Month: May 2018
Shringrix now in stock
We are pleased to say we have secured a limited stock of Shingrix at Fleet Street Clinic. These are the first doses to become available in the UK and have been specifically imported from other EU markets.
Globally, this vaccine is in extremely short supply and full supply is unlikely to be able to meet the demand for a number of years. This is even the case in the USA, where the vaccine was first launched since the vaccine has been recommended for routine use in over 50’s. There is unlikely to be an NHS program for the foreseeable future.
‘We believe we are the first medical practice in the UK to be able to offer our patients the new Shingrix vaccine, which provides powerful protection against a deeply unpleasant disease. As a full service medical practice with a longstanding commitment to cutting edge care, this follows an established tradition of UK vaccine “firsts” – including HPV for both sexes, Meningitis B, Zostavax, and Quadrivalent Flu.’
– Richard Dawood, Medical Director
What is Shingles?
Shingles, also called herpes zoster, is a painful skin rash caused by the chickenpox virus (varicella-zoster virus).
After you’ve recovered from chickenpox, the varicella-zoster virus lies dormant in your nerve cells and can reactivate at a later stage when your immune system is weakened. Anyone who has had chickenpox can get shingles.
Who can get Shingles?
While you can get shingles at any age, the odds start climbing at 50, then more sharply with each decade. As your immune system weakens with age, that puts you at an increased risk for shingles.
Your risk for shingles increases as you age. Previously we had recommended the Zostavax vaccination for shingles; which is still available. The difference in vaccinations being, Zostavax is only around 50% effective in preventing shingles, but Shingrix efficacy is up to 90% in preventing shingles and it’s complications.
Shingrix Vaccination Schedule…
The primary vaccination schedule consists of two doses of 0.5 ml each: an initial dose followed by a second dose 2 months later. If flexibility in the vaccination schedule is necessary, the second dose can be administered between 2 and 6 months after the first dose.
> Due to the scarcity of the vaccine, we recommend all those having the Shringrix vaccination to prepay for the second dose in advance.
At Fleet Street Clinic, we have seen a rise in the number of women opting to use the coil as their contraception of choice.
We have 2 options available, the Copper IUD and the Mirena IUS. Both options are fitted into the womb and are 99% effective against unwanted pregnancies, working straight away.
The main difference between the IUD and the IUS is what it releases into the womb. The IUD releases copper and the IUS releases the hormone progestogen. In most cases, the choice is down to personal preference but you can speak with our nurse/ GP in your appointment if you’re undecided which option you’d prefer.
The coil is a popular choice as it works straight away after insertion, it doesn’t interrupt sex and doesn’t interrupt other medications. In addition, for those who’re planning a family, once removed, it is possible to get pregnant straight away. It is also safe to use if planning on breastfeeding.
The coil requires a removal and replacement after a set time period and is dependant on the type of coil fitted.
- Copper IUD – Lasts for 5 to 10 years before replacement.
- Mirena IUS – Lasts for 3 to 5 years before replacement.
Your coil can be removed at any time by a trained doctor or nurse. Find out more about the contraceptive coil.
We strongly believe that women shouldn’t have to wait unnecessarily to have a coil either fitted or removed.
Copper IUD Coil Fitting is £375*
Duration: 45 minutes
Mirena IUD Coil Fitting is £375*
Duration: 45 minutes
Coil Removal is £195*
Duration: 30 minutes
All examinations are carried out by a female doctor in a comfortable and private setting.
Book your Coil Appointment Online
*Pricing is subject to change, this is based on 2021 clinic pricing and includes appointment fee.
Measles: Don’t Get Caught Out
Cases of measles have risen rapidly in recent months in Europe, United Kingdom but most recently, Brazil. Measles is a highly contagious virus with potential for serious complications. It is a serious viral infection, spread by airborne droplets and is highly infectious. It is recommended that two doses of the measles vaccination should be given to individuals to prevent infection. Although many countries include the vaccination as part of the routine childhood immunisation schedule, international travellers should check that they are immune before departure.
Most UK citizens will have immunity in one of two ways:
Natural immunity can be assumed for those born before 1970, where individuals would have been exposed to the infection naturally.
Having received two doses of vaccination against measles. The vaccination was introduced in 1970 and is usually given in combination with rubella and mumps as the MMR vaccine.
Initial symptoms can include:
- Runny nose
- High Temperature
- Spots in the mouth
- Aches and pains
- Sore eyes and swollen eyelids
A rash appears after 2-4 days which can present as blotchy spots, often starting at the head and progressing down.
Advice for Adults
If you are in doubt about whether you have immunity to measles, a simple blood test can be taken to determine your immunity status. If you have no immunity to measles, you can be offered the MMR vaccination.
Advice for Children
Infants normally receive the MMR vaccination at 13 months old, as part of the national schedule. However, if you are travelling to a country where there is a significant risk of infection, the vaccination can be given to infants from 6 months.
Medical Advice
If you think you may be suffering from measles, or are concerned about the risk of infection when travelling, please see your doctor straight away.
The Fleet Street Clinic stocks travel sickness medication, travel vaccines and medical travel kits. Our experienced travel clinic nurses can help advise with any queries or more information on Measles.
Fleet Street Travel Clinic
Shingles Vaccine Now Available at Fleet Street Clinic
We are pleased to tell you that the Shingles Vaccine (Zostavax) is now in stock at Fleet Street Clinic.
This vaccine is given as a single dose and costs £170 plus a £20 appointment fee.
To Book
For further details and appointments call us today on 0207 353 5678, email us at info@fleetstreetclinic.com or book an appointment online here.
Zostavax will eventually be superseded by a newer and more effective vaccine (Shingrix), but unfortunately, this is not likely to become available in the UK in the near future. Zostavax is therefore recommended for anyone needing protection in the interim until the new vaccine becomes available.
Travel Tips for a Kenya Trip of a Lifetime
Wandering with wildebeests this summer?
The spectacular wildebeest migration sees over 2 million animals traverse the plains of the Serengeti National Park in Tanzania into the Masai Mara Reserve in Kenya. The best time to witness this breathtaking event this year is in June.
If you’re planning to travel to East Africa this summer, here are our top tips for staying healthy:
- Be sensible with food and water to avoid travellers’ diarrhoea. See our worldwide gastro kits.
- Take a small first aid kit with you for minor injuries and illnesses, including medications for upset stomachs. Parks can often be located far from medical help and have medical facilities with varying health standards.
- Although the main attraction on a safari is the wildlife, remember that rabies exists throughout Africa. Whilst most cases result from dog bites, all mammals have the potential to transmit the virus, and treatment can be difficult to obtain. It is advisable to obtain vaccinations prior to travel.
