Category: News
If you’ve recently discovered that CityDoc has closed, it’s completely understandable to feel unsettled, particularly if you were mid-treatment, waiting for results or due a repeat prescription.
For many people, the first worry is whether everything now has to start again. In most cases, it doesn’t.
With an appropriate medical review, care can usually continue safely and smoothly once a doctor understands your history and current treatment plan.
Take a breath first
A sudden clinic closure can feel disruptive, especially when health is involved. You don’t need to solve everything immediately.
The priority is simply continuity of care – making sure a clinician reviews where you are now and advises on the safest next step.
Arranging an appointment with a suitable clinic allows a doctor to:
- review your current medication or treatment
- assess any upcoming deadlines (prescriptions, vaccines, monitoring)
- advise how to continue safely and appropriately
If you have copies of emails, letters, test results, or medication packaging, bring them along. If you don’t, that’s very common and it won’t prevent a doctor from helping you move forward.
What about prescriptions?
This is often the biggest concern. In many situations, a doctor can continue necessary medication once they’ve reviewed your medical background and confirmed it’s appropriate. Sometimes a brief review or updated information is needed, but this is usually straightforward.
If your medication is time-sensitive, it’s helpful to mention this when booking so it can be prioritised.
Will tests need to be repeated?
Not necessarily. Doctors aim to avoid unnecessary duplication. Any available information will be used, and investigations are only repeated if they’re clinically required to ensure your care remains safe. The focus is always on balancing continuity with good medical practice.
Ongoing treatment plans or travel vaccinations
If you were part way through a vaccination course or monitoring programme, this can usually continue once reviewed. The timing and schedule matter more than the original provider. This is something clinicians manage routinely.
Feeling unsure is normal
For many patients, the hardest part of a clinic closure is simply not knowing who to contact next or worrying they’ve somehow been left in limbo.
In reality, continuity of care is something experienced medical teams handle regularly. Once a new doctor has assessed your situation, the process is often far simpler than expected.
If you’re unsure what to do next, speaking with a medical professional can help you understand your options and move forward with confidence.
At Fleet Street Clinic, we regularly support patients who find themselves in this position. Our GPs can review your situation, advise on next steps, and help ensure your care continues safely and appropriately without unnecessary delays or repetition.
If you’d like guidance, you can learn more or book an appointment today.
- On-site flu jab clinics (at your office, your schedule)
- Drop-in appointments at our Fleet Street location
- Tailored communications for your teams to boost uptake
- High fever
- Severe joint and muscle pain
- Fatigue
- Rash
- Headache
Lyme Disease: Awareness, Action, and Early Detection
Recent news coverage of Justin Timberlake’s account of his own Lyme disease experience shines a light on a condition many still struggle to recognise early, particularly in the UK, where clinicians and the public are much less familiar with ticks and tick-borne diseases than in the USA. This presents an opportunity, not just to raise awareness, but to improve how we support patients from first symptoms through recovery.
Lyme disease, caused by Borrelia burgdorferi and spread by Ixodes ticks, is most effectively treated when identified early. A high index of suspicion is key, especially for patients presenting with fatigue, fever, joint pain, or a recent history of spending time outdoors – even if the classic rash (shown helpfully on NHS and CDC websites here – https://www.nhs.uk/conditions/lyme-disease/ and https://www.cdc.gov/lyme/hcp/clinical-care/erythema-migrans-rash.html) isn’t present.
With changing climates and wider distribution of ticks, we’re seeing cases in new regions. This makes it all the more important for clinicians everywhere to ask about travel, outdoor exposure, and symptom onset timing. Patient outcomes improve when we listen carefully and act promptly.
As I outlined in my recent article for The Telegraph, preventing tick bites is simple, effective, and key to avoiding Lyme disease and other tick-borne infections. Here’s a condensed guide that travellers may find helpful:
Quick Tips to Prevent Tick Bites
- Stick to paths – Avoid tall grass and dense undergrowth
- Dress wisely – Long sleeves, trousers tucked into socks, and light-coloured clothing help
- Use repellent – Apply DEET (20–30%) to skin, permethrin to clothing
- Do a tick check – Shower and check the body thoroughly after outdoor activities
- Clean clothes properly – Wash and tumble dry on high heat to kill ticks
To fellow practitioners: What strategies have you found most effective in promoting early recognition and patient education around Lyme disease in your practice?
