When it comes to looking after your people, prevention really is better than cure.
At Fleet Street Clinic, we’ve seen time and again how a simple, structured occupational health (OH) referral process can transform how businesses manage sickness absence, productivity and staff wellbeing.
But how do you know when it’s time to get one in place?
Here are five signs to watch out for
1. Sickness absence is creeping up
If you’ve noticed more staff taking time off, you’re not alone. According to the ONS, the UK sickness absence rate in 2024 was 2.0% (about 4.4 days lost per worker). That’s the highest level in over a decade.
Often, a pattern of rising absence hints at underlying issues such as physical, psychological or environmental. A referral process ensures those employees get timely specialist support rather than letting things drift.
2. Staff are off sick regularly or for long stretches
Frequent short absences or one long spell can quickly impact your team.
Occupational health input helps identify the root cause and recommends adjustments or next steps to help people return safely and sustainably.
3. People return… but keep relapsing
If someone’s back at work but struggles to stay there, it might not be resilience, it might be a missing piece of support. An OH referral can guide phased returns, recommend adjustments and help both you and your employee move forward confidently.
4. You’re unsure of your legal responsibilities
Employers in the UK have a duty of care under the Health & Safety at Work Act and the Equality Act 2010. If an employee has a health condition or disability, you may need to make reasonable adjustments. OH reports provide the medical context to help you meet those obligations fairly and safely.
5. Your business is changing
New equipment, hybrid work, different roles… all of these can introduce new risks.
A structured referral process ensures everyone is assessed appropriately and supported as roles evolve.
When you have the right referral process, you’re not just reducing absence… you’re showing your employees that their wellbeing matters.
At Fleet Street Clinic, we help businesses of all sizes design clear, compliant and compassionate OH referral pathways.
Get in touch to discuss how we can support your team’s health and keep your business thriving. Contact us to discuss how we can support your organisation.
Sources:
https://www.ons.gov.uk/releases/sicknessabsenceintheuklabourmarket2023to2024
If you’ve recently discovered that CityDoc has closed, it’s completely understandable to feel unsettled, particularly if you were mid-treatment, waiting for results or due a repeat prescription.
For many people, the first worry is whether everything now has to start again. In most cases, it doesn’t.
With an appropriate medical review, care can usually continue safely and smoothly once a doctor understands your history and current treatment plan.
Take a breath first
A sudden clinic closure can feel disruptive, especially when health is involved. You don’t need to solve everything immediately.
The priority is simply continuity of care – making sure a clinician reviews where you are now and advises on the safest next step.
Arranging an appointment with a suitable clinic allows a doctor to:
- review your current medication or treatment
- assess any upcoming deadlines (prescriptions, vaccines, monitoring)
- advise how to continue safely and appropriately
If you have copies of emails, letters, test results, or medication packaging, bring them along. If you don’t, that’s very common and it won’t prevent a doctor from helping you move forward.
What about prescriptions?
This is often the biggest concern. In many situations, a doctor can continue necessary medication once they’ve reviewed your medical background and confirmed it’s appropriate. Sometimes a brief review or updated information is needed, but this is usually straightforward.
If your medication is time-sensitive, it’s helpful to mention this when booking so it can be prioritised.
Will tests need to be repeated?
Not necessarily. Doctors aim to avoid unnecessary duplication. Any available information will be used, and investigations are only repeated if they’re clinically required to ensure your care remains safe. The focus is always on balancing continuity with good medical practice.
Ongoing treatment plans or travel vaccinations
If you were part way through a vaccination course or monitoring programme, this can usually continue once reviewed. The timing and schedule matter more than the original provider. This is something clinicians manage routinely.
Feeling unsure is normal
For many patients, the hardest part of a clinic closure is simply not knowing who to contact next or worrying they’ve somehow been left in limbo.
In reality, continuity of care is something experienced medical teams handle regularly. Once a new doctor has assessed your situation, the process is often far simpler than expected.
If you’re unsure what to do next, speaking with a medical professional can help you understand your options and move forward with confidence.
At Fleet Street Clinic, we regularly support patients who find themselves in this position. Our GPs can review your situation, advise on next steps, and help ensure your care continues safely and appropriately without unnecessary delays or repetition.
If you’d like guidance, you can learn more or book an appointment today.
Many people begin January feeling tired, more than they expected. After a busy December, disrupted sleep routines, richer food, travel, darker days and the pressure of returning to work, it’s normal for energy levels to dip. Most people recover within a week or two once routines settle.
However, persistent or unexplained fatigue is not something to ignore. At Fleet Street Clinic, we see fatigue regularly and for many patients it becomes clear that their tiredness is not simply “post-holiday sluggishness”, but a symptom of an underlying issue that needs attention.
Recognising the difference matters. Fatigue is one of the most common reasons people delay seeking help and one of the symptoms most likely to improve with early assessment.
Understanding what’s normal
Short-term fatigue at the start of the year usually has a clear cause: disrupted sleep, social overstimulation, poor hydration, irregular meals, increased alcohol intake or jet lag. Once life settles, most people notice gradual improvements in energy, concentration and sleep quality.
If your energy steadily improves day by day, this is generally reassuring.
When fatigue becomes a concern
Fatigue becomes medically significant when it persists, is worsening, or begins to affect normal functioning.
People often report:
- Difficulty concentrating or thinking clearly
- Struggling to wake up despite adequate sleep
- Feeling physically weak or drained
- Increased irritability or low mood
- Needing to rest more than usual
- Recurrent minor infections or slower recovery
These are often early signs that something in the body needs attention.
What many patients don’t realise is that fatigue is not a diagnosis, it’s a symptom. And that symptom may point to issues such as thyroid imbalance, iron deficiency, B12 deficiency, diabetes, chronic stress, post-viral changes, sleep disorders or hormone shifts. All of these are manageable, but only when identified.
Why a GP assessment is so important
When a patient comes to us with fatigue, our first step is to understand the full picture. That includes sleep patterns, diet, stress levels, recent infections, travel, menstrual cycles, medication and general health history.
From there, a targeted set of blood tests can reveal the underlying reason for tiredness. Depending on the individual, this can include:
- Iron and ferritin (iron deficiency is extremely common)
- Thyroid function
- Vitamin B12 and folate
- Vitamin D
- HbA1c to assess blood sugar regulation
- Full blood count
- Liver and kidney health markers
- Inflammation markers
Many fatigue related conditions present subtly, especially in the early stages. Blood tests allow us to identify issues before they progress and to create a tailored plan based on your physiology, not guesswork.
Fatigue that is left uninvestigated can gradually affect mood, memory, immunity, productivity and overall wellbeing. For some, fatigue is linked to a treatable deficiency; for others, it’s the first sign of hormonal changes or a developing metabolic issue. In most cases, once we identify the cause, meaningful improvement follows.
What recovery looks like
Treatment depends entirely on the cause. For some, correcting a nutritional deficiency restores energy quickly. For others, small adjustments to sleep timing, stress load, hydration or routine can make a significant difference. In certain cases, we may recommend specialist referrals, monitoring or lifestyle guidance tailored to the individual.
What matters most is that you don’t ignore persistent fatigue or assume it is “just January”. Your body is signalling something and it’s worth listening.
Book your GP Health Review at Fleet Street Clinic here: https://booking.fleetstreetclinic.com/medicals_and_health_screenings
BACKGROUND & PRESENT CASE
A professional services organisation referred an employee in a senior leadership role for Occupational Health advice following a period of work-related stress. The employee had experienced symptoms such as fatigue, reduced concentration, low mood and disrupted sleep, which developed after taking on a new set of responsibilities. After a short sickness absence, the employer sought guidance on supporting their return to work, managing workload expectations and exploring workplace adjustments.
OUR ASSESSMENT
Following a clinical consultation, review of medical information and a risk assessment, we identified the following:
• Stressors were primarily perception-based, relating to workload, expectations and available support.
• Psychological therapy was underway and proving beneficial in managing symptoms
• There was no significant past mental health history and the employee had good personal support.
• The employee was fit for work at the time of assessment with no clinical limitations.
OUR RECOMMENDATIONS
We advised a clear and structured set of workplace actions to support continued recovery and prevent recurrence:
• A collaborative management-led discussion to address workload, expectations and available support.
• Use of a validated structured stress-assessment tool to support conversations around domains of perceived stress including job demands, control and support.
• Continuation of psychological therapy, with flexibility for appointment times.
• Encouraging positive lifestyle habits to maintain resilience as part of a multi-faceted approach to wellbeing.
• Regular check-ins with management to monitor wellbeing and escalate concerns early.
• Access to the organisation’s Employee Assistance Programme if required.
OUTCOME / RESULTS
• The employee successfully returned to full duties with improved concentration and energy levels.
• Ongoing therapy continues to support recovery.
• No further Occupational Health follow-up was advised unless symptoms recur or work circumstances change.
• The Equality Act 2010 was unlikely to apply based on the clinical picture.
• Sustainable improvement was considered dependent on continued organisational dialogue around workload and expectations.
KEY LEARNING POINTS
• Early, structured discussions around workload and support can prevent escalation of work-related stress.
• Psychological therapy combined with workplace engagement is highly effective in restoring function.
• Perception-based stressors often require organisational, not purely clinical, action for long-term resolution.
CLINICIAN COMMENTS
“Addressing work-related perceptions early, alongside supportive therapy, made a significant difference in achieving a safe and sustainable return to full duties.”
CONFIDENTIALITY NOTICE
All personal and organisational details in this case study have been anonymised to protect confidentiality.
January is a natural reset point for many of us. After the busyness of the festive season, it’s a good time to pause and check in on your health for the year ahead. At Fleet Street Clinic, we often see patients who want to improve their wellbeing but aren’t sure where to begin. An annual health review is an effective, structured way to understand what your body needs and what to prioritise.
Here’s our checklist to help you start the year feeling informed and supported.
1. Blood tests worth considering annually
Routine blood tests can identify changes long before symptoms develop. Depending on your medical history, your GP may recommend:
• Full blood count: Screens for anaemia, infection and several systemic issues
• Thyroid function: Evaluates unexplained fatigue, weight change, temperature sensitivity
• Vitamin D: Commonly low in winter months, affects immunity, energy, bone health
• B12 and folate: Important for energy production and neurological function
• Iron studies: Particularly relevant for women and anyone with fatigue
• HbA1c (diabetes screening): Identifies issues with blood sugar control
• Liver and kidney function: Important for overall metabolic health
Having a baseline each year helps track small changes early and target any underlying causes of fatigue, low mood or hormonal symptoms.
2. Review your cardiovascular health
High blood pressure and cholesterol can develop silently.
Your GP may recommend:
• Blood pressure monitoring
• Cholesterol & lipid panel
• ECG if there are symptoms or cardiovascular risk factors
Heart health should be reviewed annually for adults over 40 or earlier based on family history or symptoms.
3. Mental wellbeing check-in
January can affect mood for many reasons. The days are shorter, disrupted sleep routines and post-holiday pressure. A GP check-in can help identify early signs of:
• Stress overload
• Low mood
• Anxiety or sleep disturbance
• Hormone-related mood changes
Early support is always more effective than waiting until symptoms escalate.
4. Travel health for the year ahead
If you’re planning holidays or work travel this year, now is the time to review:
• Required or recommended vaccines
• Malaria risks
• Travel medications
• Family travel considerations
• Gut health / gastro kits for common travel illnesses
Early planning helps avoid last-minute stress and ensures wider vaccine coverage windows when needed.
5. Women’s and men’s health screens
Depending on age and medical history:
Women may review:
• Cervical screening (if due)
• Breast checks and breast pain concerns
• Hormone testing for fatigue, irregular cycles or perimenopause
• Iron levels
Men may review:
• Prostate symptoms or PSA testing if appropriate
• Testosterone concerns
• Cardiovascular risk factors
6. Immunisation updates
A GP can confirm whether you are up to date with:
• Flu (seasonal)
• Covid-19 boosters
• Tetanus
• HPV (available privately up to age 45)
• Travel vaccinations
Vaccination status is often overlooked but plays a big role in long-term prevention.
7. Build a personalised wellbeing plan
Once you’ve reviewed the essentials, your GP can help you map out a wellbeing plan that includes:
• Sleep support strategies
• Nutrition guidance
• Stress management
• Exercise routines based on your health profile
• Follow-up tests or referrals if needed
A personalised plan turns good intentions into actionable steps.
If you’re unsure where to start or feeling overwhelmed by symptoms, a GP consultation is an excellent first step. Early conversations give you clarity, reassurance and a tailored roadmap rather than waiting until symptoms impact daily life.
Book your GP Health Review at Fleet Street Clinic here: https://fleetstreetclinic.com/services/gp-services/screenings/
BACKGROUND & PRESENT CASE
A professional services organisation asked Occupational Health for advice on supporting an administrative employee who was returning to work while still receiving treatment for a cancer-related condition. The employee had restarted work from home and was managing ongoing therapy, but the employer needed guidance on managing fluctuating fatigue, changes in concentration, and the increased risk of infection.
OUR ASSESSMENT
After a clinical consultation, review of medical information, and a workplace risk assessment, we identified the following:
• The employee remained clinically vulnerable to infection, making office attendance unsafe at this stage.
• Remote working was effective, and the employee was meeting expected performance levels.
• Fatigue and occasional dips in concentration were expected around treatment cycles or during particularly busy tasks.
• Ongoing therapy and further medical procedures were planned.
• The employee demonstrated good self-management strategies and had a solid support system outside of work.
OUR RECOMMENDATIONS
We recommended practical, evidence-based adjustments to help the employee work safely and sustainably:
• Continued remote working as a medically appropriate adjustment.
• Flexible absence management, in line with the Equality Act 2010.
• Flexibility for medical appointments and days when symptoms are more noticeable.
• Regular, supportive check-ins with management.
• Task adjustments during periods of increased fatigue – for example, during busy billing cycles or high-concentration work.
• Task rotation to help balance workload and manage symptoms.
• Access to emotional wellbeing support, either through the GP or the employer’s Employee Assistance Programme (EAP).
• Office attendance to be reviewed only when medically appropriate, based on advice from the treating specialist.
OUTCOME / RESULTS
• The employee has continued to work full-time from home with satisfactory performance.
• Workplace attendance remained medically unsuitable due to the ongoing infection risk.
• Further treatment is anticipated, with a short period of recovery time expected.
• The case demonstrates effective long-term disability management in line with the Equality Act 2010.
KEY LEARNING POINTS
• Remote working can be a safe and effective adjustment during long-term medical treatment.
• Flexibility around symptoms and appointments supports productivity and reduces sickness absence.
• Following advice from Occupational Health enables employers to make safe, consistent and legally defensible decisions.
CLINICIAN INSIGHT
“Remote working was essential in protecting the employee’s health while enabling them to continue contributing effectively during ongoing treatment.”
CONFIDENTIALITY NOTICE
All personal and organisational details in this case study have been anonymised to protect confidentiality.
Clear vision plays a bigger role in workplace wellbeing than many people realise.
A recent report estimates that eyesight related issues could be costing UK businesses up to £21.4 billion every year, with employees losing time through slower reading, reduced focus and increased fatigue (Specsavers, 2025).
At Fleet Street Clinic, we see this regularly. People often come to us feeling unusually tired at work, struggling with headaches, or noticing that their concentration isn’t what it used to be… yet they don’t always connect these changes to their vision.
In many cases, a small, undetected vision issue or an outdated prescription is enough to make the working day feel significantly harder.
Vision is closely connected to many aspects of health.
If your eyesight isn’t fully supported, your body tends to compensate, often without you realising. Some examples are:
– Leaning forward to see the screen
– Squinting or widening the eyes
– Holding tension in the neck and shoulders
– Losing focus or reading more slowly
Over time, this can contribute to headaches, neck strain, mental fatigue and a sense of “burnout” that’s actually rooted in visual stress. This is particularly relevant for people who spend long periods at a computer or who work in visually demanding roles.
Eyes can also reveal early health issues. During an eye examination, clinicians can sometimes pick up early signs of broader medical conditions, such as:
– Hypertension, visible as subtle retinal vessel changes
– Diabetes, which can cause early retinal changes even before other symptoms appear
– High cholesterol, sometimes seen as cholesterol deposits in retinal arteries
– Vascular or neurological changes, which may be visible in the optic nerve
These findings can act as important early warning signs, allowing people to seek medical advice before symptoms become more serious.
Why does this matter for employers?
When employees can’t see comfortably, their productivity, accuracy and energy levels naturally suffer. From an occupational health perspective, we know that visual comfort directly influences:
– Focus and concentration
– Task accuracy
– Reading speed
– Fatigue and presenteeism
– Workplace safety
– Overall wellbeing
It’s not about ticking a box, it’s about supporting people to work safely, comfortably and sustainably.
Under the UK’s Display Screen Equipment (DSE) regulations, employees who use screens regularly are entitled to an eye test paid for by their employer. But beyond compliance, regular vision checks are simply good practice. They help prevent strain, reduce discomfort and support productivity — which benefits both employees and businesses.
We work directly with companies to offer:
– Comprehensive occupational health assessments
– Vision screening for employees
– Pathways to specialist care when needed
– Preventive health checks that support long-term wellbeing
– Advice for employers on DSE requirements and workplace adjustments
Our approach is practical, collaborative and centred on looking after people, not just compliance.
Investing in eye care, whether through occupational health programmes or regular eye examinations, is a simple and cost-effective way to improve wellbeing and performance across a team. If your organisation is interested in supporting employee health in a meaningful way, we’re here to help.
Sources:
Specsavers workplace productivity report
WHO – Blindness & Vision loss
WHO – Screen Use & Eye health
WHO – Hypertension (retinal signs)
WHO – Diabetes (diabetic eye disease)
UK HSE – DSE Regulations
Stress Awareness Week is a reminder that while stress is a normal part of life, how we manage it makes all the difference. At Fleet Street Clinic, we see how ongoing stress can affect both mind and body, often long before people realise it’s taking a toll.
Short bursts of stress can be motivating, but when it becomes constant, it can lead to high blood pressure, poor sleep, headaches, digestive issues and burnout. According to the World Health Organization (WHO, 2024), stress-related conditions contribute to a growing number of workplace absences and chronic health problems worldwide. A UK poll by the Mental Health Foundation found that 74% of adults felt so stressed at some point in their life that they felt overwhelmed or unable to cope.
Here are some simple, evidence-based ways to manage stress and protect your health:
1. Recognise early signs of stress
Irritability, fatigue, disrupted sleep or frequent tension headaches are early warning signs. Many people try to “push through”, but early recognition allows for early action. If you notice physical symptoms like rapid heart rate or frequent colds, it might be time for a health check.
2. Move your body, even briefly
Exercise releases endorphins and helps your body process stress hormones more efficiently. Even a 10 minute walk can reset your nervous system, improve mood and enhance focus.
3. Build small pauses into your day
Constant digital engagement makes it hard for your brain to switch off. Try short “no-screen” breaks, mindful breathing or a walk outside. Small, consistent habits are more effective than one-off wellness resolutions.
4. Support your body through nutrition and sleep
Caffeine and sugar might give a temporary boost but can increase cortisol levels. Eat regularly, prioritise hydration and aim for 7 to 8 hours of sleep as this is vital for hormone balance and emotional regulation.
5. Talk to a professional early
Stress isn’t a sign of weakness, it’s a physiological response. Speaking with a GP can help identify underlying issues such as anxiety, fatigue, or physical stress symptoms. At Fleet Street Clinic, our doctors take an integrated approach, addressing both mental and physical wellbeing.
6. Prevent, don’t just treat
Regular health checks can catch stress related changes early from elevated blood pressure to disrupted sleep patterns. Preventive care helps keep you balanced, even during busy or demanding periods.
If stress is interfering with your daily life, relationships, or physical health, it’s time to talk. Early guidance can prevent escalation and support recovery. Our GPs can assess your symptoms, offer advice and refer you to further mental health support if needed.
Your health matters every day, not just during Stress Awareness Week.
Book a consultation today to discuss your wellbeing and explore personalised ways to protect your health.
Sources:
https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work (WHO, Sept 2024)
https://www.mentalhealth.org.uk/explore-mental-health/statistics/stress-statistics (Mental Health Foundation, 2018)
https://isma.org.uk/ (ISMA, 2025)
You’ve sent the email. You’ve put up the posters. You’ve booked the clinic.
So why do some people still not get their flu jab?
The answer might be less about health and more about human behaviour.
“I’ll do it later.”
One of the strongest behavioural tendencies is present bias… our tendency to prioritise short-term comfort over long-term benefit. Even if someone fully intends to get vaccinated, they might delay it because “it’s not urgent.”
“I didn’t get it last year and I was fine.”
People tend to stick with what they did last time. If they skipped the jab last year and didn’t get ill, their brain logs that as success, even if it was just luck.
“Another one?”
After several years of Covid boosters, some employees are experiencing vaccine fatigue. That’s why flu comms need to feel relevant and not repetitive.
So what can employers do?
– Make the jab the default: pre-filled forms, “your slot is booked” reminders
– Use peer influence: team leads and managers going first sets the tone
– Add friction to opting out: make it easier to say yes than to ignore
Reframe the message:
– “Protect your team” works better than “protect yourself”
– “One small action = full season of protection”
– “Book it now, thank yourself later”
But most importantly, reduce the effort. The simpler the process, the higher the uptake.
A 2024 study found that effective messaging around flu can also positively influence COVID-19 vaccine uptake, and vice versa. (MDPI Vaccines Journal, 2024)
At Fleet Street Clinic, we help organisations apply behavioural insight to flu campaigns, from poster design to email strategy, so that uptake doesn’t come down to luck but to smart, simple systems.
Discounted flu vaccine prices available for your workplace programme while stock lasts.
Email: flu_admin@flujabs.org
Sources: https://www.mdpi.com/2673-8112/4/3/24, (MDPI Vaccines Journal, 2024)
Why your jet-setting colleagues need to be vaccinated against flu.
Few people realise that flu is the commonest travel-associated infection. People are six times more likely to pick up a respiratory infection when they travel than they are at home. This is how flu infection moves seasonally around the globe. Busy airport terminals, the aircraft cabin, crowded buses, conference centres and even the wrong cab driver on the wrong day, can increase the risk. (Cruise ships are closed communities that are especially vulnerable to outbreaks.)
And although flu is seasonal each winter in the northern and southern hemispheres, it occurs year-round in tropical countries, constantly present.
The consequences are not surprising: reduced productivity for people who travel for work; disruption of travel plans and reduced enjoyment for those on holiday; and an increased risk to co-workers and family members on return home.
How many of us travel prepared to treat colds or flu on the go? If we become ill abroad, the simple, familiar remedies we rely on at home – like decongestants and paracetamol – may not be so easy to identify or find.
If you or your work colleagues are travelling abroad this winter, don’t miss out on the easiest, simplest way to protect yourself and those around you: get vaccinated against flu.
At Fleet Street Clinic, we understand that your time is valuable. Located in the heart of Temple, Central London, our clinic is designed around the needs of busy professionals who want expert healthcare that fits their schedule.
That’s why we’re proud to offer extended opening hours, including early mornings and late evenings – making it easier than ever to book the care you need, when you need it.
Our Opening Hours:
- Monday: 8:00am – 7:30pm
- Tuesday: 8:00am – 7:30pm
- Wednesday: 8:00am – 6:30pm
- Thursday: 8:00am – 7:30pm
- Friday: 8:00am – 5:30pm
- Saturday: By appointment only
Evening Doctors’ Appointments Available
We’re open late three evenings a week (Monday, Tuesday, and Thursday) – ideal for those who can’t step away from work during the day. Whether you need a last-minute vaccination, a travel health consultation, or a confidential STI check, our expert team is here when it suits you.
Expert Care Under One Roof
Our Central London clinic is a one-stop destination for your health needs. We provide:
- Travel vaccinations and advice for global travellers
- Comprehensive full medicals for individuals and corporate clients
- STI testing and sexual health services with same-day results
- Occupational health assessments for businesses and professionals
- On-site laboratory testing, so you get fast and accurate results
Conveniently Located in Central London
You’ll find us just moments from Temple, Blackfriars, and City Thameslink stations, making it simple to stop by before or after work. If you’re looking for a private clinic in London that offers expert medical care with flexible hours, Fleet Street Clinic is here to help.
Or explore our most popular services:
Flu jabs might not be at the top of everyone’s to-do list, but protecting your people and your business should be. And if you’re booking your workplace flu programme, it’s smart to think double: flu and Covid.
With higher-than-expected demand for both the flu and updated Covid vaccines, some suppliers are already reporting limited availability. Combining flu and Covid vaccinations into one workplace clinic is the most efficient way to protect your team and your business from the two biggest seasonal health threats.
Flu and Covid-19 haven’t gone anywhere. Both viruses are expected to co-circulate during the 2025/26 winter season, especially in indoor workplaces where people spend long hours together. Offering both vaccines in a single appointment helps ensure your team is protected from both threats before the peak hits. According to the latest GOV UK data, Covid cases rose by 20% in the last week of September, with early signs of an uptick in flu as the season gets underway (Gov, 2025).
Co-infection with flu and Covid can happen and it’s not something you want your team dealing with during the busiest months of the year. One common concern is whether getting both jabs at once is “too much” for the immune system. It isn’t. A study published in The Lancet confirmed that co-administering flu and Covid vaccines is safe, effective and does not reduce the immune response to either jab (PubMed). So yes, we recommend two jabs, one appointment.
From an organisational point of view, a combined flu and Covid vaccination clinic is a no-brainer. It means:
- A single visit
- Less time away from desks
- Easier scheduling
- No need to send multiple reminders or manage two booking systems. Plus, it improves uptake. Employees are more likely to get both when it’s quick, convenient, and all in one go.
The cost of absenteeism continues to rise, and preventable illnesses like flu and Covid are major contributors. According to Verve Healthcare, UK employers lose up to £702 per employee each year due to absenteeism, much of it linked to illnesses that vaccination can help prevent (Verve Healthcare, 2025). Running a combined vaccine clinic is one of the most effective ways to reduce that cost.
It also sends a clear message: your business cares about health, safety, and staying operational through the most unpredictable months of the year. Whether your team is on-site, hybrid, or split across multiple locations, we can help design a solution that works for you.
Protect your people. Protect your productivity.
Get in touch to learn more.
Sources: https://www.gov.uk/government/publications/flu-vaccination-programme-information-for-healthcare-practitioners/flu-vaccination-programme-2023-to-2024-information-for-healthcare-practitioners – GOV UK, 2025 https://pubmed.ncbi.nlm.nih.gov/34800365/ – Pubmed https://www.vervehealthcare.co.uk/blog/the-real-cost-of-absenteeism-to-uk-employers-in-2025-a-complete-analysis/ – Verve Healthcare, 2025
Your mental health matters every day and is just as important as your physical health.
October 10th is World Mental Health Day, a reminder that mental wellbeing matters for everyone. This year’s theme “Access to Services: Mental Health in Catastrophes and Emergencies” highlights how life’s unexpected events, from personal challenges to broader crises, can put pressure on our mental health. At Fleet Street Clinic, we see how even small, subtle changes in mood, energy, or sleep can signal a need for support, long before someone might feel they “can’t cope.”
Mental health conditions affect many people in the UK. According to the World Health Organization (WHO, 2025), one in eight people globally experience mental health issues, yet access to services is often limited, particularly during emergencies. Stress, anxiety and low mood can arise from major life events, workplace pressures, or ongoing personal challenges. Even everyday stress, if ignored, can build up, affecting sleep, appetite, focus and relationships.
At Fleet Street Clinic, we encourage patients to seek support early, before problems escalate. Regular GP consultations are a safe space to discuss changes in mood, energy, or mental clarity. Early assessment allows healthcare professionals to provide reassurance, offer coping strategies and, if needed, guide patients to specialist services. Addressing mental health proactively helps prevent it from impacting physical health, daily routines or overall quality of life.
Building resilience doesn’t have to be complicated. Maintaining consistent routines, including regular sleep, balanced nutrition, gentle exercise, and taking small breaks during the day, can help build a foundation for mental stability.
By combining practical strategies, early support and professional guidance, patients can feel empowered to manage mental health proactively. Our approach is supportive, personalised and focused on long-term wellbeing. Even in challenging times, having reliable, professional support can make a significant difference in how patients cope and maintain balance.
Fleet Street Clinic is here to provide GP consultations, guidance and referrals where needed, helping patients feel supported and informed.
Source: who.int
Even when flu jab clinics are free, convenient and promoted well, uptake can still lag and more often than not, the reason is simple: misinformation or confusion.
At Fleet Street Clinic, we frequently hear concerns from our patients about the flu vaccine. In UK studies, a substantial share of vaccine-hesitant adults report uncertainty or mistrust citing doubts about safety, efficacy or health systems as barriers to getting the flu jab. Paired with myths like “I never get ill” or “It gave me flu last time,” these beliefs can seriously affect workplace health outcomes.
So, we’re here to clear them up:
Myth 1: “The flu jab gives you the flu.”
Fact: It’s impossible. Flu vaccines don’t contain live virus.
Myth 2: “I’m healthy, so I don’t need it.”
Fact: Healthy people can still get flu and spread it to others.
Myth 3: “I got the jab last year and still got sick.”
Fact: No vaccine is 100% effective, but the jab reduces symptom severity and speeds up recovery.
Myth 4: “I’m pregnant/allergic/on medication, so I shouldn’t get it.”
Fact: Most people with health conditions are encouraged to get vaccinated. Always consult your GP if unsure.
Myth 5: “I’ll just wait until more people get it.”
Fact: Flu season moves fast. Early protection is far more effective.
When teams understand the real benefits of vaccination, uptake improves, protecting not just individuals but the wider workplace. Busting these myths helps reduce sick days, maintain productivity and create a healthier, more resilient team environment.
At Fleet Street Clinic, we support workplaces by:
– Providing clear guidance on vaccine suitability for staff
– Answering questions in consultations
– Helping organisations plan flu vaccination campaigns that are easy, convenient and trusted
Let’s make this the year your team gets protected and informed. Book your workplace flu clinic today or get in touch to learn how we can support your campaign.
Sources:
- National Library of Medicine, 2023 – https://pmc.ncbi.nlm.nih.gov/articles/PMC9861815/
- National Library of Medicine, 2022 – https://pmc.ncbi.nlm.nih.gov/articles/PMC8935008/
- BMJ Public Health , 2024 – https://bmjpublichealth.bmj.com/content/2/1/e000929
- BMC Health Services Research, 2023 – https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-10141-2
October marks Breast Cancer Awareness Month, an opportunity to focus on breast health and the importance of early detection. In the UK, approximately 55,000 women are diagnosed with breast cancer each year (Breast Cancer Now, 2025). Detecting changes early allows women and healthcare professionals to make informed decisions about care. Routine mammogram screening is recommended for women aged 50 – 70. However, women under 50 may also benefit from earlier screening if they have: – A family history of breast cancer – Known genetic mutations such as BRCA1 or BRCA2 – Previous breast conditions or other risk factors
For these individuals, a personalised plan can be created. This may include: – Earlier or more frequent mammograms – Additional imaging such as ultrasound or MRI – Regular check-ins with a GP to monitor changes
Being familiar with your own breast tissue is an important part of early detection. – Aim to check your breasts once a month, ideally a few days after your period if you menstruate.
How to check – Look at your breasts in the mirror for changes in shape, size, skin texture, or nipple appearance. – Raise your arms and look for the same changes. – Gently feel your breasts lying down and standing, covering the whole breast and armpit area.
Alongside screening and self-checks, lifestyle choices support breast health: – Maintain a healthy weight – Engage in regular exercise – Moderate alcohol consumption – Eat a balanced diet At Fleet Street Clinic, we offer: – Comprehensive preventive health consultations – Guidance on screening – A professional and reassuring environment to discuss concerns and plan care
By taking a proactive approach, patients can stay informed, supported, and confident in managing their breast health at every stage of life. Speak to one of our GP’s.
Sources: (Breast Cancer Now) – https://breastcancernow.org/about-us/why-we-do-it/breast-cancer-facts-and-statistics
Every year, flu season puts intense pressure on healthcare systems, families and businesses. But while headlines often focus on how bad it’s getting, the real success stories sometimes go unnoticed.
In the 2024–25 season, flu vaccinations in England prevented between 96,000 and 120,200 hospitalisations.*(gov.uk, 2025)
That’s tens of thousands of people who avoided emergency care, complications, or weeks spent recovering from serious illness because of a simple, preventative jab.
As a business, your decision to offer workplace flu vaccinations doesn’t just protect your immediate team. It contributes to something bigger:
– Lower transmission in public transport, coffee shops, gyms and shared offices
– Reduced strain on the NHS, freeing up beds for other urgent care
– Improved outcomes for vulnerable populations who can’t fight off flu as easily
Ultimately, your jab strategy is a public health strategy.
At Fleet Street Clinic, we work with corporates and creative teams alike to deliver professional, fast, and minimally disruptive flu vaccinations. Whether you have a team of 20 or 2,000, we tailor your programme with real care.
We’re proud to be part of the collective effort that prevented up to 100,000 hospital stays. And we’d love to help your organisation contribute this year, too.

Source:
(gov.uk, 2025) – https://www.gov.uk/government/news/flu-vaccine-prevented-around-100000-hospital-admissions
Flu season is often underestimated, reduced to tissues, paracetamol and a few days off work. But influenza is a serious highly contagious viral illness (travel health pro) that is that can lead to significant health impacts, lost productivity and widespread disruption in the workplace
The employees presenteeism days can reduce productivity by 32%. It is estimated that the cost to the employer, in terms of productivity loss either due to absence or presenteeism is at £852 per year, peremployee(OHE, 2024).
