes aegypti mosquito. This mosquito tends to bite during the day and is present in many lowland areas of South America and in all areas below 2,300m in Bolivia. Travellers who intend to visit the lowlands, such as the Chaco, Santa Cruz district and the Amazon may be advised to have the vaccine.

If your travel route includes other South American countries, you may also require the vaccination and an accompanying Yellow Fever Certificate in order to enter that country. The vaccination is not suitable for everybody. A careful risk assessment should be undertaken by a practitioner that specialises in the vaccine. Yellow Fever can only be given at designated Yellow Fever vaccination centres (YFVCs) – Fleet Street Clinic is a registered clinic.
Altitude
Bolivia is home to some of the highest peaks of the Andes mountains, with elevations of over 6,000m. The frequently visited cities of La Paz, Potosi and Uyuni all soar over 3,500m, making altitude sickness a real risk. The risk can be reduced by ensuring you stay hydrated, plan a slow ascent and factor in some acclimatisation days. Acetazolamide (Diamox) can be used to help aid the process. Book a pre-travel assessment and speak to a travel nurse about your options.
Insects
Mosquitoes, bugs and flies do more than just bite. They have the ability to transmit diseases that aren’t always preventable by vaccination or medication. Illnesses such as dengue fever, chikungunya, Zika, yellow fever, malaria and sleeping sickness are a few risks.
The best prevention is to entirely avoid mosquito bites. Cover up as much as possible and apply a minimum concentration of 50% DEET to any areas of exposed skin. Spraying your clothes with permethrin before travelling can provide extra protection. Sleep under a mosquito net, especially, if you plan to stay anywhere remote or rural.
See our Ultimate Bug Kit.
Malaria
Malaria occurs in the northern parts of Bolivia, in the Beni and Pando districts. Travellers heading to these areas should ensure they take anti-malarial medication. Mosquitoes that spread malaria are predominantly night-time biters. So, extra precautions should be taken between dusk and dawn. Any travellers who experience fever or flu-like symptoms on return from their trip should ensure they get tested for malaria, as unfortunately, no single prevention method is 100% effective.
First Aid
Whilst medical services and pharmacies are available in bigger cities, access to basic services is limited or even non-existent in the remote regions. Travel prepared and take a small medical kit that can treat basic complaints. Pack painkillers, antiseptic cream, plasters or dressing, and medication in case you suffer from an upset stomach. Head over to our online shop to purchase an essential first aid medical kit. This contains all your travelling medical essentials.
If you are prone to allergies, a non-drowsy antihistamine is helpful. Furthermore, if you take prescription medication, be sure to pack enough to last you for your entire trip.
Book your travel appointment today
By Anna Chapman | Travel Nurse | May 2019
Travel nurse Anna takes us on a journey to Tel Aviv. A city on Israel’s Mediterranean coast steeped in history and a vibrant cultural scene. From vaccinations to sun protection follow the top tips to travel safely.
Vaccines
All travellers are advised to ensure that they are in date with their routine vaccinations. Measles outbreaks have been reported in Israel since September 2018, and there are concerns that the increase of travellers heading to Israel for Passover in mid-April could see cases rise. Travellers should ensure that they have received two doses of measles vaccination (often referred to as the MMR) prior to departure.
Other travel vaccinations to be considered are diphtheria, tetanus and polio, and Hepatitis A. Some travellers may also wish to consider vaccinations against Hepatitis B and Rabies. It is always best to discuss which vaccinations are necessary for your trip with a travel nurse.
However, vaccinations cannot protect you from many diseases and dangers in Israel, the risk can be reduced through your behaviours…
Sun
Israel lies within the sub-tropical region with a Mediterranean climate. Summer temperatures can reach 40 degrees Celsius, and even higher in the Negev desert. Don’t let the Mediterranean summer breezes deceive you and stay sun safe. Keep hydrated, wear a high factor sunscreen and avoid the suns rays between 11am-3pm when at its strongest.
Food and Water
Israel is foodie heaven but travellers should still maintain good food and water practices to avoid tummy trouble whilst away. Avoid tap water and ice made from tap water: stick to bottled water. Ensure you wash your hands thoroughly before eating and after using the toilet. Ensure all food you eat is cooked thoroughly and served straight to you. For those who would still like the freedom to eat and drink without worry, it is advisable to carry a gastro kit with you. Inside will be various medications that can assist with travellers’ diarrhoea, should it occur.
