Tag: travel clinic
Egypt has long been a fascinating destination for travellers with its ancient monuments, rich culture, and vibrant landscapes. Now, there’s even more reason to consider Egypt as a travel destination: the World Health Organization (WHO) has officially declared the country malaria-free.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, said “Malaria is as old as Egyptian civilisation itself, but the disease that plagued pharaohs now belongs to its history and not its future.
This is a significant milestone in public health and brings an added layer of safety and assurance to travellers planning to visit.
Here’s what you need to know about this important achievement and what it means for your health when traveling to Egypt.
What does it mean to be “Malaria-Free”
To be certified as malaria-free, a country must demonstrate that it has interrupted local transmission of malaria for at least three consecutive years. Egypt met this requirement, showing consistent results in controlling the disease, improving healthcare infrastructure, and reducing the risk of reintroduction.
According to the WHO, Malaria in Egypt has been traced as far back as 4000 B.C.E., with genetic evidence of the disease found in Tutankhamun and other ancient Egyptian mummies.
Egypt is one of the latest countries to receive this certification, contributing to a global push toward eradicating malaria worldwide.
What does it mean for travellers?
Malaria has long been a concern in various tropical and subtropical regions, causing severe illness, fever, and sometimes even death.
Travellers often must take preventative steps, such as antimalarial medication and mosquito avoidance measures, when visiting areas where malaria is prevalent.
Egypt’s certification as malaria-free means travellers now have one less health risk to consider when planning their holiday.
For the tourism and travel health sectors, this achievement reassures visitors that Egypt is safe from malaria transmission, especially in rural areas and near water sources, which are typically high-risk locations for malaria-carrying mosquitoes.
Are there any precautionary measures still needed?
While Egypt’s malaria-free status is excellent news, it’s still essential to practice general travel health precautions to stay safe.
Here are some tips:
- Protect Against Other Mosquito-Borne Diseases: While malaria may not be a concern, other mosquito-borne illnesses, such as West Nile Virus and Dengue Fever, can still pose risks. Use insect repellent, wear long sleeves, sleep under a mosquito net and consider vaccinations where possible, like Qdenga for Dengue Fever.
- Stay Up-to-Date on Vaccinations: Egypt does require certain vaccinations for travellers, such as Rabies, Hepatitis A, Hepatitis B, and Typhoid. Make sure you are aware of any health advisories and have up-to-date vaccinations before your trip.
- Practice General Travel Hygiene: Staying hydrated, avoiding untreated water, and being cautious with food preparation are essential for staying healthy on your travels.
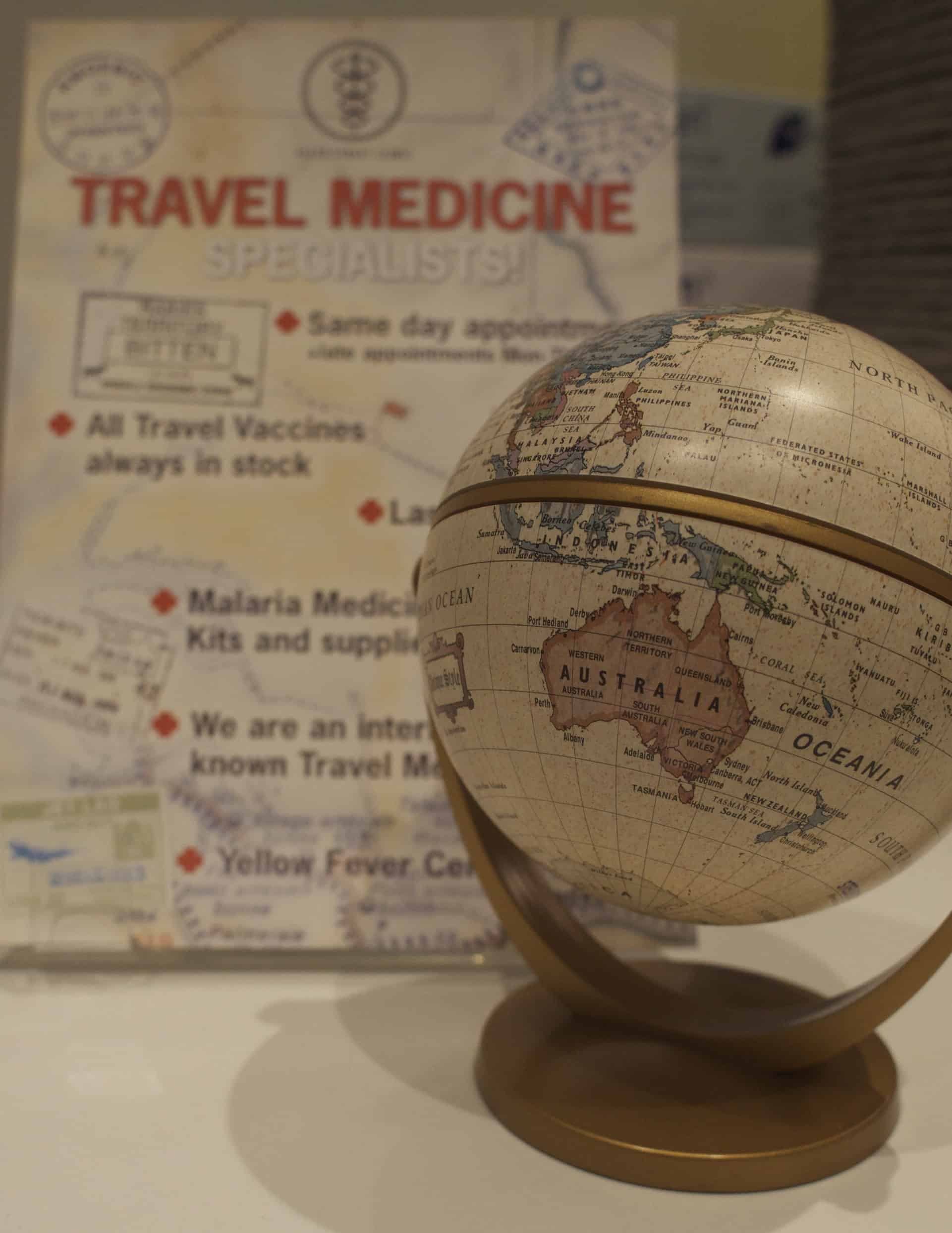
Is a travel consultation still necessary?