Flu doesn’t just stay in the office. Employees often bring it home to families, prolonging illnesses and extending time off work and effecting team momentum. It’s not only a health issue; it’s a workforce disruption. The good news is it is preventable. At Fleet Street Clinic, we provide fast, professional workplace flu vaccinations designed to protect your team and maintain performance through the winter months.
Why invest in workplace flu jabs?
– They minimise downtime during a critical business quarter
– Prevent cross-infection across the teams and departments
– Minimise staff absence and lost revenue
– They are tax-deductible business expenses
Invest in your people and keep your business running smoothly this winter.
Book your workplace flu clinic today. Let’s protect your team and your productivity.
Sources:
Travel Health Pro, 2024 – https://travelhealthpro.org.uk/factsheet/51/influenza-flu
OHE, 2024 – https://www.ohe.org/publications/employer-costs-from-respiratory-infections/
CIPD Health & Wellbeing at Work 2025 – https://www.personneltoday.com/hr/sickness-absence-2025-cipd-simplyhealth 
A recent outbreak of Chikungunya virus (CHIKV) in Italy has raised alarms across Europe, urging travellers to take extra precautions. Approximately 110 locally acquired chikungunya cases have been reported in Emilia-Romagna and Veneto regions in Italy since July 2025. Chikungunya cases have not been reported in Italy since 2017.
While Chikungunya is typically found in tropical and subtropical regions, the spread of the Aedes mosquito responsible for transmission – active from sunrise to sunset – has now extended into Italy. This has led to heightened concerns, particularly as the region remains a popular destination for UK travellers.
Chikungunya is a viral infection that can cause sudden high fever, debilitating joint and muscle pain, headaches, skin rashes, and photophobia. While most people recover in 1–2 weeks, up to 12% of people can suffer from joint pain that can persist for months to years, and in rare cases, the virus may lead to more serious complications.
At Fleet Street Clinic, we now offer two Chikungunya vaccines for eligible travellers:
IXCHIQ: A live attenuated vaccine suitable for immunocompetent individuals aged 18–59 years.
Vimkunya: A virus-like particle vaccine using recombinant DNA technology available for individuals aged 12 years and older
There is no specific antiviral treatment for Chikungunya, therefore making prevention through vaccination and mosquito bite avoidance essential. Travellers to affected areas should consult a healthcare professional for up-to-date advice and vaccine suitability.
References
https://travelhealthpro.org.uk/disease/31/chikungunya
https://www.travax.nhs.uk/news/news-record-page?newsid=24899
https://www.travax.com/account/login/index?ReturnUrl=%2Flibrary%2Fchikungunya
September is Alzheimer’s Awareness Month, highlighting the importance of brain health and dementia prevention. In the UK, over 900,000 people live with dementia (Alzheimer’s Society, 2024), with Alzheimer’s disease being the most common type. Whilst there is no cure, taking proactive steps can reduce your risk or delay onset.
There are several proven ways to help protect your brain:
– Stay physically active as exercise improves circulation and supports brain function.
– Eat a balanced diet by prioritising lean protein, fruits, vegetables, whole grains and healthy fats.
– Keep mentally and socially engaged like reading, puzzles and social interaction stimulate your brain.
– Manage cardiovascular risk factors as high blood pressure, cholesterol and diabetes can increase dementia risk.
– Prioritise sleep and stress management as poor sleep and chronic stress negatively impact brain health.
Recent observational studies (npj vaccines, 2025) suggest that certain adult vaccines may also support long-term brain health. Research on the shingles vaccine (Shingrix) and the RSV vaccine (Arexvy) both containing the AS01 adjuvant shows a potential link to reduced dementia risk.
- Adults who received Shingrix had an 18% lower dementia diagnosis rate compared to those who only received the flu vaccine.
- Adults who received Arexvy had a 29% lower dementia diagnosis rate.
- Receiving both vaccines was associated with a 37% reduction in dementia risk, suggesting a potential additive effect.
These findings highlight an exciting area of research and the importance of keeping vaccinations up to date.
Our clinic can help you to:
– Review your vaccination history for shingles and RSV vaccines
– Book same day appointments
– Provide personalised advice for preventive health strategies
Alzheimer’s Awareness Month is a reminder to take proactive steps for your brain health. Keeping up to date with vaccines like Shingrix (NHS, 2023), alongside lifestyle measures, can be a simple yet impactful way to protect your future.
Book your appointment today to review your vaccinations and receive expert advice. (link booking system)
Read The Times article on vaccines and dementia (https://www.thetimes.co.uk/article/shingles-vaccine-dementia-risk-study-2025)
Sources:
Alzheimer’s Society, 2024 – https://www.alzheimers.org.uk/about-us/policy-and-influencing/dementia-scale-impact-numbers
npj vaccines, 2025 – https://www.nature.com/articles/s41541-025-01172-3
NHS, 2023 – https://www.nhs.uk/vaccinations/shingles-vaccine/
Our feet carry us thousands of steps every day through work, exercise and daily life but they’re often neglected until pain or problems appear. Keeping your feet healthy is key to staying active, preventing injury and avoiding common issues like corns, fungal infections and cracked heels.
Podiatrists often see the impact that poor footwear, nail care and lack of daily attention can have. That’s why our in house podiatrist, Megan, has put together these five simple foot care tips to keep your feet comfortable and problem-free.
1. Choose the right footwear
Wearing the right shoes for your foot shape is one of the most important steps in preventing foot pain.
- Length: Leave a finger’s width of space from your longest toe to the end.
- Width: Shoes should match the natural shape of your foot, not squeeze it.
- Depth: Ensure enough room above your toes to avoid rubbing and blisters.
- Support: A shock-absorbing sole and cushioned insole reduce pressure.
- Fastenings: Laces or Velcro keep the foot stable and reduce injury risk. If you wear shoes with laces, it’s important to unlace them when removing so that the shoe is anchored to the foot correctly.
2. Practise good foot hygiene
Clean, dry feet are less prone to infections and odour.
- Wash feet daily with soap and water. – Dry thoroughly between the toes.
- Choose breathable socks, cotton or moisture-wicking sports fabrics and change daily (or more if exercising)
3. Moisturise to prevent dry skin
- Cracked heels and calluses can cause discomfort and even infection.
- Apply a urea-based foot cream (10% for mild dryness, 25%+ for tougher skin).
- Avoid applying cream between toes (to prevent fungal growth).
- Allow 10–15 minutes for the cream to absorb before putting on socks or shoes.
4. Trim toenails correctly
Incorrect toenail trimming is a common cause of ingrown toenails.
- Cut straight across, never too short.
- Smooth edges with a file to prevent digging into the skin.
- See a podiatrist if nails are thick, painful, or difficult to cut.
5. Manage hard skin & calluses
- Hard skin builds up in pressure areas and can lead to corns.
- File little and often (1 to 2x per week).
- Use a pumice stone on wet feet, or a foot file on dry skin.
- For painful corns or stubborn calluses, book an appointment with a podiatrist.
- Healthy feet are essential for mobility, comfort and quality of life. With these foot care tips, you can reduce your risk of foot problems and stay active every day.
If you’re experiencing persistent pain, fungal infections, thick nails, or hard skin, our podiatry team can help. Click here to book your appointment online today.
- On-site flu jab clinics (at your office, your schedule)
- Drop-in appointments at our Fleet Street location
- Tailored communications for your teams to boost uptake
- High fever
- Severe joint and muscle pain
- Fatigue
- Rash
- Headache
Lyme Disease: Awareness, Action, and Early Detection
Recent news coverage of Justin Timberlake’s account of his own Lyme disease experience shines a light on a condition many still struggle to recognise early, particularly in the UK, where clinicians and the public are much less familiar with ticks and tick-borne diseases than in the USA. This presents an opportunity, not just to raise awareness, but to improve how we support patients from first symptoms through recovery.
Lyme disease, caused by Borrelia burgdorferi and spread by Ixodes ticks, is most effectively treated when identified early. A high index of suspicion is key, especially for patients presenting with fatigue, fever, joint pain, or a recent history of spending time outdoors – even if the classic rash (shown helpfully on NHS and CDC websites here – https://www.nhs.uk/conditions/lyme-disease/ and https://www.cdc.gov/lyme/hcp/clinical-care/erythema-migrans-rash.html) isn’t present.
With changing climates and wider distribution of ticks, we’re seeing cases in new regions. This makes it all the more important for clinicians everywhere to ask about travel, outdoor exposure, and symptom onset timing. Patient outcomes improve when we listen carefully and act promptly.
As I outlined in my recent article for The Telegraph, preventing tick bites is simple, effective, and key to avoiding Lyme disease and other tick-borne infections. Here’s a condensed guide that travellers may find helpful:
Quick Tips to Prevent Tick Bites
- Stick to paths – Avoid tall grass and dense undergrowth
- Dress wisely – Long sleeves, trousers tucked into socks, and light-coloured clothing help
- Use repellent – Apply DEET (20–30%) to skin, permethrin to clothing
- Do a tick check – Shower and check the body thoroughly after outdoor activities
- Clean clothes properly – Wash and tumble dry on high heat to kill ticks
To fellow practitioners: What strategies have you found most effective in promoting early recognition and patient education around Lyme disease in your practice?
Here’s a link to the article for anyone interested: https://www.telegraph.co.uk/gift/dd43d39bde2df95d
Measles is back in the news, and it’s not just affecting children. Many adults may not realise they are not fully protected against this highly contagious disease. With travel, schools, and public spaces being common areas for exposure, now is the time to make sure your vaccinations are up to date.
We’re here to help guide you through the process of understanding your vaccination status, offering MMR catch-up appointments, vaccine reviews and expert advice for individuals, families and businesses.
Measles outbreaks have increased globally, particularly in areas where vaccination rates have dropped. The pandemic has contributed to gaps in vaccination coverage, with many children missing MMR doses and adults assuming they’re fully protected.
A key reason for low vaccination rates in certain populations is a misinformation campaign that occurred in the 1990s. Led by Andrew Wakefield, the campaign falsely linked the MMR vaccine to autism, causing widespread fear and leading to thousands of children missing out on their measles coverage. Many of these individuals are now adults who, as children, were not vaccinated due to their parents’ decision not to vaccinate them. Fortunately, many of these individuals are now choosing to take the vaccine and catch up on their missed doses. At Fleet Street Clinic, we’ve vaccinated many of these individuals, offering them the protection they were previously denied. Whilst measles is commonly associated with childhood it’s important to understand that adults can also be at risk if they missed the MMR vaccine or didn’t receive a booster dose. Vaccination rates have also been affected by the pandemic as many children missed out on their MMR doses, leaving them vulnerable. This means that public health could be at risk, particularly in communities where vaccination rates have dropped below the 95% threshold. Measles spreads easily through airborne droplets when an infected person coughs or sneezes. This makes it highly contagious in crowded places like schools, airports and travel hubs. If you’re travelling abroad, particularly to countries with lower vaccination rates, your risk of contracting measles can be higher. Schools and day-care centres are also common places where outbreaks happen due to close contact among children.
Want to protect yourself? If you’re unsure of your MMR vaccination status, it’s important to speak with your GP about getting a catch-up vaccine. For children, the MMR vaccine is typically given in two doses, the first at 1 year old and the second at 3 years old. However, if your child missed doses, it’s important to get them up to date. For adults, a booster dose may be needed to ensure continued immunity against measles, mumps, and rubella. We offer same-day appointments for MMR catch-ups and immunity blood tests. Our trusted GP led team is here to provide expert travel health advice, ensuring you’re fully protected.
Book your appointment today.

We would like to welcome our new podiatrist Christopher Barrett to the Fleet Street Clinic team.
Christopher is a podiatrist with over 10 years experience working in both NHS and private clinics.
Christopher is experienced in a wide range of podiatry care and treatments including routine podiatry, wound treatment, verrucae management, nail surgery and foot mobilisation.
Christopher will be working at Fleet Street Clinic on Mondays starting from the 23rd of June 2025.
There is a new name for the most advanced of the pneumococcal pneumonia vaccines: the previous version, Apexxnar, has now been re-branded as Prevenar 20. Although this may result in some initial confusion for medical stall and patients alike, the composition and effectiveness of the vaccine are unchanged. Under its new name, however, it is now licensed for adults and children alike – in fact for everyone over 6 weeks of age.
If you have been previously vaccinated with Apexxnar, there is no reason to be revaccinated. However, if you have been vaccinated with a previous version of Prevenar (such as Prevenar 13), it makes good sense to update now to Prevenar 20, which covers more strains.
Prevenar 20 provides protection against the 20 most important strains (called serotypes) of pneumococcal bacteria, offering a more comprehensive defence against pneumonia.
Covid vaccine updated
Another respiratory vaccine has also had an important update: privately available Covid vaccines will now cover the currently predominant variant, KP.2. Covid cases rose by ten per cent in February, and vaccination is an important protective measure, reducing the likelihood and severity of infection. (It seems that the NHS spring Covid booster campaign is based on the previous JN.1 vaccine.)
Prevenar 20 and the updated Covid vaccine, together with vaccination against RSV, flu and whooping cough, make up the 5 vaccines now available to prevent respiratory infection.
If you would like to find out more about these vaccines, consider making an appointment with one of our knowledgeable nurses or doctors.
About Pneumonia:
Pneumonia is a lung infection that can cause a range of symptoms, including:
- Cough: A persistent cough that produces mucus or phlegm is a common symptom of pneumonia. The cough may be dry or productive, and the mucus or phlegm may be green, yellow, or rust-coloured.
- Fever: Pneumonia often causes a high fever, which may be accompanied by chills and sweats.
- Shortness of breath: Pneumonia can cause difficulty breathing, especially during physical activity. The shortness of breath may be accompanied by chest pain or tightness.
- Fatigue: Pneumonia can cause extreme tiredness and weakness, making it difficult to carry out normal daily activities.
- Muscle aches: Pneumonia can cause muscle aches and joint pain, which may be mistaken for the flu.
- Chest pain: Pneumonia can cause chest pain, especially when breathing deeply or coughing.
- Nausea and vomiting: Some people with pneumonia may experience nausea and vomiting, especially if the infection is caused by a type of bacteria known as Legionella.
- Confusion or disorientation: Pneumonia can cause confusion or disorientation, especially in older adults and people with underlying health conditions.
It’s important to seek medical attention if you experience any of these symptoms, as pneumonia can be a serious and potentially life-threatening condition.
More information on pneumonia.
Who is considered “high-risk”?
Individuals considered to be at high risk for hospitalisation due to pneumonia include the elderly, young children, people with weakened immune systems (including people who have had their spleen removed), and individuals with underlying health conditions such as chronic heart or lung diseases, diabetes, and liver or kidney problems.
At the Fleet St. Clinic, we also regard anyone who has had a previous significant episode of pneumonia as likely to benefit from being vaccinated.
When is the best time for a pneumonia vaccine?
The best time to vaccinate against pneumonia depends on various factors such as the type of vaccine, the individual’s age, and underlying health conditions.
Pneumonia vaccine is not necessarily a winter vaccine, and can be given at any time of year.
How to book an appointment?
Booking an appointment is easy. You can book online through our online booking system.
If you would like to discuss anything further or would like to book with our reception team, you can call them on +44 207 353 5678 or email us at info@fleetstreetclinic.com
If you’re taking a medication like tirzepatide (Mounjaro) or semaglutide (Ozempic or Wegovy), for weight loss or type 2 diabetes, and you’re also using the combined oral contraceptive pill, it’s important to know that these might not always work well together. Weight loss injections belong to a group called GLP-1 receptor agonists (or dual agonists in the case of tirzepatide), which help lower blood sugar, reduce appetite, and support weight loss. One of the ways they do this is by slowing down how quickly food moves through your stomach—and that can also slow down how your body absorbs other medications, like the pill.
This can be a problem because the pill relies on being absorbed properly to be effective. If your stomach is emptying more slowly, or if you’re feeling nauseous, vomiting, or have diarrhoea (which are common side effects when starting weight loss injections), there’s a chance your body might not absorb enough of the hormones from the pill to prevent pregnancy. Because of this, the Faculty of Sexual and Reproductive Healthcare (FSRH) in the UK has issued guidance saying that there’s a potential risk of reduced effectiveness when taking oral contraception with GLP-1 medications like tirzepatide or semaglutide.
To stay on the safe side, the FSRH recommends using a non-oral form of contraception—such as the contraceptive implant, IUD (coil), injection, patch, or vaginal ring—since these options aren’t affected by the digestive system and are more reliable in this situation. If you prefer to stay on the pill, you might be advised to use extra protection like condoms, especially during the first few weeks of starting the weight loss medication or if you’re unwell.
If you’re currently on something like Mounjaro or Wegovy and using the pill, it’s a good idea to book an appointment to speak to one of our GPs or sexual health nurses. We can help you figure out what contraceptive method works best for you and make sure you’re fully protected. Everyone’s situation is different, so having that conversation can help you make the best choice for your health and peace of mind.
What is health clearance for the National Performers List?
As part of the application process to apply to the National Performers List, candidates are required to submit a Certificate of Health Clearance. This certificate confirms that the worker is medically fit to practice and ensures all relevant vaccinations have been completed. This certificate is an essential document that is required as part of the application process.
How do I apply for the Certificate of Health Clearance?
All individuals need to complete a medical questionnaire to apply for their health clearance certificate. The questionnaire will ask some general questions about your medical history, which countries you have lived in, and about any previous vaccinations or blood tests you may have taken. Once you have submitted your medical questionnaire, an occupational health nurse will review your application. After review, if any vaccinations or blood tests are required, they will let you know.
How do I know what tests and vaccinations are required?
All candidates need to demonstrate immunity to measles, rubella, hepatitis b, varicella and tuberculosis. In addition, candidates will also need to undertake EPP screening for HIV, hepatitis B and hepatitis C. C
Individuals who have spent 3 months or more in TB prevalent settings, or countries with a high risk of TB will also need to undertake tuberculosis screening.
Once you have submitted your application form, an occupational health nurse will advise you on what tests or vaccination are required as this can vary slightly between individuals.
I don’t live in the UK, will you accept blood test or vaccinations completed abroad?
There are strict requirements in occupational health for compliance. We are unable to accept blood tests and vaccination records from outside the UK. The exception to this is the BCG vaccination where we can accept a record from abroad. This is because there is no lab test available to confirm immunity for tuberculosis.
What is EPP clearance and what does an ID validated sample mean?
EPP clearance is required for doctors and dentists applying for the National Performers List. Exposure prone procedures (EPP) are invasive procedures where there is a risk that an injury to the worker may result in the patient being exposed to the blood of the health care worker. These procedures include those where the worker’s gloved hands may be in contact with sharp instruments, needle tips or sharp tissues (such as spicules of bone or teeth) inside a patient’s open body cavity.
EPP clearance requires blood tests to be taken for
- Hepatitis B surface antigen
- Hepatitis C antibody
- HIV
Blood tests for EPP clearance need to be taken from an ID validated sample.
ID validation requires the candidate to show photo ID at the time of the blood test being taken , and for this to be documented on their results.
Where can I get the necessary tests done?
The Fleet Street Clinic is able to offer all the necessary blood tests and vaccinations required. As a healthcare worker you will be eligible for a discounted rate. Alternately you may use a provider of your choice and send your blood test results or immunisation to us for review.
How long will the process take?
You have 3 months from submitting your application to complete all the necessary tests and vaccinations. Once you have met all the criteria to be compliant, your certificate of health clearance is issued via email within 48 hours.
It states that the certificate must be issued from a Safe, Effective, Quality Occupational Health Service. What does this mean?
Safe, Effective, Quality Occupational Health Service (SEQOHS) is an accreditation scheme that sets the standards of occupational health services. The Fleet Street Clinic is SEQOHS accredited and can issue compliant certificates for the Performers List.
How can I submit my application?
If you need health clearance to join the National Performers List, contact the clinic or occupational health team prior to making an appointment.
Fill out the form below and we will send you the forms and information needed to submit your application.
At Fleet Street Clinic, we uphold a steadfast commitment to delivering the highest standards of patient care. We are pleased to announce that we have successfully attained reaccreditation from SEQOHS (Safe Effective Quality Occupational Health Service) in 2025. This notable achievement underscores the dedication and expertise of our professional team, as well as our unwavering commitment to maintaining exemplary standards in the field of occupational health services.

Understanding SEQOHS
SEQOHS is an accreditation programme that establishes a benchmark for quality in occupational health services throughout the United Kingdom. It ensures that healthcare providers adhere to stringent standards in various areas, including patient care, clinical governance, and the overall quality of services rendered. Administered by the Faculty of Occupational Medicine (FOM), the reaccreditation process for SEQOHS involves an exhaustive review of clinical practices, staff qualifications, and patient satisfaction, among other crucial factors.
The Significance of SEQOHS Reaccreditation
The attainment of SEQOHS reaccreditation affirms our clinic’s ongoing dedication to providing safe, effective, and superior quality occupational health services. For our patients, this achievement represents a guarantee that the care and guidance they receive align with national standards. Furthermore, it highlights the expertise and experience of our team in delivering solutions designed to enhance employee well-being and organisational health.
The reaccreditation process is comprehensive, ensuring that our clinic continually evolves to meet the demands of regulatory standards and patient needs. It instills confidence in our partners, clients, and patients that we prioritise quality and are committed to consistently improving our services.
The Advantages of SEQOHS Reaccreditation for Our Patients
Quality Care: Through SEQOHS accreditation, our clinic ensures the delivery of all services in accordance with best practices, thus providing patients with confidence in the quality of care they receive.
Expertise: SEQOHS establishes high standards for staff training and qualifications, ensuring our team remains at the forefront of developments in occupational health.
Consistency: Reaccreditation guarantees that we uphold high standards consistently, allowing patients to depend on us for reliable and quality services over time.
Accountability: The accreditation process necessitates regular reviews and audits, ensuring that we consistently meet or exceed the requisite standards of care.
Moving Forward
The reaccreditation by SEQOHS represents a significant milestone in our continued journey toward delivering the highest level of care. At Fleet Street Clinic, we remain committed to providing outstanding occupational health services tailored to fit the needs of both employees and employers.
If you have any questions or want to find out more about how we can help, get in touch with us today on: occhealthadmin@fleetstreetclinic.com
 Among the journalists, television crews, lawyers and other professionals who often have to travel at short notice one of the longest-standing users of the Fleet Street Clinic’s same-day vaccination and travel-health service is the celebrated war photographer Goran Tomasevic.
Among the journalists, television crews, lawyers and other professionals who often have to travel at short notice one of the longest-standing users of the Fleet Street Clinic’s same-day vaccination and travel-health service is the celebrated war photographer Goran Tomasevic.
Softly spoken, calm and courteous, the 6 ft 4 56-year-old Serbian has been ducking bullets and reporting from the world’s battle zones for almost 35 years. Carrying the same equipment wherever he goes – three Canon cameras and three spare lenses, so if one gets damaged he can still continue working – he has spent most of that time working for the global news agency Reuters. His Reuters’ assignments have seen him cover conflict in warzones from Afghanistan, Colombia and Iraq to Libya, Somalia and South Sudan. Voted Reuter’s Photographer of the Year a record-breaking four times, in 2016 he achieved the unique feat of having 100 newspapers around the world put his extraordinary photograph of a fireball in an anti-Gaddafi attack in Libya on their front cover. In 2023 one reviewer of the 444-page book of his pictures, published by Edition, called him ‘ a Caravaggio of photography’. “I want to show exactly how it was … if there’s enough light, I will stay until the end,” he says.
Now working for the Canadian newspaper The Globe and Mail, he will only answer with a cryptic “Asia” when asked about his next assignment. But he is happy to add that wherever precisely that might be – Taiwan, we wonder; perhaps Myanmar? – he will detour via Fleet Street to get any necessary vaccinations and to collect a locale-and-calamity appropriate travel kit. As usual, that will have been made up for him by Fleet Street Clinic’s founder – and now his friend – Dr Richard Dawood.
Q) How did you come across the Fleet Street Clinic?
A) I grew up in Belgrade, and I started working with the Politika news agency during the Bosnian war, in 1991. After all our trouble finished, in 1996 I joined Reuters, and they started sending me to the Middle East and Africa. Their offices were in Fleet Street (they’re in Canary Wharf now) and as they had a contract with Fleet Street Clinic they sent me to the clinic to get jabs and the medical kit, trauma kit, travel kit. From the beginning Dr Richard, he say to me: “Call me any time you’re in trouble!”.
Q) So have you ever had to make that kind of call?
A) Ha ha, many times! The last time, I get a bad reaction for the dengue fever jab. I was about to cross the border between Dominican Republic and Haiti but they sent me back. I had a fever. I was feeling very bad. But after calling Dr Richard I knew where I was standing. He said, don’t worry, it’s not common, but stay in bed and after three days you’ll be ok. Absolutely brilliant! And with an iPhone of course I can send a picture of a rash or a wound and say, Dr Richard, what’s your opinion?
Q) What’s inside your travel kit?
A) It depends where I’m going – tropical area, somewhere very remote, whatever. Not every medication for every possibility, but for a lot of possibilities. In Africa, sometimes you need to walk five to 10 days to find any medical facilities. It’s the nature of the job that often I’m following rebels in a very remote area so you can quickly go through all the kit. In Central African Republic I got some infection and needed to test if I had malaria again. I was in Bambari with Seleka Islamist rebels and there’s nothing there, really. No medical facilities. So the medical kit’s sterile syringes, tests, antibiotics, everything, it’s very useful.
Q) You once said ‘the eye of the sniper is everywhere’. Has it ever caught you?
A) I was shot in my right leg in Egypt. It was a bad experience because the Egyptians told me “It’s just a small pellet, not very deep. It’ll get infected and just jump out.” So I took the antibiotics in the kit but after 10 days I see the infection again and Dr Richard said, “That’s not good, you know.” I saw another Egyptian doctor; he said the same thing: “It’ll jump out!” So I went back to Serbia and I found a military doctor who said, “They’re mad! Look at your leg! If you didn’t come now, you might need amputation.” I always like soldiers, they know what they are doing. He had been in the war in Bosnia. He told me, “I took a lot of metal out of humans. I’ll fix you, boy.” He took out a 8.2mm pellet, gave me more antibiotics, and I was ok.
Q) You’ve also said you love to go into a conflict zone – so where have you been recently?
A) Last year I did Lebanon, spent lots of time in south Lebanon. What else? I can’t remember but I was three times in Port au Prince in Haiti. That was tough. It’s like an outlaw country. Eighty per cent controlled by different gangs. Raiding, burning, taking everything. The last time, I was focussed on child soldiers, kid gangsters. Kids nine, ten, 11, with 9mm guns. Shooting without hesitation, quick reactions, handling guns well. I’ve been in the army but was in total shock, seeing that.
Q) How do you relax when you’ve finished work for the day?
A) Cigarettes. In Haiti I found a hotel at the edge of the front line, the Hotel Plaza.
No one else was staying. Only me with a fixer and two motorbike drivers to move us around. All night you could hear bang, bang and stuff. But the staff were really nice. The food was wonderful. The biggest trouble was, I’m sitting on the balcony, it’s really humid, I’m sweating, and I’m looking at the beautiful blue swimming pool and it’s tempting to jump in it. But Dr Richard told me a long time ago, if a pool isn’t treated with chlorine there’s a high possibility of getting giardia. No guests – hmm, I knew the manager he wouldn’t be spending money on chlorine. My fixer jumped in and he was unwell for two days.
Q) Do you often have to just bed down on the ground while working?
A) Often. One picture I took which became quite famous, that was in Afghanistan, a US Marine Sergeant Bee being shot at. It was very early morning; we had been camping and I had just wake up. When Taliban suddenly started shooting I was still in my just boots and underpants. It was so quick, I didn’t even know if I had the picture.
Q) When did you first pick up a camera?
A) When I am 14, 15, my parents had a bit of desperation to take me off the streets, playing football, fighting, messing around, so my father gave me a camera. And I loved it! It was amazing. It’s a beautiful toy. It was a Russian copy of a German Leica with no light meter. A friend of my sister, Mico Smiljanic, a photographer, helped me a lot. I learned to understand light, what is reflecting light, what is coming in at an angle, how it’s behaving. Everything in photography is about the situation of the light.
Q) How you start working as a photographer?
A) In Belgrade, 1987, when I was 18, I did one year of national service. I was still not behaving well, so my father – he was a chemical technician in a factory – wanted to put me in order. I loved it. It was just before the Bosnian war, so my father did me a great favour. Discipline, waking up early, exercising, all good. Then the Bosnian war started. Serbia was bombed by NATO. I had my camera, I knew how to look after myself, and that’s how I started.
Q) What kind of conflict produces the best pictures?
A) When you’re with soldiers on foot, although now with drones it’s more difficult, drones have really changed the dynamic. When governments and armies create restrictions, then you don’t have good pictures. I don’t want to do only what I’m allowed and what the new security advisors show me. But us who have field experience, we understand we have no idea how we’re going to get the picture. You look, and you see opportunities. You need to be very patient. Sometimes I wait weeks, months. I don’t have any vision of the pictures I want to get. Zero. But when I see an opportunity, I’m going to push for it. I want to see the fear, I want to see the faces, I want to tell the story properly.
Q) Are you usually sympathetic to the cause or side you’re photographing?
A) I’m a journalist: I’m not supporting any side. You have good guys, you have bad guys, and the truth is somewhere in between. I try to cover untold stories important to people.
Q) Do you feel traumatised by what you’ve witnessed – the maiming, desperation, death?
A) You need to be stable in your head, doing this. A couple of years ago in Canada, Anthony Feinstein, a psychologist, wrote a book, Shooting War, about how war affects journalists, especially photographers. They brought a bunch of us with this kind of experience to talk.
A lot of my colleagues have PTSD, mental troubles, as a result of what they’ve seen. I don’t think I have PTSD. But crazy people don’t believe they’re crazy, so maybe I have.
Q) You’ve said you love to go into a conflict zone. Is that still true?
A) When I go to say Syria, I know exactly what I’m doing, where I’m going. I’m not going to Nice or Cannes, the red carpet. I started this work very young, and when you work, if you’re emotional, you are not for this job. You have to work hard, be disciplined. I always joke when the correspondents start running, I’m starting to work. As a journalist, you can write your story about Syria from London. I need to see everything and I need to come close, close, closer.
Q) Your life must be hard on your family
A) Ha ha, I am the perfect husband, away all the time! I’ve been married three times although not now. My daughter, she’s 29. I live now in a village outside Belgrade; when I’m home, I dig my garden, I use the gym, I use the punchbag under my walnut tree. When I say to my daughter, “Do you want to come over, to stay this evening?”, she says, “Dad, I know that just means you want to go to the bar and have me get you home!” But what else am I going to do, be a bus driver? I’m just a yob from Belgrade! A peasant! But I work hard. My mother said once, “I’m just glad you’re not in prison!”
Q) Any regrets?
A) I’m sorry I missed the Battle of Stalingrad. That was the mother of all battles. But 1942, 1943. I was born too late!
HAY FEVER: TIPS AND TEST
Are you one of the many millions in the UK suffering from hay fever at the moment? Learn more about the condition here.
WHAT CAUSES HAY FEVER?
Many allergens are in the air, where they come in contact with your eyes and nose. Airborne allergens include pollen, mould, dust and pet dander.
Other causes of allergies, such as certain foods or bee stings, do not typically affect the eyes the way airborne allergens do. Adverse reactions to certain cosmetics or drugs such as antibiotic eye drops also may cause eye allergies.
Some people actually are allergic to the preservatives in eye drops such as those used to lubricate dry eyes. There are now a wide range of preservative-free brands in unit (single) dose, novel multi-dose bottles and even sprays.
SUMMERTIME EYE ALLERGY TIPS
- Get an early start. See your optometrist before allergy symptoms start this year to learn how to reduce your sensitivity to allergens.
- Try to avoid what’s causing your eye allergies, whenever possible.
- Don’t rub your eyes if they itch! This will release more histamine and make your eye allergy symptoms worse.
- Use plenty of artificial tears to wash airborne allergens from your eyes. Ask your optometrist what they recommend.
- Reduce contact lens wear or switch to daily disposable lenses to reduce the build-up of allergens on your lenses.
- Consider purchasing an air purifier for your home, and purchase an allergen-trapping filter for your furnace.
QUIZ: HAY FEVER EYE ALLERGIES SELF-TEST
Take this quiz to see if you might have eye allergies. Always consult your optometrist / general practitioner if you suspect you have an eye condition needing care.
- Do your eyes often itch, particularly during spring pollen season?
- Are you allergic to certain animals, such as cats?
- Have you ever been diagnosed with “pink eye” (conjunctivitis)?
- Do allergies run in your family?
- Do or have you ever used antihistamines and/or decongestants to control sneezing, coughing and congestion?
- When pollen is in the air, are your eyes less red and itchy when you stay indoors under an air conditioner?
- Do your eyes begin tearing when you wear certain cosmetics or lotions, or when you’re around certain strong perfumes?
If you answered “yes” to most of these questions, then you may have eye allergies.
See here for more information.
Pollen Calendar

For the best course of action or if you have any concerns about the health of your eyes, you can make an appointment online here.