Insects
Mosquitoes and sand flies can be particularly problematic during the summer months. Not only can their bites cause irritation, but they can also spread diseases such as West Nile Fever, dengue fever and leishmaniasis. There are no specific vaccinations and preventative treatments for these diseases, and bite avoidance is the only way. Try and cover up especially between dusk and dawn, and wear a good insect repellant that contains at least 50% DEET.
See our Ultimate Bug Kit.
From Red to Dead…
From the riches of the coral seas in the red to the abyss of the dead sea, take sensible precautions when taking the plunge. The dead sea lies 413m below sea level and is actually rather tricky to swim in. Tourist usually come to float on its surface as the high salt content makes it hard to submerge. Be careful. Cover any cuts you have with waterproof plasters to avoid a sharp sting. Do not splash when in the water, as it may cause injury or irritation to your eye if it enters. If you wear contact lenses, it’s best to swap to your glasses.
You can book all vaccination appointments or travel consultations online.
By Anna Chapman | Travel Nurse | May 2019
What is HPV?
Human Papillomavirus, or HPV, is the name of a group of viruses with around 200 different types, that is most commonly passed on via genital contact.
Although HPV is highly common, 90% of HPV infections go away by themselves and do not cause any harm. Most people with HPV never develop symptoms or health problems.
However, it is possible for HPV infections to persist and cause cellular change in your body. This can lead to:
- Cancer of the cervix, vulva, and vagina in women
- Precancerous lesions in men and women
- Genital warts in men and women
- Head and neck cancers in men and women
HPV vaccines have a well-established role in preventing cervical cancers as well as these other aforementioned conditions.
Who Should Be Vaccinated against HPV?
In theory, HPV vaccines are best given to young people before they become sexually active, and therefore before they can be exposed to HPV.
Individuals who are already sexually active might also benefit as they may not have yet acquired all of the HPV strains covered by the vaccine. Patients aged under 16 can only be vaccinated with their parents present.
Why Boys should receive the HPV Vaccine
- About 15% of UK girls who are eligible for vaccination are currently not receiving both doses. This figure is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries which have no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high: treating anogenital warts alone in the UK is estimated to cost £58 million a year, while the additional cost of vaccinating boys has been estimated to cost about £20 million a year
Source: HPV Action
To book an HPV vaccination for yourself or your child, you can book an appointment online. Or find out more information about HPV here.
Brazil: Yellow Fever
The incidence of Yellow Fever cases in Brazil has been increasing recently, with over 1000 cases of Yellow Fever in Brazil since July 2017. The cases were reported in Sao Paolo, Minas Gerais, Rio de Janeiro, Espiritu Santo and Distrito Federal.
As well as an increase in human cases of yellow fever, 738 cases of yellow fever virus in monkeys have been reported. Since the outbreak, several unvaccinated travellers have contracted yellow fever, and there has been at least one death. Due to the ongoing outbreak, travellers going to at risk areas of Brazil are advised to get the Yellow Fever vaccination.
In addition the World Health Organisation also advised travellers heading to the states of Parana, Santa Catarina and Rio Grande do Sul should receive the vaccination, irrespective of location.
What is Yellow Fever?
Yellow Fever is a flavirus found in the tropics of Africa and South America.
Monkeys are a natural carrier for the virus and it is spread between monkeys and humans via the bite of an aedes mosquito.
Illness: It causes an acute viral illness which has a 50% mortality rate.
Prevention: The yellow fever vaccination should be considered for travellers who are visiting a high risk area. A single vaccination affords life long protection. The vaccination many not be suitable for everyone, so ensure you seek a full travel consultation.
Map of current areas with a risk of Yellow Fever

Book your travel appointment today
By Anna Chapman | Travel Nurse | February 2019
With November being Mouth Cancer Awareness month, it is important to highlight the signs and symptoms of mouth cancer.
During a dental appointment, your dentist will naturally look for abnormalities within the mouth and these include signs of oral cancer. It is important that in between dental appointments you also take notice of what is going on inside your mouth. If you notice any changes is it essential you tell your dentist or doctor immediately.
Mouth cancer can develop in most parts of the mouth, including the lips, tongue, gums, cheek and the throat. If it is caught early, the chances of surviving mouth cancer are nine out of ten – those odds are pretty good, and that’s why early detection is so important.
– If in doubt, get checked out.