Here’s a link to the article for anyone interested: https://www.telegraph.co.uk/gift/dd43d39bde2df95d
Measles is back in the news, and it’s not just affecting children. Many adults may not realise they are not fully protected against this highly contagious disease. With travel, schools, and public spaces being common areas for exposure, now is the time to make sure your vaccinations are up to date.
We’re here to help guide you through the process of understanding your vaccination status, offering MMR catch-up appointments, vaccine reviews and expert advice for individuals, families and businesses.
Measles outbreaks have increased globally, particularly in areas where vaccination rates have dropped. The pandemic has contributed to gaps in vaccination coverage, with many children missing MMR doses and adults assuming they’re fully protected.
A key reason for low vaccination rates in certain populations is a misinformation campaign that occurred in the 1990s. Led by Andrew Wakefield, the campaign falsely linked the MMR vaccine to autism, causing widespread fear and leading to thousands of children missing out on their measles coverage. Many of these individuals are now adults who, as children, were not vaccinated due to their parents’ decision not to vaccinate them. Fortunately, many of these individuals are now choosing to take the vaccine and catch up on their missed doses. At Fleet Street Clinic, we’ve vaccinated many of these individuals, offering them the protection they were previously denied. Whilst measles is commonly associated with childhood it’s important to understand that adults can also be at risk if they missed the MMR vaccine or didn’t receive a booster dose. Vaccination rates have also been affected by the pandemic as many children missed out on their MMR doses, leaving them vulnerable. This means that public health could be at risk, particularly in communities where vaccination rates have dropped below the 95% threshold. Measles spreads easily through airborne droplets when an infected person coughs or sneezes. This makes it highly contagious in crowded places like schools, airports and travel hubs. If you’re travelling abroad, particularly to countries with lower vaccination rates, your risk of contracting measles can be higher. Schools and day-care centres are also common places where outbreaks happen due to close contact among children.
Want to protect yourself? If you’re unsure of your MMR vaccination status, it’s important to speak with your GP about getting a catch-up vaccine. For children, the MMR vaccine is typically given in two doses, the first at 1 year old and the second at 3 years old. However, if your child missed doses, it’s important to get them up to date. For adults, a booster dose may be needed to ensure continued immunity against measles, mumps, and rubella. We offer same-day appointments for MMR catch-ups and immunity blood tests. Our trusted GP led team is here to provide expert travel health advice, ensuring you’re fully protected.
Book your appointment today.

We would like to welcome our new podiatrist Christopher Barrett to the Fleet Street Clinic team.
Christopher is a podiatrist with over 10 years experience working in both NHS and private clinics.
Christopher is experienced in a wide range of podiatry care and treatments including routine podiatry, wound treatment, verrucae management, nail surgery and foot mobilisation.
Christopher will be working at Fleet Street Clinic on Mondays starting from the 23rd of June 2025.
There is a new name for the most advanced of the pneumococcal pneumonia vaccines: the previous version, Apexxnar, has now been re-branded as Prevenar 20. Although this may result in some initial confusion for medical stall and patients alike, the composition and effectiveness of the vaccine are unchanged. Under its new name, however, it is now licensed for adults and children alike – in fact for everyone over 6 weeks of age.
If you have been previously vaccinated with Apexxnar, there is no reason to be revaccinated. However, if you have been vaccinated with a previous version of Prevenar (such as Prevenar 13), it makes good sense to update now to Prevenar 20, which covers more strains.
Prevenar 20 provides protection against the 20 most important strains (called serotypes) of pneumococcal bacteria, offering a more comprehensive defence against pneumonia.
Covid vaccine updated
Another respiratory vaccine has also had an important update: privately available Covid vaccines will now cover the currently predominant variant, KP.2. Covid cases rose by ten per cent in February, and vaccination is an important protective measure, reducing the likelihood and severity of infection. (It seems that the NHS spring Covid booster campaign is based on the previous JN.1 vaccine.)