Yes, whilst it is fantastic news that Egypt is now malaria-free, there are other health risks to consider when travelling and it is still important to seek travel health advice from an expert.
We advise booking a travel consultation at least 4-6 weeks before your departure date to allow enough time for any necessary vaccinations, medications, and preventive advice to take full effect.
If you’re planning a last-minute trip, don’t worry! Book a consultation as soon as possible; even a brief appointment can provide valuable advice, essential vaccinations, and immediate preventive tips to keep you safe during your travels.
The Future of Malaria Control in the Region
Egypt’s success in eradicating malaria is a hopeful indicator for neighbouring regions where malaria is still a concern. The country’s strategies and investments in healthcare could serve as a model for other nations aiming to reduce or eliminate malaria.
Planning Your Malaria-Free Trip to Egypt
Whether exploring the pyramids, cruising the Nile, or enjoying the coastal resorts, travellers to Egypt now have added peace of mind regarding malaria. However, consulting with a travel health specialist before your trip remains important to ensure your overall health and safety. By staying informed and prepared, you can focus on enjoying the cultural and natural wonders Egypt has to offer.
As always, our travel health experts are here to provide personalised advice, vaccination guidance, and preventive health tips to make sure your journey is as safe and enjoyable as possible.
Book a travel consultation to discuss your upcoming trip to Egypt.
Related services at Fleet Street Clinic
Specialist Travel Clinic
Travel Vaccinations
Dengue Fever
Rabies Vaccination
Antimalarials
On 14th August 2024, the World Health Organization declared outbreaks of mpox in Africa to be a Public Health Emergency of International Concern.
What is mpox?
Mpox is a viral infection that was previously known as “monkeypox”.
It shares some similarities with smallpox, to the extent that smallpox vaccine may be cross-protective; however, the illness is much less severe. (Waning population immunity to smallpox, since vaccination programmes ended in 1980, is one possible reason for the increased tendency to outbreaks now.)
So far, there have been 14,000 cases reported in Africa, with 524 deaths. Sweden has just reported the first case of clade I mpox outside Africa in the current outbreak (see below).
Previously confined to central Africa, recent outbreaks have ultimately spread globally, which is why the WHO has now decided to urge a concerted global response.
How is it spread?
The infection is spread mainly by close direct / intimate contact with body fluids and secretions, and by sexual exposure.
It can also be spread by contact with animals, or their droppings, or by eating under-cooked contaminated meat – so-called “bush meat”. The animal reservoir of infection is mainly among rodents and non-human primates.
The illness
Infection may be symptomless, but in most cases, symptoms appear 7 to 14 days following exposure.
Mpox is characterised by blistering skin lesions that are often extremely painful (and highly infective to other people), occurring particularly on the skin, genitals and face. They can be sparse, or even single blisters.
Other symptoms include fever, chills, headache, muscle aches, fatigue and swollen lymph glands.
The blisters may appear first on the face, spreading to other parts of the body; or alternatively in the genital area if the infection was acquired by sexual contact. Extensive lesions around the mouth may make eating and drinking painful or impossible, requiring intravenous treatment.
The illness is considerably more serious in people with HIV infection or reduced immunity. Severity of infection is also linked to the degree of exposure.
Mpox strains
There are two strains (called clades – Clade I and Clade II) that differ in severity and ease of spread.
Clade II tends to be more severe (up to 1,000 times more virulent than clade II) and occurs in Central Africa, Clade II occurs mainly in West Africa and may sometimes be more easily transmissible. Mutations into sub-strains is also occurring, which makes testing more complicated, especially in countries where resources are poor.
Where are cases occurring?
It is important to bear in mind that official statistics generally underestimate true numbers of cases, since not everyone with symptoms seeks medical attention, and not all cases undergo full testing.
Laboratory-confirmed cases have been reported in:
- Burundi: over 100 cases (Clade Ib) throughout the country
- Central African Republic: 28 cases (Clade I) throughout the country
- Côte d’Ivoire: 6 cases (Clade II) in Abidjan and Bas-Sassandra districts
- Democratic Republic of the Congo: > 14,000 cases (Clades Ia and Ib) throughout the country, mainly in Équateur, Sankuru, South Kivu, and Sud Ubangi provinces
- Kenya: 1 case (Clade Ib) in Taita-Taveta County
- Republic of the Congo: > 120 cases (Clade I) throughout most of the country, mainly in Cuvette, Kouilou, Likouala, and Point-Noire departments
- Rwanda: 4 cases (Clade Ib); no specified locations
- South Africa: 24 cases (Clade IIb) in Gauteng (12 cases and 2 deaths), KwaZulu-Natal (11 cases and 1 death), and Western Cape (1 case) provinces
- Uganda: 2 cases (Clade Ib) in Kasese District; no secondary transmission has been reported
A previous outbreak in 2022 resulted in spread to over 40 countries – with over 30,000 cases in the USA, for example, mainly in the MSM community.
Are visitors at risk?
Although current news reports of mpox cases are alarming and intended to generate a global public health response, so as to raise awareness and help bring outbreaks under control, most tourists and travellers to Africa are not at risk.
Travel to Africa for the usual tourist activities (e.g. safari, outdoor activities, beach) should be unaffected by the outbreak.