It can be hard to spot symptoms of mouth cancer, which is why it is important to regularly attend your dental appointments. Your dentist can perform a check-up and look for slight abnormalities that you might otherwise miss. If anything is found, your dentist will provide onward referral to a specialist for further investigation.
Given that early detection is so crucial for survival, it’s extremely important that we all know what to look out for. In between dental appointments you should look out for changes in your mouth health that could indicate mouth cancer.
Signs & Symptoms of Mouth Cancer:
Three signs and symptoms not to ignore are:
- Ulcers which do not heal within three weeks.
- Red and white patches in the mouth; or
- Unusual lumps or swellings in the mouth or head and neck area.
If you notice anything unusual in your mouth, it’s advisable to make an appointment with your dentist.
Checking for Mouth Cancer:
When checking for signs of mouth cancer you should follow the following routine:
Head and neck
Check if both sides look the same and search for any lumps, bumps or swellings that are only on one side of the face. Feel and press along the sides and front of your neck being alert to any tenderness or lumps to the touch.
Lips
Pull down your lower lip and look inside for any sores or changes in colour. Use your thumb and forefinger to feel the lip for any unusual lumps, bumps or changes in texture. Repeat this on the upper lip.
Cheek
Use your finger to pull out your cheek so that they can see inside. Look for red, white or dark patches.
Then place your index finger inside your cheek, with your opposing thumb on the outside gently squeeze and roll the cheek to check for any lumps, tenderness or ulcers, repeat this action on the other cheek.
The roof of the mouth
With your head tilted back and mouth open wide, your dentist will look to see if there are any lumps or if there is any change in colour. They will run their finger on the roof of your mouth to feel for any lumps.
Tongue
Examine your tongue, looking at the surface for any changes in colour or texture.
Stick out your tongue or move it from one side to another, again looking for any swelling, change in colour or ulcers. Finally, take a look at the underside of the tongue by placing the tip of your tongue on the roof of your mouth.
The floor of the mouth
Look at the floor of the mouth for changes in colour that are different than normal. Press your finger along the floor of your mouth and underside of your tongue to feel for any unusual lumps, swellings or ulcers.
If you find anything unusual in any of these areas, or are unsure of anything, visit your dentist or doctor as soon as possible.
The best ways to prevent mouth cancer:
- Cut down on alcohol consumption;
- Cut down or stop smoking;
- Getting the HPV vaccine, Gardasil 9; and
- Enjoy a healthy diet.

You can book a dental appointment with Temple Dental.
Are you considering setting up a corporate health programme for your company?
The benefits of introducing a workplace health and wellbeing programme are clear: it has been proven that a successful corporate wellbeing programme leads to higher productivity, decreases in absenteeism and lower staff turnover. Ultimately, if your employees feeling healthy and looked after at work, it allows them to reach their potential and helps your company to achieve its business goals.
Perhaps as a result of the growing evidence in favour of such initiatives, businesses are now investing more than ever into corporate wellness programmes.
But with so many options available, how do you begin to create your own bespoke workplace programme? Firstly, be prepared to set aside time and budget. At the initial planning stage, there are several important factors to consider: how to structure the programme to your company’s ethos and business objectives, how to ensure staff involvement (at all levels), considering the size of your workplace, personalisation according to the needs of your company and the requirements of individual employees.
Fleet Street Clinic Corporate Wellbeing Programmes
At Fleet Street Clinic, we create bespoke corporate programmes across the UK. We work with companies of all sizes – from local businesses to City firms to international media agencies. We have a wealth of medical experts available, from hypnotherapists, osteopaths, dieticians, and can offer all kinds of services on site such as flu jabs, health screens and GP services.
We deliver programmes designed to boost the health and happiness of your staff, building and strengthening your workforce.
Want to find out more? You can visit our Corporate Healthcare Services page and make an enquiry. One of our Corporate Managers will be in touch soon.
Sepsis Signs:
World Sepsis Day – 13 September
Sepsis is a global health crisis and affects 27 to 30 million people every year. Out of those affected, 7 to 9 million dies. That’s one death every 3.5 seconds.
Sometimes called the silent killer, Sepsis is a bacterial infection of the blood which can become life-threatening. It is very hard to detect in the early stages, with symptoms similar to many other conditions and illnesses. In the UK alone, around 37,000 people die from sepsis each year.
Thankfully, due to public awareness increasing due to medical bodies and health campaigns, sepsis is being talked about more. As a result, parents and doctors have the condition forefront-of-their mind. The condition is treatable with early recognition and care.