In today’s fast paced world, finding the time to visit a doctor can be challenging. Whether you are juggling a busy work schedule, looking after family, facing mobility issues, or travelling, accessing quality healthcare shouldn’t be difficult. This is where a home visit GP service in London can make all the difference. Fleet Street Clinic offers private GP home visits, ensuring that expert medical care comes directly to you, whenever and wherever you need it.
Why Home Visits Are Essential in London
1. Convenience at Your Doorstep
Navigating London’s traffic and packed public transport can make a short trip to the doctor extremely stressful. A GP home visit removes travel time, allowing you to receive expert medical care in the comfort of your home, office, or hotel.
2. Same-Day Appointments for Immediate Care
Waiting for a GP appointment at a busy surgery can take days, if not weeks. Often, NHS appointments require a registration process that can take several days. With same-day GP home visits in London, Fleet Street Clinic ensures you receive prompt medical attention when you need it most.
3. Personalised and Unhurried Care
Unlike traditional 15- or 30-minute clinic visits that may feel rushed, a private GP home visit allows for a more in-depth consultation. Your doctor can assess your condition in a familiar environment and provide tailored treatment plans suited to your lifestyle.
4. Ideal for Families, Elderly Patients, Busy Professionals, and Travellers
- Parents with young children can avoid exposing them to germs in waiting rooms.
- Elderly patients or those with mobility issues benefit from receiving care without the challenge of travelling.
- Professionals with demanding schedules can fit a GP consultation into their day without taking time off work.
- People travelling into London may need urgent medical attention before flights back home; home visits can also take place in hotels, airbnbs, or any other third party location.
5. Comprehensive Medical Services at Home
Fleet Street Clinic’s private doctor home visits cover a wide range of medical services, including:
- Diagnosis and treatment of illnesses. Prescriptions and medication advice.
- Vaccinations, including flu and travel vaccines. Health check-ups and screenings.
- Chronic disease management.
- Medical certificates and sick notes.
- Wide range of services including blood tests, urine samples, swabs, and more.
Book a GP Home Visit in London Today
If you need a home visit GP in London, Fleet Street Clinic is here to help. We provide professional, same-day medical care wherever you are, ensuring your health remains a priority without the hassle of travel.
Call us now at +44 207 353 5678 to book your appointment or schedule a home visit directly on our website. Take control of your health with the convenience of private GP home visits in London.
Step into the realm of Movember, where the Chevron, the Dali, or the Handlebar becomes more than just a style statement – it’s a symbol of men’s health awareness.
Are you ready to join the Mo-gang and make a statement this Movember?
Movember transcends mere facial hair growth; it’s a global movement dedicated to transforming the landscape of men’s health. This renowned charity, a beacon of hope and change, addresses critical issues like prostate cancer, testicular cancer, and mental health and suicide prevention.
In the heart of London, at Fleet St. Clinic, we’re not just embracing the ‘Mo’ spirit; we’re championing the cause of male health. As the statistics reveal, one man succumbs to prostate cancer every 45 minutes in the UK. It’s time to take charge of your well-being and be part of a movement that’s making a difference.
Prostate Cancer –
Our clinic offers a comprehensive Prostate Cancer check, with an experienced doctor committed to your health journey. This thorough examination includes a detailed health discussion covering lifestyle and family history, an internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Early detection is the key, and we’re here to guide you every step of the way.
Testicular Cancer –
Testicular cancer, the most common cancer among young men in the UK, demands attention. Knowledge is power, and understanding the symptoms can be a lifesaver. A lump or swelling, a heavy scrotum, or discomfort in the testicle or scrotum are health signals not to be ignored. At Fleet St. Clinic, we emphasise the importance of awareness and early detection.
Mental Health –
Let’s break the silence surrounding mental health. The Movember Foundation has spearheaded programs globally, fostering resilience and mental well-being in men. It’s not just about growing a mustache; it’s about cultivating conversations that matter.
Now, let’s talk about your health journey with Fleet Street Clinic’s essential men’s health screenings and medicals.
Medical Health Check (From £495) –
Essential
Review your health with one of our experienced GPs. Benefit from a thorough physical examination and carefully selected health checks and blood tests, including thyroid function.
1 hour appointment with a GP – £495
book online
Executive
Check your health from top to toe, with our more enhanced Executive medical, including an audiometry test to assess your hearing, spirometry tests to assess your lung function, and cancer checks and markers.
1.5 hour appointment with a GP – £745
Executive+
For maximum reassurance and peace of mind, consider our most advanced medical. Benefit from advanced health screenings including a sophisticated cardiac (CaRi-Heart) scan, and a bone density DEXA scan.
3 hour appointment with a GP – £3,950
View our medical health checks in more detail and book online.
Prostate Cancer Check (£225)
Prostate cancer is the most commonly diagnosed cancer in men in the UK. Early diagnosis is crucial.
Our prostate cancer check is carried out by an experienced male GP, who’ll conduct a detailed health discussion, internal (rectal) examination of the prostate gland, and a prostate-specific antigen (PSA) blood test. Swift courier services ensure timely analysis at our nearby pathology laboratory. Our GP will provide you with full support throughout the process and provide aftercare services and referrals if required.
In a world where ‘strong, silent men’ are rewriting their narrative, Movember beckons. Join us at Fleet St. Clinic, where your health is not just a checkup; it’s a commitment to a longer, healthier life.
Book your Appointment now, and let your Mo make a statement for men’s health in London.
According to Prostate Cancer UK, 1 in 8 men will get prostate cancer in their lifetime and it is the most common cancer in men in the UK.
In 2021, around 52,000 men were diagnosed with prostate cancer in the UK alone and the risk of developing it increases with age, as most cases are diagnosed aged 65 and over.
It’s not uncommon for men find out by complete chance, and often it can be too late when the diagnosis is less treatable. For that reason, it’s essential to understand the symptoms, available tests, and the importance of early detection.
What is the Prostate?
The prostate gland is a small, walnut-sized gland located below the bladder and in front of the rectum in males. It plays a key role in the male reproductive system by producing seminal fluid, which nourishes and helps transport sperm during ejaculation.
As men age, the prostate can undergo changes, including enlargement (benign prostatic hyperplasia) or other conditions, such as prostatitis (inflammation) and prostate cancer.
Regular check-ups and awareness of symptoms are important for prostate health.
What is Prostate Cancer?
Prostate cancer occurs when cells in the prostate gland grow uncontrollably.
An enlarged prostate is very common in men over the age of about 50, but having an enlarged prostate is not the same as having prostate cancer.
Having an enlarged prostate doesn’t increase your risk of getting prostate cancer. But it’s possible to have an enlarged prostate and prostate cancer at the same time.
While many men with prostate cancer may not experience symptoms, early detection is vital for effective treatment.
Symptoms of Prostate Cancer
In its early stages, prostate cancer may not cause noticeable symptoms. However, as the disease progresses, some common symptoms include:
- Needing to urinate more often than usual, especially at night
- Difficulty starting or stopping urination
- Weak or interrupted urine flow
- Painful urination or ejaculation
- A feeling that your bladder hasn’t emptied properly
If prostate cancer breaks out of the prostate (locally advanced prostate cancer) or spreads to other parts of the body (advanced prostate cancer), it can cause other symptoms, including:
- Persistent pain in the lower back, hips, or pelvis
- Unexplained weight loss or fatigue
- Blood in urine or semen
- Problems getting or keeping an erection
If you experience any of these symptoms, it’s crucial to consult a healthcare professional for evaluation.
All these symptoms are usually caused by other things that aren’t prostate cancer. But it’s still a good idea to tell your GP about any symptoms so they can find out what is causing them and make sure you get the right treatment, if you need it.
Who Should Consider a Prostate Screening?
- Men aged 50 and older: if you’re at average risk, starting at 50 is recommended.
- Men aged 45 and older: if you have a higher risk, such as a family history of prostate cancer.
Tests for Prostate Cancer at Fleet Street Clinic
Several tests can help confirm the presence of prostate cancer:
- Prostate-Specific Antigen (PSA) Test: This blood test measures the level of PSA, a substance produced by the prostate gland. Elevated PSA levels can indicate prostate cancer, but they can also be elevated due to benign conditions such as an enlarged prostate. A normal PSA indicates that the chance of a prostate cancer is very low.
- Digital Rectal Exam (DRE): During this exam, a doctor manually examines the prostate for any irregularities or lumps. While this test can help identify abnormalities, it is typically used in conjunction with the PSA test.
Consider booking a GP appointment for either of these Prostate Cancer tests, or for a more comprehensive assessment, opt for our Prostate Cancer Check, which includes both tests.
Factors That Can Cause the PSA to be Falsely Raised
Several factors can cause a false elevation in Prostate-Specific Antigen (PSA) levels, potentially leading to misleading test results. Here are common causes:
- Recent Ejaculation: Sexual activity, especially ejaculation, can elevate PSA levels temporarily. Avoid sexual activity for 24–48 hours before a PSA test.
- Prostate Manipulation: Any recent procedures or physical manipulation, such as a digital rectal exam (DRE) or catheter insertion, can elevate PSA levels. Let your doctor know if you’ve had any recent prostate exams or urological procedures.
- Vigorous Exercise: Activities that put pressure on the prostate, like cycling or horseback riding, can raise PSA levels temporarily. Avoid these activities for a f48 hours before the test.
- Prostate Infections or Urinary Tract Infections (UTIs): These infections can cause inflammation and increase PSA levels. Treat infections and allow recovery before testing.
- Benign Prostatic Hyperplasia (BPH): An enlarged prostate from BPH can raise PSA levels even though it’s not cancerous. Make sure your doctor considers this in the interpretation.
- Certain Medications: Some drugs, like testosterone, can increase PSA levels, while others like finasteride (for hair loss or BPH) can decrease it. Inform your doctor of any medications you’re taking.
Avoiding or managing these factors before a PSA test can help improve the accuracy of the results. Always discuss any concerns with your doctor.
You may need additional tests, as listed below, if your PSA is raised or if there is concern from the examination. We can refer you to specialists who may be available for same-day consultations to provide further evaluation.
- Imaging Tests: Additional imaging tests, such as an MRI or CT scan, may be conducted to visualise the prostate gland.
- Biopsy: If initial tests indicate potential cancer, a biopsy is often performed to confirm the diagnosis. During this procedure, a small sample of prostate tissue is removed and examined under a microscope for cancer cells.
Movember, an organisation focused on raising awareness of men’s health issues, including prostate cancer, emphasises the importance of regular check-ups and understanding one’s own health risks. Their campaigns encourage men to talk openly about health issues, promoting early detection and treatment.
Prostate cancer is a serious health concern for men, but awareness and early detection can lead to better outcomes. Regular check-ups and understanding the symptoms are essential steps in addressing this disease.
If you have concerns about prostate cancer or related symptoms, don’t hesitate to seek medical advice by booking a GP appointment. Early action can make a significant difference in your health and well-being.
Related services at Fleet Street Clinic
Prostate Cancer Check
Private GP Appointments
Annual Medical
Blood Tests
Egypt has long been a fascinating destination for travellers with its ancient monuments, rich culture, and vibrant landscapes. Now, there’s even more reason to consider Egypt as a travel destination: the World Health Organization (WHO) has officially declared the country malaria-free.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, said “Malaria is as old as Egyptian civilisation itself, but the disease that plagued pharaohs now belongs to its history and not its future.
This is a significant milestone in public health and brings an added layer of safety and assurance to travellers planning to visit.
Here’s what you need to know about this important achievement and what it means for your health when traveling to Egypt.
What does it mean to be “Malaria-Free”
To be certified as malaria-free, a country must demonstrate that it has interrupted local transmission of malaria for at least three consecutive years. Egypt met this requirement, showing consistent results in controlling the disease, improving healthcare infrastructure, and reducing the risk of reintroduction.
According to the WHO, Malaria in Egypt has been traced as far back as 4000 B.C.E., with genetic evidence of the disease found in Tutankhamun and other ancient Egyptian mummies.
Egypt is one of the latest countries to receive this certification, contributing to a global push toward eradicating malaria worldwide.
What does it mean for travellers?
Malaria has long been a concern in various tropical and subtropical regions, causing severe illness, fever, and sometimes even death.
Travellers often must take preventative steps, such as antimalarial medication and mosquito avoidance measures, when visiting areas where malaria is prevalent.
Egypt’s certification as malaria-free means travellers now have one less health risk to consider when planning their holiday.
For the tourism and travel health sectors, this achievement reassures visitors that Egypt is safe from malaria transmission, especially in rural areas and near water sources, which are typically high-risk locations for malaria-carrying mosquitoes.
Are there any precautionary measures still needed?
While Egypt’s malaria-free status is excellent news, it’s still essential to practice general travel health precautions to stay safe.
Here are some tips:
- Protect Against Other Mosquito-Borne Diseases: While malaria may not be a concern, other mosquito-borne illnesses, such as West Nile Virus and Dengue Fever, can still pose risks. Use insect repellent, wear long sleeves, sleep under a mosquito net and consider vaccinations where possible, like Qdenga for Dengue Fever.
- Stay Up-to-Date on Vaccinations: Egypt does require certain vaccinations for travellers, such as Rabies, Hepatitis A, Hepatitis B, and Typhoid. Make sure you are aware of any health advisories and have up-to-date vaccinations before your trip.
- Practice General Travel Hygiene: Staying hydrated, avoiding untreated water, and being cautious with food preparation are essential for staying healthy on your travels.
Is a travel consultation still necessary?
Yes, whilst it is fantastic news that Egypt is now malaria-free, there are other health risks to consider when travelling and it is still important to seek travel health advice from an expert.
We advise booking a travel consultation at least 4-6 weeks before your departure date to allow enough time for any necessary vaccinations, medications, and preventive advice to take full effect.
If you’re planning a last-minute trip, don’t worry! Book a consultation as soon as possible; even a brief appointment can provide valuable advice, essential vaccinations, and immediate preventive tips to keep you safe during your travels.
The Future of Malaria Control in the Region
Egypt’s success in eradicating malaria is a hopeful indicator for neighbouring regions where malaria is still a concern. The country’s strategies and investments in healthcare could serve as a model for other nations aiming to reduce or eliminate malaria.
Planning Your Malaria-Free Trip to Egypt
Whether exploring the pyramids, cruising the Nile, or enjoying the coastal resorts, travellers to Egypt now have added peace of mind regarding malaria. However, consulting with a travel health specialist before your trip remains important to ensure your overall health and safety. By staying informed and prepared, you can focus on enjoying the cultural and natural wonders Egypt has to offer.
As always, our travel health experts are here to provide personalised advice, vaccination guidance, and preventive health tips to make sure your journey is as safe and enjoyable as possible.
Book a travel consultation to discuss your upcoming trip to Egypt.
Related services at Fleet Street Clinic
Specialist Travel Clinic
Travel Vaccinations
Dengue Fever
Rabies Vaccination
Antimalarials
According to Menopause Support, approximately 13 million peri, current and post-menopausal people are living in the UK today.
This makes up a whole third of British women.
Despite making up such a large portion of society, a lot of women find themselves feeling ashamed, shunned or invisible due to their symptoms and the lack of discussion surrounding the subject of menopause.
What is menopause?
Menopause simply means no periods for 12 months and usually begins between the ages of 45-55, but it may start earlier. 80% of women are menopausal by the age of 54 years, so an average woman spends one third of her life being menopausal. In the lead up to menopause, women often experience symptoms of ‘perimenopause’. Changes in the menstrual cycle, hormonal fluctuations and ‘hot flashes’ can all occur as the ovaries begin to stop producing eggs. It is important to note that menopause is a natural transitionary period in life and is not a disease or illness.
What are the symptoms of menopause?
80% of women suffer some symptoms.
Meaning 20% of women have no symptoms at all, and of the 80 % who do suffer some symptoms, only 25% want or need treatment.
Some of the physical symptoms of menopause may include, but are not limited to:
- Night sweats
- Hot flushes
- Dizziness
- Fatigue
- Headaches
- Recurring UTIs
- Stiff joints, aches and pains
- Heavy periods
- Insomnia
- Itchy skin
- Osteoporosis
- Weight gain
Menopause is not only characterised by physical health symptoms, but mental health can also be affected by it too.
Some symptoms might include:
- Anxiety
- Memory loss
- Depression
- Reduced concentration
- Brain fog
How can I manage symptoms for menopause?
A healthy diet and regular exercise, alongside simple lifestyle changes, may improve some symptoms and are important parts of the toolkit in dealing with menopause. Reducing nicotine, alcohol and caffeine intake further assist in reducing symptoms as well.
‘Phytoestrogens’ also help, and these are found in foods like soya protein, beans, yams and nuts. These non-hormonal treatments should always be tried first before hormonal treatments like HRT, which top up hormone levels.
World Menopause Day
World Menopause Day is recognised every year on October 18th to attempt to break the stigma around menopause and highlight the support available to women when they’re experiencing symptoms.
This year’s theme is based on HRT and the various pros and cons.
HRT works by replacing the hormones lost in the menopause process and can relieve symptoms of menopause to a manageable degree. Many women see it as a necessity for managing their menopause symptoms.
However, studies have shown that HRT can slightly increase the risk of breast cancer. This may sound concerning but the risk reduces when using oestrogen only HRT, rather than combined. HRT for managing menopause is an ongoing discussion in the medical field, but a lot of women experiencing menopause find the benefits outweigh the risks, and your GP will be able to advise whether HRT is the right solution for you.
How can Fleet Street Clinic help me?
If you think that you are beginning to experience symptoms of perimenopause or are suffering with your current symptoms, it may be time to book a GP appointment to discuss your menopause and see how we can help you.
Menopause can be a scary transition, but we want to do everything we can to make it as easy as possible for you.
Book a GP appointment today and let us support you.
More information:
October is Breast Cancer Awareness Month
You may notice an increased amount of pink during this month, especially iconic pink ribbons, and it’s for a good reason: October is Breast Cancer Awareness Month.
This annual campaign aims to increase the awareness of the disease and to raise funds for research into its cause, prevention, diagnosis and treatment. With the hope that in the not too distant future, a cure will be found!
Breast Cancer is the most common cancer in the UK. 1 in 8 women in the UK will be diagnosed at some point in their lives.
In the UK, over 55,000 women each year are diagnosed with Breast Cancer which is the most common cancer. Thanks to research, more people are surviving breast cancer than ever before, yet there are still nearly 1,000 women who’ll die of breast cancer each month. Breast cancer is often thought of as something that only affects women, but men can get it in rare cases. It is important for males (especially those over 75 years with a high BMI) to check breast tissue for abnormalities as well.
We will be sharing important information on symptoms, causes and lifestyle alteration you can make to reduce your risk.
We are urging everyone, especially women, to check their breasts regularly and get checked out by a professional if something seems unusual for you.
REMEMBER: The earlier breast cancer is diagnosed, the easier it is to treat and the better the chance of successful treatment.
BREAST CANCER SYMPTOMS TO LOOK OUT FOR:
- a new lump or thickening in your breast, upper chest area or armpit
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
- Unexplained pain in your breast or armpit that’s there all or almost all the time
How to check your breasts
Checking your breasts yourself means you’ll get to know what is “normal” for you. As a society we are probably not that familiar with how our body currently is and so that makes it difficult to know what subtle changes happen. It’s most likely that unless a dramatic change has occurred a subtle change will go unnoticed.
So, how do you check your breasts?
There is no special technique and you don’t need any training to start checking your breasts. It may feel like you’re unsure what you’re doing but get to know your body and any breast check is better than no breast check.
The easiest and most accurate way is to divide the breasts into four quadrants; the upper outer quadrant, outer lower quadrant, inner lower quadrant and inner upper quadrant. Examine each quadrant with the flat of your hand. It is important to do this regularly so that you are familiar with what each breast feels like normally. That way, should you notice any changes, (hopefully not), you will pick them up straight away and changes won’t go unnoticed. It is important to remember to check your armpits as well. It is surprising how many breast lumps are discovered after an “axillary” or armpit lymph node is found and checked.
Breast Cancer Now advises the TLC method – “touch, look and check”.
Touch: Can you feel anything new or unusual?
Look: Does anything look different?
Check: Any changes with your GP
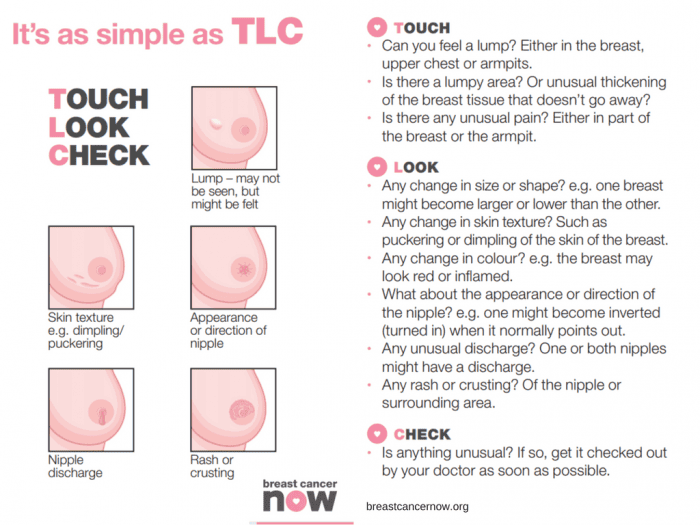
You should check your breasts Regularly
Get to know your “normal” by checking your breasts regularly. Get in the habit of checking your breasts at least every month. It can be easier whilst in the bath or shower.
Your breasts can change throughout your life for many reasons – like the menopause, pregnancy and breastfeeding, or puberty. So, if you check them regularly, you’ll be able to spot any new or unusual changes that should be checked out by a GP.
For young and pre-menopausal women it is advised to check mid-cycle (a week after their period finishes) if there are any changes this requires checking with your GP.
As older women are of a higher risk of breast cancer, due to age, it is advised they check even more frequently. Older women should check on a monthly basis without exception. It is advised for men to check also.
Any lump requires attention and checking with your GP immediately.
In addition to regular self-checks, it is important to never miss a mammogram appointment. They may be painful and momentarily uncomfortable, but a mammogram can save your life. If you have a long wait for a mammogram, are unable to access an appointment or just want an additional check, contact the Fleet Street Clinic and we should be pleased to help.
What are the causes of breast cancer?
There are several factors that contribute to increasing your risk of developing breast cancer. There is no single cause, and has to do with our lifestyle, environment and genetics. There are factors which we simply cannot control such as getting older, family history, inherited genes, dense breast tissue, hormones and age at which period started and stopped. However, there are some lifestyle choices that if altered can reduce your risk of breast cancer.
Lifestyle change that will reduce your risk of breast cancer
1. Your weight
Being overweight or obese has a high risk of breast cancer in both men and women (especially after menopause). You can work out your ideal weight using a BMI (Body Mass Index) calculator, this checks your height and weight to see if you are at a healthy weight. For the majority of adults an ideal BMI ranges from 18.5 to 24.9. A BMI between 25 – 30 means overweight. Obesity means a BMI of 30 and above.
2. How much alcohol you drink
Alcohol consumption increases the risk of breast cancer. The risk is greater with each extra unit per day, the latest UK guidelines state no more than 14 units a week.
3. How much exercise you do
Being inactive contributes to a small increased risk of breast cancer, this qualifies as doing less than 150min of moderate activity on a weekly basis. This does not necessarily mean sport and exercise, anything that makes you warmer and out of breath counts.
Throughout October we’ll be highlighting the reasons to support this campaign across our social media platforms. We will be sharing inspirational stories from those who have survived the disease and those who are currently battling. We will also hear from those who have supported a suffering loved one during treatment. Sharing these stories humanises the disease and can provide support/tips for those who may be struggling with a current diagnosis. We will be sharing ways of checking for early warning signs. We’ll also be encouraging all to undertake a Well-Woman or Well-Man health checks. Both of which contain a breast examination.
At Fleet Street Clinic, we specialise in women’s health and have four female GPs on-site to facilitate well-woman health checks. Our Executive Well Woman medical is focused on protecting your well-being and involves a full examination including breast examinations and cervical screen tests. Our comprehensive medical is designed to screen for health problems at the earliest possible stage.
Book Your Well Woman Medical Online. Or if you notice any changes to your breast or have any concerns, you should book a GP appointment as soon as possible.
_______________
To find out more from Breast Cancer Now, visit breastcancernow.org
Here at Fleet Street Clinic, we have had many stool samples come through our laboratory. One recent clinical case using our in-house Full Gastrointestinal PCR Panel, presented unprecedented results.
Patient overview:
- 51-year-old patient
- Travelled to and from Pakistan for a trekking trip
- The patient presented with a history of severe diarrhoea
- Symptoms recorded: erratic bowel movement and weight loss.
Test results:
The PCR result came back quicky as positive for four pathogens:
- Cyclospora cayetanensis,
- Enteroaggregative E. coli (EAEC),
- Enteroinvasive E. coli (EIEC)/Shigella,
- and Enteropathogenic E. coli (EPEC)
This is highly unusual and it is little wonder why our patient was feeling so unwell with severe symptoms.
Our Biomedical Scientist, Jenny Reyes commented; “This is my first time in all of my time as a Biomedical Scientist to encounter such a result with four pathogens presenting all at once.”
Without our GI PCR test, this patient may have undergone many tests to identify the cause and may not have identified that the symptoms were the result of four simultaneous pathogens causing a mixed infection.
The advantage of a panel PCR test is its ability to identify the exact cause, enabling targeted treatment.
In this case, the clinician overseeing this patient’s care was able to tailor treatment to address all four identified pathogens simultaneously with precision.
Without this technology, diagnosing a mixed infection could have taken significantly longer, requiring multiple different tests to pinpoint each cause.
This would have increased the risk that only one pathogen would have been identified, leaving the symptoms caused by the others untreated even after addressing the diagnosed cause.
We encourage all patients with unexplainable gastrointestinal symptoms to consider the GI PCR Panel. It really does offer faster, more targeted care and can identify mixed infection with ease!
More information on our GI Panel:
Our Gastrointestinal Panel Test delivers accurate and reliable results quickly, often within a matter of hours.
It is capable of detecting any of the 23 commonest pathogens that cause diarrhoea – such as E. coli, campylobacter, norovirus salmonella, shigella and giardia, from a single stool sample – all that’s needed is a simple swab.
This supports our rapid diagnostic process, clinical management and educated treatment decisions which improve overall patient outcomes.
Learn more and book today
Dengue has been declared an epidemic in the state of Karnataka in India.
Dengue fever is an unpleasant viral infection spread by the bites from infected Aedes mosquitoes. Unlike the mosquitoes that transmit malaria and are active at dusk, Aedes mosquitoes are most active during daylight hours, making dengue prevention more challenging.
As of this week, Karnataka has reported 25,589 cases and 12 deaths so far, with a staggering 15,000 new cases in the last 45 days alone—the highest in a decade.
Bengaluru, one of the hardest-hit cities, has recorded over 11,500 cases, driven by the rainy season that has created ideal mosquito breeding conditions.
To combat this, the government is enforcing strict measures, including penalties for property owners who allow mosquito breeding. However, personal protection remains critical, especially for those planning to travel to India.
At Fleet Street Clinic, we offer Qdenga®, the newest dengue vaccine. As a live vaccine, it’s not suitable for everyone, so we recommend booking a consultation with one of our specialist travel nurses to determine if it’s right for you.
Safety Tips:
In addition to vaccination, follow these safety tips:
- Cover up, wear long sleeves and trousers when there are mosquitoes around.
- Use mosquito repellent creams, coils, and sprays.
- Use a mosquito net at night
- If you experience symptoms like fever, muscle aches, nausea, or vomiting, seek medical attention.
If you’re planning to travel, ensuring your vaccinations are up-to-date is essential for your safety. To determine if the Qdenga® vaccine is right for you, we recommend booking an online consultation with one of our expert travel nurses.
The Qdenga® vaccine requires two doses, with each dose priced at £148. Our specialists will provide personalised advice and help you navigate your vaccination needs.
Click to book your appointment.
For more information on:
Dengue Epidemic in Karnataka, India
Karnataka declares Dengue an Epidemic
Holidays are a time to relax, unwind and have fun!
However, this excitement can lead to us making decisions we may not usually make when we are at home. If you have unprotected sex whilst abroad whether it is oral, vaginal or anal you are at risk of catching sexually transmitted infections.
You could be at risk of catching these common STIs: HIV, chlamydia, HPV, herpes, syphilis and gonorrhoea.
What can you do to prevent an STI?
Abstaining from sex is the most reliable way to avoid infection. However, if you wish to be sexually active follow some of the tips below:
- Use a condom from start to finish every time during sex including oral, vaginal and anal.
- Get vaccinated to protect against diseases such as Hepatitis B and HPV.
- Do not assume that your partner is STI-free. Talk openly and discuss your sexual health histories.
- Taking drugs and/or alcohol can lead to bad decisions. Be cautious when having sex whilst inebriated as you are more likely to take risks. These include not wearing a condom or having sex with someone you usually would not.
What are the symptoms of an STI?
Symptoms are different depending on the infection. Some diseases also do not cause any symptoms which makes them very hard to spot. If symptoms do occur, they could be some of the following:
- Pain when you urinate or have sex
- Discharge from the vagina, penis, or anus
- Unexplained rash, sore, or ulcer on your skin, genitals, or throat
- Jaundice (yellow colour of the skin and eyes)
What do you do if you think you have an STI?
Having an open and honest conversation, discussing your sexual health with your doctor is a good start to help guide you towards any tests or medication that you may need.
Long-term problems can be prevented by testing for STIs early and also prevent the spreading to other partners.
If you are worried that you may have an STI you should:
- Not have sex with anyone. This will reduce the risk of spreading the disease to anyone else.
- See a doctor or nurse as soon as possible.
- Discuss your sexual history and international travel with the doctor or nurse as some diseases are more common in some countries.
- If you have a positive result notify your recent partners. They may also be infected and unaware.
Fleet Street Clinic offers a discreet and trusted sexual health service including confidential sexual health advice, instant testing, and comprehensive STI screening.
You can book a sexual health appointment online.
On 14th August 2024, the World Health Organization declared outbreaks of mpox in Africa to be a Public Health Emergency of International Concern.
What is mpox?
Mpox is a viral infection that was previously known as “monkeypox”.
It shares some similarities with smallpox, to the extent that smallpox vaccine may be cross-protective; however, the illness is much less severe. (Waning population immunity to smallpox, since vaccination programmes ended in 1980, is one possible reason for the increased tendency to outbreaks now.)
So far, there have been 14,000 cases reported in Africa, with 524 deaths. Sweden has just reported the first case of clade I mpox outside Africa in the current outbreak (see below).
Previously confined to central Africa, recent outbreaks have ultimately spread globally, which is why the WHO has now decided to urge a concerted global response.
How is it spread?
The infection is spread mainly by close direct / intimate contact with body fluids and secretions, and by sexual exposure.
It can also be spread by contact with animals, or their droppings, or by eating under-cooked contaminated meat – so-called “bush meat”. The animal reservoir of infection is mainly among rodents and non-human primates.
The illness
Infection may be symptomless, but in most cases, symptoms appear 7 to 14 days following exposure.
Mpox is characterised by blistering skin lesions that are often extremely painful (and highly infective to other people), occurring particularly on the skin, genitals and face. They can be sparse, or even single blisters.
Other symptoms include fever, chills, headache, muscle aches, fatigue and swollen lymph glands.
The blisters may appear first on the face, spreading to other parts of the body; or alternatively in the genital area if the infection was acquired by sexual contact. Extensive lesions around the mouth may make eating and drinking painful or impossible, requiring intravenous treatment.
The illness is considerably more serious in people with HIV infection or reduced immunity. Severity of infection is also linked to the degree of exposure.
Mpox strains
There are two strains (called clades – Clade I and Clade II) that differ in severity and ease of spread.
Clade II tends to be more severe (up to 1,000 times more virulent than clade II) and occurs in Central Africa, Clade II occurs mainly in West Africa and may sometimes be more easily transmissible. Mutations into sub-strains is also occurring, which makes testing more complicated, especially in countries where resources are poor.
Where are cases occurring?
It is important to bear in mind that official statistics generally underestimate true numbers of cases, since not everyone with symptoms seeks medical attention, and not all cases undergo full testing.
Laboratory-confirmed cases have been reported in:
- Burundi: over 100 cases (Clade Ib) throughout the country
- Central African Republic: 28 cases (Clade I) throughout the country
- Côte d’Ivoire: 6 cases (Clade II) in Abidjan and Bas-Sassandra districts
- Democratic Republic of the Congo: > 14,000 cases (Clades Ia and Ib) throughout the country, mainly in Équateur, Sankuru, South Kivu, and Sud Ubangi provinces
- Kenya: 1 case (Clade Ib) in Taita-Taveta County
- Republic of the Congo: > 120 cases (Clade I) throughout most of the country, mainly in Cuvette, Kouilou, Likouala, and Point-Noire departments
- Rwanda: 4 cases (Clade Ib); no specified locations
- South Africa: 24 cases (Clade IIb) in Gauteng (12 cases and 2 deaths), KwaZulu-Natal (11 cases and 1 death), and Western Cape (1 case) provinces
- Uganda: 2 cases (Clade Ib) in Kasese District; no secondary transmission has been reported
A previous outbreak in 2022 resulted in spread to over 40 countries – with over 30,000 cases in the USA, for example, mainly in the MSM community.
Are visitors at risk?
Although current news reports of mpox cases are alarming and intended to generate a global public health response, so as to raise awareness and help bring outbreaks under control, most tourists and travellers to Africa are not at risk.