Older travellers who have previously been vaccinated against smallpox may still have some additional cross-protection against mpox.
- Risk arises from close contact (especially sexual contact) with infected people.
- Those at highest risk are men who have sex with men (MSM).
- High-risk behaviour is easily avoided, and safe-sex precautions reduce the risk of infection.
- Risk also arises from close physical contact with infected animals, or by eating under-cooked bush meat – which should be avoided. (Thorough cooking kills the virus.)
- Healthcare workers may be at risk if caring for people who are ill with mpox
- Journalists and news media personnel should avoid physical contact, keep their distance and observe the usual hygiene precautions when reporting on the evolving mpox outbreak situation
Mpox vaccines and treatment
- In the UK, vaccination is available for MSM and healthcare workers via the NHS.
- Current vaccines protect against all strains.
- Vaccination within 14 days of possible exposure also appears to confer protection (post-exposure protection).
- Several antiviral drugs can provide benefit in the most severe cases.
More information:
Oropouche Virus Disease: A growing concern in Central and South America.
As of mid-2024, Central and South America are experiencing a significant outbreak of Oropouche virus disease, impacting countries such as Brazil, Bolivia, Colombia, Peru, and Cuba.
The Oropouche virus is primarily transmitted through the bites of infected midges (Culicoides paraensis) and mosquitoes. The virus is mainly spread in tropical and subtropical regions where these vectors are prevalent.
Symptoms of Oropouche virus disease include:
- sudden-onset fever,
- severe headaches,
- muscle and joint pain,
- rash,
- eye pain,
- nausea,
- and dizziness.
While most cases are mild and self-limiting, lasting 3 to 7 days, some individuals may experience more severe symptoms like meningitis and encephalitis.
There is no specific antiviral treatment or vaccine for the disease, so care focuses on symptom relief, such as rest, hydration, and pain management.
How to protect yourself from Oropouche virus
Preventing Oropouche virus disease involves reducing exposure to vector bites. Unlike mosquitoes, the main vector (midges) lacks a proboscis, and so is unable to bite through clothing.
Covering up, and wearing long-sleeved clothing, is therefore a keyway of preventing infective bites.
Other key measures include using plenty of insect repellent, impregnating clothing with Permethrin insecticide, using bed nets, and staying indoors during peak biting times.
Eliminating standing water where vectors breed is an important public health measure.
Prevention is key!
With no vaccine available, prevention remains the best defence against Oropouche virus disease.
Personal protective measures against insect bites also help protect against dengue, yellow fever, Zika, chikungunya, malaria, and a wide range of other tropical insect-borne infections, and should be followed carefully by travellers to tropical countries.
Cases found in Europe
Spain, Italy and Germany reported infections in numerous patients who had recently travelled to Cuba and Brazil.
The European Centre for Disease Prevention and Control (ECDC) warned of a moderate threat to travellers visiting Brazil, Bolivia, Colombia, Peru and Cuba, where Oropouche virus (Orov) is currently spreading.
If you’ve recently travelled to a known outbreak area and are experiencing any of the symptoms mentioned above, it is important to mention this to your doctor. This will help them rule out an Oropouche virus infection.
Worried about your upcoming travel plans?
Schedule a travel consultation with one of our specialist travel nurses.
They will guide you through potential health risks and recommend the necessary preventive measures and vaccinations to ensure your safety while travelling.
For more information on:
If caught and symptoms develop, rabies is almost invariably fatal.
Rabies is spread through the saliva of an infected animal and is present in over 150 countries worldwide. Up to 100 children die each day from rabies, and more than 55,000 people a year are killed from the disease, mainly in Asia and Africa.
If bitten or scratched by an infected animal you need to act quickly. Your pre-exposure vaccines simplify medical care in case of a potential rabies exposure, reducing the number of post-exposure vaccine doses needed and providing more time to seek medical care because your antibodies will start to respond. This is crucial when traveling to remote areas with limited access to medical facilities.
If you haven’t had pre-travel vaccinations, the treatment is much more complicated; it is also expensive and can be hard to access in lower income countries. If treatment is given correctly and promptly after exposure, it is 100% preventable.
It is extremely important that if you are travelling somewhere with a known risks of rabies it only seems sensible to protect yourself against it. Rabies is a vaccine-preventable disease, so make sure you get vaccinated before you travel.
For more information on rabies and travel health, visit our rabies page here.
The Fleet Street Clinic is passionate about travel. We have provided rabies vaccinations for over 20 years. Our team of expert travel medical professionals provide advice and detailed consultations to ensure you have a healthy trip.
You can book a travel consultation or rabies vaccination appointment online.
UTIs can strike unexpectedly, casting a shadow over an otherwise fantastic holiday.
Whether you’re a seasoned traveller or embarking on your first adventure, the risk of urinary tract infections (UTIs) is real and more likely to occur during travel, especially in hot countries.
This blog compiles expert advice and practical tips to empower you to minimise the chances of developing a troublesome UTI during your travels.
1. Stay hydrated
One of the simplest yet most effective ways to prevent UTIs is to stay well-hydrated. Proper hydration helps flush bacteria out of your urinary system, reducing the likelihood of infection.
Aim to drink at least eight glasses of water a day, and avoid excessive consumption of caffeinated and alcoholic beverages, as they can contribute to dehydration.
Bring a reusable water bottle and make a habit of refilling it throughout the day, ensuring you have access to clean and safe drinking water wherever you are.
2. Don’t delay going to the toilet
It can be tempting to “hold it in” during long journeys, delayed or remote travel but putting off going to the bathroom can cause UTIs.
Holding your bladder for too long can contribute to the growth of bacteria in your urinary tract. Since urination flushes bad bacteria out of the bladder before they get a chance to multiply to dangerous levels, going to the toilet as soon as you can means less bacteria are left to sit in your bladder for longer than necessary, reducing your risk of a painful infection.