Causes of Sepsis
Bacterial infections are the most common causes of Sepsis. However, Sepsis can also be caused by infections like seasonal influenza viruses, dengue viruses, and highly transmissible pathogens.
Children under 1, the elderly and those with chronic diseases and a weakened immune system are most at risk of sepsis.
Symptoms of Sepsis
Sepsis can display in a variety of ways including:
-
Slurred speech or confusion
-
Extreme shivering or muscle pain or fever
-
Passing no urine all-day
-
Severe breathlessness
-
It feels like you’re going to die
-
Skin mottled or discoloured
If someone is ill and is getting progressively worse with two or more of the above symptoms, then it is advised for you to go to A & E without delay.
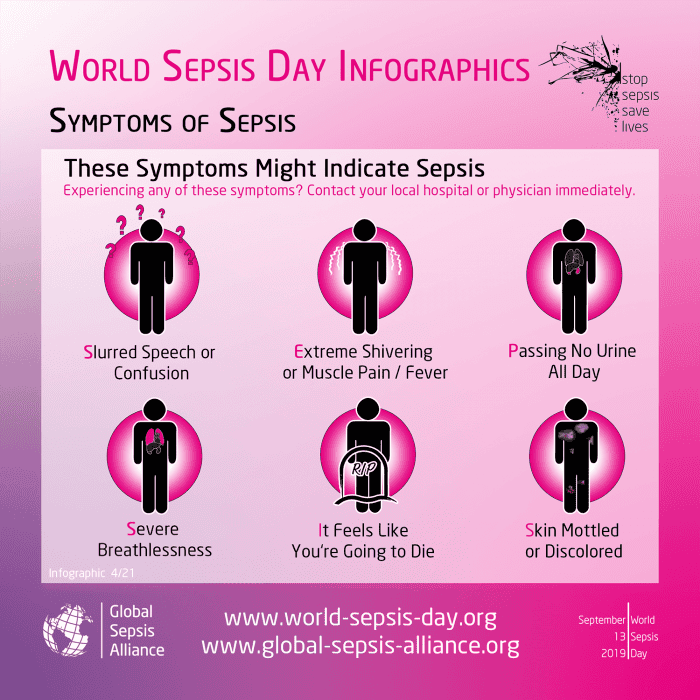
Preventing Sepsis
Preventing infection in the first place is the best way to prevent Sepsis from occurring.
This can be done by:
- Vaccinations – protect yourself from diseases which if serious, could lead to Sepsis.
- Hand Hygiene – reduce the spread of diseases and infections.
- Safe Childbirth – reducing infection to the mother and baby.
- Awareness of Sepsis– knowing the causes and symptoms can save lives.
If you think you are experiencing symptoms of sepsis, you should call 111 as you may require immediate medial attention.
For general GP health checks or vaccinations, you can book an appointment online.
National Smile Month is a UK campaign to promote good oral health.
Fleet Street Clinic is proud to be supporting this great campaign.
Dr Pilar Gesto, one of our highly-qualified dentists, explains why good oral health is key…
“In our busy and sometimes stressful lives, it is common to forget the power of a smile. This simple gesture can affect our work, our social life and our love life. But don’t worry. Beautiful smiles all have one thing in common: they always come from healthy mouths!”

To achieve a healthy and beautiful smile, simply follow the straightforward advice below:
- Clean and floss your teeth after every meal.
- Visit your dentist for regular check-ups.
- Avoid too much food and drinks that may stain your teeth, such as coffee and red wine.
- Do not smoke.
- Do not use abrasive toothpaste or products that may damage your enamel, such as sticky foods and acidic diet.
- In some cases, a whitening treatment may be appropriate if recommended by your dentist.
- Most importantly: smile as widely as you can!
We are very sorry to hear that Interhealth is ceasing to trade. As a hugely respected health practice, it is a great loss for Travel Medicine in the UK.
Fleet Street Clinic is in contact with Interhealth to offer support and provide continuity of medical care for existing individual and corporate Interhealth clients as required.
If you are looking for continuity with Interhealth services as an individual, or if you require corporate services such as Occupational Health and Travel Healthcare including travel vaccinations, please get in touch.
For more information please call Fleet Street Clinic on 0207 353 5678 or email at info@fleetstreetclinic.com
Stoptober is a good time to reflect on smoking habits and how to improve health issues related to tobacco use.