Travel to Africa for the usual tourist activities (e.g. safari, outdoor activities, beach) should be unaffected by the outbreak.
Older travellers who have previously been vaccinated against smallpox may still have some additional cross-protection against mpox.
- Risk arises from close contact (especially sexual contact) with infected people.
- Those at highest risk are men who have sex with men (MSM).
- High-risk behaviour is easily avoided, and safe-sex precautions reduce the risk of infection.
- Risk also arises from close physical contact with infected animals, or by eating under-cooked bush meat – which should be avoided. (Thorough cooking kills the virus.)
- Healthcare workers may be at risk if caring for people who are ill with mpox
- Journalists and news media personnel should avoid physical contact, keep their distance and observe the usual hygiene precautions when reporting on the evolving mpox outbreak situation
Mpox vaccines and treatment
- In the UK, vaccination is available for MSM and healthcare workers via the NHS.
- Current vaccines protect against all strains.
- Vaccination within 14 days of possible exposure also appears to confer protection (post-exposure protection).
- Several antiviral drugs can provide benefit in the most severe cases.
More information:
Oropouche Virus Disease: A growing concern in Central and South America.
As of mid-2024, Central and South America are experiencing a significant outbreak of Oropouche virus disease, impacting countries such as Brazil, Bolivia, Colombia, Peru, and Cuba.
The Oropouche virus is primarily transmitted through the bites of infected midges (Culicoides paraensis) and mosquitoes. The virus is mainly spread in tropical and subtropical regions where these vectors are prevalent.
Symptoms of Oropouche virus disease include:
- sudden-onset fever,
- severe headaches,
- muscle and joint pain,
- rash,
- eye pain,
- nausea,
- and dizziness.
While most cases are mild and self-limiting, lasting 3 to 7 days, some individuals may experience more severe symptoms like meningitis and encephalitis.
There is no specific antiviral treatment or vaccine for the disease, so care focuses on symptom relief, such as rest, hydration, and pain management.
How to protect yourself from Oropouche virus
Preventing Oropouche virus disease involves reducing exposure to vector bites. Unlike mosquitoes, the main vector (midges) lacks a proboscis, and so is unable to bite through clothing.
Covering up, and wearing long-sleeved clothing, is therefore a keyway of preventing infective bites.
Other key measures include using plenty of insect repellent, impregnating clothing with Permethrin insecticide, using bed nets, and staying indoors during peak biting times.
Eliminating standing water where vectors breed is an important public health measure.
Prevention is key!
With no vaccine available, prevention remains the best defence against Oropouche virus disease.
Personal protective measures against insect bites also help protect against dengue, yellow fever, Zika, chikungunya, malaria, and a wide range of other tropical insect-borne infections, and should be followed carefully by travellers to tropical countries.
Cases found in Europe
Spain, Italy and Germany reported infections in numerous patients who had recently travelled to Cuba and Brazil.
The European Centre for Disease Prevention and Control (ECDC) warned of a moderate threat to travellers visiting Brazil, Bolivia, Colombia, Peru and Cuba, where Oropouche virus (Orov) is currently spreading.
If you’ve recently travelled to a known outbreak area and are experiencing any of the symptoms mentioned above, it is important to mention this to your doctor. This will help them rule out an Oropouche virus infection.
Worried about your upcoming travel plans?
Schedule a travel consultation with one of our specialist travel nurses.
They will guide you through potential health risks and recommend the necessary preventive measures and vaccinations to ensure your safety while travelling.
For more information on:
If caught and symptoms develop, rabies is almost invariably fatal.
Rabies is spread through the saliva of an infected animal and is present in over 150 countries worldwide. Up to 100 children die each day from rabies, and more than 55,000 people a year are killed from the disease, mainly in Asia and Africa.
If bitten or scratched by an infected animal you need to act quickly. Your pre-exposure vaccines simplify medical care in case of a potential rabies exposure, reducing the number of post-exposure vaccine doses needed and providing more time to seek medical care because your antibodies will start to respond. This is crucial when traveling to remote areas with limited access to medical facilities.
If you haven’t had pre-travel vaccinations, the treatment is much more complicated; it is also expensive and can be hard to access in lower income countries. If treatment is given correctly and promptly after exposure, it is 100% preventable.
It is extremely important that if you are travelling somewhere with a known risks of rabies it only seems sensible to protect yourself against it. Rabies is a vaccine-preventable disease, so make sure you get vaccinated before you travel.
For more information on rabies and travel health, visit our rabies page here.
The Fleet Street Clinic is passionate about travel. We have provided rabies vaccinations for over 20 years. Our team of expert travel medical professionals provide advice and detailed consultations to ensure you have a healthy trip.
You can book a travel consultation or rabies vaccination appointment online.
ESSENTIAL CHICKENPOX VACCINE FACTS:
- The chickenpox vaccine is not currently given by the NHS, but is part of the childhood vaccination schedule in other countries
- Chickenpox is a highly contagious infection caused by the varicella zoster virus
- In the UK, it mostly affects children
- It can be itchy and uncomfortable, can leave scars, and can sometimes cause severe disease – adults may suffer more serious symptoms, including pneumonia
- Chickenpox is spread by inhaling droplets coughed up by people infected with the virus
- People with chickenpox become contagious about 2 days before the appearance of the rash, which can make it difficult to avoid infection
- The chickenpox vaccine (varicella vaccine) can be administered from the age of twelve months onwards
- Two doses of vaccine are needed, with a 4 week gap between doses
- If your child is receiving the MMR vaccination or a Yellow Fever vaccine, the varicella vaccination must either be given on the same day, or 4 weeks later
HOW TO BOOK A VACCINATION APPOINTMENT
Fleet Street Clinic is dedicated to maintaining a good supply of the chickenpox vaccine.
Our private chickenpox vaccine service is undertaken by doctors and nurses with long experience of vaccinating children. Our family friendly clinic is sympathetic to parents’ needs and concerns, and we welcome any vaccine-related queries. We operate a Saturday vaccination clinic once a month, the next will be held on Saturday April 8th.
To book your chickenpox vaccination for yourself or your child, you can book online now.
The summer holidays will fly by and be over as quickly as they began, much to your relief, but probably the disappointment of your kids! Unfortunately, alongside the general back to school chaos, September also brings with it the start of the flu season.
Flu season not only means that people have to take time off of work due to being ill themselves, but parents often have to take time off work to look after their children who have the flu, because schools are rife with superspreaders. It seems that the best solution to the frustrating effects of the flu on school and parenting life is to nip it in the bud early enough in the season for immunity to make a significant difference.
This is where the flu vaccine comes in.
The flu vaccine comes in two forms, the traditional syringe-administered jab, and a nasal spray vaccine. While the nasal spray vaccine may be the preferred administration tactic for parents of children who don’t like needles, supply issues have resulted in limited availability, and it may still be worth considering the alternative.
When might the jab be preferable?
The nasal spray vaccine is protective and an excellent choice, but is not suitable for everyone. It is a live vaccine, and so cannot be administered to children who are immunocompromised or who live with anyone who may be immunocompromised. It is also unsuitable for anyone with bad asthma, since it may trigger an attack. The injected vaccine is not a live vaccine and is an obvious solution for a lot of people.
The nasal spray vaccine contains traces of gelatine and egg, and so may be unsuitable for vegetarians, vegans, Muslims or those with a severe egg allergy. There is a cell-culture based injectable vaccine that is egg-free, which may be a more acceptable alternative.
The nasal spray vaccine can only be given from age two onwards. However, if there is a special reason for needing to vaccinate your child at a younger age than this, the standard injectable vaccine can be given from the age of 6 months. (The best way to protect babies younger than this is by vaccinating mums during pregnancy.)
For the past three winters, the nasal spray vaccine has been in limited supply. It has not been available privately but only through the NHS, and supply issues have resulted in extended delays. By contrast, injected vaccines have been available reliably from September onwards.
A well-timed dose of the injected vaccine, early in the season, may be a better option than the uncertainty of a delayed dose.
At the Fleet Street Clinic, we have been happy to offer the nasal spray vaccine previously but having been unable to obtain reliable supplies for the past three years, we will not be offering it this season.
If you decide to book the injected flu vaccine for your child this winter, you can rely on guaranteed supplies as well as our expertise in vaccinating babies and children of all ages.
__________________________
24/25 Winter Flu Vaccination Pricing:
Cell-Based Quadrivalent Flu Jab – £42 – Suitable from 2 years
Standard Quadrivalent Flu Jab – £20 (while stocks last) – Suitable from 6 months old
Book Your Flu Jab Online Today
Recent media reports have raised awareness of the effects of Meningitis B and the importance of the meningitis vaccine (if your child is aged under 12 months, the vaccine still readily available via your NHS doctor). Less well-known is the fact that there are different strains of Meningitis, with different vaccines protecting against them.
Strains and Meningitis Vaccines:
- Meningitis B: the protective single-strain meningitis B vaccine is Bexsero
- Meningitis A C W Y: the 4-strain vaccines Menquadfi and Nimenrix offer protection.
Meningococcal Meningitis and its Symptoms
Meningococcal meningitis is a bacterial infection that causes inflammation of the protective membranes surrounding the brain and spinal cord. It can affect people of any age, but those most commonly affected are children under 5, and teenagers and young adults heading off to university.
Initial symptoms may be similar to flu, progressing to:
- A high temperature/fever, with cold hands and feet
- Vomiting
- Refusal to eat
- Drowsiness
- Floppy and unresponsive
- Rapid breathing
- Neck stiffness
- Bright light sensitivity
- Pale, blotchy skin, and a red rash that doesn’t fade when a glass is rolled over it
- Convulsions or seizures
Further information: https://www.meningitisnow.org/meningitis-explained/
The specialists at the Fleet Street Clinic recommend getting your children vaccinated not just against Meningitis B, but against Meningitis A,C,W & Y strains as well (the vaccine is currently available and in stock).
Meningitis B Vaccines Availability
We currently have a good supply of Meningitis B vaccine, available on a first come, first served basis. You can book a Meningitis B vaccination appointment online.
Respiratory Syncytial Virus (RSV) is a common and highly contagious virus that primarily affects the respiratory tract, causing significant illness, particularly in infants.
It is present year-round but peaks during the winter months, and spreads through droplets from coughs and sneezes or via contact with contaminated surfaces. RSV is a virus, so antibiotics are not an effective treatment.
Each year, RSV poses a substantial health risk to infants and older adults worldwide.
In the UK, RSV accounts for approximately 33,500 hospitalisations annually in children aged 5 and under, resulting in 20 to 30 deaths per year. 75-80% of hospitalisations due to RSV happened during the first 6 months of life.
Is there a suitable RSV vaccine for pregnant woman?
Abrysvo is a recombinant vaccine for the prevention of severe lower respiratory tract disease caused by RSV in infants up to six months old. It is the only maternal RSV immunisation given to the pregnant woman between 28 – 36 weeks of pregnancy to help protect newborns. It can also be used for older adults over the age of 60 years, in preventing RSV that can lead to breathing difficulties and pneumonia.
Maternal vaccination involves administering vaccines to pregnant women to protect their newborns through the transfer of antibodies. This approach has been effectively used for diseases like whooping cough.
Vaccinating pregnant women against RSV provides passive immunity to their babies, safeguarding them against RSV until they can receive their own vaccines. The RSV vaccine should ideally be given at least 2 weeks apart from the whooping cough vaccine.
In the UK, the Joint Committee on Vaccination and Immunisation (JCVI) has assessed the impact of RSV and now recommends vaccination to protect vulnerable groups, including infants and older adults with the aim of reducing the incidence of RSV-related illnesses among infants, ultimately reducing RSV-related morbidity.
At Fleet Street Clinic, we can offer private RSV vaccination to protect you and your baby, ahead of the NHS roll out.
Abrysvo is an inactivated vaccine and only requires a single dose for protection.
Price: £296
Please contact our reception team to book by phone, +44 20 7353 5678 or by emailing info@fleetstreetclinic.com
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Every year, Brits take more than 70 million trips abroad. Most notably for holidays, business trips and to visit family and friends. Whilst the majority of people have a safe trip, some people do experience illness or have an accident. In most cases, minor accidents and illnesses don’t require a visit to a medical centre or hospitalisation and can be self-treated with the help of a medical kit.
Where you are travelling to and the activities you plan to do there will dictate what type of medical kit(s) you would need.
Essential First Aid Kit £27
If you are planning to travel outside of a major city, you’re best to travel with an Essential First Aid Kit. It’s very easy to get scratched, twist an ankle or develop a blister. Particularly if you’re sight-seeing, hiking or even just taking a trip to the beach. Having a few essential supplies handy will reduce the need for a trip to the local chemist. Inside this kit, you will find items aimed at treating minor cuts, grazes, blisters, cleaning wounds, minor burns and sprains.
Worldwide Travellers’ Diarrhoea Kit £29.95
When you travel to a developing country, you have a high likelihood of catching a stomach bug. Also known as traveller’s diarrhoea. This is not always brought on by unsafe water and can be due to a change in diet or the high levels of impurities in the local water that you’re not used to. However, if the cause is a microorganism such as bacteria, parasite or virus, your symptoms may be much more severe and lead to complications. Travelling with a Worldwide Gastro Kit covers all eventualities. Including preventative items, plus medications for common symptoms such as nausea, vomiting, dehydration and travellers diarrhoea.
Sterile Needle Kit £9.50
The adventure traveller is likely to travel to remote areas where medical supplies are not sterilised to a safe standard or medical care in a hospital setting is not available at all. In these scenarios, it is safest to travel with a Sterile Needle Kit. This kit is to be provided to a medical professional to be used for medical emergencies such as a blood transfusion, fluid replacement, general vaccinations or blood tests. This kit is to reduce the spread of diseases such as HIV & Hep B.
Female Health Kit £29.95
There are many female-specific health concerns that may occur whilst travelling. Unfortunately, urinary tract infections (UTI’s) and thrush (yeast infections) are common among female travellers. Therefore travelling with a Female Health Kit is highly recommended.
Travelling with a fit-for-purpose medical kit is not glamorous. However, you’ll be glad you have it if you suffer any mishaps. Saving you time, money and stress involved in finding a local chemist, medical centre or hospital quickly when you are abroad. And if you don’t, then at worst you’ve lost out on a tiny amount of suitcase space.
Before International Travel you should consider a pre-travel consultation with a specialist travel nurse to discuss the health risks at your destination. You can book a travel appointment online or email us for more information at info@fleetstreetclinic.com.
SUMMER TREKKING
Do you enjoy the great outdoors and active holidays? If so, you may be contemplating a trekking adventure. Top summer trekking destinations include Cotopaxi, Ecuador, the Atlas Mountain Range in Morocco, The Ladakh Ranges in India and Mont Blanc in the French Alps.
Fleet Street Clinic offers travel tips for trekkers from Anna Chapman, one of our specialist travel nurses, to help prepare for your holiday and make the most of your adventure.
-
Ensure that you are up to date with vaccinations. It comes as a surprise to most people that vaccination should be considered before hiking in northern Europe. Tick borne Encephalitis is a serious viral infection that causes swelling of the brain. As the name suggests, it is spread by the bite of an infected tick, and it is endemic throughout northern Europe, Russia and China. If you’re heading further afield, to South America or Africa, you may need Yellow Fever vaccination for your own protection, or for border control.
- The most common illness amongst travellers is upset stomachs. Pack hand sanitiser to use when soap and water for hand washing is unavailable. Take water purification tablets if you have not got access to safe water. Medicines such as rehydration salts and anti-motility medicines can be helpful if you do become unwell.
- Most trekking routes are at high altitudes. Understand the effects of altitude sickness. Take time to acclimatise to altitudes and consider taking medication such as Diamox to reduce the severity of acute altitude sickness.
- Look after your feet. Invest in good trekking boots, socks and wear them in before you go. Keep your feet dry when trekking by changing your socks and using foot powder. Zinc oxide tape or Compeed dressings can be helpful if you do get blisters.
- Pack suitable clothing. Trekking in mountain ranges usually involves variable temperatures: Warm days, thin air, strong sunshine and cool nights. Pack breathable clothing, a waterproof jacket and warm base layers. Sun protection is essential, especially in high altitude ranges, so apply the “Slip, Slop, Slap” rule. Slip on a shirt, slop on some sunscreen and slap on a hat.
FLEET STREET TRAVEL CLINIC
Travelling with children can be an enlightening and wonderful experience for the family – creating memories and opening their minds to other cultures and ways of life. But on the flip side it also can be quite daunting, especially if this is your first time travelling with children. The best way to establish a safe travel experience abroad is to take early precautions.
Before Your Travels
When it comes to travelling with children, careful planning and preparation should be considered. It is highly advised to have a travel consultation well in advance of your travels. The travel nurse will make you aware of any travel risks and take into consideration your child’s current wellbeing. Depending on where you are travelling, your child may require certain vaccinations.
These preventative measures will safeguard your child from any diseases or illness.
Your may be advised the following vaccinations:
- Rabies
- Yellow Fever
– Some countries require this as a condition of entry and will ask for proof of vaccination when you arrive into the country. - Hepatitis A
- Typhoid
- Tick-borne Encephalitis
- Japanese Encephalitis
- Hepatitis B
- Meningitis ACWY
- Cholera
All vaccinations require a duration of time following vaccination to reach full protection, usually 10 – 14 days, so factor this time in before your travels. In addition, some vaccinations require a multi-course dose before they are considered effective, such as rabies which requires 3 vaccinations to be considered a complete course. Book a travel consultation early to ensure you have enough time before you travel.
In addition to travel vaccinations it is worth discussing any upcoming childhood vaccinations that could be beneficial to have at the same time so your child is protected against any other common diseases that aren’t necessarily associated with just travel.
If you intend to go to countries with a high malaria risk it is important to discuss antimalarial protection during your travel consultation. Malaria can be fatal and there is a higher risk for children. Antimalarials (malaria tablets) are generally taken for a duration before, during and after your trip and need to be purchased in advance of your travels. There are a number of different types and are suitable for different people so it is important to discuss your options with a travel health expert. The tablets work by ensuring the malaria parasite doesn’t reach unmanageable numbers, keeping you healthy whilst you travel.
Travelling abroad can be exhausting, especially for young children. Jet Lag is known to cause temporary sleep disturbance, which can have an impact on your mental health and other bodily functions. To prepare ahead, The Jet Lag Calculator can tell you how long it will take the body to adjust to your new time zone when you travel – and to adjust back again when you come home.
To undergo a Pre-Travel Consultation, book online or for more information on Travel Health Services.
During Your Travels
Travelling can sometimes result in unexpected situations. For the protection of your child/ren and your family in general, always carry a First Aid Kit. This will reduce your need to seek medical aid for minor accidents or journeys to a chemist, especially if local towns are at a further distance.
When travelling to warmer climates, sun safety is crucial as young children are more vulnerable to sunburn from outdoor activities. To protect the skin apply sunscreen of at least SPF 30, with broad spectrum UVA and UVB protection throughout the day. In addition, hot weather can also pose a risk of dehydration and heat stroke. Ensure you and your child are hydrated throughout the day by drinking water from a safe source. This can be bottled water, boiled water, or water that has been filtered.
To further avoid traveller’s diarrhoea:
- Wash your hands regularly, especially before eating
- Carry an alcohol-based sanitiser
- Keep children from crawling or sitting on the ground
- Avoid swimming in contaminated water
- Don’t swallow any shower or pool water
- Eat raw fruits and vegetables only if washed in clean water or peeled
- Stick to foods that are well cooked and served hot
- Stick to canned or bottled beverages
- Avoid food that has been sitting on a buffet to avoid contamination
We have launched a new, free online consultation for Travellers’ Diarrhoea – by answering a few simple medical questions about yourself, we can check if antibiotics are recommended for your trip. You can pay online and we’ll dispatch them directly to you if you are suitable.
Alternatively, you can have a more comprehensive travel consultation in-clinic with one of our experienced travel nurses.
For more information on the prevention and treatment of Travellers’ Diarrhoea.
The feeling of discomfort from bug bites can truly be a nightmare whilst travelling. Insect bites such as mosquitoes, ticks, biting fleas and kissing bugs can cause pain, irritation and even spread diseases. However, they can be avoided through protective clothing. Our Ultimate Bug Kit has everything you need from repellents to aftercare. Alternatively, you could purchase individual items and create your own kit.
After Your Travels
Travelling can expose your child to certain diseases. If your child falls unexpectedly ill – contact your doctor or emergency services right away. A high temperature/ fever could mean an infection. For most people, travellers’ diarrhoea usually clears up within a few days. However, if your stomach bug has been ongoing for weeks after returning home, then you will need to do testing to investigate the root cause. Viruses, bacteria or parasites all cause similar symptoms but require an entirely different treatment approach. Our Gastrointestinal (GI) Panel PCR test looks for any microbes that are causing your symptoms and can quickly identify the exact cause of your Travellers’ Diarrhoea. Results can be provided in as little as 1-hour, so that accurate and effective treatment can begin straight away.
I picked up Covid early in the pandemic and put my newly acquired immunity to good use by joining the Covid medical team at my local hospital for the weeks that followed. There was a side-effect however: a sense of invincibility that has perhaps made me take less care to protect myself from respiratory viruses ever since.
My luck ran out recently while looking after a group of patients with upper respiratory infections. Not all respiratory viruses are equal: we may call them “colds”, but some varieties are considerably more unpleasant than others.
Using PCR, we can now tell the difference between 22 different bugs with pinpoint accuracy, in about an hour. Mine turned out to be parainfluenza type 1 (there are four serotypes, who knew?) – a nasty virus, more common in the USA and among children.
My bout ranked alongside my experience with Covid: the symptoms lasted over three weeks and included a secondary lower respiratory infection requiring antibiotics to clear.
There’s no vaccine as yet against parainfluenza, but there are vaccines against other important respiratory infections – pneumococcal pneumonia, RSV, Covid-19, a newly-recommended adult top-up against whooping cough, and of course flu.
I shall be having all of these vaccines this winter and will take much greater care to protect myself when those around me have “colds”.
Women between the ages of 25 and 64 are invited for regular cervical screenings where a healthcare professional looks at the health of the cervix to detect any cell changes or abnormalities. However, in 2022-2023, the number of women who attended their cervical screen fell. Nearly a third of the women invited to do their cervical screen didn’t attend their appointments, this is around 4.6 million women, a deeply concerning number, as over 3000 women are diagnosed with cervical cancer each year and 99.8% of those cases are preventable. Prevention is better than curing, and the earlier you are aware of any cell changes, the easier it is to treat.
Why do some women not attend their cervical screenings?
One of our general practitioners, Dr Belinda Griffiths, has found that in her experience women don’t attend their cervical screenings for a number of reasons including: difficulties with taking time off work for a GP appointment, fear of embarrassment, and fear of the process being uncomfortable or painful.
However, to combat these concerns, the NHS has launched at-home HPV kits. Dr Griffiths explains how they work – “The HPV test is highly sensitive so it separates out those who are HPV-positive and HPV-negative. Those who are HPV-negative will be considered ‘low risk’ for cervical cancer and will be asked to do a future test. Those who are HPV-positive will be deemed ‘high risk’ and be asked to attend for follow-up with a clinician whereby they will conduct a cervical screening to check the health of their cervix and investigate if any abnormal cells are present.”
These new tests are the same process as at-home STI tests whereby a simple swab collects the sample from the vagina. Having the option of this sort of test at home removes the fear some women may have surrounding the slightly more intrusive cervical screen.
What is HPV?
HPV (human papillomavirus) is a common virus passed on via skin-to-skin contact, usually through genital contact. There are many types of HPV, most of which are harmless, don’t usually cause any symptoms and the infection will go away on its own. However, others are deemed ‘high risk’ as they can persist and cause cell changes which can lead to cancer. It is thought that these ‘high risk’ HPV strains are responsible for around 80% of cervical cancer cases, making the detection of HPV all the more important.
How can you prevent HPV?
You can be protected from certain HPV strains through vaccination. There are two HPV vaccines currently available in the UK: Gardasil which protects against 4 strains of HPV used in the NHS and the vaccine used here at the Fleet Street Clinic, Gardasil-9, which protects against 9 of the high-risk HPV strains.
When can you be vaccinated against HPV?
The NHS now routinely offers the Gardasil vaccine to girls and boys around age 12/13, before the age people generally become sexually active. However, the vaccination programme only came into full force in 2019, meaning many people are currently unvaccinated. It should be pointed out that adults can get vaccinated at any age and even if you have already been exposed to HPV, the vaccine can still offer protection against other strains to which you have not yet been exposed.
It is a particularly good idea for people to get vaccinated before they attend university or before they go travelling on a ‘gap year’, as these are typically times where young people are more sexually active and therefore more likely to be exposed to HPV.
It is important to note that getting the HPV vaccination most certainly doesn’t mean missing or not participating in HPV tests or cervical screenings. A combination of these preventative measures gives you the highest possible chance of preventing cervical cancer.
Book your Cervical Screen or HPV vaccine online today.
As the threat from the disease grows, here is everything the modern traveller needs to know about malaria.
What is malaria?
Malaria is an infection caused by a tiny, blood-borne parasite, transmitted by the bites of infected female Anopheles mosquitoes. Symptoms can often be delayed until sometime after exposure (a minimum of seven days but often four weeks or much longer), meaning the connection with travel may be forgotten, delaying diagnosis.
Returning from a tropical holiday should come with a suntan and sense of relaxation – not a tropical disease. However, the number of British travellers catching malaria abroad is rising, and scientists are warning it could get worse.
The UK Health Security Agency (UKHSA) has just published its latest data on malaria in travellers returning to the UK, and the numbers are troubling. Over 2,000 cases were reported in 2023, the highest total in over two decades. Globally, the number of cases of malaria has risen by 16 million, compared with pre-pandemic levels.
No less worrying is the potential impact of climate change. Warmer temperatures can extend malaria transmission season, as well as extend the disease’s geographical range to higher altitudes and cooler places where transmission was previously uncommon. Flooding and extreme weather events create perfect conditions for mosquitoes to thrive, resulting in outbreaks of the disease.
In tropical countries where malaria is widely prevalent, the disease takes a huge toll. In 2022, there were 249 million cases, 94 per cent of which were in Africa. These led to at least 608,000 deaths, mostly in children.
But research recently presented at the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Global Congress in Spain suggested that if the world’s carbon emissions and population growth remain on the current trajectory, the populations at risk of malaria and other mosquito-borne diseases could increase by an additional 4.7 billion people by 2100, relative to 1970-1999.
Diagnosing malaria depends on knowing that a person has been in a destination with a risk of the disease, since early symptoms can be non-specific, and malaria has a remarkable ability to be mistaken for other conditions.
The most common symptoms of malaria:
- Fever, usually above 38C and often intermittent
- Fatigue
- Aching muscles and joints
- Headache
- Chills (often with sweating and shivering)
- Abdominal pains and diarrhoea
- Sometimes jaundice (yellowing of the skin and whites of eyes)
Severe malaria can result in headache, fits and even death. Suspected malaria is therefore a medical emergency, and prompt treatment is effective and lifesaving.
The bottom line
If you develop a fever or become unwell on returning home from travelling abroad, seek medical advice promptly and make sure you doctor know that you have been away.
What areas have risks of malaria?
Risk areas for malaria include many parts of Africa, Asia, Central and South America, the Caribbean and Oceania – including holiday destinations in parts of Thailand, India and Peru.
How to prevent malaria on your travels
Medical prevention
Four to six weeks before your holiday begins, book a travel consultation regarding antimalarials – a travel nurse can advise on where and whether they are needed, and the options likely to suit you best.
Malarone and doxycycline are the two most-commonly prescribed medications, usually tablets or capsules taken once a day. They need to be commenced before travel, taken while you are away and continued on your return home.
For now, there are no suitable malaria vaccines for travellers. However, promisingly, two important vaccines have recently become available to combat malaria as part of public health campaigns in parts of Africa.
Avoiding insects
Bite prevention measures dramatically reduce the risk of disease, with insect repellents containing DEET, plug-in insect killers, mosquito bed nets and a wide range of other options. Our expert travel nurses can recommend suitable products during your travel consultation.
Other mosquito-borne diseases
Malaria is not the only disease on the rise due to climate change. Other mosquito-borne diseases include Dengue Fever (currently causing a large outbreak in South America), Japanese encephalitis, Chikungunya, Yellow Fever and Zika. The Zika outbreak in 2016 demonstrated how quickly mosquito-borne diseases can turn into an international health emergency. Climate change is expanding the range of mosquitoes capable of spreading them, and constant vigilance will be needed to combat them.
If you’re travelling to areas that are at risk for Malaria, book a travel consultation for a stress-free holiday.
Find more travel health information at fitfortravel.nhs.uk and travelhealthpro.org.uk.
Related services at Fleet Street Clinic
Specialist Travel Clinic
Antimalarials
Travel Vaccinations
Dengue Fever
Continued Reading about “Why malaria is on the rise – and how to protect yourself on holiday”
Read – Why malaria is on the rise – and how to protect yourself on holiday
Read – Britons catching Malaria at highest number in over 20 years
Read – Climate change drives deadly malaria surge as elimination efforts reach ‘crunch point’
Read – Vaccines are a glimmer of hope against malaria, but the battle has only just begun
Trusted London clinic now offers private Covid-19 vaccines.
As a trusted name in healthcare for the past three decades, Fleet St. Clinic are proud to announce the expansion of our services to include private Covid-19 vaccination for individuals and businesses alike. We offer the most up-to-date Pfizer Covid vaccines at a cost of £115 per dose.
Covid Vaccinations for Individuals
Until now, Covid vaccination has only been available through the NHS, which has rightly prioritised access those most likely to suffer complications. However, coronavirus infection remains a hazard for everyone, and many other people also wish to be protected. Protection can be especially important for people keen to avoid illness abroad, for people in key occupations, and for those in close contact with vulnerable friends and relatives.
Covid vaccination will now be available year-round for all those who would like to be protected, including those who have not been eligible for NHS care. Whether you need a booster vaccination or would like to consider having the Covid vaccine for the first time, we can help.
Book your private covid vaccination here.
Covid Vaccinations for Businesses
Fleet St. Clinic has provided large-scale flu vaccination initiatives for businesses across the United Kingdom since 1995. These programmes are now being expanded to include long-awaited vaccination against Covid-19. Many of our clients have been keen to protect those in business-critical roles as well as to protect employee health and wellbeing more generally.
Workplace vaccination programmes are offered as a straightforward and fully-managed service, enabling employees to access vaccinations they might otherwise find challenging to obtain. Introducing vaccination against Covid-19 reflects our longstanding commitment to keeping companies and their employees healthy.
Book your private covid vaccination workplace programme here.
Fleet St. Clinic Medical Director, Dr Richard Dawood commented:
“We are delighted to be one of the first medical practices in the UK to offer Covid-19 vaccinations outside the NHS. Now that Covid has transitioned from being a pandemic to an endemic disease, it is important that vaccination against Covid should become as “normal” and accessible as vaccination against other infectious diseases.
As a private, multi-disciplinary medical practice, the Fleet St. Clinic has specialised in vaccines for three decades, delivering hundreds of thousands of doses. Through the pandemic, most of our doctors and nurses volunteered to deliver Covid-19 vaccines in the NHS. We are especially pleased that being vaccinated against Covid-19 can now be a matter of choice for individuals and businesses alike, no longer restricted to those in the most vulnerable groups.”
Pre-Book Your Covid Vaccine
Covid vaccination will become available in March, but you can pre-book your own Covid vaccine or a Workplace vaccination programme, from today. Fill in our online form and we will be in touch with more information.
Pre-book your private covid vaccination programme here.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Full Respiratory Panel PCR Test
There has been a huge rise in measles cases already this year inciting a national campaign to ensure that children and adults are adequately vaccinated against measles.
Measles is a highly contagious virus that can cause serious illness. Complications of the disease include pneumonia and meningitis. In some cases, the virus can be fatal.
The MMR vaccine is a highly safe and effective vaccine that not only offers protection against measles but also against mumps and rubella, as a 3-in-1 vaccine.
In the UK, the uptake of the MMR vaccination has declined significantly, resulting in an increase in measles infection. It is estimated that 3.4 million children under the age of 16 years remain unprotected against the disease.
The UK is not alone with rising cases of measles. The World Health Organization has reported a 30-fold increase of measles in Europe. Over 30,000 measles cases were reported by 40 of the Region’s 53 Member States between January and October 2023. Compared to 941 cases reported in all of 2022.
The MMR vaccination forms part of the national childhood schedule where the vaccinations are given at one year of age and then at 3 years of age.
Two doses of the vaccination provide over 99% protection against illness.
ADVICE
Although measles is a highly contagious illness, it can be easily prevented with vaccination.
MMR VACCINATION:
For full protection, ensure your child has received their routine childhood immunisations of 2 doses of the MMR vaccine.
Children at high risk of measles exposure can receive an accelerated vaccine schedule of MMR if they are high risk for contracting the disease, where two doses are given one month apart.
Infants at high risk contracting the disease can receive the MMR from as early as 9 months of age.
In some cases, a catch-up vaccination may be recommended for individuals who have not received the vaccine at the recommended ages.
Additionally, in certain situations, infants may receive an early dose of MMR, such as during outbreaks or if they will be traveling to areas where there is an increased risk of exposure.
Travellers who are visiting countries reporting outbreaks of measles should ensure that their routine immunisations against MMR have been completed. A simple blood test can confirm immunity if in doubt.
HOW MANY VACCINES ARE NEEDED?
Two doses of the MMR vaccine will provide lifetime immunity.