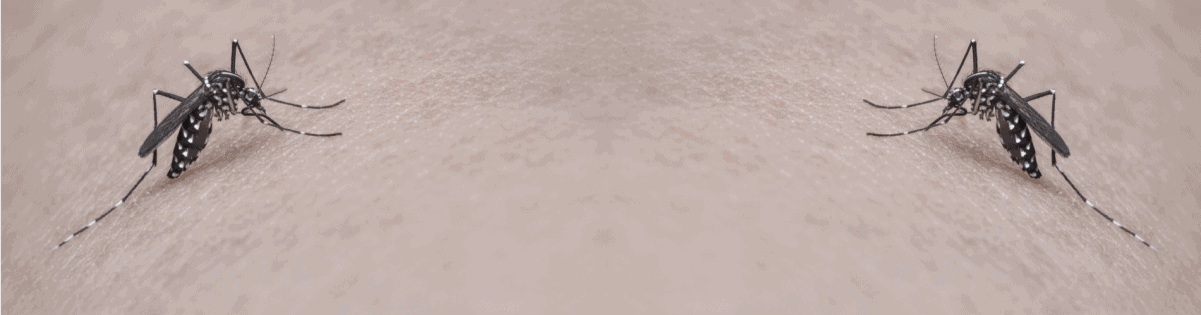
- Mosquitoes and insects are ubiquitous in game parks, especially around watering holes. They carry diseases such as malaria, dengue fever, leishmaniasis and sleeping sickness. Take precautions against insect bites by covering up with long loose clothing, wearing insect repellent and sleeping under a mosquito net at night. You can also purchase our Ultimate Bug Kit.
- With Kenya lying on the equator, the sun’s rays are extremely powerful. Be sun safe by wearing a high factor sunscreen, sunglasses, and hat.
- Wear light, long-sleeved clothing. Avoid dark clothing – Tse Tse flies are attracted to dark blue colours and can cause sleeping sickness.
- Ensure you receive your pre travel vaccinations which should include Diphtheria, tetanus and polio (DTP), Hepatitis A and Typhoid, Rabies, Hepatitis b.
- Don’t forget to take malaria tablets as all of Tanzania poses a risk of malaria.
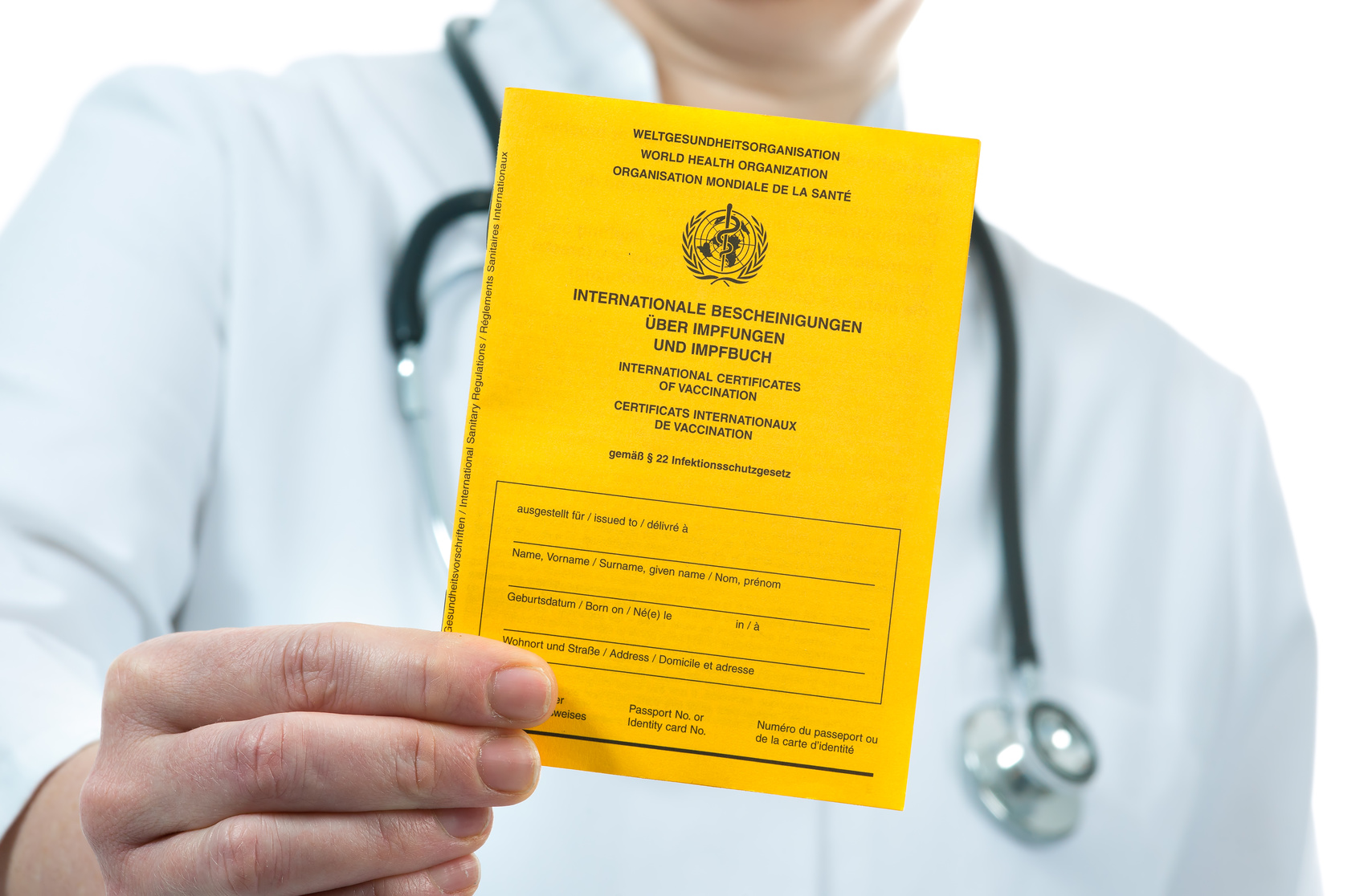
- Whilst the Yellow Fever vaccination is not usually recommended for travellers to Tanzania, it may be recommended for parts of Kenya. Additionally , travellers may need to present proof of the vaccinations on entry, depending upon their flight route and countries travelled. Ensure you get up to date advice.
Fleet Street Travel Clinic
By Anna Chapman | Travel Nurse | May 2018
Tick-borne encephalitis in Sweden
The summer months are great for exploring Scandinavia. What many people don’t realise is that vaccinations against Tick-borne encephalitis should be considered if your travel plans take you out into the countryside. If you plan on spending time in forested areas, particularly around Gothenburg, Upland, Sodermanland and the Islands around Stockholm, you could be at risk of the disease.
What is Tick-borne Encephalitis (TBE) ?
TBE is a viral infection that affects the central nervous system. It is spread via the bite of a tick, or by ingesting unpasteurised milk and dairy precasts from animals that carry the diseases. Transmission season is usually in the summer months between April and October. There is an effective vaccination available against tick borne encephalitis to prevent the disease. It requires 2 vaccinations 14 days apart with a booster dose given 1 year later.
Other countries that have a risk of the disease include Eastern and Western Europe, Russia, Finland, China and Japan.
In addition to the vaccination, preventing tick bites is really important, especially if you plan to do outdoor activities such as camping, hiking in rural areas during transmission seasons.
Prevention
You can prevent ticks by:
- Wearing DEET insect repellent with a minimum of 50% DEET concentration.
- Wearing long trousers and tucking them into your socks, and shirts with long sleeves.
- Treating clothes with permethrin.
- Inspecting your body for ticks and removing them promptly.
- You can purchase out Ultimate Bug Kit.
All travellers going to Sweden should ensure that they are in date with their routine immunisations including diphtheria, tetanus and polio (DTP) and measles, mumps and rubella (MMR).