Prevenar 20 and the updated Covid vaccine, together with vaccination against RSV, flu and whooping cough, make up the 5 vaccines now available to prevent respiratory infection.
If you would like to find out more about these vaccines, consider making an appointment with one of our knowledgeable nurses or doctors.
About Pneumonia:
Pneumonia is a lung infection that can cause a range of symptoms, including:
- Cough: A persistent cough that produces mucus or phlegm is a common symptom of pneumonia. The cough may be dry or productive, and the mucus or phlegm may be green, yellow, or rust-coloured.
- Fever: Pneumonia often causes a high fever, which may be accompanied by chills and sweats.
- Shortness of breath: Pneumonia can cause difficulty breathing, especially during physical activity. The shortness of breath may be accompanied by chest pain or tightness.
- Fatigue: Pneumonia can cause extreme tiredness and weakness, making it difficult to carry out normal daily activities.
- Muscle aches: Pneumonia can cause muscle aches and joint pain, which may be mistaken for the flu.
- Chest pain: Pneumonia can cause chest pain, especially when breathing deeply or coughing.
- Nausea and vomiting: Some people with pneumonia may experience nausea and vomiting, especially if the infection is caused by a type of bacteria known as Legionella.
- Confusion or disorientation: Pneumonia can cause confusion or disorientation, especially in older adults and people with underlying health conditions.
It’s important to seek medical attention if you experience any of these symptoms, as pneumonia can be a serious and potentially life-threatening condition.
More information on pneumonia.
Who is considered “high-risk”?
Individuals considered to be at high risk for hospitalisation due to pneumonia include the elderly, young children, people with weakened immune systems (including people who have had their spleen removed), and individuals with underlying health conditions such as chronic heart or lung diseases, diabetes, and liver or kidney problems.
At the Fleet St. Clinic, we also regard anyone who has had a previous significant episode of pneumonia as likely to benefit from being vaccinated.
When is the best time for a pneumonia vaccine?
The best time to vaccinate against pneumonia depends on various factors such as the type of vaccine, the individual’s age, and underlying health conditions.
Pneumonia vaccine is not necessarily a winter vaccine, and can be given at any time of year.
How to book an appointment?
Booking an appointment is easy. You can book online through our online booking system.
If you would like to discuss anything further or would like to book with our reception team, you can call them on +44 207 353 5678 or email us at info@fleetstreetclinic.com
If you’re taking a medication like tirzepatide (Mounjaro) or semaglutide (Ozempic or Wegovy), for weight loss or type 2 diabetes, and you’re also using the combined oral contraceptive pill, it’s important to know that these might not always work well together. Weight loss injections belong to a group called GLP-1 receptor agonists (or dual agonists in the case of tirzepatide), which help lower blood sugar, reduce appetite, and support weight loss. One of the ways they do this is by slowing down how quickly food moves through your stomach—and that can also slow down how your body absorbs other medications, like the pill.
This can be a problem because the pill relies on being absorbed properly to be effective. If your stomach is emptying more slowly, or if you’re feeling nauseous, vomiting, or have diarrhoea (which are common side effects when starting weight loss injections), there’s a chance your body might not absorb enough of the hormones from the pill to prevent pregnancy. Because of this, the Faculty of Sexual and Reproductive Healthcare (FSRH) in the UK has issued guidance saying that there’s a potential risk of reduced effectiveness when taking oral contraception with GLP-1 medications like tirzepatide or semaglutide.
To stay on the safe side, the FSRH recommends using a non-oral form of contraception—such as the contraceptive implant, IUD (coil), injection, patch, or vaginal ring—since these options aren’t affected by the digestive system and are more reliable in this situation. If you prefer to stay on the pill, you might be advised to use extra protection like condoms, especially during the first few weeks of starting the weight loss medication or if you’re unwell.
If you’re currently on something like Mounjaro or Wegovy and using the pill, it’s a good idea to book an appointment to speak to one of our GPs or sexual health nurses. We can help you figure out what contraceptive method works best for you and make sure you’re fully protected. Everyone’s situation is different, so having that conversation can help you make the best choice for your health and peace of mind.