In the UK, these are normally given to a child around their first birthday. The second is normally given at around the age of three. If there is a risk of an outbreak or an infant is at higher risk to contract the disease, vaccines are sometimes given as early as 9 months of age.
You can easily book an MMR vaccine appointment online.
SHOULD I BE WORRIED?
Adults are also encouraged to check their own and their children’s vaccination status. This is especially important for those who are considered vulnerable or those travelling to countries that have reported outbreaks of measles.
In the first instance, you should call your GP for confirmation of your vaccination history. If you didn’t have the MMR vaccine or your course is incomplete, you can book your MMR catch up vaccinations online.
Alternatively, if you are unable to find your records, a simple blood test will be able to confirm if you are immune or not. If you were born before 1970, it is assumed you will be immune through natural infection with the disease.
DO YOU HAVE ANY ADVICE FOR PARENTS?
Yes, we wrote a separate blog for parents who are worried about measles. We cover symptoms of measles, what to do if you suspect your child has measles, what to do if your child has been exposed to measles, amongst other important information.
The take home message being that the risk to you child dramatically reduces if they have had the full course of the MMR vaccine. If they are part-way through the course or have missing vaccinations, we encourage you to consider catch up vaccinations for full protection and peace of mind.
Read our full blog on what to do if you think your child has measles and when you should keep them off school.
CAN ADULTS RECEIVE THE VACCINE?
Yes, it is perfectly safe to have catch up vaccinations if they are required.
If you are unsure of your vaccination status, we would recommend a blood test to check your antibody level first. If we discover that you are not immune, you will require two vaccine doses, given a month apart.
WERE THERE ANY WARNING SIGNS OF AN OUTBREAK?
In July last year, the UK Health Security Agency (UKHSA) issued a warning that, unless vaccination rates improve, London is at risk of a major measles outbreak. Even after that, the vaccination rates did not improve.
It is predicted that in some areas of the capital, up to forty per cent of children are not protected from measles by the time they start school. Young adults between the ages of nineteen and twenty-five are also particularly vulnerable. Referred to as the ‘Wakefield cohorts’ by UKHSA, this generation were exposed to misinformation published in the early 2000s and as a result, many were left unvaccinated.
In a bid to mitigate risk, councils wrote to households across the capital explaining the possibility of isolation requirements; Children who are identified as close contacts of a measles case, and who do not have an up-to-date vaccination record, may be required to self-isolate for up to twenty-one days. The NHS are therefore urging parents to check their children’s’ vaccination status. Records of their vaccines should be kept at their GP practice, or in their red book.
Book your MMR vaccination appointment today.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
CONTINUED READING ABOUT THE UK HEALTH SECURITY AGENCY (UKHSA) “ISOLATION WARNING FOR LONDON CHILDREN WITHOUT MEASLES JAB”
Read: Isolation warning for London children without measles jab
CONTINUED READING ABOUT THE LATEST MEASLES STATISTICS AND GUIDELINES (UKHSA) “LATEST MEASLES STATISTICS PUBLISHED” & “NATIONAL MEASLES GUIDELINES”
Read: Latest Measles Statistics Published
Read: National Measles Guidelines
What to do if you think your child has measles and when to keep them off school.
Measles cases are increasing throughout England, particularly among children. This highly contagious infection can lead to severe complications for some individuals.
Since there is no specific medical treatment for measles, obtaining vaccination is crucial for the best defence against serious illness. The measles, mumps, and rubella (MMR) vaccine is part of routine childhood vaccinations, meaning most children are already immunised against measles.
If your child has received both doses of the vaccine, it is unlikely that they will contract the virus.
Here, we’ll provide everything you need to know about measles, from ensuring your child’s vaccination to knowing when to keep them away from school.
What are the symptoms of measles?
Measles usually starts with cold-like symptoms, followed by a rash a few days later. Some people may also get small spots in their mouth.
Symptoms of measles usually start to appear 7-14 days after you become infected, which include:
- Runny/blocked nose
- Sneezing
- High temperature
- Sore, red eyes that may be sensitive to light
- Sore throat
- White spots inside the mouth
What does a measles rash look like?
Measles usually begins as flat red spots that appear on the face at the hairline and spread downward to the neck, body, arms, legs, and feet. Small, raised bumps may also appear on top of the flat red spots. The spots may become joined together as they spread from the head to the rest of the body.
What should you do if you think your child has measles?
If you suspect that you or your child might have measles, it’s important to request an immediate GP appointment or seek assistance from NHS 111.
Before visiting the GP or any healthcare facility, make sure to call ahead for guidance.
In the event of a measles diagnosis for your child by a doctor, it is advisable for them to refrain from attending nursery or school for a minimum of 4 days from the onset of the rash. Additionally, they should steer clear of close interactions with infants and individuals who are pregnant or have compromised immune systems.
What is the best way to protect against measles?
The best protection against measles for children and adults is to get both doses of the MMR vaccine.
MMR vaccination is available at Fleet Street Clinic for children and adults who would like catch-up on doses. If you or your child haven’t been vaccinated yet, or have an unfinished course of vaccines, either book an appointment online or contact our reception team on +44 20 7353 5678 to book an appointment.
We can usually accommodate same day appointments.
Alternatively, children receive the vaccine at no cost on the NHS at 12 months and then a second dose at 3 years and 4 months. You may find the NHS vaccination service has a longer wait time that us.
If you prefer a version of the MMR vaccine without pork products, please get in touch, explaining your preference and we will do our best to accommodate. It’s important to note that we would be ordering this product specially for you, so there may be a longer wait time for delivery and prepayment will be required. Either call our reception team on +44 20 7353 5678 or email info@fleetstreetclinic.com
Cold-like symptoms can be an early sign of measles. Should you still send your child to school?
If your child has been vaccinated, it’s very unlikely that they have measles. Check if they have a high temperature or a fever, and if not, we’d advise it’s fine to send your child to school.
Keep an eye on their symptoms and adapt accordingly if they worsen.
When should you keep your child off school or nursery and how long for?
If your child has measles, they should stay off nursery or school for at least 4 days from when the rash first appears and avoid close contact with babies and anyone who is pregnant or has a weakened immune system.
The school will let you know if your child has been in contact with someone who has measles and advise what you need to do.
They may advise people who are more susceptible to contracting the virus, such as unvaccinated siblings to stay away from school for the incubation period to be on the safe side.
The incubation period is the length of time it can take to develop the illness after being in contact with someone with measles. For measles, the incubation period can be up to 21 days.
Anyone, child or adult, who has been vaccinated is unlikely to be considered susceptible.
If you’re not sure whether your child is due a vaccination or has missed a vaccination, you can check their Red Book or contact your registered GP practice for confirmation.
If your child has missed their first or second dose of the MMR vaccine, we’d advise you book an appointment for catch up vaccines. You can book an appointment online.
Should you keep your child off school if another pupil has been diagnosed with measles?
Most children will be protected against measles and there is no need to keep your child off school if they have had both their MMR vaccinations.
Your school will let you know if your child has been in contact with someone with confirmed measles and will advise what the next steps are.
Can I still get my child vaccinated even if they’re older?
Yes. The MMR vaccine is suitable for adults and children, therefore, anyone who has not had 2 doses of the MMR vaccine can book an appointment for catch up vaccinations.
It’s best to have vaccines on time, but you can still catch up on most vaccines if you miss them. Two doses of the vaccine are needed to ensure full protection.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Related Blogs:
Measles outbreak & isolation warning
UTIs can strike unexpectedly, casting a shadow over an otherwise fantastic holiday.
Whether you’re a seasoned traveller or embarking on your first adventure, the risk of urinary tract infections (UTIs) is real and more likely to occur during travel, especially in hot countries.
This blog compiles expert advice and practical tips to empower you to minimise the chances of developing a troublesome UTI during your travels.
1. Stay hydrated
One of the simplest yet most effective ways to prevent UTIs is to stay well-hydrated. Proper hydration helps flush bacteria out of your urinary system, reducing the likelihood of infection.
Aim to drink at least eight glasses of water a day, and avoid excessive consumption of caffeinated and alcoholic beverages, as they can contribute to dehydration.
Bring a reusable water bottle and make a habit of refilling it throughout the day, ensuring you have access to clean and safe drinking water wherever you are.
2. Don’t delay going to the toilet
It can be tempting to “hold it in” during long journeys, delayed or remote travel but putting off going to the bathroom can cause UTIs.
Holding your bladder for too long can contribute to the growth of bacteria in your urinary tract. Since urination flushes bad bacteria out of the bladder before they get a chance to multiply to dangerous levels, going to the toilet as soon as you can means less bacteria are left to sit in your bladder for longer than necessary, reducing your risk of a painful infection.
Remember, maintaining good personal hygiene is crucial in preventing gynaecological infections, particularly UTIs and cystitis. When travelling, it’s essential to prioritise cleanliness. Carry antibacterial wipes to clean your hands before and after using public toilets.
3. Choose comfortable clothing
Believe it or not, your choice of clothing can impact your risk of developing UTIs. Tight-fitting clothes, especially in the pelvic area, can trap moisture and create an environment conducive to bacterial growth.
Opt for loose-fitting, breathable fabrics to allow proper air circulation. Additionally, change out of wet bathing suits promptly to prevent the proliferation of bacteria.
By paying attention to your wardrobe choices, you can significantly reduce the risk of developing uncomfortable infections during your travels.
4. Treat constipation
Exploring new cuisines can lead to various challenges for travellers. While some may grapple with traveller’s diarrhoea, others might experience constipation due to altered eating patterns, dehydration, increased alcohol consumption, and a more sedentary lifestyle.
Unfortunately, constipation increases your risk of contracting a UTI. To mitigate this risk, aim to eat a diet rich in fibre, stay active, and drink plenty of water.
5. Carry a female health kit with you whilst you travel
If you experience any symptoms of a UTI or gynaecological infection, it’s crucial to have medications on hand so you can continue your holiday or travel unaffected.
Carrying a female health kit with you whilst you travel means you can detect and treat your UTI symptoms whilst on-the-go. It contains urine test strips which can confirm if you have a urine infection as well as antibiotics and cystitis relief sachets to alleviate symptoms of inflammation.
Symptoms of a UTI may include frequent and painful urination, lower abdominal discomfort, blood in your urine, a high temperature or lower back pain.
Take our free online consultation to see if you can buy a female health kit online.
Remember, in addition to self-treatment, it’s crucial to seek prompt medical attention, especially if symptoms worsen.
Your travel experience should be memorable for all the right reasons, not marred by the discomfort of a urinary tract infection.
By following these essential tips – from prompt bathroom breaks, to arming yourself with the right travel medicine – you can significantly reduce the risk of encountering a UTI while abroad.
Our female health kits are designed for travel and contain everything you would need to treat and alleviate symptoms for a urinary or gynaecological infection. Begin by completing our free online consultation today.
Whether you’re prone to urinary tract infections, or have never experienced one before, it’s a good idea to buy a female health kit before any trip or holiday and arm yourself against the discomfort and misery of a UTI while abroad.
Fleet St. Clinic is here to support your well-being whilst you travel.
Stay healthy, stay informed, and make the most of your travels!
Related services available at Fleet Street Clinic
Blue Monday happens every year on the third Monday of January. It is supposedly the most depressing day of the entire year, based on a crude calculation of bad weather, long nights, back to work dread and post-Christmas debt.
It does sound very plausible perhaps because we so familiar with the term “January Blues” but Blue Monday is in fact, a myth!
The phrase “Blue Monday” was coined by Sky Travel back in 2005 as a way to encourage people to book their next holiday as something to look forward too. They highlighted all the seasonal negatives to reinforce the benefits of booking a holiday – a clever marketing trick.
But can we really pinpoint the most depressing day of the year?
There is no actual scientific studies that have ever backed up any claims about Blue Monday being true or that there could even be a “most depressing day of the year”. This does make sense because this would be different for each and every one of us based on personal circumstances and the variables are extensive. It did, however, get use thinking about our mood, mental health and overall wellbeing at this time of year.
January is cold, often wet and everyone is trying to shake off the Christmas comedown and get excited about the new year ahead, but the January blues can creep in.
Remember you are not alone, and many people experience a dip in mood this time of year but it is important to identify when the January blues are actually symptoms of depression.
Depression is more than simply feeling unhappy, fed up or low for a few days. It can be long lasting and the symptoms range from mild to severe. Once accessed by a doctor, they will conclude the severity of your depression.
A simplified description follows:
Mild depression will have some impact on your daily life.
Moderate depression has a significant impact on your life.
Severe depression makes it almost impossible to get through daily life.
Sometimes there’s a trigger for depression. Life-changing events, such as bereavement, losing your job or giving birth, can bring it on. Other times, it can be linked with family history; people with family members who have depression are more likely to experience it themselves. But you can also become depressed for no obvious reason. It is quite complex and each person is unique.
There are many symptoms of depression and the combination is unpredictable.
They can be categorised at physiological, physical and social symptoms.
Some examples of psychological symptoms of depression include:
- continuous low mood or sadness
- feeling hopeless and helpless
- having low self-esteem
- feeling tearful
- feeling irritable and intolerant of others
- having no motivation or interest in things
- finding it difficult to make decisions
- not getting any enjoyment out of life
- feeling anxious or worried
- having suicidal thoughts or thoughts of harming yourself
Some examples of physical symptoms of depression include:
- moving or speaking slower than usual
- changes in appetite or weight (usually decreased, but sometimes increased)
- constipation
- unexplained aches and pains
- lack of energy
- low sex drive
- changes to your menstrual cycle
- disturbed sleep – for example, finding it difficult to fall asleep at night or waking up very early in the morning
Some examples of social symptoms of depression include:
- avoiding contact with friends and taking part in fewer social activities
- neglecting your hobbies and interests
- having difficulties in your home, work or family life
The most common symptoms of depression tend to be a low mood, feelings of hopelessness, low self-esteem, lack of energy, problems with sleep and a loss of interest in things you used to enjoy but it can be any number of symptoms listed above.
It’s important to seek help from a GP if you think you may be depressed. The sooner you see a doctor, the sooner you can be on the way to recovery.
For more information on GP services at Fleet Street Clinic, click here.
With every change of season comes a host of different medical issues, and winter can be one of the worst. With colder temperatures, shorter days, and seasonal illnesses circulating, it is one of the harder seasons to keep fit and healthy. There are certain conditions which are known to worsen in the colder months and so it is important to be aware of them and how you can best prepare yourself to keep healthy throughout winter.
These conditions include:
- Asthma
- COPD
- Circulatory disorders, such as claudication, Raynaud’s disease, and chilblains
- Ischaemic heart disease
- Hypothyroidism (if untreated)
- Osteoarthritis and any joint disorder to include rheumatoid arthritis
- Seasonal Affective disorder
- Allergic rhinitis
To reduce the increased risk associated with the above conditions, it is important to have a check up with your GP, ideally in the early Autumn before the Winter months. This will give you the best chance of getting ahead and allowing you to prepare for the coming season. But, if for whatever reason, you were unable to have a check up in Autumn, it is still beneficial to have a check up during the Winter months.
During a check up for asthma and COPD it’s advised to have a peak flow and lung function check. Asthma and COPD are worse in the dry, cold weather, so it is important to make sure you have plenty of your prescribed inhalers. It is best to be prepared rather than be taken unawares by an attack of wheezing. It is extremely important to see a doctor if you develop winter wheezing and are short of breath, especially during the night as this is when asthma and COPD attacks are most dangerous.
Circulatory disorders are worse in the cold weather as lower temperatures constrict blood vessels, increasing the likelihood of pain due to claudication (pain in the calves after walking a certain distance), Reynaud’s (discolouration of the fingertips due to constriction of the blood vessels) and chilblains (small, itchy, red patches on the skin). You can prepare for all of these conditions by obtaining prescriptions for treatment but most importantly, by keeping warm and preparing for the cold.
Ischaemic heart disease is also worse in the cold weather due to the effect of constricting blood vessels. It is important to have a cardiac check to include blood pressure, and if you suffer from angina, to ensure you have the medication to treat this painful condition which is likely to be much worse in the cold weather. Avoiding the extreme cold and wearing thermal clothing may also mitigate against the likelihood of a heart attack or myocardial infarction if you do suffer from Ischaemic heart disease.
If you suffer from Hypothyroidism, it is a good idea to have an annual blood test. Left untreated, hypothyroidism can cause increased sensitivity to cold, which can be particularly unpleasant in winter.
For those with arthritis of any kind, the best way to avoid pain and stiffness in the joints is to keep warm and keep the joints moving. Find more information on Arthritis in Winter here.
If your mood tends to be lower in the winter months, each year, you should have a check up with your GP to discuss Seasonal Affective Disorder (SAD). If you are diagnosed with SAD, consider CBT (Cognitive Behavioural Therapy) rather than medication if you can, and invest in a daylight lamp as these do help.
Allergic rhinitis is another ailment that tends to crop up a lot around winter time. This is diagnosed when you have a persistent nasal discharge. This can occur either as a result of pine or autumnal tree leaf mould, or due to house dust or mould which is often exacerbated by central heating. In this instance, nasal sprays and antihistamines are often required.
Finally, the Norovirus peaks in November until April. This is a really unpleasant vomiting virus which is picked up from contaminated surfaces or foods. To help avoid this nasty bug, always wash hands when handling food and make sure food is washed thoroughly before cooking or eating raw.
If you know or suspect that you might suffer from any of these conditions, please do visit your GP to help you keep prepared. Similarly, if anything new arises you should see your GP as soon as you can; the earlier a health condition is addressed, the easier it is to treat.
In general, an annual medical is a good way to give you a full-body overview of your health, as well as monitor the progression of any existing health conditions. A varied, balanced diet and regular exercise will also be crucial in keeping you generally fit and healthy throughout winter.
For more information on our GP Services.
Book a GP Appointment or an Annual Medical.
Arthritis is a common condition that causes pain and inflammation in joints. It is not a single disease but an informal way of referring to joint pain or joint disease. There are more than 100 types of arthritis and related conditions. There are thought to be 10 million people with some form of arthritis in the UK. It is the most common cause of disability in the UK and can affect people of all ages but it does occur more frequently as people get older.
Common arthritis joint symptoms include swelling, pain, stiffness and decreased range of motion. Symptoms can range dramatically from person to person, with some experiencing mild symptoms with occasional flare ups to those who experience constant debilitating pain everyday. The sad truth is that there is no cure for arthritis, so it is all about pain management and how to best reduce flare ups.
The impact of the weather on the symptoms of arthritis has been debated for many years and people tend to report more arthritis flare-ups in the winter, but the reason why is not specifically known.
Quite often sufferers will state that their symptoms get worse when the weather is damp and cold and some state they are able to tell when the weather is about to change based on their arteritis symptoms worsening.
Even if there is currently nothing to support this scientifically, this doesn’t remove the pain felt by sufferers and so rather than comment on where this is true or not, let’s look at ways to reduce flare ups in winter.
Our top 4 tips:
1. Stay warm
When the temperature drops both inside and outside, dress warmly. Make sure all arthritis prone areas are kept warm.
2. Stay hydrated
Drink plenty of water throughout the day. Even mild dehydration might make you more sensitive to pain.
3. Take warm baths
A warm bath or visiting a heated swimming pool will ease joint pain and comfort you. If you visit a heated swimming pool, gentle exercise will also help your mobility.
4. Stay active
It is now clear that active people experience less joint pain than those who are sedentary. If you are experiencing an arthritic flare then reduce your usual activity (but don’t stop altogether) and use simple anti-inflammatory medication such as ibuprofen if it is safe for you to do so.
Enjoy winter while taking the above precautions for Arthritis.
If you are facing extreme discomfort and pain in your joints due to arthritis, book an appointment with a GP to discuss your options.
In the months since its release in the UK, we have seen a huge demand for the new Dengue vaccine, Qdenga.
For those with experience of the disease, the news of its licensing has been much anticipated and we are proud to be one of the first clinics in the UK to offer the vaccine.
What is Dengue Fever?
Dengue is a viral infection that is spread through the bite of an infected aedes mosquito, a species easily recognisable by its striped legs. It occurs in over 120 countries worldwide, mainly in the tropics and sub-tropics, and is the second most common cause of fever in the returning traveller.
The most seriously impacted regions are the Americas, South-East Asia, and Western Pacific, with Asia accounting for around 70% of the world’s disease burden.
It is also spreading to new areas, including Europe, where outbreaks have been increasing in recent years. Read more about this in our recent blog, Dengue Fever in Europe: Temperature Risk.
Since it is transmitted from person to person, via the mosquito vector, it is of particular concern in populated, urban areas.
What are the symptoms of Dengue Fever?
Whilst most cases are asymptomatic, some will develop a severe flu like illness that can require hospitalisation. In rare cases, this will be life threatening.
Common symptoms include;
a high fever,
severe headache,
pain behind the eyes,
muscle ache,
joint pains,
nausea,
vomiting and rash.
There are four serotypes of Dengue virus; for those infected by one type, a subsequent infection is more likely to be life threatening. The severe type of Dengue usually starts a few days after the initial symptoms began. After feeling a bit better, symptoms suddenly return and can include severe abdominal pain, persistent vomiting and bleeding.
Approximately 1 in 20 patients with Dengue will progress into the severe form of the disease.
Dengue Fever Vaccination
Historically, the only protection we could provide was advice surrounding mosquito bite avoidance. With the arrival of Qdenga, we now have the option of a vaccination which provides safe and effective protection.
Studies have shown Qdenga to offer 80% protection from the first dose, with long term immunity achieved after the second.
Who should get vaccinated?
Qdenga can be safely given to those who have previously had the disease, and it is especially important for this group. We would also encourage frequent or long stay travellers to consider the vaccine. The vaccine is licensed for the prevention of Dengue in individuals from 4 years of age and requires two doses, to be given three months apart.
It is a live vaccine, so it’s not suitable for everyone. To discuss your suitability with one of our specialist travel nurses, please book a travel consultation online, or call our reception team on +44 20 7353 5678.
We can usually accommodate same day bookings and suitable vaccinations can be given within the same appointment.
Related services available at Fleet Street Clinic
Travellers’ Diarrhoea Online Consultation
For further reading
In September 2021, Public Health England released new rules surrounding the timing of BCG vaccination, increasing the minimum age of vaccination to 28 days. This has been implemented in line with a pilot disease screening programme that tests eligible newborns for Severe Combined Immunodeficiency (SCID), the outcome of which becomes available by the time the baby is 6 weeks old. It is important that we wait for the result of this test before giving the BCG vaccine.
What is SCID screening?
All newborn babies in the UK are currently offered blood spot screening (heel prick test) that looks for 9 rare diseases, including sickle cell and cystic fibrosis. The NHS is considering introducing an additional test for Severe Immunodeficiency (SCID), a name given to a group of rare, inherited disorders that cause major abnormalities in the immune system. Affected infants have an increased risk of life-threatening infections and will normally become severely unwell in the first few months of life. Without treatment they will rarely live past their first birthday. About 14 babies a year are born in England with SCID.
The evaluation of this testing, which began on 6th September 2021, is taking place in 6 areas across England and will cover around 60% of new born babies. It is running alongside the existing blood spot screening and the intention is to roll it out nationally once the 2 year evaluation has been made.
Why does this affect the BCG vaccination?
Bacillus Calmette-Guérin (BCG) is a live attenuated vaccine that can cause problems if given to an immunocompromised person. Treatment for SCID is more complicated if the child has received the BCG vaccine, so it is important that if your child has been tested. We wait for a negative result before vaccinating.
What we need from you:
If your child was included in the SCID programme, you will need to provide a letter that confirms the negative result of screening.
If your child was born outside of the programme areas and therefore, not included in the SCID programme, we will need to see a letter confirming this.
In either case, please bring the letter with you to your appointment, as well as your child’s vaccination book.
Nb. If your child was born before 1st September 2021, before the programme was introduced, no letter will be needed.
For more information on:
Other Childhood Vaccinations
RSV is a common and highly contagious respiratory virus that is a leading cause of lung disease. RSV is seasonal, and like other respiratory viruses, its peak incidence is during the winter months each year. It spreads from person to person via droplets, or from infected surfaces or objects. RSV is a virus, so antibiotics are not effective.
Arexvy is a new vaccination designed to protect against lower respiratory tract disease caused by respiratory syncytial virus (RSV). It is an important advance, because no specific treatment for RSV is available, and infection is often severe.
Older adults, and those with underlying medical conditions such as diabetes, heart disease and lung diseases such as asthma and COPD are at the greatest risk of the infection. RSV can exacerbate these underlying conditions and lead to pneumonia.
In the UK, RSV causes more hospitalisations and deaths than flu in those over the age of 60. It is estimated that RSV causes14,000 hospitalisations and an estimated 8,000 deaths in adults 60 years of age and older each year.
Arexvy is a recombinant adjuvanted vaccine for the prevention of RSV is adults 60 years of age and above. It is the only licensed vaccination in the UK that has been authorised for use by the Medicines and Healthcare products Regulatory Agency, meaning at risk adults are now able to be vaccinated against the disease.
Arexvy is as in inactive vaccination and only requires single dose for protection. It can be administered at the same time as other vaccinations including flu, pneumococcal, and COVID.
We are among the first practices in the UK to offer it to adults needing protection.
We are delighted to announce that Fleet Street Clinic, together with our optical practice, Whitby & Co. have achieved ISO 27001:2022 accreditation for excellent security practice across our business.
ISO 27001 is the ultimate benchmark for businesses to establish, implement, and maintain a strong information security management system.
With ever growing concern around data and cyber security, this achievement gives an additional layer of assurance to our patients and business partners alike, that our data security practices meet independently-assessed world-class quality standards.
ISO 27001 is the globally recognised standard for information security management, and we are proud of our team’s accomplishments.
‘The ISO 27001 certification gives reassurance to our current and future patients and business partners that information and data security has been, and continues to be, of the highest importance – I am proud of the entire team for this wonderful achievement.’
Dr Richard Dawood – Medical Director & Founder
Fleet Street Clinic and Whitby & Co. went through a rigorous audit, addressing risk factors across the business, and ensuring robust cyber security levels and business continuity were in place. This accreditation demonstrates our continuing commitment to risk management, cyber-resilience, digital defence and operational excellence.
Click to view our accreditation certificate.
More information on ISO 27001 accreditation
ISO 27001 accreditation details the requirements for businesses to securely manage information assets and data to an internationally recognised standard. It provides a robust approach for managing assets such as employee details, patient information, intellectual property, financial information and third-party data.
The accreditation requires the business to assess their information security risks, put in place robust security controls and processes, and embed information security management across the organisation.
Achieving accredited ISO 27001 certification demonstrates that a company is dedicated to following the best practices of information security. Additionally, ISO 27001 certification provides an expert evaluation of whether an organisation’s information is adequately protected.
Click to view our private patient services or our workplace healthcare services.
If you have a heart condition you have a greater risk of becoming more seriously ill from flu (seasonal influenza) than the general population. In addition, having the flu can exacerbate pre-existing conditions like diabetes or asthma.
According to the NHS, “every year over 11,000 people in England die from complications caused by the flu virus. Many of these deaths could have been prevented by having the flu vaccination.”
Preventing the flu in the first place is the best option.
The best protection is to have a Flu Vaccine each winter.
What is the flu?
Many people think having influenza, also known as the flu, is like having a bad cold, but in reality flu is a nasty respiratory virus that can make you very unwell. Influenza causes inflammation in the body and can be very serious – sometimes leading to hospitalisation or even death.
There is evidence that heart attacks happen more often during or immediately after an acute inflammatory illness, such as flu.
A flu jab is the best protection against flu.
In general, the flu causes stress and inflammation on the body, increasing blood pressure, heart rate and heart function. This is not good for someone with heart or circulatory problems.
Flu vaccination is strongly recommended for anyone who has ever had a heart attack, stroke or has underlying heart disease. A previous diagnosis of heart or circulatory diseases is considered a high risk factor for complications or even another heart attack, for anyone who becomes ill with flu.
Does flu affect heart medication?
If you take warfarin, flu symptoms can affect your blood clotting rate (INR). You should speak to your doctor if this happens so they can monitor your situation closely. It does also mean if you do become unwell, it may take you longer to recover than the average person.
In addition, some over-the-counter flu medicines can’t be used when taking medicines for heart conditions, so contact your doctor before taking things like painkillers and cough medicines. It is better to check before beginning any new medications.
When is the best time to get the flu jab?
Flu vaccinations become available from mid to late September, and through the season until February. It’s best to get your flu vaccine in September or October. The peak time for catching flu runs from Christmas to Easter. The aim is to be vaccinated before flu transmission starts, and to allow at least a couple of weeks post-vaccination, for maximum immunity to develop. The sooner you have the vaccination, the sooner you will be protected.
You can book your flu jab online.
We have a range of flu vaccinations available, including the premium recombinant vaccine, cell-based vaccine, FluAd (for those aged 65 year and older), kids nasal spray and the standard flu jab.
It is important to have a flu jab every year because the flu virus can change. There are many strains of flu already and some are more dominant than others. Each year strains are analysed to determine which strains are likely to be the prevalent strains circulating that year. They can vary year to year so relying on a past vaccination for protection is risky. The previous year’s vaccine may not offer you the right protection against the strains in circulation this year.
In addition, immunity to flu decreases over time. Exposure to the flu virus strengthens the immune response and offers natural protection. With less flu circulating over the past few years due to covid restriction measures, natural immunity in the general population will have decreased.
A flu vaccine will boost immunity.
With most workers now returned to the office and social distancing restrictions long gone, there is a greater chance of the flu spreading and more people falling ill this winter. With both illnesses circulating around it is highly recommended to reduce the risk by getting the flu jab.
Protect yourself against the flu.
You can find more information on the types of flu vaccines available.
For more information on the premium recombinant flu jab.
_____________
Wanting to book a Workplace Flu Vaccination Programme?
Flujabs.org is part of Fleet Street Clinic and has been providing workplace flu vaccinations to UK businesses for many years.
Fill out the online form and one of our flu coordinators will get back to you with current availability and costs.
Some infections can harm your baby if you catch them during pregnancy. Research suggests that the flu, in particular strains such as H1N1 (swine flu), can significantly increase the risk of complications to expecting mothers and their unborn babies.
Vaccinating expecting mothers against flu or before pregnancy can provide the newborn baby with significant ‘passive’ protection – which can last several weeks after birth. This is important because babies cannot be vaccinated themselves until they are 6 months old. So, a mother’s vaccination is strongly advised.
Fleet Street Clinic are urging all the mums-to-be to have the vaccine. The Quadrivalent Flu Jab can be safely given at any point during pregnancy.
Pregnant women are less able to fight off infections and therefore more likely to be seriously ill if they contract the flu virus. Pregnant women are at risk of complications from the flu at any stage of pregnancy. So therefore, it is important for those expecting to get their flu jab as early as possible.
If you are currently planning your pregnancy, it would be sensible to consider getting your flu jab prior to becoming pregnant.
The flu vaccine can safely be given to pregnant women at the same time as the whooping cough vaccine. You can have the whooping cough vaccine from 16 weeks onwards.
The vaccine is inactivated, and cannot cause flu itself.
Having the flu vaccine is the best protection.
If you are interested in booking flu vaccinations for your staff, visit flujabs.org for more information and to get a quote.
STUDENTS URGED TO GET VACCINATED BEFORE UNIVERSITY
The UK Health Security Agency (UKHSA), formerly known as Public Health England, is encouraging students to get vaccinated before they start/ return to University to protect themselves against a range of life-threatening illnesses.
Starting university and attending Fresher’s Week exposes students to a host of viruses and bacteria – some of which for the first time.
First year or returning students can be at increased risk of serious diseases such as meningitis, septicaemia and measles as they mix with large numbers of other students from around the country and overseas.
We strongly advise the following 3 vaccinations at a minimum for students:
Meningococcal ACWY (MenACWY)
– Protects against 4 common strains causing meningitis and septicaemia
Measles, Mumps and Rubella (MMR)
– Protects against measles, mumps, rubella
Human Papillomavirus (HPV)
– Protects against HPV-related cancers including cervical, penile & throat cancers, alongside protection against genital warts. HPV vaccination is estimated to prevent up to 90% of HPV-related cancers.
Meningitis Vaccinations:
– Meningococcal ACWY (MenACWY)
– Meningococcal B (MenB)
UKHSA vaccine coverage data shows around 1 in 8 new students going to college and university this year remain unprotected against these 4 strains of meningococcal bacteria, each of which can cause long term disability, serious health complications and can be life threatening.
The MenACWY vaccine is given by a single injection into the upper arm and protects against four different strains of the meningococcal bacteria that cause meningitis and blood poisoning (septicaemia): A, C, W, and Y. You can book online.
The MenB vaccine is also given as an injection to the upper arm but is a 2-dose course for full protection. It protects agains the B-strain of the meningococcal bacteria. You can book online.
Cases of meningitis, particularly virulent strain Men W & Men B, have been rapidly rising amongst students since 2009.
What is Meningitis W?
Meningitis is a bacterial infection of the protective membranes surrounding the brain and spinal cord. Meningococcal meningitis (Men W) is a highly serious form of bacterial meningitis that can lead to septicaemia. It is spread by droplets that come from a person who is infected with the bacteria.
Although the strain is most likely to affect babies, statistics reveal that older children, teenagers, and adults are also at risk. In recent times, cases amongst normally healthy teenagers have spiked and the fatality percentage is higher with Meningitis W than it is with the most common strains, Meningitis B and C.