Quitting smoking is one of the most effective ways you can improve your health and the benefits start almost immediately. And remember, it’s never too late to quit!
The benefits of stopping smoking
After 20 minutes
Blood pressure and pulse are normalised, blood circulation improves.
After 8 hours
Levels of carbon monoxide in the blood decrease.
After 48 hours
Your sense of smell and taste are improving.
After 2 to 3 days
Less or no phlegm in the throat, fewer breathing difficulties.
After 5 to 7 days
Your breath is fresher, your teeth are cleaner and energy levels higher.
After 2 to 3 weeks
Physical withdrawal symptoms will stop, and you can now go several hours without thinking about smoking. Your risk of blood clots (thrombosis) is reduced.
After 4 weeks
Coughing, blocked sinuses and breathing difficulties should subside. The lungs are better able to resist infection.
After 2 to 3 months
Lung function improves by 5%.
After 1 year
The risk of developing cardiovascular disease is halved.
After 2 to 3 years
The risk of developing severe pneumonia or flu is the same as for a non-smoker. Your risk of heart disease, angina (chest pains) and stroke continues to fall.
After 5 years
The risk of throat, oesophageal and bladder cancer is halved.
After 5 to 10 years
The risk of developing cardiovascular disease or thrombosis is the same as for a non-smoker.
After 10 years
The risk of lung cancer is halved. The risk of developing osteoporosis decreases.
After 15 to 20 years
The risk of lung, throat, oesophageal or bladder cancer is the same as for a non-smoker. But heavy smokers (20 a day) have double the risk of lung cancer for the rest of their lives.
Help with quitting
If you need any advice or help to stop smoking, you can book an appointment with one of our GPs.
Measles Outbreak – What You Need to Know
The WHO has issued a warning about recent outbreaks of measles in Europe and the USA. Cases of measles have risen rapidly in recent months in Italy, Romania and most recently in US.
Measles is a highly contagious virus with potential for serious complications.
Initial symptoms can include:
- Runny nose
- High Temperature
- Spots in the mouth
- Aches and pains
- Sore eyes and swollen eyelids
A rash appears after 2-4 days which can present as blotchy spots, often starting at the head and progressing down.
Medical Advice for Measles
If you think you may be suffering from measles, or are concerned about risk of infection when travelling, please see your doctor straight away.
Travelling to areas with a risk of measles
Make sure you are up-to-date with your vaccinations before you travel, including the measles, mumps and rubella (MMR) vaccine. If your child will be travelling, the MMR can be given from 6 months of age. If you have not had measles or if you have not had two doses of MMR, you may be at risk. Measles is easily passed from person to person and can be a serious illness in adults as well as children. It is never too late to have the vaccine.
Call Fleet Street Clinic for medical assistance, advice on vaccinations and travel precautions on 0207 353 5678 email info@fleetstreetclinic.com or book online now.
FINISHING THE LONDON MARATHON
The 2018 London Marathon is just around the corner! Are you preparing for the run this year? If so, you’ll be very aware of the struggle ahead. A challenge like a marathon is incredibly rewarding but also tough on the body. Increasing your exercise capacity to this level pushes the limits of endurance both physically and mentally.
But even though this can feel torturous at times, you should not ignore recurrent pain or discomfort that persists after adequate rest. A common mistake is to push through and wait until pain prevents training before seeking care. By then, prolonged time off is often necessary to heal. It is estimated that 50 to 70 percent of first-time marathon runners drop out before their race.
If you do pick up an injury:
- First and foremost, stop and get it assessed.
- Maintain your strength and endurance as much as possible while recovering from your injury. If it prevents you from running, low-impact cardio exercise such as swimming, cycling or pool running can continue to improve exercise tolerance.
- Don’t be over-anxious to return to running, a good indicator of readiness is once you can walk for 30 minutes without pain during or after, you can begin a slow, careful return to pain-free running.
- Do not push through the pain.
Moving forward
As you increase your training and running, consider a biomechanical assessment. Slight problems in gait caused by many issues from footwear to posture to old injuries can cause new injuries (knees are particularly susceptible), or cause you to have to slow your pace or walk during the race.
Listen and respond to your body throughout training and recovery, and that finish line is waiting for you!
Post race
As you can imagine, a marathon takes its toll on the body in many ways. A post race assessment is well worth it, to identify any issues caused, not to mention a treatment to work out some of that lactic acid and to restore full function to the joints and muscles.