At Fleet Street Clinic, we uphold a steadfast commitment to delivering the highest standards of patient care. We are pleased to announce that we have successfully attained reaccreditation from SEQOHS (Safe Effective Quality Occupational Health Service) in 2025. This notable achievement underscores the dedication and expertise of our professional team, as well as our unwavering commitment to maintaining exemplary standards in the field of occupational health services.

Understanding SEQOHS
SEQOHS is an accreditation programme that establishes a benchmark for quality in occupational health services throughout the United Kingdom. It ensures that healthcare providers adhere to stringent standards in various areas, including patient care, clinical governance, and the overall quality of services rendered. Administered by the Faculty of Occupational Medicine (FOM), the reaccreditation process for SEQOHS involves an exhaustive review of clinical practices, staff qualifications, and patient satisfaction, among other crucial factors.
The Significance of SEQOHS Reaccreditation
The attainment of SEQOHS reaccreditation affirms our clinic’s ongoing dedication to providing safe, effective, and superior quality occupational health services. For our patients, this achievement represents a guarantee that the care and guidance they receive align with national standards. Furthermore, it highlights the expertise and experience of our team in delivering solutions designed to enhance employee well-being and organisational health.
The reaccreditation process is comprehensive, ensuring that our clinic continually evolves to meet the demands of regulatory standards and patient needs. It instills confidence in our partners, clients, and patients that we prioritise quality and are committed to consistently improving our services.
The Advantages of SEQOHS Reaccreditation for Our Patients
Quality Care: Through SEQOHS accreditation, our clinic ensures the delivery of all services in accordance with best practices, thus providing patients with confidence in the quality of care they receive.
Expertise: SEQOHS establishes high standards for staff training and qualifications, ensuring our team remains at the forefront of developments in occupational health.
Consistency: Reaccreditation guarantees that we uphold high standards consistently, allowing patients to depend on us for reliable and quality services over time.
Accountability: The accreditation process necessitates regular reviews and audits, ensuring that we consistently meet or exceed the requisite standards of care.
Moving Forward
The reaccreditation by SEQOHS represents a significant milestone in our continued journey toward delivering the highest level of care. At Fleet Street Clinic, we remain committed to providing outstanding occupational health services tailored to fit the needs of both employees and employers.
If you have any questions or want to find out more about how we can help, get in touch with us today on: occhealthadmin@fleetstreetclinic.com
 Among the journalists, television crews, lawyers and other professionals who often have to travel at short notice one of the longest-standing users of the Fleet Street Clinic’s same-day vaccination and travel-health service is the celebrated war photographer Goran Tomasevic.
Among the journalists, television crews, lawyers and other professionals who often have to travel at short notice one of the longest-standing users of the Fleet Street Clinic’s same-day vaccination and travel-health service is the celebrated war photographer Goran Tomasevic.
Softly spoken, calm and courteous, the 6 ft 4 56-year-old Serbian has been ducking bullets and reporting from the world’s battle zones for almost 35 years. Carrying the same equipment wherever he goes – three Canon cameras and three spare lenses, so if one gets damaged he can still continue working – he has spent most of that time working for the global news agency Reuters. His Reuters’ assignments have seen him cover conflict in warzones from Afghanistan, Colombia and Iraq to Libya, Somalia and South Sudan. Voted Reuter’s Photographer of the Year a record-breaking four times, in 2016 he achieved the unique feat of having 100 newspapers around the world put his extraordinary photograph of a fireball in an anti-Gaddafi attack in Libya on their front cover. In 2023 one reviewer of the 444-page book of his pictures, published by Edition, called him ‘ a Caravaggio of photography’. “I want to show exactly how it was … if there’s enough light, I will stay until the end,” he says.
Now working for the Canadian newspaper The Globe and Mail, he will only answer with a cryptic “Asia” when asked about his next assignment. But he is happy to add that wherever precisely that might be – Taiwan, we wonder; perhaps Myanmar? – he will detour via Fleet Street to get any necessary vaccinations and to collect a locale-and-calamity appropriate travel kit. As usual, that will have been made up for him by Fleet Street Clinic’s founder – and now his friend – Dr Richard Dawood.