Meningitis can progress quickly leading to blood poisoning (sepsis), which can kill within 24 hours. So, it is important to know the signs and symptoms of meningitis and septicaemia (sepsis).
Early symptoms of Meningitis include:
- headache
- a high temperature (fever)
- being sick (vomiting)
- a rash that does not fade when a glass is rolled over it (but a rash will not always develop)
- a stiff neck
- a dislike of bright lights
- cold feet and hands
- or muscular pain
Sepsis is a life-threatening reaction to an infection. It happens when your immune system overreacts to an infection and starts to damage your body’s own tissues and organs. Symptoms can be vague but include:
- acting confused, slurred speech or not making sense
- blue, pale or blotchy skin, lips or tongue
- a rash that does not fade when you roll a glass over it, the same as meningitis
- difficulty breathing, breathlessness or breathing very fast
Many people confuse the symptoms with just a hangover or freshers’ flu, which is one of the theories as to why students are so high-risk. So, check-in on your friends who are unwell. Symptoms can progress rapidly so urgent action in getting medical attention is critical – call NHS 111 straight away
Protection against this strain of Meningitis W is provided through the Meningitis ACWY vaccine. Only one dose is required.
We also carry an excellent stock of the Meningitis B vaccine and can provide both vaccinations at the same time should you require it.
Book your MenACWY & MenB vaccination appointment online
Measles, Mumps and Rubella (MMR) Vaccination
Mumps is a highly contagious viral infection which is spread in the same way as the flu. Coughing, sneezing and kissing can rapidly spread the infection, especially in the close quarters of student accommodation.
Measles is a very infectious viral infection which is also spread by coughing and sneezing. There have been multiple outbreaks of Measles around the world including the UK this year, so it’s important to make sure you are protected as you socialise with new peers.
Both Mumps and Measles can be prevented by safe and effective vaccination, MMR.
Book your MMR vaccination appointment online
Human Papillomavirus (HPV) Vaccination
HPV is a common virus that is passed on via genital contact. There are more than 100 HPV types which infect genital areas. Sometimes they cause no harm and the infection can go away on its own. However, the virus can persist and cause cells to change which can lead to some forms of cancers; cervical, head, neck & throat or genital warts. More information on HPV can be found here.
The HPV vaccine is offered at our clinic for girls and boys to protect against HPV-related cancers and genital warts. Book your HPV vaccination appointment online
Other vaccinations that we recommend for students starting/ returning to University are:
Fresher’s Flu:
Every year different flu strains circulate and infect millions of people. Being exposed to a new pool of infections in University accommodation can increase the risk of catching the flu. Having the flu jab before you go to University will help protect you against the flu and stop you getting sick.
Flu jabs become available from 3rd September and can be booked online.
BCG:
If you are from outside the UK, you should be vaccinated against tuberculosis (TB) before you enter the UK. A weakened strain of tuberculosis, the BCG Vaccine, is injected to protect against the infection. Those unsure of their immunity can have a simple Mantoux test to confirm.
Book your BCG vaccination or Mantoux Test appointment online
Tetanus:
Tetanus is a rare condition caused by bacteria entering a wound. We recommend making sure you are up to date with your DTP vaccinations and boosters before leaving for university. This vaccine protects against tetanus as well as Diptheria and Polio. Don’t let a cut or burn ruin your freshers week.
Book your Tetanus vaccination appointment online
Wellness VACCINATIONS AT FLEET STREET CLINIC
Fleet Street Clinic offers a friendly environment and a team of experienced medics to administer all wellness vaccinations. We meet rigorous quality management standards to ensure we offer you the highest standards of clinical care: you can feel confident you are in safe hands.
Secure your peace of mind by ensuring you are protected. Get your vaccines before university starts to receive protection in time.
Book your vaccination appointment today
_____________
For the full The UK Health Security Agency (UKHSA) statement, click here.
Recombinant Flu Jab – The Most Advanced Protection from Influenza
In a world constantly battling the threat of infectious diseases, the importance of vaccinations cannot be underestimated. Influenza – the flu – is a year-round, global respiratory threat that remains a constant concern, owing to the ability of flu viruses to mutate rapidly and cause seasonal epidemics.
As science advances, so does our ability to protect ourselves from flu. Applying recombinant technology to flu vaccines is a remarkable breakthrough that has created a new generation of premium vaccines, capable of delivering enhanced protection.
Why are recombinant flu vaccines the premium offering in comparison to other flu vaccines?
Traditional flu vaccines are created by growing influenza viruses in chicken eggs, allowing the viruses to replicate, and then inactivating or weakening them for use as vaccines. This process, while effective, presents several challenges, including the potential for the virus to mutate during replication in eggs.
Recombinant flu vaccines offer an innovative alternative to these traditional methods. Instead of using live viruses, these vaccines utilise genetic engineering techniques to produce specific proteins found on the surface of the influenza virus. These proteins are then harvested and used as the key components in the vaccine.
Notably, recombinant flu vaccines eliminate the need for egg-based production, thus addressing concerns related to egg allergies and the risk of viral mutations.
Key benefits
Precise Targeting: Recombinant flu vaccines consist only of precise copies of the surface antigen proteins that flu viruses use to enter our cells. This enables the immune system to recognise and remember them, ensuring the most robust immune response possible whenever flu viruses are encountered.
Enhanced Effectiveness: The genetic engineering process in recombinant vaccines ensures a high degree of consistency and purity in the vaccine components. This consistency translates to enhanced vaccine effectiveness, reducing the risk of a mismatch between the vaccine strains and the circulating flu viruses.
Reduced Allergic Reactions: Individuals with egg allergies often face a dilemma when considering traditional flu vaccines, as these vaccines are cultivated in eggs. Recombinant flu vaccines eliminate this concern, providing a safe option for those with egg allergies.
Forward-Thinking Defence: The adaptability of the flu virus demands a vaccination strategy that can keep up with its mutations. Recombinant vaccines, designed with a focus on the virus’s evolutionary genetics offers a forward-thinking defence by stimulating immunity against a broader range of potential viral strains.
Broader Accessibility: Traditional flu vaccine production is dependent on the availability of fertile chicken eggs and a lengthy production process. Recombinant vaccines overcome these limitations, allowing for more rapid production and distribution, even in situations where egg supplies are compromised.
So, why choose a recombinant flu jab over a traditional standard fu jab?
In the fight against influenza, staying ahead of the mutating virus requires cutting-edge solutions. Recombinant flu vaccinations represent a quantum leap in our approach to flu protection, offering a targeted, effective, and forward-looking defence against the ever-changing flu strains.
As technology continues to evolve, these vaccines hold the promise of becoming the gold standard in flu protection, providing individuals with a safer, more reliable shield against this seasonal threat.
So, when the flu season comes around, consider the power of recombinant flu vaccinations—the premium offering for your ultimate flu protection.
Private Patients
For more information on our flu vaccinations and pricing.
Workplace Flu Vaccination Programmes
Fill out the form below for a quote for flu jabs for your employees.
______________
RELATED SERVICES AVAILABLE AT FLEET STREET CLINIC
As a leading London-based private health clinic, we at Fleet St. Clinic are committed to delivering individualised care and investing in the health and well-being of employees across various companies.
Recognising the challenges brought on by the post-pandemic surge in long-term sickness, we wholeheartedly support the government’s initiative to offer tax breaks for preventative care aimed at keeping employees fit and productive in their roles.
Addressing the Impact of Long-term Sickness: A Collaborative Approach
Recent data has highlighted a concerning increase in long-term sickness, with 2.5 million people currently off work, a number that has risen by 400,000 since the onset of the Covid pandemic. The impact on welfare bills and the economy cannot be underestimated, making it imperative for both employers and policymakers to take proactive measures to address this issue.
At Fleet St. Clinic, we believe in adopting a collaborative approach to tackle this challenge effectively. The expansion of tax breaks for tests, screenings, and preventive care will hopefully empower more businesses to invest in their employees’ well-being without incurring additional financial burdens. This will not only reduce sick days but also enhance overall performance and productivity in the workplace.
Fostering a Healthier Workforce with Occupational Health Services
As a longstanding provider of occupational health services, we understand first-hand the pivotal role that occupational health services play in preventing illness and fostering a healthier, happier workforce.
At present, less than half of employers offer any form of occupational health services, a number that drops to less than a fifth among small businesses.
While previous efforts focused on getting the long-term sick back to work, we strongly support the current approach of preventing individuals from leaving their jobs due to health issues in the first place. We are on a mission to encourage companies of all sizes and industries to provide comprehensive occupational health services to their employees throughout their careers.
How Tax Breaks Can Support Your Occupational Health Offerings
Under the proposed scheme, tax breaks will be extended to a wider range of treatments designed to maintain a healthy workforce. General medical check-ups, flu vaccinations, health screenings, and treatments that reduce workplace absence or enhance employee performance will be eligible for these tax incentives. Notably, this does not include private medical insurance or wellness treatments like gyms or spas.
The government aims to expand the current scope of tax breaks, such as remove the £500 cap for medical treatment funded by an employer to help employees return to work, benefitting both employers and employees alike.
Prioritising Workforce Participation and Health
As we move forward, we are keenly aware that the final package of incentives will be influenced by economic conditions and government priorities. Nonetheless, the government’s commitment to improving workforce participation and addressing health challenges presents an exciting opportunity for companies to prioritise the well-being of their employees and contribute to a more robust and prosperous economy.
Let us Support Your Business
At Fleet St. Clinic, we stand ready to support businesses in their efforts to implement comprehensive occupational health services, provide preventative care, and make use of the proposed tax breaks.
Our mission is to contribute to a healthier, happier, and more productive workforce for your business, offering full support start to finish.
As we await further developments, we continue to champion the benefits of employee health and well-being, and we look forward to working hand-in-hand with companies across London to build a thriving, healthy workforce that can meet the challenges of the future with strength and resilience.
Together, we can make a lasting impact on individual lives and the wider community.
If you’d like to start the conversation about how we could support your employee’s health, fill out the form below and we’ll propose suitable services for your consideration.
______________
RELATED SERVICES AVAILABLE AT FLEET STREET CLINIC
New figures from the UK Health Security Agency (UKHSA) state that England is seeing a significant increase in sexually transmitted infections in the community, specifically gonorrhoea and syphilis which have exceeded pre-Covid figures.
The data demonstrates that testing for STIs has resumed to expected levels, following a dip during the Covid years, however the number of positive results has seen a higher-than-expected increase. The UKHSA states that some of the rise will be due to increased testing, but the scale of the surge strongly suggests a genuine increase in infections in the community.
The number of gonorrhoea diagnoses rose by 50% between 2021 and 2022, with 82,592 cases reported in 2022 alone. Syphilis cases also saw a 15% increase during the same period, reaching 8,692 cases. The cases for Chlamydia and herpes are also on the rise from last year.
These numbers surpass pre-pandemic levels and signal a pressing need for more regular testing.
A snapshot of the data includes:
- Sexual health screens or tests carried out increased 13% than the previous year
- Chlamydia was the most diagnosed STI overall
- Syphilis cases reached the highest in any given year since 1948
- Gonorrhoea numbers were the highest since annual records began in 1918
Getting tested frequently is key.
Regular sexual health screenings are essential for early detection, especially as many STIs can be asymptomatic.
Getting your results quickly allows for timely treatment and faster recovery. Understanding how quickly a provider can turnaround your results is an important aspect of your research. Turnaround times vary dramatically depending on if your test can be done in-house or sent to an external laboratory.
At Fleet St Clinic, we understand the urgency for quick results. By using our in-clinic laboratory, we can rapidly turnaround results, usually within 2 hours.
We encourage all our patients to prioritise their sexual health and use our confidential sexual health services to ensure they are fit and healthy.
We can test and treat:
How can you protect yourself?
It’s important to take proactive steps to stay sexually healthy and informed.
- Practice safe sex
Consistently and correctly using barrier methods of contraception, such as condoms, can greatly reduce the risk of sexually transmitted infections (STIs) and unintended pregnancies.
- Get tested regularly
Regular testing helps detect and treat STIs early, preventing further transmission and potential complications.
- Open and honest communication
Effective communication with your sexual partners is key to maintaining a healthy sexual relationship. Discussing topics like STI status, sexual history, and contraception methods fosters mutual understanding and trust.
- Stay up to date with vaccinations
Certain vaccinations, such as those for human papillomavirus (HPV) and hepatitis B, can protect against STIs and related health issues.
- Seek healthcare when needed
Prompt diagnosis and treatment are essential for preventing complications.
How to book an appointment at Fleet St. Clinic:
Do you have symptoms? Yes.
Don’t panic – It is important to remember that most STIs can be treated with simple medication.
Book a Symptomatic Consultation with one of our GPs.
You can select the sex of your doctor, so you feel at ease to discuss your symptoms and any concerns you have. They will advise which tests are suitable for you to have during your appointment and let you know if you need to come back for any additional tests.
We’ll provide you with results and advise appropriate treatment options.
It is important to know that not everyone has symptoms.
If you don’t have symptoms, you should still get tested regularly as part of your overall health and wellbeing, especially if you have concerns about being exposed to a STI.
Book an Asymptomatic Consultation with one of our nurses.
During this consultation you can discuss any concerns you may have, your recent sexual history and one of our nurses will offer guidance on which tests would be appropriate for you to have.
The timing of STI testing after potential exposure varies depending on the specific infection so you may be advised that you will need to come back for additional tests. If you test too soon after exposure to an STI aka during the “window period”, you may not get an accurate result.
Results from all testing are discreet and timely and if anything is detected, all treatment options will be explained to you clearly and sympathetically.
By prioritising sexual health and seeking timely testing and treatment, you can mitigate the impact of STIs and reduce the infection risk in the community.
Please note: This post is for informational purposes only and should not substitute professional medical advice. Please book an appointment with a healthcare provider if you have any sexual health concerns.
Related services available at Fleet Street Clinic
Sexual Health Testing Services
Continued reading about the UK Health Security Agency (UKHSA) “Sexually transmitted infections and screening for chlamydia in England: 2022 report”
Read the full report by UKHSA here
Read: Gonorrhoea and syphilis sex infections reach record levels in England
In today’s health-conscious era, prioritising well-being has become a central focus in our lives. However, understanding just how fit we truly are requires a comprehensive approach.
A medical check-up is the optimal method for obtaining a holistic view of your overall health. Familiarising yourself with essential health indicators can play a pivotal role in preventing potential illnesses and diseases.
Here’s a breakdown of key health numbers that can provide valuable insights into your well-being:
- Body Mass Index (BMI):
- BMI, frequently mentioned in the media, is a straightforward index of weight-for-height. It classifies individuals as underweight, overweight, or obese based on the ratio of their weight to the square of their height in meters.
- Resting Heart Rate:
- Your resting heart rate serves as an indicator of your basic fitness level and is a reliable predictor of cardiovascular health. Monitoring this metric can offer valuable insights into your overall well-being.
- Waist to Hip Ratio:
- The distribution of body fat, especially around the abdominal area, can impact health significantly. Research suggests that fat stored in this region may contribute to heart disease, obesity, and diabetes. Understanding your waist-to-hip ratio is crucial for assessing this risk.
- Cholesterol:
- Surprisingly, over half of all UK adults have elevated cholesterol levels, and a cholesterol test is the only definitive way to ascertain if you are affected. High cholesterol is linked to heart disease, a prevalent cause of mortality in the UK.
- Blood Pressure:
- Elevated blood pressure places additional strain on your arteries and heart, potentially leading to severe health issues such as heart attacks, strokes, kidney disease, or dementia. Regular blood pressure tests are essential for early detection and preventive measures.
- Blood Sugars:
- Monitoring your blood sugar levels is critical for identifying diabetes or the risk of developing it. For type 2 diabetes, often associated with lifestyle factors, early detection allows for dietary adjustments that may prevent the need for medication and even avert the onset of the disease.
- Bone Density:
- Bone density testing, a non-invasive procedure known as bone densitometry or a bone mineral density scan (BMD), provides insights into the strength of your bones. This assessment can reveal potential risks of osteoporosis, guiding proactive measures for bone health.
- Mammogram/Prostate Check:
- Depending on age, routine checks like mammograms for women and prostate checks for men are advised by healthcare professionals. These screenings are crucial for early detection of tumors or cancerous cells, significantly improving the chances of successful intervention.
If you’re interested in discovering your health numbers, consider booking a comprehensive medical check-up or consulting your GP to determine which medical is best suited for you.
Prioritising these assessments can empower you to take control of your well-being and make informed decisions about your lifestyle.
Hajj and Umrah are religious pilgrimages to Mecca, Saudi Arabia. Hajj is a mandatory Pilgrimage for every Muslim to take once in their lifetime, given that the individual is physically and financially able.
It takes place in the last month of the Islamic calendar and is taken annually by 2.5 million Muslims worldwide pre-pandemic. Whereas, Umrah is a shorter pilgrimage to Mecca taken any time of the year.
Muslims from all over the world gather annually in Mecca in a display of unity, faith and solidarity. Due to the large number of participants performing the pilgrimage there are some health risks you should be aware of.
There are also health requirements set by the Health Ministry of Saudi Arabia that you could affect your VISA. It is good to be aware of those requirements before travelling.
COVID-19 Requirements:
Ministry of Health KSA states that in order to perform Hajj pilgrims, one must have the proof for the following:
- A full course of COVID-19 vaccinations (second dose of a two dose vaccine or received a single dose vaccine) approved by the Saudi Ministry of Health. The approved vaccines’ list can be found here – Ministry of Health Approved Vaccines.
- There is no longer a requirement for PCR testing to perform Hajj or to enter KSA.
Vaccine Requirements:
A pre-travel consultation should be scheduled at least 4 weeks before your trip.
Any mandatory or advised vaccinations will be discussed with a nurse and can be given in the appointment. Follow up doses can also be arranged in the appointment.
Before travelling to Hajj or Umrah, it is recommended that pilgrims be up-to-date with all of their wellness vaccinations.
– Meningitis
All British citizens travellers performing Umrah or Hajj are required to submit a valid Meningitis ACWY vaccination certificate in order to obtain a visa. The MenACWY vaccine protects against meningitis (strains A, C, W & Y) and sepsis. Adults and children over the age of 2 are required to have the vaccine and provide evidence of immunisation no less than 10 days before you plan to arrive in Saudi Arabia. This requirement also applies to seasonal workers in Hajj areas.
You may also want to consider Meningitis B vaccine – this is not a mandatory VISA requirement.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Covid-19
All travellers must be vaccinated against Covid-19 to perform Hajj Pilgrim. The vaccines that are approved by the Ministry of Health KSA can be found here – Ministry of Health Approved Vaccines.
– Polio
Travellers from countries reporting positive environmental sources samples of circulating vaccine derived polio virus 2 (cVDPV2), including the UK, are recommended to be vaccinated with at least one dose of IPV within the previous 12 months and at least four weeks prior to arrival, however there is no polio vaccination certificate requirement.
A polio certificate requirement will only apply to UK pilgrims if they are travelling to KSA via a country reporting WPV1, cVDPV1 or cases of cVDPV2 or Acute Flaccid Paralysis, and not if they are travelling directly to KSA from the UK.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Flu Vaccine
Since both Hajj and Umrah both pose crowded conditions and close contact, seasonal flu vaccination is advised, especially for those who are more vulnerable to severe influenza diseases. This precautionary measure will help reduce the potential spread of the flu.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Hepatitis B
Hep B is spread by contaminated blood and bodily fluid. Pilgrims who intend to shave their heads as one of the rites of Hajj should consider taking the vaccination. Although licensed barbers performing head shaving are obliged to use a new blade for each pilgrim, unlicensed barbers may not adhere to this practice. Vaccinations require 3 injections to be given over a 3 week period and can be given from birth.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
– Rabies
Rabies is spread through the bite of an infected animal such as cats, dogs, monkeys and bats. Saudi Arabia is classified as a high-risk country for rabies. Full protection is achieved with 3 doses – 3 vaccinations usually given over a 3 week period, however, we do offer a rapid course which can achieve full protection in 7-days. The rabies vaccine can be given from birth.
If you require a vaccination, you can choose from our available appointments online – click to book your appointment.
TRAVELLERS’ DIARRHOEA
Travellers’ diarrhoea can occur in up to 60% of travellers. Although most cases are mild, taking sensible precautions with food and water can reduce the risk. Carrying medicines for self-treatments is useful such as antibiotics – take our Online Travellers’ Diarrhoea Consultation to see if it is suitable for us to prescribe you standby Travellers’ Diarrhoea treatment.
The best protection are preventative measures such as drinking bottled or purified water, washing your hands thoroughly and frequently and eating well-cooked, hot food.
Fore more information on Travellers’ Diarrhoea.
CLIMATE HEALTH
Saudi Arabia has had some of the hottest temperatures on record this year. Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes which can cause rapid dehydration. This can result in heat exhaustion or heat stroke which can be life threatening if not dealt with promptly.
Heat related illness can be avoided by the following:
- Seek shelter and shade during the middle of the day (11am-3pm) when temperatures are the hottest
- If you are outside, ensure you protect your skin against the sun with high factor sun cream
- Wear loose fitting, lightweight and light colour clothing
- Keep hydrated by drinking plenty of fluids
- Ensure you are taking sufficient salt in your diet (sweating leads to electrolyte and salt depletion)
- Avoid caffeine and alcohol, which can worsen heat related illnesses
GENERAL HEALTH:
Both Hajj and Umrah pilgrimages require strenuous effort, it is worth considering having a full body medical check up before you travel to ensure you are in good health. To prepare for the miles of walking, try increasing your physical activities to improve mobility and movement. In case of unforeseen circumstances, remember to pack a first aid kit and extra supplies of any prescribed medication you are currently taking. We have an onsite pharmacy if you’d like to purchase any of these items during your appointment, speak with your GP or nurse whilst at the clinic.
DENGUE AND MALARIA:
Dengue is spread by day-biting mosquitoes and Malaria by mosquitoes that are active at night. You can reduce your risk of insect bites by using effective insect repellents and protective clothing. You can also sleep under a mosquito net that is impregnated with insecticide to have a peaceful sleep.
If you require complete protection from bugs and mosquitoes, you can check out our ultimate bug kit here.
Delaying your period:
If you decide you would like to delay your period for pilgrimage, you can do so by taking hormonal medication. In advance of your trip, book an appointment with a GP to discuss your options as soon as possible.
When you get home:
If you return home unwell it is important to book an appointment with a GP to determine the cause. If your symptoms worsen or becoming life-threatening do not wait to see a doctor, go straight to A&E for urgent medical care.
If you return with a stomach bug or persistent travellers’ diarrhoea, you may want to consider booking a Gastrointestinal (GI) Panel PCR test – it looks for any microbes (bacteria, viruses & parasites) that may be causing your symptoms and can quickly identify the exact cause. Results can be provided in as little as 1-hour, so that accurate and effective treatment can begin straight away. Firstly, you need to book a GP appointment, express your interest in a GI PCR test and they will advise whether you are suitable or not.
As a leading private occupational health provider in London, Fleet St. Clinic is pleased to see the recent developments in UK Government policies regarding occupational health services.
The latest Budget announcement in March 2023 included the launch of a new occupational health subsidy pilot program with tax incentives proposal. This government program is aimed at supporting small and medium-sized enterprises (SMEs) in England with the cost of purchasing occupational health services to improve the health and wellbeing of their employees. This is part of the government’s focus on improving employee health and wellbeing and reducing absenteeism.
The proposed tax incentives for businesses that invest in occupational health services are a welcome development. As many London-based businesses are struggling with the ongoing challenges of the pandemic, it’s important to recognise the importance of maintaining the health and wellbeing of the workforce. This program will incentivise businesses to prioritise employee health, which will have positive impacts for both the employee and the business as a whole.
Employer-led occupational health services can reduce health-related inactivity by identifying, monitoring and preventing health problems in the workplace, supporting employees to remain healthy and happy in work. Around half of UK employees currently have access to occupational health services, which is lower than some international comparators.
In addition to the proposed tax incentives, there have been calls to make occupational health services tax-exempt. This would further encourage London-based businesses to invest in occupational health services from providers such as us, Fleet St. Clinic, and support the growth of businesses in the UK. It would also make it more accessible for businesses of all sizes to access these services to improve the health and wellbeing of their employees.
The focus on occupational health has also been highlighted by the John Lewis Partnership, which has launched a new initiative called “Working Well” aimed at improving the mental health and wellbeing of its employees. This is a great example of a business taking proactive steps to support the health of its workforce, and it is encouraging to see more businesses in the UK following suit.
It’s important to note that occupational health services from Fleet St. Clinic aren’t just about responding to workplace injuries and illnesses. They can also be proactive in preventing health issues from arising in the first place, such as through health screenings, workplace medicals, health promotion programs, and ergonomic assessments. These preventative measures sit alongside more formal methods of occupational health services such as management referrals and mandatory health surveillance.
By investing in occupational health services in London, businesses can reduce absenteeism, increase productivity, and create a healthier and happier workforce.
The recent announcement about plans to expand occupational health services and workforce is also a positive development for businesses in London. This will help to address the shortage of occupational health professionals and ensure that businesses can access the high-quality services they need from providers like Fleet St. Clinic to support the health and wellbeing of their employees.
One potential barrier to accessing all occupational health services in the UK is the value-added tax (VAT) that is currently applied to some services that are seen as screening services rather than services that support the health and wellbeing of the employee. However, there have been further discussions about exempting all occupational health services from VAT, which would make them more affordable and accessible for businesses of all sizes.
In conclusion, as a leading private occupational health provider in London, Fleet St. Clinic is pleased to see the recent developments in government policies and business initiatives regarding occupational health. The focus on supporting SMEs, tax incentives, and VAT exemptions will make it easier for London and England-based businesses to access the services they need to maintain the health and wellbeing of their workforce. It is important to remember the potential benefits of investing in occupational health services from providers such as Fleet St. Clinic, London and the positive impact they can have on both employees and businesses.
If you’d like to start the conversation about how we could support your employee’s health, fill out the form below and we’ll propose suitable services for your consideration.
Related services available at Fleet Street Clinic
Continued reading about the new UK Government Occupation Health Budget Proposals:
Tax exemptions for employer health related interventions
Research & Analysis Report: Incentivising SME uptake of health and wellbeing support schemes
The UK is currently facing a rapidly escalating diabetes crisis.
What does that mean?
According to a recent report published by Diabetes UK, more than 5 million people are living with diabetes in the UK, and the number is only increasing. This figure is a combination of those who have been diagnosed with diabetes and an estimate of those who are currently unaware that they are diabetic.
As a private healthcare clinic in London, Fleet St. Clinic is committed to providing support and the highest quality of care to all our patients, especially those affected by this escalating crisis.
Diabetes is a chronic condition that affects how your body regulates blood sugar. There are two main types of diabetes:
Type 1 – which is usually diagnosed in childhood and is caused by the immune system attacking the cells in the pancreas that produce insulin,
Type 2 – which is usually diagnosed in adulthood and is caused by the body becoming resistant to insulin or not producing enough insulin.
Diabetes UK’s report shows that 4.3 million people have been diagnosed with diabetes in the UK. We know that approximately 90% of these diagnoses are of type 2 diabetes, and around 8% of diagnoses are type 1 diabetes, with the other forms of the condition making up the remaining 2% including gestational, neonatal, and monogenic diabetes.
In addition, Diabetes UK also estimates there are an additional 850,000 people living with diabetes who are yet to be diagnosed, bringing the overall UK-wide figure beyond 5 million.
Year-on-year the numbers for diabetes are increasing, a worrying trend, especially as most of the diagnosis are for type 2. Diabetes UK’s report states that 2.4 million people in the UK are considered at high-risk of developing type 2 diabetes and could already be pre-diabetic.
All types of diabetes can lead to serious complications, including heart disease, stroke, kidney disease, nerve damage, and blindness. With the right treatment and management, many people with diabetes can live full and active lives.
What are the symptoms of diabetes?
The 4Ts of diabetes include:
- Thirsty
- Tired
- Toilet (needing to urinate a lot, especially at night)
- Thinner (losing weight without trying)
At Fleet St. Clinic, we offer a range of services to support patients with diabetes, including regular check-ups, blood sugar monitoring, and dietary advice. Our team of experienced healthcare professionals, including doctors, nurses, and dietitians, work together to provide personalised care tailored to each patient’s needs.
Diagnosing Diabetes:
Our most non-invasive test is the instant HbA1C test which can be a standalone appointment with a nurse or suggested by your doctor during a GP appointment. This test is used to diagnose diabetes and only requires a finger prick of blood. It takes about 6 minutes to receive results meaning you can have the test and receive the result during your consultation.
We also offer specialist services for patients with diabetes-related complications, such as foot ulcers, which can be a serious problem for people with diabetes. Our podiatrist can provide expert advice and treatment to help prevent and manage foot ulcers, which can lead to amputation if left untreated.
Diabetes can have a major effect on your eye health and greatly increase your risk of certain eye conditions, so if diagnosed, it is very important that you have your eyes checked regularly. Our sister clinic, Whitby & Co. Optician, is also based at 29 Fleet St. London and offers eye examinations which include an OCT scan. OCT scans can be useful to diagnose and monitor diabetic eye conditions such as diabetic retinopathy.
In addition to our clinical services, we also offer support to help patients with diabetes manage their condition. Our doctors and dietitian can discuss topics such as healthy eating, exercise, and medication management with you.
At Fleet St. Clinic, we understand that living with diabetes can be challenging, but we are committed to providing the highest quality of care and support to our patients.
So, if you are living with diabetes or are at risk of developing the condition, please don’t hesitate to get in touch with us. We’re here to help you manage your diabetes and live your best life.
Read the full report by Diabetes UK
Diabetes UK: “Know your risk” online tool
Related Services at Fleet St. Clinic
Much like getting fit, improving posture is a long term game. Trying to stand or sit up straight when you remember isn’t really going to cut it. First of all, you obviously forget, but secondly, using those big mobility muscles to pull you upright causes them to tire quickly and build up lactic acid, at which point you slump for quick comfort.Many things can be causing bad posture and pain, so it’s worth getting it assessed first. Even if there’s no major problems but it’s been happening for a while, some mobilisation, adjustment and tailored exercises may well be needed.To help posture long term we need to do two things:
Change the habits encouraging bad posture, and get the right muscles to do the job.
Try to identify when posture is bad. If it’s sitting at a desk/computer, get the desk assessed and altered. If it is slouching on the sofa, sit upright, bottom to the back of the seat, maybe a cushion in the small of the back, feet on the floor. Be aware of looking at phones for too long. Read my full blog here on how to set up your workstation properly. Using and strengthening correct muscles to hold your posture is equally important. The postural muscles are designed to hold you in a better position with less effort for much longer without tiring. If you are nicely upright and relaxed your head is largely balanced on top of your spine. Just a little angle forward (to look at your phone for instance) or slumping, and suddenly it takes a huge muscle effort to hold it up. To get these postural muscles working and strengthened can be a little tricky at first as you try to co-ordinate them. I often suggest something like Pilates or the Alexander Technique, but even just doing more core stability exercises in the gym or at home will help.
Osteopathy can treat a vast array of joints and musculoskeletal issues of the body caused by poor posture, including:
- Non-traumatic back pain including lumbago and sciatica pain management
- Stress-related musculoskeletal problems
- Neck pain & headaches including migraine prevention
- Pregnancy-related musculoskeletal problem
- Postural-related problems including shoulder, hip, knee and/ or ankle pain
- Workstation-related problems
- Restricted Mobility
If you’d like to understand the underlying causes of your pain and discomfort and a personalised treatment plan for recovery, book an osteopathy appointment.
___________________________________
OSTEOPATHY AT FLEET STREET CLINIC
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC).
Book an appointment with him if you have any musculoskeletal injuries by calling +44 20 7353 5678, email info@fleetstreetclinic.com or book an appointment online.
As a travel nurse based in London, I was concerned to hear the recent warning from health officials about the spread of tick-borne encephalitis (TBE) virus in several parts of the country. The UK Health Security Agency (UKHSA) has confirmed three cases of TBE virus in patients in Yorkshire, Norfolk, and on the border of Hampshire and Dorset. Further tests on ticks across the country have found that the disease, which was commonly found in parts of Europe and Asia until now, is now present in the UK. The experts have warned that it is unlikely that TBE virus will disappear, so it’s essential to establish a surveillance program.
Public health officials say the risk is low, but it’s essential for walkers to take precautions and seek medical help if they fall ill after being bitten, especially if by a tick.
As a clinic that specialises in travel, we are used to urging everyone to take precautions to protect themselves from tick bites anyway, but this news reinforces the importance of doing this at home as well as when travelling abroad. It is essential to cover your ankles and legs, apply insect repellent, and check clothes and your body for ticks, particularly when visiting areas with long grass such as woods, moorlands, and parks.
In most cases the TBE virus typically causes mild flu-like symptoms, but it can also lead to severe infection in the central nervous system resulting in meningitis or encephalitis a high fever with headache, neck stiffness, confusion, or reduced consciousness, and long-term impairment.
As a travel nurse, I think it is really important to educate people about the symptoms of TBE to encourage them to seek medical help immediately if they experience any of these symptoms, but also to emphasise the fact that infections are preventable.
Ticks are becoming more common in parts of the UK, mainly due to increasing deer numbers. They live in undergrowth and latch on to humans when they walk through long grass. It is thought infected ticks may have arrived in the UK via migrating birds. Scientists had suspected the virus had arrived in the UK in 2019, following a couple of cases, but complexities involved in testing meant these could not be confirmed.