Remember, maintaining good personal hygiene is crucial in preventing gynaecological infections, particularly UTIs and cystitis. When travelling, it’s essential to prioritise cleanliness. Carry antibacterial wipes to clean your hands before and after using public toilets.
3. Choose comfortable clothing
Believe it or not, your choice of clothing can impact your risk of developing UTIs. Tight-fitting clothes, especially in the pelvic area, can trap moisture and create an environment conducive to bacterial growth.
Opt for loose-fitting, breathable fabrics to allow proper air circulation. Additionally, change out of wet bathing suits promptly to prevent the proliferation of bacteria.
By paying attention to your wardrobe choices, you can significantly reduce the risk of developing uncomfortable infections during your travels.
4. Treat constipation
Exploring new cuisines can lead to various challenges for travellers. While some may grapple with traveller’s diarrhoea, others might experience constipation due to altered eating patterns, dehydration, increased alcohol consumption, and a more sedentary lifestyle.
Unfortunately, constipation increases your risk of contracting a UTI. To mitigate this risk, aim to eat a diet rich in fibre, stay active, and drink plenty of water.
5. Carry a female health kit with you whilst you travel
If you experience any symptoms of a UTI or gynaecological infection, it’s crucial to have medications on hand so you can continue your holiday or travel unaffected.
Carrying a female health kit with you whilst you travel means you can detect and treat your UTI symptoms whilst on-the-go. It contains urine test strips which can confirm if you have a urine infection as well as antibiotics and cystitis relief sachets to alleviate symptoms of inflammation.
Symptoms of a UTI may include frequent and painful urination, lower abdominal discomfort, blood in your urine, a high temperature or lower back pain.
Take our free online consultation to see if you can buy a female health kit online.
Remember, in addition to self-treatment, it’s crucial to seek prompt medical attention, especially if symptoms worsen.
Your travel experience should be memorable for all the right reasons, not marred by the discomfort of a urinary tract infection.
By following these essential tips – from prompt bathroom breaks, to arming yourself with the right travel medicine – you can significantly reduce the risk of encountering a UTI while abroad.
Our female health kits are designed for travel and contain everything you would need to treat and alleviate symptoms for a urinary or gynaecological infection. Begin by completing our free online consultation today.
Whether you’re prone to urinary tract infections, or have never experienced one before, it’s a good idea to buy a female health kit before any trip or holiday and arm yourself against the discomfort and misery of a UTI while abroad.
Fleet St. Clinic is here to support your well-being whilst you travel.
Stay healthy, stay informed, and make the most of your travels!
Related services available at Fleet Street Clinic
Dengue Fever has been in the news following two cases linked to travel to the Spanish island of Ibiza. This has sparked concerns about the spread of mosquito-borne illnesses in Europe, which is especially unusual for this time of year.
Dengue fever is a viral infection transmitted by the Aedes mosquito, which is found in tropical and subtropical regions worldwide. With rising temperatures and changing climates, there is a risk of mosquitoes and other disease vectors spreading to new areas, potentially causing outbreaks of diseases such as dengue fever.
The two cases of dengue fever in Ibiza were reported by the Spanish Ministry of Health and were both in residents of Germany who had visited the island before becoming ill. Each case was accompanied by two family members who were also suspected to have had dengue fever.
The risk of dengue fever in Spain is highest between the months of May and November, when mosquitoes are most active so to have cases at this time of year is uncommon.
So, why are we seeing cases outside of the usual infection months?
The reason is multi-facetted.
Our medical director and travel health specialist, Dr Richard Dawood explains:
“Firstly, there is the introduction or spread of mosquitoes to “pastures new” – places that might have been previously inhospitable, perhaps through temperature; or alternatively, that offer an environment with plenty of suitable breeding sites that they are suddenly able to take advantage of. These mosquitoes can bring disease with them, or can spread it around if there is a reservoir in the local population.
Secondly, there is the possibility of introducing disease to a vector population that is already established, ready and waiting. This is exactly the (long-standing) concern with yellow fever. There are mosquito species in Asia, for example, that are easily capable of spreading yellow fever were it to be introduced by an infected traveller – which is why Asian countries are so careful to insist on proof of yellow fever vaccination from travellers arriving from the endemic zones of Africa and South America. Asia is yellow fever-free, and wants to remain so. However, this type of introduction has already recently happened in Australia, where Japanese encephalitis (a virus infection that can cause rare but serious complications in humans) has recently established a reservoir of infection in farm animals, that may be impossible to reverse. It is also happening with Lyme disease spreading gradually into parts of Europe (and the UK) with a susceptible tick population.
Similar concerns apply to Zika – there is very large potentially susceptible mosquito population that could spread the virus in many tropical countries, if introduced; dengue fever; and also potentially malaria, in parts of the world that have been the target of successful elimination campaigns, but where mosquito populations could still spread it, were it to be reintroduced, if control measures are neglected or ceased.
With changing climates, a valid concern about global warming is that it could create conditions in which populations of mosquitoes and other vectors thrive and spread – hence the crucial importance of vigilance, surveillance, and early action if needed.”
How can you protect yourself from Dengue Fever?
QDENGA, Dengue Fever Vaccination
Relatively new to the UK, QDenga is a new travel vaccine that can prevent dengue fever.
The course consists of two doses, given three months apart, and provides long lasting protection.
Learn more about QDENGA, Dengue Fever Vaccination
Book a travel consultation for your Qdenga vaccination.
Avoid Mosquito Bites
In addition to vaccination, the best way to protect yourself against dengue fever is to take measures to avoid mosquito bites. This includes wearing protective clothing, using mosquito repellent, and staying in places with air conditioning or screens on windows and doors.