Q) How did you come across the Fleet Street Clinic?
A) I grew up in Belgrade, and I started working with the Politika news agency during the Bosnian war, in 1991. After all our trouble finished, in 1996 I joined Reuters, and they started sending me to the Middle East and Africa. Their offices were in Fleet Street (they’re in Canary Wharf now) and as they had a contract with Fleet Street Clinic they sent me to the clinic to get jabs and the medical kit, trauma kit, travel kit. From the beginning Dr Richard, he say to me: “Call me any time you’re in trouble!”.
Q) So have you ever had to make that kind of call?
A) Ha ha, many times! The last time, I get a bad reaction for the dengue fever jab. I was about to cross the border between Dominican Republic and Haiti but they sent me back. I had a fever. I was feeling very bad. But after calling Dr Richard I knew where I was standing. He said, don’t worry, it’s not common, but stay in bed and after three days you’ll be ok. Absolutely brilliant! And with an iPhone of course I can send a picture of a rash or a wound and say, Dr Richard, what’s your opinion?
Q) What’s inside your travel kit?
A) It depends where I’m going – tropical area, somewhere very remote, whatever. Not every medication for every possibility, but for a lot of possibilities. In Africa, sometimes you need to walk five to 10 days to find any medical facilities. It’s the nature of the job that often I’m following rebels in a very remote area so you can quickly go through all the kit. In Central African Republic I got some infection and needed to test if I had malaria again. I was in Bambari with Seleka Islamist rebels and there’s nothing there, really. No medical facilities. So the medical kit’s sterile syringes, tests, antibiotics, everything, it’s very useful.
Q) You once said ‘the eye of the sniper is everywhere’. Has it ever caught you?
A) I was shot in my right leg in Egypt. It was a bad experience because the Egyptians told me “It’s just a small pellet, not very deep. It’ll get infected and just jump out.” So I took the antibiotics in the kit but after 10 days I see the infection again and Dr Richard said, “That’s not good, you know.” I saw another Egyptian doctor; he said the same thing: “It’ll jump out!” So I went back to Serbia and I found a military doctor who said, “They’re mad! Look at your leg! If you didn’t come now, you might need amputation.” I always like soldiers, they know what they are doing. He had been in the war in Bosnia. He told me, “I took a lot of metal out of humans. I’ll fix you, boy.” He took out a 8.2mm pellet, gave me more antibiotics, and I was ok.
Q) You’ve also said you love to go into a conflict zone – so where have you been recently?
A) Last year I did Lebanon, spent lots of time in south Lebanon. What else? I can’t remember but I was three times in Port au Prince in Haiti. That was tough. It’s like an outlaw country. Eighty per cent controlled by different gangs. Raiding, burning, taking everything. The last time, I was focussed on child soldiers, kid gangsters. Kids nine, ten, 11, with 9mm guns. Shooting without hesitation, quick reactions, handling guns well. I’ve been in the army but was in total shock, seeing that.
Q) How do you relax when you’ve finished work for the day?
A) Cigarettes. In Haiti I found a hotel at the edge of the front line, the Hotel Plaza.
No one else was staying. Only me with a fixer and two motorbike drivers to move us around. All night you could hear bang, bang and stuff. But the staff were really nice. The food was wonderful. The biggest trouble was, I’m sitting on the balcony, it’s really humid, I’m sweating, and I’m looking at the beautiful blue swimming pool and it’s tempting to jump in it. But Dr Richard told me a long time ago, if a pool isn’t treated with chlorine there’s a high possibility of getting giardia. No guests – hmm, I knew the manager he wouldn’t be spending money on chlorine. My fixer jumped in and he was unwell for two days.
Q) Do you often have to just bed down on the ground while working?
A) Often. One picture I took which became quite famous, that was in Afghanistan, a US Marine Sergeant Bee being shot at. It was very early morning; we had been camping and I had just wake up. When Taliban suddenly started shooting I was still in my just boots and underpants. It was so quick, I didn’t even know if I had the picture.