It’s crucial to emphasise the significance of vaccination for individuals who are considered of a higher risk. You are much more likely to catch TBE if you work outdoors or if you enjoy outdoor activities such as camping, hiking, dog-walking, countryside rambling and even jogging. Children playing outside may be especially vulnerable.
Vaccines can provide protection, and as there is currently no known cure for tick-borne encephalitis virus, those individuals who would be considered at higher risk are advised to be vaccinated as a precaution.
It’s worth noting that a vaccine is used routinely in areas of high incidence in Europe, and its advisable to consider vaccination for individuals with outdoor occupations in regions where the virus is prevalent.
For the general public the risk of contracting TBE is relatively low. Therefore, it’s essential to educate people about TBE and encourage them to take precautions to protect themselves from tick bites, particularly when travelling to areas where the virus is found.
Related services available at Fleet Street Clinic
Tick Borne Encephalitis Vaccination
For further reading, more news coverage can be found here:
Gov.uk – Tick Borne Encephalitis detection in England
The Times – Tick-borne encephalitis warning to walkers
The Telegraph – First cases of rare tick disease found in England
Dengue Fever has been in the news following two cases linked to travel to the Spanish island of Ibiza. This has sparked concerns about the spread of mosquito-borne illnesses in Europe, which is especially unusual for this time of year.
Dengue fever is a viral infection transmitted by the Aedes mosquito, which is found in tropical and subtropical regions worldwide. With rising temperatures and changing climates, there is a risk of mosquitoes and other disease vectors spreading to new areas, potentially causing outbreaks of diseases such as dengue fever.
The two cases of dengue fever in Ibiza were reported by the Spanish Ministry of Health and were both in residents of Germany who had visited the island before becoming ill. Each case was accompanied by two family members who were also suspected to have had dengue fever.
The risk of dengue fever in Spain is highest between the months of May and November, when mosquitoes are most active so to have cases at this time of year is uncommon.
So, why are we seeing cases outside of the usual infection months?
The reason is multi-facetted.
Our medical director and travel health specialist, Dr Richard Dawood explains:
“Firstly, there is the introduction or spread of mosquitoes to “pastures new” – places that might have been previously inhospitable, perhaps through temperature; or alternatively, that offer an environment with plenty of suitable breeding sites that they are suddenly able to take advantage of. These mosquitoes can bring disease with them, or can spread it around if there is a reservoir in the local population.
Secondly, there is the possibility of introducing disease to a vector population that is already established, ready and waiting. This is exactly the (long-standing) concern with yellow fever. There are mosquito species in Asia, for example, that are easily capable of spreading yellow fever were it to be introduced by an infected traveller – which is why Asian countries are so careful to insist on proof of yellow fever vaccination from travellers arriving from the endemic zones of Africa and South America. Asia is yellow fever-free, and wants to remain so. However, this type of introduction has already recently happened in Australia, where Japanese encephalitis (a virus infection that can cause rare but serious complications in humans) has recently established a reservoir of infection in farm animals, that may be impossible to reverse. It is also happening with Lyme disease spreading gradually into parts of Europe (and the UK) with a susceptible tick population.
Similar concerns apply to Zika – there is very large potentially susceptible mosquito population that could spread the virus in many tropical countries, if introduced; dengue fever; and also potentially malaria, in parts of the world that have been the target of successful elimination campaigns, but where mosquito populations could still spread it, were it to be reintroduced, if control measures are neglected or ceased.
With changing climates, a valid concern about global warming is that it could create conditions in which populations of mosquitoes and other vectors thrive and spread – hence the crucial importance of vigilance, surveillance, and early action if needed.”
How can you protect yourself from Dengue Fever?
QDENGA, Dengue Fever Vaccination
Relatively new to the UK, QDenga is a new travel vaccine that can prevent dengue fever.
The course consists of two doses, given three months apart, and provides long lasting protection.
Learn more about QDENGA, Dengue Fever Vaccination
Book a travel consultation for your Qdenga vaccination.
Avoid Mosquito Bites
In addition to vaccination, the best way to protect yourself against dengue fever is to take measures to avoid mosquito bites. This includes wearing protective clothing, using mosquito repellent, and staying in places with air conditioning or screens on windows and doors.
If you develop a high fever during or after travelling to an affected area, seek medical advice as soon as possible and provide details of your recent travel history. Dengue is often also accompanied by a rash and joint or muscle pain.
In conclusion, rising temperatures and changing climates have the potential to create conditions in which populations of mosquitoes and other disease vectors thrive and spread. It is crucial for public health authorities to remain vigilant and take early action if needed to prevent the spread of diseases such as dengue fever.
By receiving the Qdenga vaccine and implementing effective measures to prevent mosquito bites, travellers can lower their personal risk of contracting Dengue Fever, along with other insect-borne diseases.
If you’re considering Qdenga before your next trip, book a travel consultation with one of our specialist travel nurses.
Related services available at Fleet Street Clinic
QDENGA, Dengue Fever Vaccination
Suitable Medical Kits available to buy online
Related Online Consultations
Female Travel Health Kit: Start Consultation
SPRING IS UPON US!
A time of longer days, shorter nights, flowers in bloom, and warmer weather allowing us to spend much more time enjoying the great outdoors.
This year, March 26th marks the start of British Summer Time when the clock springs forward 1 hour, increasing daylight, prolonging our evenings and our transition to Summer begins.
Spring is the time of year when we emerge from our winter hibernation and seek more time in the fresh air, the outdoors, in nature and with friends and family.
There are so many health benefits that Spring has on our physical and mental well-being.
But in what ways specifically is Spring good for our health?
1. Spring makes us feel more energised
There’s nothing quite like the feeling of the warm sunshine on our skin after a long, cold winter.
This small act of nature, in general, makes us feel more upbeat and positive and can quite literally give us a “spring in our step!”. Exposure to natural light is thought to increase the brain’s release of a hormone called serotonin. Serotonin is associated with boosting mood and helping a person feel calm and focused with a more optimistic outlook to life.
With sunlight and sunshine increasing, spring is a natural positive energiser.
2. Spring weather encourages us to be more active
With the weather improving and the temperature rising it encourages us to get outdoors and be more active. That doesn’t mean we’re all inspired to run a marathon, but time outdoors is good for your physical and mental health.
Time in the fresh air can really help you to switch off from your daily stresses, reduce your blood pressure and improve your mood.
Spring encourages us to take up a new sport, go out for walks and spend more time being active.
3. Spring sunshine tops up our vitamin D
Getting enough vitamin D is essential for the typical growth and development of our bones, teeth and muscle health, as well as improving our resistance to certain diseases.
Extra daylight gives you more time to spend outside and soak up the nutrients from the sunshine. In Spring and Summer, most people are able to make all the vitamin D they need from the sunlight on their skin without the need for supplements.
4. Spring encourages us to clean our home
Spring is the perfect time of year to air out our homes, clean out the grime that has built up over the winter and make a fresh, clean start.
There are many health benefits to giving your house a deep spring clean, such as:
- Reducing your risk of allergies and asthma from the accumulation of dust or pet dander.
- By removing germs and bacteria, especially from hard-to-reach places, you are reducing your risk of getting sick in general.
- Visual clutter leads to mental clutter; so, doing a big tidy-up should see improvements in your mental health and even increase your productivity.
Is it time to spring clean your health?
Related services available at Fleet Street Clinic.
Cholesterol is a type of fat that is found in the blood and plays an important role in our bodies. However, high levels of cholesterol can lead to serious health issues, such as heart disease, stroke, and other cardiovascular problems. Unfortunately, cholesterol is often referred to as a “silent killer” as there are usually no symptoms and the first indication that something is wrong may be a heart attack. That’s why it’s important to have your cholesterol levels checked regularly.
Instant cholesterol testing only requires a short nurse appointment that provides you with both the test and the results during the same appointment. This type of testing makes it easy and convenient for people to understand their cholesterol levels and take steps to keep them under control.
Statistics from the National Institute for Health and Care Excellence (NICE) show that cardiovascular disease (CVD) is the leading cause of death in the United Kingdom, accounting for around 26% of all deaths. The most common type of CVD is coronary heart disease, which is caused by a build-up of fatty deposits in the arteries leading to the heart. High cholesterol levels can contribute to the formation of these fatty deposits.
By knowing your cholesterol numbers through instant testing, you can understand your risk of developing CVD and take the necessary steps to keep your levels under control. NICE recommends that all adults in the UK should have their cholesterol levels checked at least once every five years, or more frequently if they are at increased risk of CVD. Those at increased risk include people with a family history of CVD, smokers, people with high blood pressure, and people with diabetes.
To keep your cholesterol levels under control, it is important to make changes to your diet. This includes eating more fruits, vegetables, whole grains, and lean proteins, and reducing your intake of saturated and trans fats. You should also aim to maintain a healthy weight and be physically active for at least 30 minutes a day.
If lifestyle changes are not enough, medication may be required. The most common type of cholesterol-lowering medication is statins, which work by reducing the production of cholesterol in the liver. Statins are widely used in the UK and are safe and effective.
The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
Further reading on “NICE recommends wider use of statins for prevention of cardiovascular disease (CVD)”.
In conclusion, instant cholesterol testing provides an easy and convenient way to understand your cholesterol levels and take steps to keep them under control. Regular testing is important for everyone in the UK, especially those who are at increased risk of CVD. By knowing your numbers, making changes to your diet, maintaining a healthy weight, and being physically active, you can help keep your cholesterol levels in the healthy range and reduce your risk of developing serious health problems.
Related services available at Fleet Street Clinic:
Instant Cholesterol Testing with a nurse
Blood Tests at Fleet St. Clinic
Well Person Medical
GP Services
As a private healthcare clinic, our goal is to provide the best protection against pneumonia for our patients. One of the key tools in this fight is the pneumococcal vaccine. One of the latest advancements in this area is the Apexxnar vaccine. This 20-valent vaccine provides protection against 20 different serotypes of the pneumococcal bacteria, offering a more comprehensive defence against pneumonia.
We understand that choosing the right vaccine can be complex and that different patients may require different solutions. That’s why we recommend speaking with one of our healthcare providers to determine which vaccine, including Apexxnar, is best for you. They will consider risk factors such as your age, underlying health conditions, and previous vaccinations, to ensure you receive the most effective protection against pneumonia.
At Fleet St. Clinic, we believe in the power of prevention, and that the right vaccine can make all the difference. So, if you’re looking for the best defence against pneumonia, consider talking to us about the Apexxnar vaccine today.
Information about Pneumonia:
Pneumonia is a lung infection that can cause a range of symptoms, including:
- Cough: A persistent cough that produces mucus or phlegm is a common symptom of pneumonia. The cough may be dry or productive, and the mucus or phlegm may be green, yellow, or rust-coloured.
- Fever: Pneumonia often causes a high fever, which may be accompanied by chills and sweats.
- Shortness of breath: Pneumonia can cause difficulty breathing, especially during physical activity. The shortness of breath may be accompanied by chest pain or tightness.
- Fatigue: Pneumonia can cause extreme tiredness and weakness, making it difficult to carry out normal daily activities.
- Muscle aches: Pneumonia can cause muscle aches and joint pain, which may be mistaken for the flu.
- Chest pain: Pneumonia can cause chest pain, especially when breathing deeply or coughing.
- Nausea and vomiting: Some people with pneumonia may experience nausea and vomiting, especially if the infection is caused by a type of bacteria known as Legionella.
- Confusion or disorientation: Pneumonia can cause confusion or disorientation, especially in older adults and people with underlying health conditions.
It’s important to seek medical attention if you experience any of these symptoms, as pneumonia can be a serious and potentially life-threatening condition.
More information on pneumonia.
Who is considered “high-risk”?
Individuals considered to be at high risk for hospitalisation due to pneumonia include the elderly, young children, people with weakened immune systems (including people who have had their spleen removed), and individuals with underlying health conditions such as chronic heart or lung diseases, diabetes, and liver or kidney problems.
At the Fleet St. Clinic, we also regard anyone who has had a previous significant episode of pneumonia as likely to benefit from being vaccinated.
When is the best time for a pneumonia vaccine?
The best time to vaccinate against pneumonia depends on various factors such as the type of vaccine, the individual’s age, and underlying health conditions.
The pneumonia vaccine is not the same as the flu vaccine, as it doesn’t need to be given at a certain time of year.
For the pneumococcal vaccine, it is generally recommended to receive the vaccine once in a lifetime for most adults. Some individuals may need a booster shot, and this is determined by a healthcare provider such as a doctor or nurse.
How to book an appointment?
Booking an appointment is easy. If you are on the go, you can book online through our online booking system, pre-payment is required.
If you would like to discuss anything further or would like to book with our reception team, you can call them on +44 207 353 5678 or email us at info@fleetstreetclinic.com
Related services available at Fleet Street Clinic:
Ovarian cancer is a disease that affects thousands of women worldwide each year and is often referred to as the silent killer due to its silent symptoms, including bloating, abdominal pain, and changes in bowel habits, which are often mistaken for other conditions. Despite advances in treatment, the disease remains a major public health concern due to its high mortality rate. However, new data from a study funded by Cancer Research UK (CRUK) suggests that a seemingly unlikely tool – supermarket loyalty card surveillance – could help spot ovarian cancer early, when it is most treatable.
The study, which was published in JMIR Public Health and Surveillance, analysed data from supermarket loyalty card programs and found that changes in purchasing behaviour could be used to detect early signs of ovarian cancer.
Researchers found that women with ovarian cancer often experience a decline in their appetite and energy levels, which can result in changes in their grocery shopping habits. By monitoring these changes in real-time, it may be possible to detect the disease early and improve the chances of successful treatment.
This is an exciting development in the fight against ovarian cancer, and one that has the potential to revolutionise the way we detect and treat the disease. By leveraging the vast amounts of data generated by supermarket card programs, healthcare providers and public health officials could identify women who may be at risk of ovarian cancer and encourage them to seek early medical attention. This could help to improve the outcomes of treatment and reduce the overall impact of the disease on society.
One of the key benefits of supermarket card surveillance is that it allows for continuous monitoring of women’s purchasing behaviour. This means that healthcare providers can receive real-time alerts when changes occur, allowing them to act quickly and effectively. This level of monitoring is not possible with traditional screening methods, which are typically performed only once or twice per year and may miss early signs of the disease.
Additionally, supermarket card surveillance is a cost-effective way to monitor the population for signs of ovarian cancer. Unlike other screening methods, it does not require specialised equipment or trained personnel, and the cost of monitoring is negligible compared to the cost of treatment. This could make it possible to implement large-scale screening programs, even in resource-limited settings, and reach a greater number of women who may be at risk of ovarian cancer.
Of course, it’s important to keep in mind that supermarket card surveillance is not a substitute for traditional screening methods, such as ultrasound or CA-125 tests, or for regular self-reporting and awareness of symptoms. However, it could be used as an adjunct to these methods, helping to improve the accuracy of screening and reduce the number of missed cases.
Another important consideration is the privacy of women whose purchasing behaviour is being monitored. While supermarket card surveillance has the potential to help detect ovarian cancer early, it is important to ensure that women’s privacy is protected and that the data collected is used only for medical purposes. Healthcare providers and public health officials should work together to ensure that any monitoring programs are transparent, secure, and in compliance with privacy regulations.
In conclusion, the findings of this study are a major step forward in the fight against ovarian cancer. By leveraging supermarket card surveillance, it may be possible to detect the disease early, when it is most treatable, and improve the outcomes of treatment for women around the world. However, it is important to carefully consider the privacy implications of monitoring purchasing behaviour and to ensure that any programs implemented are transparent, secure, and in compliance with privacy regulations. The early detection of ovarian cancer is a critical goal, and we hope that this research will help to pave the way for new and innovative approaches to screening and treatment. Additionally, women should be encouraged to seek medical attention if they notice any changes.
Reference Source: https://publichealth.jmir.org/2023/1/e41762
Related services available at Fleet Street Clinic:
Is there such a thing as testing too early for STIs?
Yes, in fact, if you test too soon after exposure to an STI aka during the “window period”, you may not get an accurate result.
The ‘window period’ is the length of time it can take between catching an infection and when it will show in a test. It’s important to note that if you are tested earlier than the “window period”, some tests may not detect the STI, even though an individual is infected.
The timing of STI testing after potential exposure varies depending on the specific infection. In general, it is best to wait until a sufficient amount of time has passed for the infection to be detectable, but not so long that the infection has already caused damage.
The “window period” for common STIs:
Chlamydia and Gonorrhoea
– These bacterial infections can be detected 2 weeks after exposure. Symptoms can appear before this so those with symptoms shouldn’t delay testing.
HIV
– Antibody tests can be taken 4 weeks after exposure, whilst instant antibody tests are suitable for use 90 days post contact. Early detection RNA tests can be taken from 10 days after potential exposure. Your healthcare provider will be able to advise which test is most suitable for you.
Syphilis
– Antibody tests for syphilis can be detected 12-weeks after a suspected exposure. Symptoms can appear before this so those with symptoms shouldn’t delay testing, as alternative tests can be taken to diagnose.
If you have been exposed to an STI and are concerned about potential infection, it is recommended to have a sexual health consultation at the earliest opportunity. Your healthcare professional will be able to discuss your risk factors, and then advise the appropriate time interval for tests based on the type of test being used. Your healthcare provider can help you determine which test is right for you, and when to get tested. They will discuss this with you during your sexual health consultation.
It is important to note that some STIs, such as herpes and human papillomavirus (HPV), can have no symptoms, so it is possible to have an infection and not know it. Regular STI testing is the only way to diagnose and treat an infection early, which can prevent complications and reduce the risk of transmission to others.
If you have been sexually active and have concerns about potential STI exposure, it is best to consult with a healthcare provider. They can help you determine the best course of action, including when to get tested and which tests to have.
What STIs can we test for?
Fleet St. Clinic offers testing and treatment for several different STIs including:
– HIV
– Gonorrhoea
– Syphilis
– Chlamydia
– Herpes
– HPV – Genital Warts
Additional tests for symptomatic patients include:
– Mycoplasma
– Ureaplasma
– Trichomoniasis
Results
Rapid results are available for most of our STI checks meaning we can provide you with answers on the same day as your tests. Most swabs are analysed within our onsite laboratory so we can provide you with answers as soon as possible.
Remove unnecessary worry by selecting our fastest turnaround times. These vary for each type of STI, so discuss this with your nurse or doctor during your sexual health consultation.
How regularly should I be getting tested?
Getting tested for sexually transmitted infections (STIs) is an important part of maintaining sexual health. There is no one-size-fits-all answer to when to get tested, as the frequency and timing of STI testing depend on several factors, including:
1. Sexual behaviour: Individuals who engage in higher-risk sexual behaviours, such as unprotected sex, multiple sexual partners, or sexual contact with someone who has an STI, should get tested more frequently.
2. Personal health history: Individuals who have a history of STIs or other health conditions that affect sexual health should get tested more frequently.
3. Age: Young people and older adults may be at higher risk for STIs and should consider getting tested more often.
4. Pregnancy: Pregnant women should be tested for STIs during their first prenatal visit, as well as any other time during their pregnancy as recommended by their healthcare provider.
It is also important to note that some STIs can have no symptoms, so it is possible to have an infection and not know it. Regular STI testing is the only way to diagnose and treat an infection early, which can prevent complications and reduce the risk of transmission to others.
Related services available at Fleet Street Clinic:
HIV (Human Immunodeficiency Virus) is a viral infection that damages cells in your immune system. As a result, it weakens the body’s ability to fight off everyday infections such as the common cold. If you have HIV and get sick with a cold, you are much more likely to experience complications, such as developing pneumonia.
HIV is found in the body fluids of an infected person, such as semen, vaginal and anal fluids, blood and breast milk. It is not found in sweat, urine or saliva. Meaning HIV is typically spread by unprotected sex, the sharing of injecting equipment such as needles, and/ or passed from mother to baby either through birth or breastfeeding.
About National HIV Testing Week
National HIV Testing Week #HIVTestWeek aims to raise awareness of HIV and AIDS. It is an annual national campaign to encourage people to get tested for HIV regularly to reduce the number of people who are diagnosed late or remain undiagnosed.
Out of the 106,890 people in the UK with HIV, 1 in 20 of those do not realise they are HIV positive. Which is why it is so important to make sure everyone gets tested to know their status.
Data from 2019, revealed that 42% of people were diagnosed late. A late diagnosis significantly increases the risk of the virus seriously damaging your health, not to mention the fact that you are more likely to pass the virus on during the period when you are unaware of a positive diagnosis. The only means to address this issue is to increase awareness of the importance of HIV testing.
If you have HIV for a long time without knowing, it can damage your health and shorten your life expectancy. It’s a good idea to test at least once a year (or more if you have unprotected sex with more than one partner). Early detection can give you a better quality of life and reduce the spread of the disease.
While there is no ‘cure’ for HIV, thankfully there are now very effective treatments available that allow those who are HIV positive to live a healthy life and have a normal life expectancy. There is also emergency treatment available if you have been exposed to HIV within the last 72 hours (PEP). Additionally, there is medication available to prevent contracting HIV (PrEP) and even a tablet that will prevent you passing the virus on to anyone else. Access to these treatments is available to anyone HIV positive but the only way to know your HIV status is to get tested.
Know Your Status
At Fleet Street Clinic, we have two types of HIV tests available: an instant test and a blood test. An instant HIV test can provide you with results within a 15 minute nurse appointment. The test is a simple blood test done via a needle prick to the finger and is suitable for use 90 days post-exposure. It is a very simple process with extremely accurate results.
For HIV testing week we’re promoting our ‘So quick you can do whilst grabbing a coffee’ campaign to highlight just how quick an HIV test can be. We want to encourage all to make time to find out their HIV status.
Get Tested
We offer a number of HIV Tests, some of which can be performed in the clinic in just 15 minutes. You can be tested for HIV from as early as 28 days post-contact with a blood test, but don’t worry, during your appointment the clinician will let you know which test they recommend based on your history. Following an HIV test, we are on hand to offer guidance and referrals, should they be required.
Your privacy will be strictly protected.
You can book an HIV Test Online.
For more information on HIV you can visit our HIV page or HIV Prevention England.
Statins are a widely prescribed class of drugs used to lower cholesterol levels and prevent cardiovascular events such as heart disease and strokes. The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
This decision was made after the independent committee updating the NICE guideline on cardiovascular disease (CVD) risk assessment and reduction considered new evidence on the safety and side effects of statins, meaning more people could be given them.
The draft guideline recommends that doctors should consider statins for people who haven’t had a CVD event (called ‘primary prevention’) with a 10-year CVD risk score of less than 10%. The committee agreed that if more people took statins there would be a greater reduction in the incidence of heart disease and strokes.
In addition to being prescribed by National Health Service GP’s, statins can also be prescribed by private healthcare providers, such as us, Fleet Street Clinic. In fact, private GP’s can play an important role in the management of cardiovascular disease risk by offering statins as part of a comprehensive treatment plan for patients at high risk.
People can be at risk from CVD because of factors they cannot change including their age, sex, ethnicity and family history but it’s important to note that certain lifestyle changes can reduce the risk. These include stopping smoking, reducing alcohol consumption, introducing or increasing exercise and eating a healthy diet.
Therefore, the decision to take a statin should be made in consultation with a healthcare professional and should take into account the individual’s values and priorities as well as the potential risks and benefits of treatment.
With the British Heart Foundation noting that “there are around 7.6 million people living with heart and circulatory diseases in the UK” and that they “estimate that in the UK more than half of us will get a heart or circulatory condition in our lifetime” this is likely to be an impactful change in the landscape of CVD and statins.
To conclude, Paul Chrisp, director of the Centre for Guidelines at NICE, said:
“What we’re saying is that, for people with a less than 10% risk over 10 years of a first heart attack or stroke, the decision to take a statin should be left to individual patients after an informed discussion of benefits and risks.
“The evidence is clear, in our view, that for people with a risk of 10% or less over 10 years, statins are an appropriate choice to reduce that risk.
“We are not advocating that statins are used alone. The draft guideline continues to say that it is only if lifestyle changes on their own are not sufficient, and that other risk factors such as hypertension are also managed, that people who are still at risk can be offered the opportunity to use a statin, if they want to. They don’t have to, and their decision should be informed by an understanding of the risks and tailored to their values and priorities.”
Reference Source: https://www.nice.org.uk/guidance/indevelopment/gid-ng10178/documents
Related services available at Fleet Street Clinic:
Sleep plays a crucial role in maintaining overall health and well-being, and recent research has revealed a strong link between sleep and cardiovascular health. A study conducted by the University of Warwick in the UK found that individuals who get 7-9 hours of sleep per night have a lower risk of cardiovascular disease (CVD) and mortality compared to those who sleep less or more than the recommended range.
The study, published in the Journal of the American College of Cardiology, analysed data from over 116,000 participants in the UK Biobank study and found that those who slept less than 6 hours or more than 9 hours had a higher risk of CVD and mortality. These findings add to the growing body of evidence that suggests a link between sleep duration and cardiovascular health.
The exact mechanisms by which sleep affects cardiovascular health are not fully understood, but researchers suggest that it may be related to the impact of sleep on cardiovascular regulation, inflammation, and metabolic function.
It is important to prioritize sleep and aim for the recommended range of 7-9 hours to maintain cardiovascular health.
It’s worth noting that these findings are observational, and more research is needed to fully understand the relationship between sleep and cardiovascular health, but it’s a good indication that sleep plays a vital role in maintaining a healthy cardiovascular system.
To read the full study, continue reading here:
medscape.co.uk – Does sleep duration influence cvd and mortality risk?
Related services available at Fleet Street Clinic:
Travelling can have a significant positive impact on one’s physical and mental health, according to a study published in the Journal of Travel & Health. The study surveyed over 1,000 adults who had recently returned from a trip and found that the majority of them reported improvements in overall well-being, including increased energy and reduced stress levels.
One of the key reasons for these self-rated health benefits is that travelling allows individuals to step out of their daily routine and experience new environments and cultures. This can lead to increased physical activity, as travellers may be more likely to walk or bike instead of drive which may also expose them to different types of food, leading to a healthier diet.
Additionally, travelling can have a positive impact on mental health as well. The study found that the majority of participants reported feeling more relaxed and less stressed after their trip. This is likely because travelling can provide a sense of excitement and adventure, as well as a break from the demands and responsibilities of everyday life.
Another benefit of travelling is that it allows individuals to build new social connections, which can be important for mental health. Meeting new people and forming new friendships can provide a sense of belonging and can also help to reduce feelings of loneliness and isolation.
In conclusion, the study suggests that travelling can be good for one’s physical and mental health. It can help to increase energy levels, reduce stress and improve overall well-being. So, next time you are planning a trip, remember it’s not only good for your soul but also for your body.
To read the full study, continue reading here: https://www.sciencedirect.com/science/article/pii/S2214140522002079?via%3Dihub
Related services available at Fleet Street Clinic:
- Travel Vaccinations
- Jet Lag Calculator
- Travellers’ Diarrhoea Online Consultation
- Antimalarials
- DVT Rick Calculator
Chinese New Year is a festival celebrated annually by Chinese communities across the world to bring good luck and prosperity into the New Year. Every year corresponds with one of the 12 animals in the Chinese Zodiac, with 2023 being the Year of the Rabbit. Celebrations for Chinese New Year kick off on the 22nd Jan, continuing until the 5th February where the festivities culminate with the Chinese Lantern Festival. Every year, thousands of people travel to China to enjoy the celebrations. So, if you are one of those people who are planning to travel to China to join in with the festivities, please ensure you follow these tips to stay healthy whilst abroad.
Firstly, you may want to check the entry requirements for China in terms of required covid-19 testing. If you travel to China after 8th Jan, you would require a negative Covid-19 test and submit your negative result by filling a Health Declaration Form via China Custom Website or their app or WeChat account. You would also need a pre-departure Covid -19 test when coming back to England from China. If you are still travelling to China you can view what covid-19 testing entry rules are currently in place here: GOV.UK WEBSITE. You can find more information on our rt-PCR Testing service here and our Lateral Flow Testing here.
Covid aside, check your vaccination history. All travellers need to ensure they are up-to-date with their childhood vaccines, most importantly, Hepatitis A, Typhoid, Measles, Mumps and Rubella (MMR), and Diphtheria, Tetanus and Polio (DTP).
More information on our wellness vaccinations can be found here.
It is worth noting that it is still influenza season in the northern hemisphere and transmission can occur well into spring. Those travellers who haven’t received their annual flu vaccination to protect them against the most common strains for 2022-23, should ensure they receive it before travelling to China. You can still book your annual flu vaccine, here.
Travellers who are planning extended stays, and more remote and rural travel may also wish to consider vaccinations against Rabies and Hepatitis B.
More information on our travel vaccinations can be found here.
Those who are heading further south to rural areas where the weather is warmer may wish to consider vaccination against Japanese Encephalitis (JE), which is spread via the culex mosquito. You can also purchase our ‘Ultimate Bug Kit’ which will help protect you from mosquito bites.
There have been recent cases of Avian Influenza (bird flu) in both the UK and China. Bird flu is a very unpleasant illness which can cause people to fall quite unwell. It is passed on via contact with infected birds. Travellers can minimise risk by avoiding contact with any birds (dead or alive): avoid touching dead or dying birds, and steer well clear of ‘wet markets’ (marketplaces that sell meat, fish, and often live animals including birds).
Chinese New Year is heavily focused on food, with items such as fish, fruit and dumplings symbolising luck, wealth and prosperity. Travellers should ensure that they maintain good food and water practises to avoid tummy trouble whilst away. You should avoid tap water and ice made from tap water, instead stick to bottled water. Ensure you wash your hands thoroughly before eating and after using the toilet. Ensure all food that you eat is cooked thoroughly and served straight to you. And lastly, consider taking medicines for self-treatments with you, such as antibiotics – take our Online Travellers’ Diarrhoea Consultation to see if it is suitable for us to prescribe you standby Travellers’ Diarrhoea treatment.
By following these guidelines and ensuring you are generally sensible and hygienic, you will be able to relax and enjoy the sheer joys of travel and seeing the world.
Happy Chinese New Year!
You can book online for a travel consultation appointment here.
Or for more information on all of our travel vaccinations, wellness vaccinations or travellers’ diarrhoea.
Dry January grows in popularity year on year.
The campaign by Alcohol Change UK, encourages participants to give up alcohol for the entire month of January.
The dry January one-month booze-free challenge can have a significantly positive impact on your health.
Alcohol has proven to increase the risk of developing a range of health problems (including cancers of the mouth, throat and breast) and that risk increases the more you drink on a regular basis.
Ruth Kander, our dietitian, looks at what is considered a safe amount of alcohol consumption.
The UK Chief Medical Officers’ (CMOs) guideline for keeping health risks from alcohol to a low level for both men and women states that:
- It is safest not to drink more than 14 units a week on a regular basis.
- Regularly drinking as much as 14 units per week, it’s best to spread your drinking evenly over three or more days.
– If you have one or two heavy drinking episodes a week, you increase your risk of death from long-term illness and injuries. - Cutting down the amount you drink, a smart way to help achieve this is to have several drink-free days a week.
A useful website for more information about alcohol is www.drinkaware.co.uk
What is a unit of alcohol?

How long does alcohol stay in your body?
On average, it takes about one hour for your body to break down one unit of alcohol, however, this can vary, depending on:
- Your weight
- Whether you’re male or female
- Your age
- Your metabolism – how quickly or slowly your body turns food into energy
- How much food you have eaten
- The type and strength of the alcohol you have consumed
- Whether you’re taking medication and, if so, what type
- It can also take longer if your liver isn’t functioning normally
If I am on medicines can I drink alcohol?
People taking sedative drugs (like diazepam/valium) or antidepressants (like fluoxetine/Prozac) should avoid alcohol altogether.
There are some antibiotics; metronidazole and tinidazole which just do not mix with alcohol – drinking with these will make you sick. But for most commonly prescribed antibiotics, drinking is unlikely to cause problems so long as it is within the low-risk alcohol unit guidelines.
People taking long-term medications should be careful about drinking, as alcohol can make some drugs less effective and long-term conditions could get worse. Examples of long-term medications include drugs for epilepsy, diabetes, or drugs like warfarin to thin the blood.
(From www.drinkaware.co.uk)
What are the consequences of drinking too much alcohol?
- Low mood/mood swings
- Liver problems
- Heart problems
- Cancers (mouth, tongue, throat, oesophagus)
- Weight gain
- Poor sleep
- Blood pressure instability
By Ruth Kander BSc(Hons)RD | Dietitian
If you wish to discuss ways to maintain a healthy diet and reduce your alcohol consumption, Ruth holds a virtual clinic every Friday from 9am-2pm. Please call our reception team on 020 7353 5678 if you would like to request a face-to-face appointment
Cases of Strep A infections amongst children are on the rise and tragically at least 9 children are known to have died in the UK as a result.
What is Strep A?
Group A streptococcus (GAS) is a common bacteria. Lots of us carry it in our throats and on our skin and it doesn’t always result in illness. However, GAS does cause a number of infections, some mild and some more serious.
Strep A causes infections in the skin, soft tissue and respiratory tract. It’s responsible for infections such as tonsillitis, pharyngitis, scarlet fever, impetigo and cellulitis among others.
Strep A Infections are not common but it is important for parents to lookout for symptoms and consult a GP as soon as possible for early diagnosis and treatment. Strep A infections are treatable if caught early.