If you develop a high fever during or after travelling to an affected area, seek medical advice as soon as possible and provide details of your recent travel history. Dengue is often also accompanied by a rash and joint or muscle pain.
In conclusion, rising temperatures and changing climates have the potential to create conditions in which populations of mosquitoes and other disease vectors thrive and spread. It is crucial for public health authorities to remain vigilant and take early action if needed to prevent the spread of diseases such as dengue fever.
By receiving the Qdenga vaccine and implementing effective measures to prevent mosquito bites, travellers can lower their personal risk of contracting Dengue Fever, along with other insect-borne diseases.
If you’re considering Qdenga before your next trip, book a travel consultation with one of our specialist travel nurses.
Related services available at Fleet Street Clinic
QDENGA, Dengue Fever Vaccination
Suitable Medical Kits available to buy online
Related Online Consultations
Female Travel Health Kit: Start Consultation
Travelling can have a significant positive impact on one’s physical and mental health, according to a study published in the Journal of Travel & Health. The study surveyed over 1,000 adults who had recently returned from a trip and found that the majority of them reported improvements in overall well-being, including increased energy and reduced stress levels.
One of the key reasons for these self-rated health benefits is that travelling allows individuals to step out of their daily routine and experience new environments and cultures. This can lead to increased physical activity, as travellers may be more likely to walk or bike instead of drive which may also expose them to different types of food, leading to a healthier diet.
Additionally, travelling can have a positive impact on mental health as well. The study found that the majority of participants reported feeling more relaxed and less stressed after their trip. This is likely because travelling can provide a sense of excitement and adventure, as well as a break from the demands and responsibilities of everyday life.
Another benefit of travelling is that it allows individuals to build new social connections, which can be important for mental health. Meeting new people and forming new friendships can provide a sense of belonging and can also help to reduce feelings of loneliness and isolation.
In conclusion, the study suggests that travelling can be good for one’s physical and mental health. It can help to increase energy levels, reduce stress and improve overall well-being. So, next time you are planning a trip, remember it’s not only good for your soul but also for your body.
To read the full study, continue reading here: https://www.sciencedirect.com/science/article/pii/S2214140522002079?via%3Dihub
Related services available at Fleet Street Clinic:
- Travel Vaccinations
- Jet Lag Calculator
- Travellers’ Diarrhoea Online Consultation
- Antimalarials
- DVT Rick Calculator
Fear of flying, otherwise known as aerophobia, is an excessive worry about air travel. It is one of the most common forms of phobia and according to YouGov, around 24% of Brits have some form of anxiety about getting on a plane.
People suffering from fear of flying experience extremely anxious thoughts which are often so powerful they become physical symptoms. These can include shallow breathing, experiencing chest tightening, sweaty palms, feeling nauseated or lightheaded and sometimes these even develop into a panic attack, meaning many opt to avoid air travel altogether.
For some, it will have been a lifelong problem that has meant never flying at all. For others, who have flown many miles in their lifetime, it is a problem that slowly creeps up on them over time. In both circumstances, the fear can be debilitating and symptoms often trickle into other areas of life.
Like all phobias, there is little logic to support the anxiety that it causes – travel is in fact the safest form of transport and you are much more likely to die from a car accident than in a plane crash. Knowing that fact does little to ease the flying-related anxiety of an aerophobic sufferer.
So, what can be done to overcome our fear of flying?
Understand the reason why you’re a nervous flyer
Fear of flying is usually caused by a combination of factors. Understanding the root cause of your own phobia is perhaps the first step in overcoming it. Is it a fear of heights? Claustrophobia? Was it that film you watched as a child? Or has a particular world event sparked the fear? Many people suddenly developed a fear of flying after 9/11 for example. Figuring this out will then allow you to tackle it in the right way and using the appropriate techniques.
Fight fear with knowledge
Some experts suggest the first strategy for everyone suffering from a fear of flying is learning about the aeroplane and the science behind flight. Our anxiety is fed by ‘what if?’ catastrophic thoughts. Once you become knowledgeable, your ‘what if’ thoughts will be limited by the facts. There are professionally designed courses that will explain aspects like air traffic control, anti-terrorism measures, and what happens during turbulence. Some courses use Virtual Reality (VR) to simulate a flight, explaining everything along the way with the aim of injecting logic into an illogical fear.
Seek medical help for anxiety, fear and panic
From here, a form of therapy may help to identify and break anxiety cycles. There are many different types of therapy and choosing the right one for you will depend on your own needs and goals. Hypnotherapy and cognitive behavioural (CBT) are some of the most commonly used, but there are countless more to choose from. Deciding which is the most appropriate form of therapy can be daunting, so it may be helpful to seek advice from your GP or a travel nurse.
For those who manage to make it onto the plane, there are quite a few, simple personal techniques that can be used to calm your nerves.
Deep breathing techniques
Making a conscious effort to breathe slowly and deeply can interrupt panic. Deep breathing is known to trigger a comfort response and will help prevent hyperventilation.
Distract yourself
Reading a book or listening to a good podcast can refocus your mind and attention.Distracting yourself from the fact that you are flying can be a great way to keep calm if you’re a nervous flyer.. Time tends to pass much more quickly when adequately distracted.
Tell the flight attendants
Alerting the flight attendants of a nervous flyer could also help – with their training and expertise, they are ideally placed to provide reassurance and will regularly check in on you during the flight.
Avoid coffee and wine
Nervous flyers in general should avoid drinking coffee and wine before and whilst flying. Both can leave you more dehydrated than normal. The extra caffeine in coffee can aggravate anxiety issues and the Dutch courage wine offers will pass leaving you more susceptible to jet lag. Stick with water where possible.
Tea really does help
It’s very British to recommend tea to make everything better, but there are many different herbal teas available which can help with relaxation, reducing stress and calming anxiety. Peppermint, camomile, lemon balm and lavender teas are the most commonly used.