Q) When did you first pick up a camera?
A) When I am 14, 15, my parents had a bit of desperation to take me off the streets, playing football, fighting, messing around, so my father gave me a camera. And I loved it! It was amazing. It’s a beautiful toy. It was a Russian copy of a German Leica with no light meter. A friend of my sister, Mico Smiljanic, a photographer, helped me a lot. I learned to understand light, what is reflecting light, what is coming in at an angle, how it’s behaving. Everything in photography is about the situation of the light.
Q) How you start working as a photographer?
A) In Belgrade, 1987, when I was 18, I did one year of national service. I was still not behaving well, so my father – he was a chemical technician in a factory – wanted to put me in order. I loved it. It was just before the Bosnian war, so my father did me a great favour. Discipline, waking up early, exercising, all good. Then the Bosnian war started. Serbia was bombed by NATO. I had my camera, I knew how to look after myself, and that’s how I started.
Q) What kind of conflict produces the best pictures?
A) When you’re with soldiers on foot, although now with drones it’s more difficult, drones have really changed the dynamic. When governments and armies create restrictions, then you don’t have good pictures. I don’t want to do only what I’m allowed and what the new security advisors show me. But us who have field experience, we understand we have no idea how we’re going to get the picture. You look, and you see opportunities. You need to be very patient. Sometimes I wait weeks, months. I don’t have any vision of the pictures I want to get. Zero. But when I see an opportunity, I’m going to push for it. I want to see the fear, I want to see the faces, I want to tell the story properly.
Q) Are you usually sympathetic to the cause or side you’re photographing?
A) I’m a journalist: I’m not supporting any side. You have good guys, you have bad guys, and the truth is somewhere in between. I try to cover untold stories important to people.
Q) Do you feel traumatised by what you’ve witnessed – the maiming, desperation, death?
A) You need to be stable in your head, doing this. A couple of years ago in Canada, Anthony Feinstein, a psychologist, wrote a book, Shooting War, about how war affects journalists, especially photographers. They brought a bunch of us with this kind of experience to talk.
A lot of my colleagues have PTSD, mental troubles, as a result of what they’ve seen. I don’t think I have PTSD. But crazy people don’t believe they’re crazy, so maybe I have.
Q) You’ve said you love to go into a conflict zone. Is that still true?
A) When I go to say Syria, I know exactly what I’m doing, where I’m going. I’m not going to Nice or Cannes, the red carpet. I started this work very young, and when you work, if you’re emotional, you are not for this job. You have to work hard, be disciplined. I always joke when the correspondents start running, I’m starting to work. As a journalist, you can write your story about Syria from London. I need to see everything and I need to come close, close, closer.
Q) Your life must be hard on your family
A) Ha ha, I am the perfect husband, away all the time! I’ve been married three times although not now. My daughter, she’s 29. I live now in a village outside Belgrade; when I’m home, I dig my garden, I use the gym, I use the punchbag under my walnut tree. When I say to my daughter, “Do you want to come over, to stay this evening?”, she says, “Dad, I know that just means you want to go to the bar and have me get you home!” But what else am I going to do, be a bus driver? I’m just a yob from Belgrade! A peasant! But I work hard. My mother said once, “I’m just glad you’re not in prison!”
Q) Any regrets?
A) I’m sorry I missed the Battle of Stalingrad. That was the mother of all battles. But 1942, 1943. I was born too late!
On 14th August 2024, the World Health Organization declared outbreaks of mpox in Africa to be a Public Health Emergency of International Concern.
What is mpox?
Mpox is a viral infection that was previously known as “monkeypox”.
It shares some similarities with smallpox, to the extent that smallpox vaccine may be cross-protective; however, the illness is much less severe. (Waning population immunity to smallpox, since vaccination programmes ended in 1980, is one possible reason for the increased tendency to outbreaks now.)
So far, there have been 14,000 cases reported in Africa, with 524 deaths. Sweden has just reported the first case of clade I mpox outside Africa in the current outbreak (see below).