Some travellers may be recommended to be vaccinated against Hepatitis A and B.
Although rabies is not present in terrestrial animals in Sweden, bats can still carry the virus. Those travellers who plan on exploring caves, such as in Abisko in Lapland may wish to consider being immunised against rabies prior to travel.
Fleet Street Travel Clinic
Just back from…East Timor
Our travel clinic nurse Anna has been travelling in East Timor, the South East Asian nation inhabiting half of the island of Timor, which became independent from Indonesia in 2002. Here, Anna shares with us her top travel health tips from the area.
Exploring East Timor
East Timor is ringed with rugged beaches and pristine coral reefs. It is one of the most exciting places to dive in the world.
Battling the bugs
In terms of insect borne diseases, Timor Leste has them all. It has a high risk of dengue fever, Japanese encephalitis and malaria.
Whilst vaccination against Japanese Encephalitis can be sought prior to travel, and malaria prophylaxis can be used, it is still essential to avoid getting bitten in the first place.
- Take plenty on insect repellent that contains at least 50% DEET. This can be hard to come by in country so stock up before you go. Ensure it is applied both day and night time, but especially during dawn and dusk. The sunrise and sunsets are beautiful in East Timor, but it does tend to be the highest period for mosquitoes.
- Take long trousers and a long sleeve tops to wear at dawn and dusk, especially if sitting outside in the morning and early evenings when mosquito activity is at its highest.
- Take a mosquito net. The majority of accommodation on the coastal areas is basic, thatched huts and windows with shutters, meaning mosquitos have a free passage from the outside into your sleeping quarters. Make sure the the net is treated with permethrin, kept down over your bed to avoid unwanted mosquitoes invading your bed space.
- Plug in vaporisers can be useful to use to prevent mosquitoes entering your room. Unfortunately, many areas in Timor do not have access to continuous electricity, making electrical vaporisers rather ineffective. Instead use mosquito coils which can be burned like an incense stick to provide up to 10 hours of mosquito relief.
- After-bite cream. Even with the best of intentions, people can still be bitten. Taking a steroid based bite cream will help to reduce the itch and inflammation associated with any mosquito bites you many encounter.
To help keep mosquitos at bay, you can purchase our Ultimate Bug Kit online.
Fleet Street Travel Clinic
Book a travel consultation today.
By Anna Chapman | Travel Nurse | May 2018
HPV vaccine unavailable to boys on the NHS
The HPV vaccine is now offered to girls aged 12-18 years in the UK for free by the NHS.
Since its introduction in 2008, it has already shown to be very effective in reducing the cases of cervical cancer in females*. But the HPV virus doesn’t only cause cervical cancer, it can lead to other cancers such as anal, head, neck and throat cancers. Men are as much at risk of these cancers as women, so why are boys ineligible to receive the HPV vaccine as part of the NHS vaccination schedule?
The BBC has reported the case of Jamie Rae today, to highlight the issue. Mr Rae is campaigning for the HPV vaccine to be introduced, after undergoing radiotherapy for his throat cancer which he believes could have been prevented if an HPV vaccine had been available.
The article also reports that Professor Francis Vaz, a head and neck surgeon at University College London Hospital, paid privately to vaccinate his three sons, to protect them from certain cancers like anus, penis, mouth and throat. He said he saw on a daily basis that cancers driven by the HPV virus had been increasing in the past decade.
“I regularly see the bad end of that spectrum, so I thought the vaccination would be suitable for my sons,”
– he said.
“It’s just unfortunate it wasn’t available for them on the NHS. I was happy to pay for it because I think it’s a good vaccine.”
Why boys should receive the HPV vaccine
- About 15% of UK girls eligible for vaccination are currently not receiving both doses, a figure which is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries with no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high – treating anogenital warts alone in the UK is estimated to cost £58m a year, while the additional cost of vaccinating boys has been estimated at about £20m a year
Source: HPV Action
Our HPV vaccine page explains how get an HPV vaccine at Fleet Street Clinic.
FLEET STREET CLINIC – SPECIALIST VACCINE CLINIC
Fleet Street Clinic is a specialist vaccination clinic offering all vaccinations from travel jabs, to childhood immunisations to flu vaccinations programmes.
TO BOOK
You can book an appointment online.
Although fibromyalgia has long existed, it has only recently been accepted as a chronic, debilitating condition.
The NHS and the Department of Work and Pensions now list fibromyalgia as ‘real’, which is a step in the right direction.
So what is fibromyalgia?
The exact cause of fibromyalgia is unknown, but it is thought to be related to abnormal levels of certain chemicals in the brain and changes in the way the central nervous system (brain, spinal cord and nerves) processes pain messages carried around the body.
It may connected to other conditions, including various arthritis’s and may be genetic but even this is unsure. We do know it can be triggered after a traumatic or stressful event; anything from a virus to a divorce. Anyone can develop fibromyalgia at any age, but it predominantly affects women between the ages of 30 and 50. Some studies believe up to 1 in 20 people may be affected.
Symptoms
Unfortunately there is no specific test for fibromyalgia, so diagnosis is made purely on presentation and history. This makes life difficult as the symptoms of fibromyalgia vary according to the person, both in specifics and intensity. Symptoms may be aggravated by many things, from stress to the weather.
Widespread pain
If you have fibromyalgia, one of the main symptoms is likely to be widespread pain. This may be felt throughout your body, but could be worse in particular areas, such as your back or neck. The pain is likely to be continuous, although it may be better or more severe at different times.
The pain could feel like:
- an ache
- a burning sensation
- a sharp, stabbing pain
Extreme sensitivity
Fibromyalgia can make you extremely sensitive to pain all over your body, and you may find that even the slightest touch is painful.
If you hurt yourself – such as stubbing your toe – the pain may continue for much longer than it normally would.
You may hear the condition described in the following medical terms:
- hyperalgesia – when you’re extremely sensitive to pain
- allodynia – when you feel pain from something that shouldn’t be painful at all, such as a very light touch
You may be sensitive to things such as smoke, certain foods and bright lights. Being exposed can cause your other fibromyalgia symptoms to flare up.
Cognitive problems (‘fibro-fog’)
Cognitive problems are issues related to mental processes, such as thinking and learning. If you have fibromyalgia, you may have:
- trouble remembering and learning new things
- problems with attention and concentration
- slowed or confused speech
Other symptoms
Other symptoms that people with fibromyalgia sometimes experience include:
- dizziness and clumsiness
- headaches
- fatigue
- poor sleep quality
- stiffness
- feeling too hot or too cold – this is because you’re not able to regulate your body temperature properly
- restless leg syndrome (an overwhelming urge to move your legs)
- tingling, numbness, prickling or burning sensations in your hands and feet
- in women, unusually painful periods
- IBS developments
- anxiety
- depression
If you think you may be depressed, it’s important to get help from your GP or your fibromyalgia healthcare professional, if you’ve been seeing one.
So what can be done to help?
First and foremost you need a good diagnosis from your heathcare practitioner to make sure they think you have fibromyalgia and not other conditions that may need treating differently, or more importantly investigating differently to be safe.
Once this is done and other conditions have been ruled out, and fibromyalgia has been diagnosed, you may need to try a variety of treatments to find a combination that suits you.