Symptoms of Strep A
The first symptoms to appear are fever, chills, muscle aches and sore throat with difficulty swallowing.
Later, a rash may develop and the tongue may become red and inflamed. There may be pus on the tonsils which can be seen as white exudates. The disease affects the neck as well as it becomes tender due to the enlargement of the lymph nodes.
Small children may also present with headaches and abdominal pain in addition to the above symptoms, plus even nausea and vomiting.
How does the disease spread?
School children are in the close contact with each other and hence, they are more likely to spread the disease. In the past, GPs have been advised not to prescribe antibiotics if avoidable.
Strep A needs treatment with Penicillin or an alternative antibiotic in the case of penicillin allergy.
Children with strep A must stay at home until recovered to avoid spreading the bacteria.
How can you protect your child
It is very important for carers to stay vigilant and lookout for any symptoms that their child might have. If there is any suspicion of Strep A, make sure that the child is treated with antibiotics or an alternative just to be safe.
To limit the risk of infection, parents must not send children to school with tonsillitis, so that the spread of the disease can be reduced.
If your child develops symptoms:
- consult your GP for proper medical advice
- do not leave it until your child is seriously unwell to get treatment
Call 999 or go to A&E for emergency help if your child:
- develops difficulty breathing
- pauses between breaths
- will not wake or stay awake
- their skin, tongue or lips change colour to blue
The number of cases can be reduced if proper care is taken for Strep A and its symptoms.
_____________________________
We are a family friendly health clinic – if your child needs to see a GP – book online.
________
Dr Belinda Griffith’s comments in the UK news:
Independent Online: How can I protect my child from Strep A?
Yahoo! News: Health: How can I protect my child from Strep A?
The Herald Scotland: How can I protect my child from Strep A?
Flu cases in the UK have increased earlier this winter than usual, perhaps by over a month.
Other unpleasant respiratory infections such as RSV are also on the rise.
Information from around the world can help us predict what might type of flu season might be heading our way.
- Australia has just come to the end of a bad flu season, with a dramatic increase in flu cases and hospitalisations relative to the mild season it experienced last year, in a pattern likely to be replicated in the UK.
- In the USA, by the end of November 2022 there had already been more than 6.2 million flu cases, with 53,000 hospitalisations, and 2,900 deaths from flu.
- Across Europe as a whole, the flu season has commenced earlier than in the 4 previous seasons, and the proportion of positive tests from sentinel locations has exceeded the technical threshold for consideration as an epidemic.
Meanwhile, UK vaccination rates have so far been low: by the end of November, when the flu vaccination campaign should be largely complete, fewer than 40% of “at risk” adults under 65 had been vaccinated, fewer than 25% of healthy adults aged 50 to 64, and fewer than 30% of pregnant women.
So this winter’s flu season is likely to be more severe, and not enough people will be protected.
What can you do to keep well this winter?
Get Vaccinated . Get Tested . Get Treatment
Get Vaccinated
The good news is that circulating flu strains have so far been a good match with this year’s flu vaccines. It is not too late to be vaccinated. Vaccines are still available. At this point in the season, our preferred vaccine for adults is our premium recombinant vaccine, Supemtek, which is known to be highly immunogenic.
Flu cases in children are rising but the nasal spray vaccine has so far been in restricted supply. If your child has not yet been able to obtain the flu spray, injected flu vaccines are at least as effective and should be given without further delay.
You can easily book your flu jabs online.
For family or groups bookings, it may be more convenient for you to book by phone or email.
Get Tested
At the Fleet Street Clinic, we can test quickly and accurately for a full panel of respiratory viruses in our own laboratory. It is helpful to know whether you are suffering from flu, covid, or another circulating virus such as RSV or metapneumovirus. We can tailor treatment to the result, help you know how long symptoms will last, and can help you prevent spreading it to others – especially important over the Christmas period when socialising in high at work and amongst family and friends.
Get Treatment
Flu is treatable with anti-viral drugs, which reduce symptoms and speed recovery. Preventive treatment for close contacts and other members of your family is also something we can help with, available from our GPs. Knowing for certain that you have a viral infection can also help avoid unnecessary antibiotic treatment.
___________________________
For more information on Flu Jabs available at Fleet Street Clinic.
Other recommended winter vaccinations are the shingles vaccine & the pneumonia vaccine.
We can also provide onsite Workplace Flu Vaccinations for companies in the UK – for more information.
Complete the below form for a quote:
Stress, everyone has it too some degree – some is healthy, lots is not.
What effect does a lot of stress have on your body?
Stress is known to affect the whole body but we shall focus on the way it affects the neck and shoulder girdle. Much research over the years has confirmed a connection between neck pain and stress. One study, for instance, in the BMC Musculoskeletal Disorders Journal, found that of nearly 500 people tested, those with stress, anxiety or depression had significantly worse neck pain that lasted longer than those without.
Even without the research though, lots of people will tell you that stress makes their neck and shoulders feel tight. When someone consciously relaxes, one of the most noticeable things to happen is their shoulders drop a couple of inches.
I’d go even further, and say that as the brain recognises the connection between stress and neck & shoulder tightness (and in fact initiates it). Let me explain, if someone has a tight neck or shoulders due to another cause, the brain, rightfully or wrongfully interprets this as the body being stressed.
If you have those muscles massaged and loosened and the neck releases, most people feel immediately less stressed.
Some of the many causes of neck or shoulder girdle dysfunction and stress crossover, such as long hours working at a computer to meet deadlines, and not sleeping very well. From this, secondary symptoms can develop, most commonly, headaches.
Some exercises that I recommend for tension headaches can be found here.
So what can we do about it?
Well, as always, firstly make sure there is nothing else causing your symptoms. Get a health professional to assess you and diagnose what is causing your symptoms.
If the diagnosis is stress or posture-related then get it treated. It’s important to treat from both a musculoskeletal point-of-view as well as understand and address the cause of your stress.
Alongside this, there are a number of at-home techniques you can do to help ease the tension in your neck and shoulders.
1. Do neck and shoulder mobility exercises.
A couple of quick and easy exercises I would recommend would be:
Exercise 1 :
https://www.youtube.com/shorts/vSBsfMnMx6M
Exercise 2 :
https://www.youtube.com/shorts/X6XJdciru0Q
Exercise 3 :
https://www.youtube.com/watch?v=A0HWan_RPwo
2. Get a good amount of quality sleep.
Stress is known to affect your ability to sleep. There are things you can do to give yourself the best chance of sleep.
– Make sure you’re comfortable in bed
– Be strict with no blue light (screens) for at least an hour before bed
– Having a warm bath or shower to help you relax
3. Find something to relax you.
It doesn’t have to be meditation or yoga, it could be exercise or playing an instrument. Perhaps avoiding instruments such as the violin which will exacerbate neck & shoulder pain. The ides if to find something that sends you to your flow state. Something that will distract you that you really enjoy and will relax you.
4. Work in a good environment.
Set up your workstation in an ergonomic way will do wonders for your posture. Remember to have lots of breaks and consider investing in a standing desk. If you’re interested in knowing what an ergonomic workstation set up looks like, continue reading here.
5. Speak to a healthcare professional.
Your health professional may recommend you get support or therapy for your stress, anxiety or depression, or any mental health issues you may be experiencing.
_____________________
Is Osteopathy the right path for you?
Osteopathy is a holistic way to diagnose and alleviate stress-related musculoskeletal problems including shoulder and neck pain and secondary symptoms such as headaches. The treatment is catered to the individual and Andrew will take all aspects of a patient’s lifestyle into consideration when suggesting a treatment plan.
All treatment starts with an initial consultation followed by any recommended follow up treatment. You can book your initial consultation with Andrew Doody online.
A good night’s sleep is essential to your health, and an important part of your overall well-being. People spend about a third of their lives in bed, so it’s vitally important to get it right when it comes to back health. Back pain can significantly affect a person’s ability to get the quality and amount of sleep they need. Furthermore, poor bed posture can worsen or even be the cause of backache in the first place. This is because certain positions can place unnecessary pressure on the neck, hips, and back.
This blog will provide an in-depth review of different sleeping positions and types of beds and the impact both have on your quality of sleep.
Sleeping positions
Before looking at the positions to sleep better, it is important to address a few crucial things. First and foremost, you should be comfortable. For a good night’s sleep, waking up feeling properly rested and not in pain is the most important thing. If any of these positions cause issues, don’t hesitate in letting me (or another osteopath) know so that alternative suggestions can be made and you find something else that works for you.
Secondly, I know it’s not always possible to control what position you get into once you’ve fallen asleep. However, this is where perseverance comes in, if you keep trying, your body can adapt in a week or two. Pillows are always a good ally, to stop you rolling one way or the other.
Here are some positional tips that can help you get a better night’s sleep:
1. The Classic: Lying on your back.
Lying on the back is probably the best all-around sleeping position for a healthy back. It ensures good spinal alignment from the head and cervical vertebrae, through the thoracic and lumbar, all the way down to the pelvis. Because the back is the body’s largest area, weight is most widely distributed in this position, minimising pressure hot spots. This doesn’t suit everyone though, some people don’t feel as ‘nested’ as in other positions so, they struggle to get to sleep on their backs. Also, snorers may find that this position exacerbates the problem.
For people who like back sleeping, it’s definitely worth adding a pillow under your knees. It loosens the hamstrings a little and takes some pressure off the lumbar lordosis.
2. The Foetal Position: Lying on your side with your knees up a little.
This is a fairly intuitive position to get into if you have lumbar disc issues as it slightly flexes the low back and opens up the gaps in the facet joints.
Again, a good tip in this position is to use a pillow, however, this time put it in between your knees. This stops your top leg dropping forward and rotating the low back. It also aligns your hips and pelvis better, and feels more comfortable on the upper knee.
Try to swap sides from time to time if you’re lying in the foetal position.
3. Face Down: Lying on your stomach.
I normally ask people to avoid this position, it’s usually quite problematic for the neck as well as the low back. Unfortunately, for a lot of people, it’s the only position they can fall asleep in, or any other position makes them snore. If you’re one of them, reach for that extra pillow again and put it under your low stomach and upper pelvis to take the pressure off the low back. This is a good idea if you’re having a massage too. Front lying needs a much flatter pillow (or even no pillow) under the head too.
If you’re someone who falls asleep on their back or side, then rolls over in their sleep and wakes up on their stomach, try hugging a large pillow against your chest and stomach to keep you in position. Another reason sleeping on the front is considered bad is because the head is usually turned to one side. This twists the spine and places additional stress on the neck, shoulders, and back. To avoid this, you can try lying face down. Place a small firm pillow or tightly rolled-up towel under the forehead, or better still a face pillow, allowing room to breathe. In this position, you should still place a pillow under the stomach.
4. Reclined Sleeping.
If all else fails, you can try sleeping in a reclined position. People with spondylolisthesis, for instance, may resort to this after finding it comfortable falling asleep in a recliner chair. There are beds available that can be sat up slightly. So, this is worth investigating.
What about the perfect bed for sleep?
There are so many different opinions about beds that I don’t even know where to start, nonetheless here’s mine.
Spend some time and effort (and dare I say money) choosing a bed and mattress. People seem happy to spend thirty times or more on a car than a mattress, but remember, a third of your life is spent in bed!
It’s really difficult to choose a mattress on a twenty minute trip to the bed store, so really take your time, spend an afternoon there, take your shoes off, try different sleeping positions, not just lying on your back! Do your research before you go, but make sure the review sites you look at aren’t secretly run by a bed company, or affiliated to one.
Firmness
Try not to be seduced by softness. Lots of people jot down the name of a mattress they’ve found comfortable in a hotel, and while this can sometimes be a good indicator, you should know that hotels buy mattresses to give you a couple of nights feeling like you were sleeping on a cloud, but these mattresses are usually not supportive enough to be using full time, especially if you have low back issues, which can be aggravated over weeks and months. Often the mattress in a big hotel chain is not available to buy for the public as they are specifically manufactured for different hotels’ standards.
A fairly firm mattress is usually a good idea, perhaps with a shallow in-built topper. This can give you the support you need for your low back while the topper takes the pressure off bony prominences and allows shoulders and hips of side sleepers to sink in a little. I suggested a built in topper as they are usually better segmented and don’t allow stuffing to move around and bunch up as much. However, removable toppers give you more scope to adapt by removing it if needed, and also allow you to flip the mattress.
Mattresses that are fully stuffed as well as sprung are good and supportive. Price is a good indicator for a quality mattress. £1,500 for a king size mattress is not excessive. While we’re talking about price, beware of anything that seems too good to be true. The “Winning awards” mattresses need to be checked as to which award, and who’s giving it!
Memory Foam Mattress
Patients have different opinions about memory foam mattresses. While some patients swear by them, others do not get along with them. I’d like to reiterate the price, if you’re set on a memory foam mattress, find the one with better quality, so it doesn’t start to develop a permanent dip where you lie. It’s all about density which is measured in pounds of pressure per cubic square foot. More is normally more expensive and better quality, but at the same time is also more supportive and feels harder.
There can be a problem with memory foam mattresses feeling too hot. While many of the better brands have addressed this to an extent, many memory foam mattresses have become hybrids so, it’s not just 100% foam any more.
Platform Bases
Mattresses should be changed about every 8 years, but you can keep the same bed base, of course, as long as it’s not damaged. Divans have pretty thin wood tops that can crack or bow so, check it carefully.
In my opinion, a platform base is always the best. If the base is sprung, the whole mattress will start to fold which is usually not what they’re designed to do. A slatted base is slightly better than a fully sprung one, but still not as good as a solid base.
Pillows
Finally, I should mention pillows. Pillows are very subjective to the person, and especially to any neck/upper back/shoulder girdle conditions they may have.
As a rule of thumb (and this is painting with a very broad brush) people seem to usually have too much pillow depth more often than too little. One medium depth pillow is usually best if you don’t have any specific issues. I find feather works well as you can punch and mould it to the right height and shape, so there is some support under your neck but that’s very much a personal preference.
I rarely see anyone who gets on well with memory foam pillows (there are the odd one or two) or sprung pillows.
The price of a good feather pillow is probably about £50, but as I said right at the start, I want you to not only be in a good position, but also comfortable and pain-free during the night and the next day, so if a £5 pillow works for you then that’s absolutely fine. Don’t forget most pillows can be laundered regularly which may give (especially feather pillows) some of their volume back.
If you are experiencing neck pain though, get your neck examined and treated first and ask your osteopath what pillow they would suggest for you specifically going forward.
BE ‘BED FIT’
The healthier and stronger your back is, the better night’s sleep you will get and the better your back will be when you get up in the morning.
Core strengthening exercises will help support the back during the night and prevent back spasms. Gentle stretching before bed can increase flexibility and help to relax the body and reduce stress.
Take care getting in, and especially out, of bed. Take your time. When you wake up in the morning, allow a few minutes to get your muscles and joints moving fully instead of leaping out of bed at the alarm. Roll onto your side then use your arms to push you upright while your legs drop over the side, then sit there for a minute moving gently before slowly standing up.
Perhaps most importantly, if you do have a back or musculoskeletal issue, get it checked. A health professional can assess why you’re suffering and help treat the symptoms. They can suggest the correct investigations, treatment and exercises, as well as further helping you to choose that all important correct mattress.
Booking an appointment with an osteopath could be the start of ending your back pain for good!
Mental Health Awareness Week: What Is Stress?
Look around your office, do you know if anyone is struggling?
You may think those around you – fellow colleagues or your staff – are completely fine. But mental health affects us all and problems in the workplace are actually very common.
According to mental health charity Mind, at least one in six workers are experiencing common mental health problems, including anxiety and depression.
Nowadays, there is increasing recognition of stress and mental health problems, both within the workplace and in everyday life. Currently, following Stress Awareness Month in April, we are approaching Mental Health Awareness Week, which takes place from 13-19th May.
We thought it might be helpful to focus on some positive strategies to help, in terms of stress management and resilience. Whilst being particularly useful and relevant within the workplace, these can all be used in everyday life as well.
WHAT IS STRESS?
In its purest form, stress is the body’s reaction to something it perceives as dangerous or threatening. When we feel under attack, our bodies respond by producing a mixture of hormones such as adrenaline and cortisol. These prepare us for physical action by diverting blood away from our core and into our limbs. It also temporarily shuts down some less vital bodily functions such as digestion.
For immediate, short-term situations, stress can be beneficial to your health, by helping you cope with potentially serious situations.
Yet if your stress response continues, and stress levels stay elevated far longer than necessary, it can take a toll on your health.
WHY IS IT IMPORTANT TO TACKLE STRESS?
Chronic stress can cause a variety of symptoms, contribute to many health problems (such as high blood pressure, heart disease, obesity and diabetes, anxiety and depression) and affect your overall well-being.
Reducing stress can help prevent these harmful effects on both mind and body.
Looking after yourself and ensuring you have good mental health has many benefits – not just for you as an individual, but for the business too. Employees are generally more productive, passionate and motivated when in good health. Even if they’re experiencing mental health problems, knowing they are supported by their employer can help in the recovery process.
STRESS PREVENTION IS BETTER THAN STRESS MANAGEMENT
Ultimately, the best way to manage stress is through prevention rather than cure.
Research shows that those who are better informed about the practical ways in which they can lower their stress levels are far better able to tackle difficult situations with emotional resilience and determination.
Within the workplace, employers are encouraged to make promoting the wellbeing of their employees a core element of the company’s internal operations. Some examples of a proactive approach to stress-management might be:
- To invite people to take active breaks away from their desks
- Offering lunchtime yoga classes or mindfulness sessions
- Group walks in the fresh air.
So what can help you reduce stress? Continue reading our stress, with Our Top Tips For Reducing Stress.
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch. Or if you are an individual who needs help with stress management, you can book a GP appointment online.
Feeling stressed?
Everyone feels stressed from time to time. In small doses, stress can actually be quite useful; motivating us to achieve our goals. But for some, stress is chronic. Meaning it is debilitating and negatively impacts their mood, their health and wellbeing, their relationships and their work.
Experiencing a lot of stress over a long period of time can also lead to a feeling of physical, mental and emotional exhaustion, often called burnout. It is, therefore, easy to see why reducing stress across all areas of your life would be important. Stress management tips are a good place to start.
Learning how to manage your stress takes practice and time.
Here are our top 10 ways on managing and reducing stress.
10 TIPS TO REDUCE STRESS:
-
Prioritise your health
– make decisions which will benefit your physical, mental and emotional wellbeing. For example, go alcohol-free a few nights each week or allow yourself time for a hobby you enjoy. These small steps for a healthier lifestyle will help in reducing stress levels.
-
Get a good night’s sleep (regularly)
– research clearly shows that sleep deprivation amplifies the symptoms associated with stress. Aim for between 7-9 hours of good quality sleep every night.
-
Practice deep breathing
– when our bodies are stressed, the muscles that help us breathe tighten. By focussing on taking several deep breaths we can quickly and effectively relieve physical symptoms associated with feeling stressed or anxious. Try to do this regularly throughout the day.
-
Drink enough water
– being dehydrated (however mild) causes our cortisol levels to rise, which automatically makes us feel stressed. Your body is already dehydrated if you’re feeling thirsty. So try to avoid reaching this point by hydrating yourself regularly. Aim for 2-3 litres per day, more in hot weather or when exercising.
-
Eat a balanced diet
– dieticians stress how certain foods have stress-relieving properties. For example, dark chocolate is rich in antioxidants, whilst avocados and oily fish are high in omega-3 fatty acids (both of which are proven to help lower anxiety levels).
-
Exercise regularly
– physical activity causes our brains to release mood-improving chemicals called endorphins. These help us to cope with potentially challenging situations. Both Public Health England and the World Health Organisation recommend at least 150 minutes of moderate intensity physical activity each week, in bouts of 10 minutes or more. Choose activities you enjoy to achieve maximum benefit for the mind as well as the body.
-
Adopt a positive mindset
– research suggests that making a conscious effort to think positively can help protect us against a whole host of physical and mental issues, including stress.
-
Manage your time and tasks effectively
– by giving ourselves enough time in which to complete a given task, and by making sure that we don’t try and accomplish too many stressful things at once, we can reduce the likelihood of feeling overwhelmed.
-
Spend less time online
– many studies have found a strong positive correlation between internet usage and stress levels. Spending less time on our computers and phones is a simple way to practice self-care. Having screen-free time for at least an hour before bedtime has also been shown to improve sleep.
-
Learn to say no
– in a culture that demands we take on more and more responsibilities, having the confidence to say “no” will only become more important. This final tip takes us back to the start, by reiterating the importance of prioritising our health above unrealistic social pressures, and brings us onto developing an essential tool – resilience.
Continue reading about Resilience or read What is Stress?
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch.
Or if you are an individual who needs help managing stress, you can book a GP appointment online. Our doctors will be able to talk through your thoughts, symptoms and emotions and set you on the right path to diagnosis. They will also be able to recommend relevant support services for stress, if appropriate.
Mental Health Awareness Week: Resilience
WHAT IS RESILIENCE?
Resilience is the ability to recover from adversity, hardships, or significant sources of stress.
It means “bouncing back” from difficult experiences, feeling stronger and more capable to cope than before. With life becoming more stressful than ever, it is an important skill to develop which can make a big difference between surviving and thriving within work and general life.
HOW RESILIENT AM I?
Research has shown that resilience is ordinary, not extraordinary, and is not simply a trait we either have or do not have.
So here’s the good news! Resilience can be developed. It involves behaviours, thoughts and actions which can be learned and developed in anyone.
SO HOW CAN I DEVELOP RESILIENCE?
Many studies show that the primary factor in developing resilience is having caring and supportive relationships within and outside the family, including at work. Relationships fostering trust, provide role models and offer encouragement and reassurance help bolster resilience.
Several additional factors are associated with resilience, including:
- The capacity to make realistic plans and take steps to carry them out.
- A positive view of yourself and confidence in your strengths and abilities.
- Skills in communication and problem-solving.
- The capacity to manage strong feelings and impulses.
These are all factors you can develop in yourself, and which can be fostered within the work environment by employers taking an active interest in employees’ wellbeing.
TOP TIPS FOR DEVELOPING RESILIENCE
Here are a few things you could try, to develop your resilience.
Please don’t feel you need to tackle them all at once – trying one or two at a time may be enough to make a big difference!
1) Create connections
– good relationships with family, friends and colleagues are crucial. Accepting help and support from those who will listen to and care about you strengthens resilience. Assisting others in their time of need can benefit you in return.
2) Accept that change is fundamentally part of living
– accepting circumstances that cannot be changed can help you deal with these more effectively whilst focussing on circumstances that you can alter.
3) Avoid seeing stressful events as insurmountable problems
– try to look beyond the present towards how future circumstances may be a little better. Take note of any subtle ways in which you might already feel better as you deal with difficult situations – signs of good progress.
4) Take decisive action
– this can assist you in giving some control over your response to challenging situations
5) Pursue your goals
– making them small but achievable and most importantly realistic. Each day, ask yourself “What’s one thing I know I can accomplish today which will help me move in the direction I want to go? Take baby steps in the right direction!
6) Nurture a positive outlook
– developing confidence in your ability to solve problems and trusting your instincts helps build resilience.
7) Keep things in perspective
– retaining an optimistic outlook and visualising what you want, rather than worrying about what you don’t want, can all help the brain engage with this.
8) Practice mindfulness and meditation
– Mindfulness means paying more attention to the present moment – to your own thoughts and feelings, and to the world around you. Meditation involves the use of techniques such as mindfulness to train attention and awareness. Mindfulness and meditation are believed to relax and calm the brain, tackling sources of stress while improving clarity focus and even sleep. According to mentalhealth.org.uk, those practising mindfulness have shown increased activity in the area of the brain associated with positive emotions.
9) Take opportunities for self-discovery and personal growth
– by learning something about themselves, people may find that they have grown in some respect. Many people who have experienced tragedies and hardship have reported better relationships, a greater sense of strength even while feeling vulnerable, increased sense of self-worth, a more developed spirituality and heightened appreciation for life.
10) Take good care of yourself
– pay attention to your own needs and feelings. Engage in activities that you enjoy and find relaxing. Exercise regularly. Taking care of yourself helps to keep your mind and body primed to deal with situations requiring resilience.
If you would like further help and support in resilience training in your workplace, get in touch with our Corporate Health department.
Stress: Are we coping?
We all feel the effects of stress in daily life, whether it’s managing children or dealing with a problem at work. Stress is a normal response, in fact, in small doses, stress can be useful. The problems arise when you start to have a ‘fight or flight’ stress response to situations in everyday life. This can lead to illness, both mentally and physically.
The first step is to recognise symptoms of stress:
- Nail biting and fidgeting
- Over-eating or loss of appetite
- Irritability with other people
- Substance abuse, including alcohol and smoking
- Lack of concentration
- Increased and suppressed anger
- Feeling out of control
- Excessive emotion & crying
- Lack of interest in anything
- Permanently tired even after sleep
By identifying stress-related problems as early as possible, action can be taken to avoid any serious stress-related illness. For Mental Health Awareness week, which runs from 14-18 May, here are some tips to help manage your own personal stress:
- Be active – 30 minutes a day can reduce the emotions and let you take the time to think more clearly
- Take control – you are your own worst enemy, but you are also the key to empowerment!
- Find support – Connect with your family and friends, the more help the better the solutions
- Take time for yourself – remember to have time for yourself as well. Read, relax and get things done on your to do list that may be holding you back
- Create challenges for yourself – Setting achievable goals, little or big can help build confidence in your abilities
- Avoid unhealthy habits – Cut down on caffeine, smoking, and alcohol. These can enhance the feeling of stress in the long run
- Be positive – Instead of looking at problems negatively, try to see what you can get out of it to help you grow. Be grateful!
- Acceptance – Take ownership of mistakes, or acceptance of things you can’t control.
Our Occupational Health team at the Fleet Street Clinic are able to provide a full range of work health assessments to address the occupational health needs of your staff. Click here for more information.
To book an appointment with one of our friendly doctors, or for further details on what we can offer for our Occupational Health, call us today on 0207 353 5678 email info@fleetstreetclinic.com or book online now.

Cutting back on alcohol can be a really effective way to improve your health, boost your energy, loose weight and save money.
In 2016, the Chief Medical Officers in the UK reduced the recommended amount of alcohol you should consume a week due to concerns about the risk of cancer. New research confirmed that even drinking a small amount of alcohol per week can cause an increase in risk of cancer.
From then onwards, it has been recommended that men and women have the same weekly intake of units per week. According to the UK low risk drinking guidelines, you should drink no more than 14 units a week, make sure you have several drink-free days, and never binge drink.
What does 14 units of alcohol look like?
Because alcoholic drinks come in different strengths and sizes, units are a way to tell how strong your drink is. 14 units is equivalent to six pints of average strength beer or six medium (175ml) glasses of average strength wine.

It’s safest for both men and women to drink no more than 14 units a week, spread over three or more days with several drink-free days, and no bingeing.
Your risk of death from long term illness, accident or injury, is increased if you ‘binge drink’ 1 or more times a week.
How long does alcohol stay in your body:
On average, it takes about one hour for your body to break down one unit of alcohol. However, this can vary, depending on:
- Your weight
- Whether you’re male or female
- Your age
- How quickly or slowly your body turns food into energy (your metabolism)
- How much food you have eaten
What are the consequences of drinking too much alcohol:
- Low mood/mood swings
- Liver problems
- Heart problems
- Cancers (mouth, tongue, throat, oesophagus)
- Weight gain
- Poor sleep
- Blood pressure instability
What are the benefits to cutting down on alcohol?
Short-term benefits:
- waking up in a better mood
- being less tired and more energetic throughout the day
- healthier looking skin
- saving some money
Long-term benefits:
- lower your blood pressure
- lower the risk of diseases including cancer, stroke, hypertension and liver disease
- lower your cholesterol levels
- your memory will improve
- better quality of sleep
- help with weight management*
* Did you know? Alcoholic drinks are high in calories, so cutting back on the amount you drink can really help to reduce your calorie intake.
According to our GP & Occupation Health Physician, Dr Claire Braham;
“When you drink alcohol, you lose around 4 times as much fluid as you drink.
It is therefore easy to understand why dehydration often occurs. Dehydration symptoms are much like your classic hangover symptoms and will include headache, nausea and fatigue. These symptoms will become present when you are about 2-percent dehydrated, which is about when you start to feel thirst.
Avoiding alcohol means better hydration and sleep which will reduce hangovers and headaches, reduce tiredness, reduce sickness, increase your concentration and improve your overall control over emotions and behaviour. This leads to more productivity, better decision making and overall less accidents, regrets and more enjoyment.
It is not advised to drink more than 14 units a week, which is the equivalent of 6 pints of beer. That converts to 1,092 calories in total and would need 109 minutes of running to burn off those additional consumed calories. Abstinence is an easy way to avoid festivity weight gain.
Nowadays it is very easy to cut down or cut out alcohol. There is a wide variety of alcohol-free beer, wine, prosecco, gin, vodka, whisky and other spirits available on the market. These include some which are vegan and gluten-free as well as often free from sugar and artificial sweeteners. So you can still enjoy a ‘drink’, without the alcohol and high-sugar but with health benefits.”
For further detail of how alcohol can have a negative impact on your health, head to drinkaware.co.uk for more information and advice on drinking.
If you have concerns about the amount of alcohol you are drinking or about your health you should speak to a GP. You can book an appointment online.
More information on our GP service can be found here.
Tension Headaches
80% of adults will experience tension headaches at some point. They are caused by tight muscles surrounding the neck, pressing on nerves that refer pain to another location, in this case, the head.
Most often, tension headaches are triggered by lifestyle factors such as poor posture i.e. from sitting hunched over at a computer and/or stress.
Almost all types of headache activate the same pain receptors so it can be difficult to know if your headache pain is a sign of something more serious. When experienced suddenly or regularly, you should always get your headache pain assessed by a health professional to rule out any serious health conditions.
Stretches
If you have been diagnosed with tension headaches alone, the good news is they respond well to treatment. Here are a few stretches to help relieve the pain they cause:
Stretch 1
This is a neck flexion stretch that you should repeat 10 times, holding for a few seconds each time.
https://www.youtube.com/watch?v=XZe7c0kpZA4
Stretch 2
This is a stretch for the upper trapezius that you should repeat 10 times, holding for a few seconds each time.
https://www.youtube.com/watch?v=yRtWVO1zKLE
Stretch 3
This is a stretch for the scalene muscles that you should repeat 10 times, holding for a few seconds each time.
https://www.youtube.com/watch?v=dUHsyB-opYg
Stretch 4
This is a levator scapulae stretch that you should repeat 10 times, holding for a few seconds each time.
https://www.youtube.com/watch?v=3k9cNIlIE-Q
For more information on Osteopathy services at Fleet Street Clinic.
You can book an initial consultation with Andrew Doody online.
How walking can help Chronic pain
Firstly, what is chronic pain?
Chronic or persistent pain can be explained as pain that carries on for longer than 12 weeks despite medication or treatment.
The root cause can vary person-to-person, with it sometimes due to illness or an injury. In other cases it can be due to being overweight, having years of poor posture or improper lifting of heavy weights. It can be debilitating but movement is known to help.
As an osteopath, the conversation I seem to have at least once-a-day is; how much exercise should someone who is in pain be doing?
As you can imagine every case is different, and exercise advice varies hugely from person to person and condition to condition. There is a big difference between chronic pain and recovery from injury pain. I am focusing on exercises for people with chronic pain conditions, specifically walking.
Many people with chronic pain are afraid that movement, including walking, will worsen pain. But as many have subsequently discovered, the opposite is very often true. Using your muscles and joints less can often cause pain to becomes worse. Gentle exercise like walking can really help to bring those pain levels down, as well as many other benefits like improving your circulation, strengthening your bones and of course helping to keep those extra pounds off.
Here are tips before you start:
1. Talk to your healthcare professional first
You should always take the advice of a health professional before starting any exercise. They can ensure it is safe for you to start, and guide you with the types of exercises you should begin with. They will also help you understand your limits and outline suitable goals. As a rule of thumb, if you are in pain, stop!
I, or another osteopath, can check your posture and gait and give you tips on engaging the correct muscles.
2. Get the right shoes
A good pair of supportive trainers will prove invaluable. Walking boots that protect the ankle are only really required if you’re planning to walk on loose surfaces or heading off into the mountains. Otherwise, walking trainers will suffice. To find out more about choosing the right footwear, read our blog on How To Avoid Running Injuries.
3. Start slow
What we’re aiming for is about half an hour to an hour of physical activity five days a week, but this may take some time to achieve. There’s no rush! A good indicator that you are at the right intensity level is that even though your heart rate is up a little, you are still able to carry on a conversation while walking. When starting your walk don’t go full speed immediately. Allow your muscles and joints to warm up for the first few minutes before getting up to speed. This will help prevent damage and injuries.
4. Keep hydrated
You may need to carry a bottle of water, especially for walking in hot weather. If the weather is hot, make sure you also take sunscreen and a hat to stop sunburn.
5. Finally, try to enjoy it!
The more you enjoy it, the easier it becomes. Find somewhere nice to walk, even if that means
driving somewhere. Listen to music/ podcasts/ audiobooks, or even better get a walking buddy to join you for a chit chat along the route.
For more information on osteopathy services, visit the main page.
___________________________________
OSTEOPATHY AT FLEET STREET CLINIC
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC).
Book an appointment with him if you have any musculoskeletal injuries by calling +44 20 7353 5678, email info@fleetstreetclinic.com or book an appointment online.