We advise nervous flyers and people with aerophobia to seek further information and guidance from their GP who will be able to make a formal diagnosis and treatment options.
For more advice and information you can book a travel consultation appointment.
Botswana is one of the greatest safari destinations.
The Okavango Delta offers exceptional opportunities to view wild creatures and birdlife. Elephants roam freely and herds of buffalo crowd around the winding waterways the river. The stark and desolate landscape of the Kalahari desert can be found in the south with the longest unbroken stretch of sand there is. Whatever your itinerary, ensure you follow our top travel tips.
Vaccines
All travellers should ensure they are up-to-date with their routine vaccinations including measles, hepatitis A, typhoid, diphtheria-tetanus and polio (DTP). You may want to consider getting vaccinations for rabies and hepatitis B as well. Both these diseases are classed as high-risk in Botswana. We would advise you to speak with a travel nurse ideally 4-6 weeks before travel. At this appointment, you can discuss where you’re going and what you plan to do. They can then advise you of all the recommended vaccinations you should consider.
Find out more information about our travel and wellness vaccinations.
Malaria
There is a high risk of malaria throughout the year in the northern areas of Botswana including the Okavango Delta, Chobe and Moremi. There is a low risk of malaria in the rest of the country including the central Kalahari, Gaborone and Gemsbok. Individuals travelling to hight risk regions are advised to take anti-malarial medications to prevent the disease. As well as taking precautions against mosquito bites. The mosquitoes that spread malaria predominantly bite at night. For that reason, it is essential you sleep under a mosquito net.
Insect prevention
All travellers need to take extra precautions against insect bites. Mosquitoes, ticks, mites and lice are able to spread diseases such as African tick bite fever, dengue fever, filariasis and myiasis. Travellers should wear good insect repellent with at least 50% DEET and try to cover up with long loose clothes. You can add extra protection to your clothes by treating them with an insecticide. We would recommend using a permethrin spray.
See our Ultimate Bug Kit.
What about Yellow Fever?
The is no risk of Yellow Fever in Botswana. It is therefore not recommended that travellers get vaccinated. Travellers may require a valid Yellow Fever Certificate if they are entering Botswana from a country that has yellow fever, or who have transited through a country with a risk of yellow fever.
First Aid Supplies
Areas of Botswana can be remote, and access to medication and first aid supplies can be limited. Packing a good basic first aid kit is a good idea to help treat minor injuries and illnesses. Basic items such as anti-histamines, pain relief and medicines to treat upset stomachs are useful. Likewise, pack small dressings, plasters and antiseptic cream to treat minor scrapes and scratches. If you take prescription medication to ensure you pack sufficient for your trip and carry a record of the medication with you.
Book your travel appointment today
By Anna Chapman | Travel Nurse | October 2019
Greenland is home to truly magnificent mountainscapes and glaciers.
Jakobshavn Glacier, the world’s fastest-moving glacier in the Northern Hemisphere can be found here.
In the Winter, tourist travel to this wonderland to potentially see the wondrous the Northern Lights. Things are quite different in the Summer.
Chasing the Midnight Sun
Summer in Greenland is an image not often associated with the country. Summertime offers eternal light in the land of ‘The Midnight Sun’ whereby the day has neither a beginning nor an end. Those wanting to experience this time-shifting experience must travel north or the Arctic Circle. The low-lying sun makes the surrounding scenery appear almost dreamlike; icebergs and hilltops are bathed in a surreal palette of pink, purple, yellow and red. Travellers to Greenland have options of hiking the land or sailing the fjords between icebergs.
If you plan to travel to Greenland this summer follow our top travel tips to ensure you stay healthy.
Vaccinations
Even though Greenland resides in the Arctic Circle, travellers should still ensure they receive appropriate pre-travel vaccinations. This includes being up-to-date with Measles, diphtheria-tetanus and polio. Greenland has a high risk of Rabies, a virus spread through the infected bite of a mammal. Travellers who plan to trek inland may wish to consider this vaccination before they travel to reduce the risk.
Suncare
Despite Greenland having long, dark winters, the summer months provide almost constant light. Bright sun, combined with the effects of lights reflection from snow and water can increase the risk of sun damage from UV light. Despite temperatures remaining cold, travellers still need to be sun smart. Ensure you wear a high factor SPF, and use lip balm to prevent cracking. Polarised sunglasses that wrap around will prevent the UV rays causing damage to your eyes.
Sea Sickness
Many activities in Greenland involve taking to the water and visiting the infamous Disko Bay in search of Icebergs. Sometimes the seas can be rough which can make for a miserable time if you are prone to travel sickness.
Sea Sickness can be reduced by:
-
Sit in the centre of the boat where the motion will be less aggressive
-
Close your eyes or focus on a point on the horizon, this can help your inner ear balance.
-
Avoid alcohol and large heavy meals, instead, keep hydrated on water and eat smaller lighter meals
-
Sucking on a mint or ginger sweet can help with nausea
-
Seas Sickness medication tablets
-
Patches that can be used to prevent sea-sickness
Trekking
Parts of Greenland can be remote so taking a good First aid kit with you is essential. Basic provisions include pain relief, plasters and medication to treat an upset stomach, such as loperamide and oral rehydration salts. If you take prescription medication to ensure you pack enough and carry the prescription with you. If you plan on trekking the hinterland, pack additional items such as blister dressings and plasters.
Book your travel appointment today
By Anna Chapman | Travel Nurse | July 2019
June to September is the best months to trek to Machu Picchu, although you can visit all year round. The weather is at its driest and coolest with gloriously sunny days. Trekking to the roof of the Andes is a rewarding experience that many travellers to Peru sign up for. Travellers who are trail-blazing their way on the Inca road to catch a glimpse of the forgotten city should follow our top travel tips to ensure they stay healthy on the road.