Fibromyalgia has numerous symptoms, meaning that no single treatment will work for all of them. Treatments that work for some people won’t necessarily work for others.
These treatments include medication, lifestyle changes (from diet to identifying and avoiding trigger factors), exercises, physical treatment, relaxation techniques, counselling and CBT.
Article by Andrew Doody – Osteopath for Fleet Street Clinic
There are many helpful bodies out there who can help and support if you are concerned you may suffer from fibromyalgia including UK Fibromyalgia, Fibromyalgia Action UK and the Fibromyalgia Association.
HOW TO BOOK AN APPOINTMENT
You can find more information about out osteopathy services here. Or book an appointment with out osteopath, Andrew Doody.
Our InBody scanner lets you take control of your health
Do you want to take steps to manage your weight? Are you looking to lose weight or gain muscle? If so, the first step to changing your body is to get accurate measurements of your current stats.
Here at the Fleet Street Clinic, our Inbody scanner provides you with a detailed analysis of your body’s composition. This gives you an accurate way to measure your weight g oals.
You can use the InBody scanner by booking an appointment. Our nurse will measure your height, document your age and the scanner does the rest! Accurately measuring your weight, body fat, muscle mass, BMI and basal metabolic rate, the InBody scanner tells you if you are above, below or in the normal range for your age and height. You’ll receive your results as a one-page analysis, which we will talk through with you. From this, you can set your achievable long-term health goals.
Look for more help with your health goals?
If you’re looking to get some more direction on how to achieve your health goals, our dietitian provides weight management advice to improve your health to optimal levels.
Many people in the UK view tuberculosis as a Victorian disease, but in fact even today, 5000 people a year are affected by TB.
World TB day gives the opportunity to raise awareness of tuberculosis and lead to fewer cases. An easy way to help stop the spread TB is by having a BCG vaccine, which can be given to newborn babies soon after birth.
In some parts of London, the BCG is not readily available on the NHS, in which case you might consider getting the BCG vaccine privately.
BCG Vaccine for Children
At the Fleet Street Clinic in Central London, we have been providing specialist vaccination services for over 20 years.
We run a BCG clinic once a week for babies and children under the age of 6. Our baby/child BCG clinic runs on Wednesday’s.
Why have the BCG Vaccine?
The BCG vaccine protects against tuberculosis. TB is a bacterial infection that affects the lungs in most cases but can affect other parts of the body such as the bones and kidneys. Typical of many bacterial infections, tuberculosis can be spread through long-lasting exposure to an infected person via sneezing or coughing. The BCG vaccine is a proven way to ensure protection against the tuberculosis bacteria.
FLEET STREET CLINIC – NATIONAL PERFORMERS LIST
At Fleet Street Clinic, we specialise in providing vaccinations and occupational health, often working with medical staff to make sure they have all vaccines, tests and ‘fitness for work’ checks needed to work for agencies supplying the NHS.
We offer services to Medical, Dental and Ophthalmic performers requiring occupational health clearance to join the National Performers List.
WHAT IS THE NATIONAL PERFORMERS LIST?
There are three lists of National Performers, which are maintained for dentists, GPs and opticians. Managed by NHS England, these National Performers Lists “provide an extra layer of reassurance for the public that GPs, Dentists and Opticians practicing in the NHS are suitably qualified, have up to date training, have appropriate English language skills and have passed other relevant checks such as with the Disclosure and Barring Service and the NHS Litigation Authority.”
These checks include occupational health screening to check the practitioner is fit to work and has had the necessary tests and immunisations required for their role.
WHY CHOOSE FLEET STREET CLINIC
Dentists, GPs and opticians applying to join the National Performers List must obtain their Occupational Health Clearance from a SEQOHS-accredited occupational health provider, which Fleet Street Clinic has. We have vast experience in providing occupational health clearance in accordance with Department of Health guidance. Immunisation requirements can sometimes be complex and Fleet Street Clinic provides a personal service with clear, informed and helpful advice.
HOW CAN I APPLY FOR OCCUPATIONAL HEALTH CLEARANCE TO JOIN THE NATIONAL PERFORMERS LIST?
If you need health clearance to join the National Performers List, contact the clinic or occupational health team prior to making an appointment.
Fill out the form below and we will send you the forms and information needed to submit your application.
Around 8 in 10 people don’t know what encephalitis is and so World Encephalitis Day aims to raise awareness of this illness, which causes brain inflammation and affects 6,000 people a year in the UK and has a high mortality rate.
Symptoms of Encephalitis
Infectious encephalitis usually begins with a ‘flu-like illness’ or a headache. Typically more serious symptoms follow hours to days, or sometimes weeks later. The most serious finding is an alteration in the level of consciousness. This can range from mild confusion or drowsiness to loss of consciousness and coma. Other symptoms include a high temperature, seizures (fits), aversion to bright lights, inability to speak or control movement, sensory changes, neck stiffness or uncharacteristic behaviour.
Autoimmune encephalitis often has a longer onset. Symptoms will vary depending on the type of encephalitis related antibody but may include: confusion, altered personality or behaviour, psychosis, movement disorders, seizures, hallucinations, memory loss, or sleep disturbances.
WHAT IS ENCEPHALITIS?
Encephalitis is an inflammation of the brain. It is caused either by an infection invading the brain (infectious encephalitis) or through the immune system attacking the brain in error (post-infectious or autoimmune encephalitis).
Anyone at any age can get encephalitis. There are up to 6,000 cases in the UK each year and potentially hundreds of thousands worldwide. In the USA there were approximately 250,000 patients admitted to hospital with a diagnosis of encephalitis in the last decade.
CAUSES OF ENCEPHALITIS?
The inflammation is caused either by an infection invading the brain (infectious encephalitis) or through the immune system attacking the brain in error (post-infectious or autoimmune encephalitis). Viruses are the most frequently identified cause of infectious encephalitis (e.g. herpes viruses, enteroviruses, West Nile, Japanese encephalitis, La Crosse, St. Louis, Western equine, Eastern equine viruses and tick-borne viruses). Any virus has the potential to produce encephalitis, but not everybody who is infected with these viruses will develop encephalitis. Very rarely, bacteria, fungus or parasites can also cause encephalitis.
SYMPTOMS OF ENCEPHALITIS
Infectious encephalitis usually begins with a ‘flu-like illness’ or a headache. Typically more serious symptoms follow hours to days, or sometimes weeks later. The most serious finding is an alteration in the level of consciousness. This can range from mild confusion or drowsiness to loss of consciousness and coma. Other symptoms include a high temperature, seizures (fits), aversion to bright lights, inability to speak or control movement, sensory changes, neck stiffness or uncharacteristic behaviour.
Autoimmune encephalitis often has a longer onset. Symptoms will vary depending on the type of encephalitis related antibody but may include: confusion, altered personality or behaviour, psychosis, movement disorders, seizures, hallucinations, memory loss, or sleep disturbances.
DIAGNOSIS OF ENCEPHALITIS
Symptoms alone often do not allow sufficient ability to distinguish between the many diseases that can mimic encephalitis. Therefore, doctors perform a variety of hospital tests – it is important that investigations are carried out as soon as possible as prompt diagnosis reduces mortality and improves the outcomes.
With increasing numbers of people travelling worldwide, it is important to highlight the risk of infectious encephalitis which can be spread by mosquitoes (Japanese encephalitis ), ticks (Tick-borne encephalitis,) or other animals (Rabies).