Our osteopath Andrew Doody and podiatrist George Hill can help with any marathon-related complaints. For more training tips and advice, or marathon injury treatment you can book an appointment online.
MARCH IS OVARIAN CANCER AWARENESS MONTH
A vital month raising awareness of ovarian cancer to improve early diagnosis to save lives.
More women died from ovarian cancer in the UK (4,227) than from all other gynaecological cancers combined in 2016, according to Cancer Research UK. However, worryingly one in five women in the UK (22%) mistakenly believe that a smear test (cervical screening) can detect ovarian cancer, according to research Target Ovarian Cancer carried out with YouGov.
We are committed to raising awareness of the disease.
Speak to one of our female GP’s about any concerns you may have about your gynaecological history and your families medical history. During your consultation, we will also conduct a breast check and pelvic examination.
“In the UK a woman dies every two hours from ovarian cancer, but the earlier the diagnosis the better the chances are”
Professor Hani Gabra – Director of Ovarian Cancer Action Research Centre
What is ovarian cancer?
Ovarian cancer is when abnormal cells in the ovary begin to grow and divide in an uncontrolled way and eventually form a growth (tumour). Every year 7,300 women in the UK are diagnosed with ovarian cancer.
Who can get ovarian cancer?
The risk of developing ovarian cancer increases as you get older. The most common type of ovarian cancer is epithelial ovarian cancer, this usually occurs in women older than 50 years old. We don’t know exactly what causes epithelial ovarian cancer. But some factors may increase or reduce the risk.
Factors that increase the risk include:
- getting older
- inherited faulty genes
- having breast cancer before
Factors that may reduce the risk include:
- taking the contraceptive pill
- having children
- breastfeeding
Ovarian Cancer is notoriously difficult to spot.
With non-specific symptoms in the early stages. It is hoped that this new method of early diagnosis could help save lives.
How to recognise the symptoms of Ovarian Cancer:
Early Ovarian Cancer symptoms can be similar to those of other conditions, these some to watch out for:
- Persistent bloating – not bloating that comes and goes
- Pain in the lower stomach and pelvis
- Difficulty Eating and feeling full quickly
- Back pain
- Fatigue
- Change in bowel habits
What should you do if you’re worried?
It is important to contact your GP as soon as possible if you spot any symptoms that are abnormal for you.
We understand talking about your concerns and having an examination can be quite worrying and for some, embarrassing, therefore, to make you as comfortable as possible, all our well woman services are booked with a female GP.
There is an Ovarian Cancer Blood Test – CA 125 available
Levels of protein CA125 in the blood are recognised as a marker for ovarian cancer. This simple and effective blood test will detect early stages of ovarian cancer. You can either have this as a stand-alone blood test or add it on to your medical for an additional cost. Please inquire for prices..
Links:
Target Ovarian Cancer
Cancer Research UK
For more information about Fleet Street Clinic’s Women’s Health Services.
You can also book a GP appointment online.
Tennis Elbow and Golfer’s Elbow
As our glorious British Summer continues and everyone basks on the tennis court, our osteopath, Andrew Doody, calls time on an old problem.
Tennis elbow is a condition that causes pain around the outside of the elbow. It’s clinically known as lateral epicondylitis and often occurs after strenuous overuse of the muscles and tendons of the forearm, near the elbow joint.
You may notice pain:
- on the outside of your upper forearm, just below the bend of your elbow
- when lifting or bending your arm
- when gripping small objects, such as a pen
- when twisting your forearm, such as turning a door handle or opening a jar
You may also find it difficult to fully extend your arm.
The name tennis elbow is because the tennis backhand shot is a common way to develop the problem, however any strain or overuse can cause it.
Lesser known golfer’s elbow (medial epicondylitis) is a similar issue but on the other side of the elbow.
These conditions are easy to get but can hang around for weeks and months if left untreated. This is largely due to the fact that lots of the muscles in the hand and forearm attach to those two spots on either side of the elbow. This means that once the area is enflamed, most everything you do with the hand can re-aggravate it, from drinking a cup of tea (or Pimms) to opening a door (or raising a trophy).
Once diagnosed, treatment involves firstly reducing the inflammation with rest, cold compresses and anti-inflammatories, followed by massage and careful mobilisation to help relieve pain and stiffness and restore the range of movement. Specific supports can also be quite beneficial at this time.