Vaccinations
All travellers to Peru should ensure that they are up-to-date with measles, diphtheria, tetanus and polio (DTP), and have received vaccinations against Hepatitis A and Typhoid. There is a risk of Rabies and Hepatitis B in Peru, and all travellers attempting the Inca Trail should consider vaccinations against these.
There is no risk of Yellow Fever on the Inca Trail or Cusco. However, the vaccination may be recommended to travellers who are doing further travel in Peru, such as the Amazon rainforest. Those planning to extend their trip to South America may require the Yellow Fever vaccination for personal protection. Additionally, you may require a valid yellow fever certificate to enter some other countries. It is best to book in a travel consultation with our specialist travel nurses to discuss your route.
Altitude Sickness
The highest altitude of the Inca trail is 4,215m, a whopping 1,800m higher than Machu Picchu itself! Most people start the hike from Cusco which lies at 3,400m, meaning trekking this wonder of the world poses a real risk of altitude sickness. Altitude sickness is unpleasant and can develop into something serious and become life-threatening. It is best avoided by taking time to acclimatise. Ideally, if you are arriving from sea level, spend a few days in Cusco before your trek begins to adjust to the different altitude. Choose a longer trek, a slower ascent over more days will reduce your risk considerably. Alternatively, you can get a prescription of acetazolamide (Diamox) to aid the process. Speak to a specialist travel nurse about this at your pre-travel consultation. Don’t let altitude sickness ruin your trip.
Stay Hydrated
Treks on the Inca trail usually last around 5 days, meaning that an average trekker will probably consume at least 15 litres of water over the course of their trek. Unclean and unsafe drinking water can lead to sickness and diarrhoea so it is important that travellers have access to safe water. Carrying 15 litres of water on the trail is a near impossibility so travellers should ensure that they have a way to make water safe to drink. Carrying water purification tablets, or a bottle with a filter can ensure you have access to safe drinking water throughout.
Travellers Diarrhoea
Travellers diarrhoea and other common gastrointestinal infections can put a dampener on any adventure but especially when hiking. Access to toilets is likely to be limited throughout your journey so it is important to stay healthy. Ensure all food you eat is thoroughly cooked. Pack an alcohol hand gel so you can keep your hand clean before you eat and after using the toilet. It is wise to carry medication with you, so, if you do become unwell you have doctor-approved medication available to take. We recommend packing one of our Worldwide Gastro Kits. Inside there is medicine to prevent and treat travellers diarrhoea, dehydration, mild infections, nausea and vomiting. Hopefully, you won’t have to use this kit, however, for peace of mind, it is better to be safe than sorry.
Foot Health
The Inca trail typically consists of between 6-9 hours of walking a day, with shared tent accommodation. Hiking the Inca Trail through the Sacred Valley to Machu Picchu is both arduous and awe-inspiring. Make sure you have good walking boots that are broken in before you start. Book an appointment with a podiatrist and osteopath if you have any niggles or pain before setting off. Take care of your feet throughout your adventure – keep them clean and dry to avoid problems. Any blisters should be cleaned and covered with a dressing to prevent pain and infection. Pack your own first aid kit with some basic medications for pain, allergies and upset stomachs in case you do become unwell. Access to medical supplies will not be until Aguas Calientes at the end of the trek. You can buy a Fleet Street Clinic Essential First Aid Kit online to save you the hassle of assembling yourself. We would recommend considering a medical pedicure upon your return. Treat our feet a little bit of TLC for taking you on an adventure of a lifetime.
We would encourage all those taking on the Inca trail adventure to consider booking a travel consultation with either myself or another of our specialist travel nurses. We all have extensive knowledge on what vaccines and health precautions you should take on an individual basis to remain healthy throughout your adventure. Chances are at least one of us has done a similar adventure so we can give you some first-hand experience on what to expect too!
Book your travel appointment today
By Anna Chapman | Travel Nurse | July 2019
Uzbekistan is home to spellbinding architecture and ancient cities. In terms of sights alone, Uzbekistan is Central Asia’s biggest draw and most impressive showstopper. Fabulous mosques, medressas and mausoleums are just some of the pulls for tourists when visiting Uzbekistan while more eccentric views can be seen at the fast disappearing Aral Sea and Nuratau Mountains.
Travel Nurse, Anna, shares her top tips on how to stay healthy during your trip to Uzbekistan.
Vaccinations
Ensure you are up-to-date with your travel vaccinations. The minimum advised for a trip to Uzbekistan is diphtheria tetanus and polio, and Hepatitis A. Typhoid, Hepatitis B and Rabies can be considered by some travellers. It is advisable to attend for a pre-travel assessment with a travel nurse 6-weeks before your trip as some vaccinations requires several injections to complete the course.
Food and water
Precautions against the dreaded traveller’s diarrhoea should be taken to prevent an upset stomach ruining your trip. Do not drink tap water in Uzbekistan, stick to bottled water or water that has been boiled. If you are trekking or visiting remote areas it’s a good idea to take either a water bottle with a filter or some chlorine dioxide tablets to make water safe to drink, should you not be able to find a shop with bottled water.
Sour milk dishes dominate the Uzbek cuisine. Cue caution if you want to try ‘kurt’, the famous fermented cheese balls. There is a risk of a bacterial disease called brucellosis that can be spread through unpasteurised dairy products such as cheese and milk.
Travelling further afield
Uzbekistan forms one of the countries on the old silk route. If you plan on a tour of the ‘Stans’ or attempting the whole Beijing to Istanbul route, you may need to consider other travel health precautions. Depending on your route, and also the time of year you intend to travel, you may wish to consider vaccinations against Tick-Borne Encephalitis and Japanese Encephalitis.