If you are concerned about travelling to an area with the possibility of encephalitis infection, please visit our country vaccination guide for specific advice on your destination.
Information from The Encephalitis Society
You can protect yourself from Japanese Encephalitis and Tick-borne Encephalitis with vaccinations. Book your travel vaccination appointment today.
Flu Vaccines in London
Private Flu Vaccination Clinic London
Are you looking for a flu vaccine in London?
Fleet Street Clinic’s flu vaccination clinic in central London is open until March 2021. We have highly-qualified staff on hand, experienced at vaccinating all ages, including young children and babies.
Due to the Covid-19 pandemic, we are inviting all patients to book in their chosen appointment. This was we can manage the number of people waiting at any given time.
Please arrive at your appointed time and you will be seen by our welcoming team. Help us keep you safe by booking in your appointment and turning up to it alone, wearing a face covering.
Here are a few useful things to know before you come:
FLUJABS CLINIC LOCATION
We are based in central London at Fleet Street Clinic, 29 Fleet Street, London, EC4Y 1AA. Our flu vaccine service runs by appointment-only most weekdays, Monday – Friday 9am – 5pm.
Find all available dates and times here.
WHEN IS THE FLU VACCINE SERVICE AVAILABLE?
You can be vaccinated against flu at Fleet Street Clinic most weekdays between 9am – 5pm (please note these opening times are different to those of Fleet Street Clinic). Check availability and book an appointment prior to turning up.
The flu clinic is open until March 2021.
HOW MUCH DO THE FLU VACCINES COST?
View a full list of costs here.
WHAT FLU VACCINES DO YOU USE?
As a specialist centre, we offer a wide choice of flu vaccine types and technologies available. Find out more…
DID YOU KNOW?
The Fleet Street Clinic is the only UK medical practice to offer point-of care flu diagnosis using molecular technology. We can provide a laboratory-confirmed diagnosis of flu and other upper respiratory viruses including Covid-19 – in just over an hour. We don’t just vaccinate against flu, we can diagnose and treat in a single visit.
If you have any further questions about the flu jab or other travel vaccinations, our experienced team of nurses can help.
Arthritis and Osteopathy
Are you living with arthritis or know someone who is? Many people have experience of arthritis – there are currently 10 million people in the UK affected. Sufferers can often resign themselves to living with the pain, without realising there are a number of ways to manage it. For World Arthritis Week, we take a look at arthritis and the benefits of using osteopathy to help treat the condition.
What is arthritis?
Arthritis is a common condition which causes pain, swelling and inflammation in the joints of the body.
The most common types are osteoarthritis and rheumatoid arthritis. Osteoarthritis is a result of wear and tear of the joints in the body. It is common in people over 50 and can affect the knees, hips, neck and back, feet and hands.
Symptoms of Arthritis
Arthritis may be hereditary but can often be caused by poor posture, heavy manual work and previous injury, symptoms include:
- Hip / Knee Pain
- Neck Pain
- Lower back pain
- Early morning stiffness
- Joint Pain
- Swelling and Inflammation
- Referred muscle pain
What can osteopaths do to help with arthritis?
The Institute of Osteopathy purports osteopathy as a way to manage arthritis and the associated symptoms. Mobilising arthritic joints and treating surrounding muscles can help reduce pain. Osteopaths work on the general mobility of the other joints and muscles in the body to improve overall function. Osteopaths may advise on posture, diet, exercise and health improvements.
Osteopaths in Central London
Top Osteopath, Andrew Doody works at Fleet Street Clinic in London and is able to treat arthritic conditions and help to alleviate pain. Osteopathic treatment can be used in conjunction with help from a dietitian, use of acupuncture and support from your GP to ensure a holistic treatment of the condition.
HEPATITIS A and Hepatitis B VACCINES AT FLEET STREET CLINIC LONDON
Although Hepatitis A and Hepatitis B vaccinations are currently in short supply in the UK and globally, Fleet Street Clinic is committed to maintaining the stock of all vaccines and currently has a good supply of both.
Hepatitis A
Hepatitis A is a viral infection that is spread through food and water contaminated with the virus. It occurs world wide including Central and South America, Africa, Eastern Europe, Middle-East, Asia, and the Indian Subcontinent.
Hepatitis A affects the liver causing jaundice, and whilst most people make a full recovery, it can result in chronic liver disease and be fatal.
HEPATITIS A VACCINATION
Hepatitis A is easily preventable through vaccination, and there are several types of vaccination available in the UK that offer protection. The vaccination is available to adults and children over the age of 1 year. It can be given alone (Avaxim, Vaqta) or in combination with typhoid (Viatim), whereby a single injection provides protection for 12 months. A second injection given 6 months later will provide 25 years of protection against Hepatitis A.
The vaccination is available to adults and children over the age of 1 year. It can be given alone (Avaxim, Vaqta) or in combination with typhoid (Viatim), whereby a single injection provides protection for 12 months. A second injection given 6 months later will afford 25 years of protection against Hepatitis A.
It is also possible to receive Hepatitis A in combination with Hepatitis B (TwinRix or Ambirix) whereby 2 or 3 doses of the vaccination can be given between 3 weeks or 6 months.
In addition to the vaccination, travellers should exercise caution with food and water by:-
- Ensuring all food is cooked thoroughly and served hot
- Sticking to bottled water only with a seal or boiled water– no tap water
- Avoiding ice
- Only consuming fruit that can be peeled or sliced without contamination (such as bananas)
- Avoiding high-risk food such as shellfish, raw or rare meat, salad, buffet food, reheated food
HEPATITIS B
- Hepatitis B is a viral infection spread by contaminated blood and bodily fluids.
- 350 million people worldwide are carriers of the Hepatitis B virus.
- The highest risk countries for Hepatitis B infection are central, western and southern Africa and south-east Asia.
- Chronic infection with Hepatitis B can cause liver disease and liver cancer.
Hepatitis B is contracted through contact with infected blood or bodily fluids. These can include:
- Mother to baby transmission at the time of birth
- Unprotected sexual intercourse
- Through contaminated blood products (such as unscreened blood transfusion)
- Contaminated medical equipment (such as needles and syringes)
- Contaminated tattoo or body piercing equipment
- Through contaminated needles and syringes from injecting drug use
VACCINATION AGAINST HEPATITIS B IS ADVISED FOR:
- Those who are at occupational risk (such as health care workers, aid workers where their job puts them at risk of injury)
- Travellers who visit high-risk areas, or those who travel frequently or for longer periods
- Travellers who have pre-existing conditions whereby their condition may make it more likely for them to need medical attention
- Travellers who carry out activities associated with risk (adventure sports, body piercing, tattoos)
- Those who participate in lifestyle behaviours that may increase the risk (such as, unprotected sex and injecting drug use)
A Hepatitis B vaccine is available and can be given from birth. It requires a primary course of 3 vaccinations to be given over a 6 month period (0, 1 months, 6 months) with a booster dose given 5 years later. Those who require the vaccinations to be given more quickly, such as last-minute travellers, can receive the primary course over a shortened 3 week period. Hepatitis B can also be given in combination with Hepatitis A when protection against both diseases is required. TwinRix is available for both adults and children and adheres to the vaccination schedule outlined above. Ambirix is licenced for children under the age of 15 years and requires 2 doses 6 months apart.