Preventing tennis elbow
Preventing tennis elbow is tough but here are a few pointers:
- If you have tennis elbow, stop doing the activity that is causing pain, or find an alternative way of doing it that does not place stress on your tendons.
- Avoid using your wrist and elbow more than the rest of your arm. Spread the load to the larger muscles of your shoulder and upper arm.
- If you play a sport that involves repetitive movements, such as tennis or squash, getting some coaching advice to help improve your technique may help you avoid getting tennis elbow.
- Before playing a sport that involves repetitive arm movements, warm up properly and gently stretch your arm muscles to help avoid injury.
- Use lightweight tools or racquets and enlarge their grip size to help you avoid putting excess strain on your tendons.
- Wear a tennis elbow support when you are using your arm, and take it off while you are resting or sleeping to help prevent further damage to your tendons. Ask your osteopath for advice about the best type of brace or splint to use.
Increasing the strength of your forearm muscles can help prevent tennis elbow. Your osteopath can advise you about exercises to build up your forearm muscles.
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC). Book an appointment with him if you have any musculoskeletal injuries.
Ask the average person what viral disease they think claims the most lives, and HIV might be the likely response. However, this is not so, according to research in the Lancet. The research suggests that viral hepatitis caused 1.45m deaths in 2013 compared to 1.2m lives claimed by AIDS in 2014. What is Hepatitis?
Hepatitis is best defined as an inflammation of the liver caused by the hepatitis virus. There are 5 types of hepatitis virus called; A,B,C,D and E. Contaminated food is usually the cause of virus types A and E. Types B, C and D are spread via infected bodily fluid contact. Virus types B and C lead to the most deaths.
Prevention
Hepatitis A and B are vaccine preventable. Many countries offer these vaccines routinely on the childhood schedule but this is not the case in the UK.
Hepatitis Vaccination at the Fleet Street Clinic
Vaccinations are needed to give protection against hepatitis A and B and they currently are not part of the childhood vaccination schedule in the UK. At the Fleet Street Clinic, we make it a priority to have a good supply of hepatitis A and B vaccines for children all year round. The hepatitis vaccinations can be given individually, or as a combined injection. For long lasting protection, several doses are required. Our vaccination team are highly trained, well-qualified and have dozens of years’ experience between them. Our vaccination service takes place in a clean, comfortable and safe environment.
You can learn more about our vaccinations here.
While hepatitis is causing millions of fatalities across the globe, you can take steps towards protection against the virus by booking an appointment for hepatitis vaccinations at Fleet Street Clinic today.
With the Rugby World Cup in full swing, our osteopath Andrew Doody takes you through some of the most common injuries in this most physical of sports.
The five most common rugby injuries:
A medial collateral ligament tear
This is the ligament on the inside of the knee. It stabilises the knee (along with the lateral collateral and cruciate ligaments). Due to the nature of tackling a player by hitting into the outside of the leg, this can often gap the opposite side, putting the ligament under enough strain to tear or even rupture. Quick changes of direction can also strain this ligament.
Haematoma of the thigh
In similar circumstances as the MCL injuries during tackling, impact on the thigh can often cause severe bruising of an area as the soft tissues are smashed against the thigh bone with blood vessels being damaged and blood then clotting around the area.
Hamstring tears
The three muscles on the back of the thigh, commonly known as the hamstrings are often injured in many sports, not only rugby. Rapid changes of pace can strain the muscle, especially if it is not fully warmed up (although research is beginning to show it’s not quite as simple as previously thought). Mechanical issues in the leg such as gait on running can also add to the danger of a tear.
Calf strain
In a similar fashion, the calf muscle is often strained, usually where it attaches to the Achilles tendon. Again, overuse, especially on a tired muscle, can cause strains, as can the mechanics of the foot and ankle complex.
Concussion
The one that has the spotlight on it most recently is, of course, concussion. Any blow to the head can cause varying degrees of concussion. This can be from mild to extremely serious. Very difficult to prevent in rugby, the emphasis has fallen on rapid identification of when a concussion has occurred and immediate action to minimise the danger of ongoing damage.
Rugby is a rough sport and it is always difficult to greatly lower the risk of injury without hugely compromising what is a great game. The RFU is working hard to achieve this though, through changes to the laws of rugby. As well as raising awareness of injuries, both in regard to preventative factors and response after injury occurs.
Osteopathy can stretch and condition the muscles and ease the pain; a routine of stretches to carry out at home can also be recommended. Andrew Doody offers a trusted osteopathy service which can assist with pain relief and also address the underlying causes of injuries, decreasing your chances of future injury.