Previously confined to central Africa, recent outbreaks have ultimately spread globally, which is why the WHO has now decided to urge a concerted global response.
How is it spread?
The infection is spread mainly by close direct / intimate contact with body fluids and secretions, and by sexual exposure.
It can also be spread by contact with animals, or their droppings, or by eating under-cooked contaminated meat – so-called “bush meat”. The animal reservoir of infection is mainly among rodents and non-human primates.
The illness
Infection may be symptomless, but in most cases, symptoms appear 7 to 14 days following exposure.
Mpox is characterised by blistering skin lesions that are often extremely painful (and highly infective to other people), occurring particularly on the skin, genitals and face. They can be sparse, or even single blisters.
Other symptoms include fever, chills, headache, muscle aches, fatigue and swollen lymph glands.
The blisters may appear first on the face, spreading to other parts of the body; or alternatively in the genital area if the infection was acquired by sexual contact. Extensive lesions around the mouth may make eating and drinking painful or impossible, requiring intravenous treatment.
The illness is considerably more serious in people with HIV infection or reduced immunity. Severity of infection is also linked to the degree of exposure.
Mpox strains
There are two strains (called clades – Clade I and Clade II) that differ in severity and ease of spread.
Clade II tends to be more severe (up to 1,000 times more virulent than clade II) and occurs in Central Africa, Clade II occurs mainly in West Africa and may sometimes be more easily transmissible. Mutations into sub-strains is also occurring, which makes testing more complicated, especially in countries where resources are poor.
Where are cases occurring?
It is important to bear in mind that official statistics generally underestimate true numbers of cases, since not everyone with symptoms seeks medical attention, and not all cases undergo full testing.
Laboratory-confirmed cases have been reported in:
- Burundi: over 100 cases (Clade Ib) throughout the country
- Central African Republic: 28 cases (Clade I) throughout the country
- Côte d’Ivoire: 6 cases (Clade II) in Abidjan and Bas-Sassandra districts
- Democratic Republic of the Congo: > 14,000 cases (Clades Ia and Ib) throughout the country, mainly in Équateur, Sankuru, South Kivu, and Sud Ubangi provinces
- Kenya: 1 case (Clade Ib) in Taita-Taveta County
- Republic of the Congo: > 120 cases (Clade I) throughout most of the country, mainly in Cuvette, Kouilou, Likouala, and Point-Noire departments
- Rwanda: 4 cases (Clade Ib); no specified locations
- South Africa: 24 cases (Clade IIb) in Gauteng (12 cases and 2 deaths), KwaZulu-Natal (11 cases and 1 death), and Western Cape (1 case) provinces
- Uganda: 2 cases (Clade Ib) in Kasese District; no secondary transmission has been reported
A previous outbreak in 2022 resulted in spread to over 40 countries – with over 30,000 cases in the USA, for example, mainly in the MSM community.
Are visitors at risk?
Although current news reports of mpox cases are alarming and intended to generate a global public health response, so as to raise awareness and help bring outbreaks under control, most tourists and travellers to Africa are not at risk.
Travel to Africa for the usual tourist activities (e.g. safari, outdoor activities, beach) should be unaffected by the outbreak.
Older travellers who have previously been vaccinated against smallpox may still have some additional cross-protection against mpox.
- Risk arises from close contact (especially sexual contact) with infected people.
- Those at highest risk are men who have sex with men (MSM).
- High-risk behaviour is easily avoided, and safe-sex precautions reduce the risk of infection.
- Risk also arises from close physical contact with infected animals, or by eating under-cooked bush meat – which should be avoided. (Thorough cooking kills the virus.)
- Healthcare workers may be at risk if caring for people who are ill with mpox
- Journalists and news media personnel should avoid physical contact, keep their distance and observe the usual hygiene precautions when reporting on the evolving mpox outbreak situation
Mpox vaccines and treatment
- In the UK, vaccination is available for MSM and healthcare workers via the NHS.
- Current vaccines protect against all strains.
- Vaccination within 14 days of possible exposure also appears to confer protection (post-exposure protection).
- Several antiviral drugs can provide benefit in the most severe cases.