Health Risks of European Travel
How many of us know that European travel can pose a threat to our health? Health risks aren’t normally associated with European travel – we think of quick flights and familiar cultures so assume we’ll be relatively safe on short-haul holidays. However, there are actually several diseases to watch out for, especially if you are not vaccinated.
Stay aware of these key diseases so that you can prepare properly to have a safe and happy holiday.
Four illnesses to be aware of when holidaying in Europe:
1. Measles
- Measles continues to spread within and throughout Europe this year. Large outbreaks of the disease have occurred, and it is thought that the drop in vaccination coverage within populations is responsible. Countries that are currently reporting outbreaks of measles include: AUSTRIA, BELGIUM, BULGARIA, CZECH REPUBLIC, FRANCE, GERMANY, HUNGARY, ICELAND, ITALY, PORTUGAL, ROMANIA SPAIN, SWEDEN.
- Measles is a highly contagious virus which can have life-threatening complications.
- International travel has played a large factor in the international spread of measles.
2. Tick-Borne Encephalitis (TBE)
- TBE season has begun in Europe this summer. TBE is a viral infection spread through the infected bite of a tick.
- TBE effects areas of northern and Eastern Europe, Russia and even China.
- Those at highest risk of the diseases are those that intend to spend time in rural forested areas during spring summer and autumn where ticks are present. Activities such as camping and hiking and cycling increase the risk.
- Those who are travelling to areas of transmission can minimise the risk of the disease by taking strict precautions against tick bites.
3. Hepatitis A
- Europe has seen an increase in Hepatitis A cases this year. The virus is spread through contaminated food and water.
- The highest risk countries are those in Eastern Europe, the Baltics, the Balkans and Turkey, but in recent months Germany and Portugal have seen an increase in cases.
4. Rabies
- Rabies is virus-spread through the bite of an infected mammal. The virus is almost always fatal if left untreated. Animals that can spread this disease include dogs, cats, bats, foxes and wolves.
- Eastern Europe poses the highest risk of rabies in Europe.
- Travellers at highest risk include those who plan on travelling to remote areas.
Vaccines can prevent travel-related illnesses
The good news is that all these diseases are vaccine preventable and can be avoided by organising vaccines before you travel.
Measles – All travellers should ensure that they have had at least 2 doses of vaccinations against measles. This is usually given as a routine vaccination in childhood (MMR vaccine) at 1 year of age, and then again as a pre-school booster
Tick-Borne Encephalitis – vaccination against the disease is available for individuals aged 1 year and above. It requires 2 vaccination 2 weeks apart.
Hepatitis A – A highly effective vaccination is available against Hepatitis A and can be given to children from 1 year of age. Once the schedule of 2 Hepatitis A vaccinations has been given, immunity lasts for 25 years.
Rabies – a vaccine-preventable disease which requires three doses of vaccination to be given prior to departure. Those who have not received the vaccination with potential exposure to rabies require more extensive treatment which is not always accessible.
Travel Vaccinations at Fleet Street Clinic
Fleet Street Clinic is a leading vaccination centre and offers all travel vaccinations at our clinic in the heart of London.
Book your appointment online today.
By Anna Chapman, Travel Nurse at Fleet Street Clinic
BCG Vaccine Shortage in the UK
As the media has reported, the UK is in short supply of the BCG vaccine, impacted by global shortages.
The BCG vaccination gives worthwhile protection against tuberculosis, a serious infection spread by coughs and sneezes. In 2014, more than 6,500 TB cases were reported in the UK. Babies most at risk of contracting TB are those living in London and the Midlands, so if you live in these areas it is strongly recommended to have your baby inoculated.
At the Fleet Street Clinic, we have over 20 years experience as a specialist vaccination centre. We have a good supply of the BCG vaccine and run a designated BCG clinic for babies and children on Wednesday’s each week. All our vaccines are administered by highly qualified nurses or doctors, who will be happy to answer any queries or concerns.
What is TB?
TB is a bacterial infection spread through coughs and sneezes and affects the lungs, lymph glands, bones, and nervous system.
Where is the clinic?
The Fleet Street Clinic is located in Central London. Our address is 29 Fleet Street, London EC4Y 1AA.
How to Book?
With the new football season in full swing, it’s apt time to address one of the most common football injuries; hamstring pulls.
Hamstring Injury
This injury occurs when there’s a tear or strain to the muscles at the back of the thigh. By definition, hamstrings are a set of three muscles at the back of the thigh that all cross both the knee and hip joint, with only half of one (the biceps femoris) originating from the thighbone. Rapid acceleration movement is the main course of hamstrings getting injured. With football being a sport that relies heavily on quick movement in this area of the body, it is an injury your favourite footballer is highly likely to suffer from this season. There are three levels of severity to hamstring injuries. These are:
- Grade 1 – a minor strain
- Grade 2 – a partial tearing of the muscle
- Grade 3 – a complete tearing of the muscle
Symptoms of Hamstring Injury
This depends on what grade of the injury the player has.
- Grade 1 injury – consists of tenderness and sudden pain at the back of the thighs. Muscle strength will likely remain the same, but moving the leg might be painful.
- Grade 2 injury – more painful and more tender. Some bruising and swelling could occur in the area. There will also be a loss of strength in the leg.
- Grade 3 injury – have grade 1 and 2 symptoms at a more severe level. A popping or snapping sensation may be felt. The injured person may struggle to even be able to stand.
Treatment
There are initial steps that can be taken to treat hamstring injuries including compression, applying ice, elevation and good rest. Taking painkillers such as paracetamol can help reduce pain. Full recovery time will depend on the grade of injury. Professional footballers have access to equipment and health professionals that can help speed up recovery. Although self-treatment is an option for the everyday person, seeing a healthcare professional is advised if you’re concerned the injury is severe, the symptoms worsen or healing is very slow.
Osteopathy Treatment for Hamstring Injuries
Osteopathy is a medical specialty focused on musculo-skeletal problems. An osteopath deals with diagnosing, management and treatment of these types of injuries. If you’re concerned that you might be suffering from a hamstring injury or your self-treatment is not working out, book an appointment online and we can book you a session with Andrew Doody, our osteopath.
Prevention of Hamstring injury
There’s no surefire way of preventing an hamstring injury but there are steps that can be taken to reduce the likelihood. These include;
- Gentle stretching the hamstring area after exercise
- Warming up
- A longer warm-up period in cold weather
- If you feel any tightness, you might want to stop as this could be a signal that a tear might occur
BCG Vaccine for Children
At the Fleet Street Clinic in Central London, we have been providing specialist vaccination services for over 20 years. Our excellent relationship with a range of suppliers enables us to maintain good stock levels of vaccines, even where there may be supply shortages elsewhere.
We run a BCG clinic once a week for babies and children under the age of 6. Our baby/child BCG clinic runs on Wednesday’s.
Why have the BCG Vaccine?
The BCG vaccine protects against tuberculosis. TB is a bacterial infection that affects the lungs in most cases but can affect other parts of the body such as the bones and kidneys. Typical of many bacterial infections, tuberculosis can be spread through long-lasting exposure to an infected person via sneezing or coughing. The BCG vaccine is a proven way to ensure protection against the tuberculosis bacteria.