If you have had a rugby injury or are experiencing any musculoskeletal problems, you can book an appointment online.
The Fleet Street Clinic is pleased to advise that it is has been awarded SEQOHS Accreditation by the Royal College of Physicians, a quality mark endorsing the provision of Safe Effective Quality Occupational Health Services.
We undertake a full range of Occupational Health Services:
- Management Referrals, Fitness to Work and Absence Management
- Pre-Placement Assessments (formerly Pre-Employment Assessments)
- Pre Deployment Medicals and certificated fitness for deployment
- Post Deployment Medicals
- Ergonomic Assessments
- Immunisations & blood tests
- Health Clearance Services for healthcare workers
If you would like further information about our occupational health services or wish to discuss your company’s needs, our OH Administrator can be contacted on occhealthadmin@fleetstreetclinic.com or 020 7353 5678.
Sexual Health Awareness
We are focusing on Sexual Health Awareness at Fleet Street Clinic this week, to encourage people to talk about their sexual health with health care professionals and help to diagnose and treat STIs.
Did you know:
– More than two-thirds of people have never had an STI test.
– Many people carrying an STI do not display symptoms.
This is why it is worth getting tested, even if you don’t feel that something is wrong. Having an STI check can sometimes make people nervous, but a sexual health appointment with a professional is quick and helps keep your health on track.
STI Symptoms
Although not everyone presents symptoms, some common complaints in men and women suffering from an STI can be:
- Pain when passing urine
- Itching or burning around the genital area
- Discharge that smells
Having these symptoms doesn’t mean you have an STI, but make sure you go to a GP to get checked out and find out the cause.
Health professionals advise to always use condoms to help reduce the chance of STI transmission from intercourse and oral sex.
Sexual Health Advice at Fleet Street Clinic
At Fleet Street Clinic, we provide access to Sexual Health tests and advice from our trained medical professionals.
You can learn more about our sexual health services here.
If you would like a sexual health appointment, you can book online.
With summer just around the corner, many are busy shopping for essentials. Sun cream, swimwear and toiletries are more likely on the list rather than travel vaccines. Many forget to check if they are up-to-date on the recommended travel vaccines. To make sure you get full enjoyment out of your holidays it’s important to stay safe during and after your break.
Below we have highlighted some health concerns you need to know if you are travelling this Summer:
Measles:
Throughout this year we have seen an increased rise in measles cases all over the world. The disease can be easily prevented with two doses of the safe and efficient MMR vaccine. A review of your childhood vaccine records will indicate if you have had the MMR course or if in need of a booster or the full course. Those struggling to confirm their immunity can have a simple immunity blood test which will either confirm if they are immune or not.
Hepatitis:
When visiting areas with poor sanitation, which can affect the water and food consumed, travellers, should consider the Hepatitis A vaccination. A safe and effective vaccination which prevents the viral infection and stop travellers falling ill whilst away. In addition to the vaccination, travellers also should take caution and ensure all food is cooked thoroughly and served hot, stick to bottled water which is sealed and avoid ice (usually tap water).
Hepatitis B is a viral infection spread by contaminated blood and bodily fluids. Examples in which travellers can be at risk are contaminated medical equipment which may be used in an emergency for example needles and syringes. Hepatitis B can also be prevented with a vaccine course before travelling.
Malaria:
Every year there are more than 200 million new cases of malaria, another preventable and treatable disease. The World Health Organizations lists 91 countries and territories at risk of malaria transmission. Preventative medication can be taken to reduce the risk of catching Malaria as there is currently no vaccination.
Infectious diarrhoea:
In about 20% of travellers with diarrhoea, more than one bug turns out to be responsible for the illness. Bugs can be caught from drinking tap water and eating uncooked food or salads washed in tap water. It can put a dampener on holiday plans and make you feel under the weather. Antibiotics can be prescribed prior to travel, in case of a severe infection. Our gastro kit is designed to help travellers who may need medication to help cases of infectious diarrhoea whilst travelling.
“There may be avoidable risks to your health depending on your overall health, destination and planned travel activities. We can assess the risks and provide you with the best travel health advice to ensure you have an enjoyable trip and return healthy.”
If you wish to discuss how to stay safe on holiday or would like more advice on what vaccinations you may need, our travel nurses can help. Book a travel consultation to discuss your needs.