Altitude
Khazret Sultan, Uzbekistan’s highest peak stands at 4643m. Many popular walking and hiking routes such as Big Chimgan exceed over 3000m, making altitude related illnesses a hazard. Tips for reducing altitude sickness include a slow ascent route, keeping hydrated, ensuring that your sleeping altitude doesn’t exceed 500m per day. Diamox (acetazolamide) is a prescription medication that can reduce the symptoms of altitude related illness.
Book your travel appointment today
By Anna Chapman | Travel Nurse | April 2019
Stay healthy at Holi
Holi is a famous spring Hindu festival that is celebrated in every part of India. It is known as the festival of colours and is mostly celebrated in March in Rajasthan.
The celebration signifies the beginning of spring beginning and the end of winter. It is sometimes known as the “festival of colours” or the “festival of love”. During the festival, it is encouraged to throw powdered paint (gulal) into the air. This symbolises the abundance of colours of spring and the celebration of a new season.
Here are top travel tips to stay healthy at Holi.
Don’t forget your travel vaccinations
Travellers going to India should ensure they are up-to-date with their travel vaccinations. These include Hepatitis A, Typhoid and Diphtheria, Tetanus and Polio. Rabies, Hepatitis B and Japanese Encephalitis are sometimes suggested and are dependent on where you’re travelling to and the activities you plan to do there. A consultation with a travel nurse will provide you with all the information needed to make an informed decision either way.
You can find more about vaccinations on our travel and wellness vaccine pages.
Eat, drink and be merry…
India is food heaven but don’t let travellers diarrhoea turn it into a Holi holiday hell. Avoid tap water or ice from an unknown source. Ensure bottled water has an intact seal if buying from a vendor. Alternatively, invest in a water-to-go bottle which has a built-in filter making unsafe water safe to drink. You can pick one up during a travel appointment at the clinic whilst getting your vaccines.
Eat well-cooked food served piping hot, and avoid fruits and salad items that might have been washed in the local water. It is worth investing in a gastro medical kit which contains all the necessary medicines should you get sick at any point during your travels.
Colour vision…
Holi festival is synonymous with the throwing of coloured powder. Contact lens wearers should stick to their glasses during the festival so to avoid getting dye in their eyes. Any dye that makes its way into your eye could cause a chemical injury and lasting damage. If any powder does get in your eye, wash it well with clean running water.
Don’t let the dye stop the DEET.
Dengue fever, chikungunya, Zika, Japanese Encephalitis and even malaria can occur in parts of India. Therefore, banish the bugs bites by covering up as much as possible, wearing a good insect repellent with at least 50% DEET. See our Ultimate Bug Kit.
If you are trying to conceive, travelling to ‘at-risk countries’ is not advised.
For more information on the Zika virus and advise, you can speak to one our travel nurses during a travel consultation.
We’d always recommend for travellers to book a 30-minute travel consultation with a travel nurse prior to travelling to ensure all necessary vaccinations are given and any risks are discussed.
Book your travel appointment today
By Anna Chapman | Travel Nurse | February 2019
Dr Richard Dawood, Medical Director of Fleet Street Clinic, was featured in an article published in The Telegraph: ‘Is there a doctor on board? What really happens during a medical emergency at 35,000 feet’.
The article discusses the issue of a medical emergency in the air, and Dr Dawood recounts some of his experiences where his medical expertise has been required during a flight.

Dr Dawood shares how he is happy to volunteer if a doctor is required, and details his experience of caring for a cabin crew member after she was taken ill during an 11 hour flight to Toyko. As an eminent Travel Medicine specialist, Dr Dawood is accustomed to helping with all kinds of travel-related health issues both pre and post travel, and as the article demonstrates, sometimes during travel as well!
As founder of Fleet Street Clinic, Dr Dawood has developed a multidisciplinary medical practice with a strong focus on Travel Medicine. If you require a travel appointment, you can book online.
The Zika Virus has been making headlines recently for it’s frightening links to rare birth defects. Brazil has even gone as far as to warn women to avoid falling pregnant whilst an epidemic is rife. The link between 400 cases of new-borns with microcephaly in the north-east of Brazil is being investigate by health authorities.
The increase in microcephaly, a neurological disorder that stunts the growth of the baby’s cranium, limiting it to a circumference of less than 33cm, has increased in Brazil from 59 cases in 2014, rising to 1,248 cases throughout 2015. Typically, life expectancy for babies born with the condition is reduced. In 90% of cases, brain function is also reduced. There are currently no travel restrictions in affected areas.
How is the virus contracted?
The Zika virus is spread to people through the bite of an infected mosquito. Outbreaks have been seen across Africa, Asia, Central and South America.
What are the the symptoms and treatment?
The common symptoms, usually mild and often lasting from a few days to one week, can be a rash, fever, joint pain, and conjunctivitis. There is currently no vaccine to prevent or medicine to treat the virus. Pain killers can be used to alleviate these symptoms which often go mistaken as a fever, and can easily be missed, especially in the early stages of pregnancy.
Is there a way to reduce my risk?
Insect bite precautions is paramount, especially for pregnant women in the affected areas. The NHS travel website, Fit For Travel, recommends:
- Covering up – wearing long sleeved tops and long trousers
- Spraying thinner clothing with insect repellent
- Burning pyrethroid coils and heating insecticide impregnated tablets
- Sleeping in a screened room where possible or using a treated mosquito net
If you are travelling to Brazil or any of the infected areas, book an appointment with one of our dedicated Travel Clinic nurses for information on vaccines and travel wellbeing now on 020 7353 5678.
Zika Virus – Additional Resources
Zika virus: medical advice for travellers – The Telegraph – Richard Dawood
Zika Virus – Video
Watch Fleet Street Clinic’s Dr Richard Dawood discuss Zika Virus on Victoria Derbyshire.