Vaccination for Babies and Children Under 6 years of age
The BCG vaccination is not offered to all children by the National Health Service. Some NHS boroughs do offer it as routine but are unable to supply at present due to the national shortage. The TB vaccination has to be sourced privately instead. With two decades of experience providing vaccination services, the Fleet Street Clinic provides a safe, child-friendly environment and the guarantee of an expert medical support service.
To protect your baby with the BCG Vaccine, you can book an appointment online.
There is currently an outbreak of Cyclospora related to travel in Mexico.
A Public Health England Health Protection Report highlights 204 confirmed cases since June 1st, 2016.
The cases are mainly associated with travel to Mexico, specifically the Riviera Maya Coast. The average incubation period is a week and infection is characterised by watery diarrhoea, fatigue, muscle pain, weight loss, nausea and low-grade fever. The foods previously involved in cyclospora outbreaks include soft fruits, such as raspberries, and salad products such as coriander, basil and lettuce. If untreated the illness can last for several weeks.
The Fleet Street Clinic can run a stool sample test that can diagnose Cyclosporiasis among many other causes of diarrhoea in returning travellers, and you will get your reults back in an hour of the test being done. If you are worried about any symptoms you have post travel to Mexico or any other country then call our reception team on 02073535678.
Or you can book an appointment online.
Bowel Cancer in the UK
The beginning of April marked the start of Bowel Cancer Awareness month. Bowel cancer is very treatable and one of the most common cancers in the UK.
40,000 cases are diagnosed every year. 1 in every 20 people will develop bowel cancer in their life time.
Symptoms of bowel cancer are often ones that you may find difficult to talk about or explain to your doctor. Nobody enjoys an uncomfortable conversation, especially when it comes to being candidly honest about something so private but the earlier it’s diagnosed, the greater the chance of survival is. It’s difficult, but let’s talk about it.
WHAT ARE THE SIGNS AND SYMPTOMS?
- Bleeding from your bottom and/or blood in your bowel movements
- A change in your bowel habits that lasts three weeks or longer
- Sudden and unexplained weight loss
- Extreme tiredness for no obvious reason
- A pain or a lump in your stomach
AM I AT RISK OF BOWEL CANCER?
Currently we do not know what causes this cancer. We have been able to identify some factors that can increase your risk of getting the disease:
- Aged over 50
- A strong family history of bowel cancer
- Being overweight or obese
- Lack of exercise and being inactive
- Longstanding inflammatory bowel disease such as Crohn’s disease or ulcerative colitis
HOW CAN I HELP PREVENT BOWEL CANCER?
There is no way to 100% prevent bowel cancer unfortunately. Things like family history, you cannot change.
However, there are some ways you can help yourself as recommended by the NHS.
- Improve your diet – eat less processed foods and red meat, eat more fish and fibre
- It is recommended that adults exercise for at least 2.5 hours a week
- Making sure you are a ‘healthy’ weight
- Stop smoking
- Cut down on alcohol
You can read all about these tips here on the NHS website.
GET SCREENED FOR BOWEL CANCER
If you are concerned about possible symptoms and are not eligible for NHS screening (aged between 60 – 74 and registered with a GP), you can make an appointment to speak with one of our experienced GPs (male or female GP’s).
If you need advice, get in touch with our expert GP’s and dietician at Fleet Street Clinic.
To book an appointment, head to our online booking system here. Alternatively, call us on 020 7353 5678 or email us at info@fleestreetclinic.com.
Dr Richard Dawood, our Medical Director and Travel Medicine specialist answers frequently asked questions about Yellow Fever and the Yellow Fever vaccine in our new video.
Do you often find yourself trawling through Instagram just before going to bed? Waking up and checking your emails before you even have a shower or a coffee? Former Facebook chief marketing officer Randi Zuckerberg hit the nail on the head when she said that people need to understand that while “the phone is an amazing tool, we own our devices, they don’t own us.” It’s time for your digital detox.
The average smartphone user checks their phone 221 times a day. The Oxford English Dictionary defines a digital detox as “a period of time during which a person refrains from using electronic devices such as smartphones or computers, regarded as an opportunity to reduce stress or focus on social interaction in the physical world.”
By periodically unplugging, you can start reclaiming real life experiences rather than living in a virtual world. So how can we get this started?
Appreciate the silence – We have become so accustomed to filling every spare moment with digital noise. Try hitting reset on your brain from time to time and take a few moments to just let your mind wander. Be comfortable with silence, slow down and be present in the moment without the glow of a screen.
Kick technology out of the bedroom – Give yourself a technology curfew and when you say “lights out” actually mean it. Harvard researchers have found that technological devices such as phones, tablets and laptops can disrupt melatonin production, sleep quality and mood. To avoid temptation, banish your devices from the bedroom and try using an old fashioned alarm clock!
Socialise in the real world – Let’s face it, how many of the people you follow on your social media are actually your close friends? At 1am when you are struggling to sleep, do you really need to look at pictures of what they ate for lunch? Whilst social media can have its uses and be a positive influence, it can have a negative effect on our wellbeing as a result of comparing our lives to those carefully edited for show.
Hit the pause button – Be conscious of how often you check your phone – next time you go to reach for technology, hit the metaphorical pause button. Take a breath and think about what you are going to get out of it. Is there a more meaningful and productive way to spend your time, such as going for a walk and getting some fresh air and movement instead?
We get 525,600 precious minutes a year, how you choose to spend them is up to you.
“If it doesn’t add to your life it doesn’t belong in your life”
Speak to our occupational health experts for advice on how to take a digital detox today on 020 7353 5678.
The Zika Virus has been making headlines recently for it’s frightening links to rare birth defects. Brazil has even gone as far as to warn women to avoid falling pregnant whilst an epidemic is rife. The link between 400 cases of new-borns with microcephaly in the north-east of Brazil is being investigate by health authorities.
The increase in microcephaly, a neurological disorder that stunts the growth of the baby’s cranium, limiting it to a circumference of less than 33cm, has increased in Brazil from 59 cases in 2014, rising to 1,248 cases throughout 2015. Typically, life expectancy for babies born with the condition is reduced. In 90% of cases, brain function is also reduced. There are currently no travel restrictions in affected areas.
How is the virus contracted?
The Zika virus is spread to people through the bite of an infected mosquito. Outbreaks have been seen across Africa, Asia, Central and South America.
What are the the symptoms and treatment?
The common symptoms, usually mild and often lasting from a few days to one week, can be a rash, fever, joint pain, and conjunctivitis. There is currently no vaccine to prevent or medicine to treat the virus. Pain killers can be used to alleviate these symptoms which often go mistaken as a fever, and can easily be missed, especially in the early stages of pregnancy.
Is there a way to reduce my risk?
Insect bite precautions is paramount, especially for pregnant women in the affected areas. The NHS travel website, Fit For Travel, recommends:
- Covering up – wearing long sleeved tops and long trousers
- Spraying thinner clothing with insect repellent
- Burning pyrethroid coils and heating insecticide impregnated tablets
- Sleeping in a screened room where possible or using a treated mosquito net
If you are travelling to Brazil or any of the infected areas, book an appointment with one of our dedicated Travel Clinic nurses for information on vaccines and travel wellbeing now on 020 7353 5678.
Zika Virus – Additional Resources
Zika virus: medical advice for travellers – The Telegraph – Richard Dawood
Zika Virus – Video
Watch Fleet Street Clinic’s Dr Richard Dawood discuss Zika Virus on Victoria Derbyshire.
5 excellent ways the Fleet St, Clinic’s occupational health services can benefit employee health and well being:
- Recruiting a new employee? Arrange a pre-placement assessment.
Why? The OH nurse or doctor can check whether the employee is fit to undertake the role. If any health concerns are identified, s/he can make recommendations, where appropriate, to promote the employee’s well being and health at work. - Staff reporting back problems? Arrange an ergonomic assessment.
Why? It could be that your employee’s workplace arrangement is causing or contributing to the problem. Our ergonomics consultant can assess their workplace in relation to the problem(s) reported/diagnosed and provide advice and recommendations on how to reduce symptoms. - A staff member returning to work after illness? Arrange a Fitness Assessment.
Why? Employees and employers can benefit from advice and recommendations on how best for the employee to enter back into work to minimise risk of relapse and aid a successful and healthy return to work. - Assigning one of your employees to a project abroad? Arrange a pre-deployment medical.
Why? Depending on the assignment and location, working abroad can increase stresses on the individual and often with limited access to medical care. A pre-deployment medical can assess whether the employee is fit to undertake the post, provide advice and recommendations to promote their health while away and advise on any travel precautions to prevent illness.
You can find out more about our occupational health services here.
Alternatively, fill out the form below and we’ll propose suitable services for your consideration.
- We have a small, friendly team of specialists, who are all HCPC registered professionals, with a broad range of skills and experience.
- We take a team approach to care: our podiatrists work together with our in-house osteopath, GPs, acupuncturist and dietician to give you the best support for your foot health problems.
- We have an excellent network of trusted colleagues to whom we can refer, with expertise in dermatology, physiotherapy, radiography, sports medicine and surgery.
- We will look after your foot-health at a time convenient to you – day and evening appointments always available!
- We stock a range of professional foot-care products to help you to get the best out of self-care between appointments.
Book your Podiatry appointment today. Or find out more about our podiatry clinic here.
With #Wimbledon in full swing again and everyone digging out their racquets in the beautiful sunshine, our osteopath, Andrew Doody, calls time on an old problem.
Tennis elbow is a condition that causes pain around the outside of the elbow. It’s clinically known as lateral epicondylitis and often occurs after strenuous overuse of the muscles and tendons of the forearm, near the elbow joint. You may notice pain: on the outside of your upper forearm, just below the bend of your elbow when lifting or bending your arm when gripping small objects, such as a pen when twisting your forearm, such as turning a door handle or opening a jar. You may also find it difficult to fully extend your arm.
The name tennis elbow is because the tennis backhand shot is a common way to develop the problem, however, any strain or overuse can cause it. The condition is easy to get but can hang around for weeks and months if left untreated. This is largely due to the fact that lots of the muscles in the hand and forearm attach to either side of the elbow. This means that once the area is inflamed, almost everything you do with the hand can re-aggravate it, from drinking a cup of tea (or Pimms) to opening a door (or raising a trophy).
Once diagnosed, treatment involves firstly reducing the inflammation with rest, cold compresses and medication, followed by massage and careful mobilisation to help relieve pain and stiffness and restore the range of movement. Specific supports can also be quite beneficial at this time. Preventing tennis elbow Preventing tennis elbow is tough but here are a few pointers: If you have tennis elbow, stop doing the activity that is causing pain, or find an alternative way of doing it that does not place stress on your tendons. Avoid using your wrist and elbow more than the rest of your arm. Spread the load to the larger muscles of your shoulder and upper arm. If you play a sport that involves repetitive movements, such as tennis or squash, getting some coaching advice to help improve your technique may help you avoid getting tennis elbow.
Before playing a sport that involves repetitive arm movements, warm up properly and gently stretch your arm muscles to help avoid injury. Use lightweight tools or racquets and enlarge their grip size to help you avoid putting excess strain on your tendons. Wear a tennis elbow support when you are using your arm, and take it off while you are resting or sleeping to help prevent further damage to your tendons. Ask your GP or osteopath for advice about the best type of brace or splint to use. Increasing the strength of your forearm muscles can help prevent tennis elbow. An osteopath can advise you about exercises to build up your forearm muscles.
If you think you might be suffering from tennis elbow and are seeking treatment or advice, you can book an osteopathy appointment online.
The popular Thai tourist resorts of Krabi and Phuket are reporting high incidences of dengue fever this year.
Since January 2015 over 400 cases of dengue fever have been reported, resulting in one fatality.
Cases of dengue fever also soared in Malaysia with over 40,000 reported cases this year. It is estimated between 6-10 cases of dengue are diagnosed each day – double the rate of last year. The most dramatic increases have been seen in Penang, Johor and the state of Selangor.
Dengue Fever Advice for Travellers
Unfortunately, there is no vaccine or medication that can prevent dengue. The only way to reduce the risk is to prevent mosquito bites, particularly during daylight hours.
If you are off on an Asian adventure this summer, follow these simple steps to reduce the risk of dengue fever:
- Cover up with clothing
- Use insect repellents containing a minimum of 50% DEET on any exposed skin
- Consider treating clothes with permethrin
- Sleep under bed nets and use insect screens on doors.
- Reduce mosquito breeding sites by removing any water containers from outdoor areas
- Use air-conditioning
- Consider the use of plug-in electrical vaporisers which deter mosquitoes
Our Ultimate Bug Kit contains everything you need to help keep mosquitos at bay and is available to purchase online.
Fleet Street Clinic
For more information on Dengue or any other travel-related topic, you can book travel consultation appointment online.
India is currently experiencing a heat wave, with temperatures exceeding 47 degrees Celsius. The heat wave has now spread westwards, with temperatures in Pakistan and the Middle East reaching 50 °C. The highest temperature ever recorded was in Sweihan, Abu Dhabi at 50.5 °C.
Up to 2000 people have died in India as a result of sunstroke and dehydration related to the heat. It is expected that heat waves will continue through summer with Eastern Europe and the Balkans expecting temperatures exceeding 38 °C throughout July and august.
Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes causing rapid dehydration. This can result in heat exhaustion or heatstroke which can be life threatening if not dealt with promptly.
Any traveller can be at risk of sun and heat related injuries, but the highest risk is in the elderly, babies, children and those with pre-existing medical conditions.
Travellers who perform strenuous physical activity will increase the risk of illness related to the heat.
It can take the body up to 10 days to acclimatize to the heat, so it is important that travellers are prepared to prevent heat related illness.
What can travellers do?
*Seek shelter and shade during the middle of the day (11am -3pm) when temperatures are at their hottest
*If you are outside, ensure you protect your skin against the sun with a high factor sun cream
*Wear lose fitting light weight and light colour clothing
*Keep hydrated by drinking plenty of fluids and eating food with a high water content (such as fruit)
*Ensure you are taking in sufficient salt in your diet (sweating leads to electrolyte and salt depletion).
*Avoid caffeine and alcohol, which can worsen heat related illness
Heat stroke can be a life-threatening emergency and medical help should be sought.
http://www.aljazeera.com/news/2015/06/heat-wave-spreads-pakistan-gulf-150603102018356.html