More information:
Oropouche Virus Disease: A growing concern in Central and South America.
As of mid-2024, Central and South America are experiencing a significant outbreak of Oropouche virus disease, impacting countries such as Brazil, Bolivia, Colombia, Peru, and Cuba.
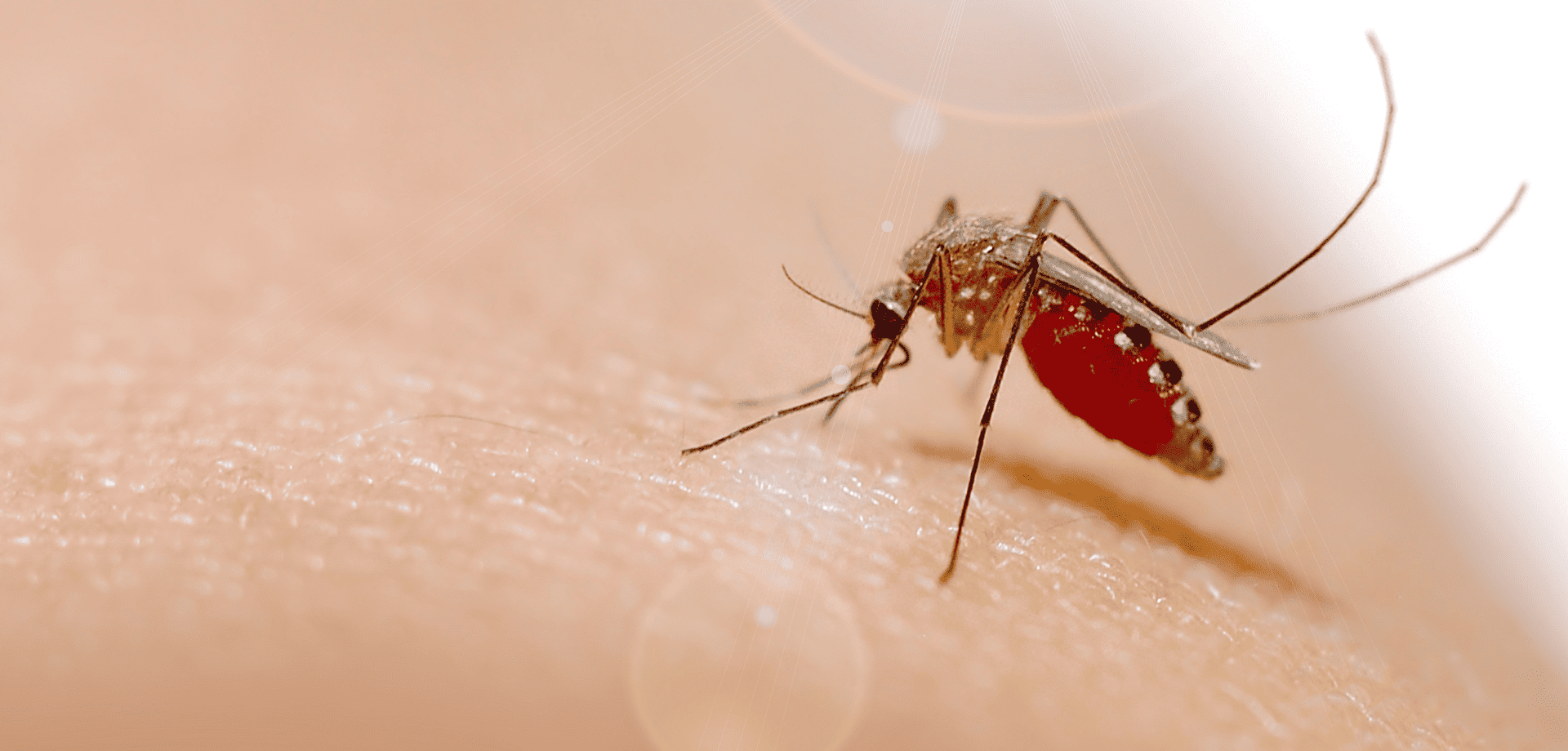
The Oropouche virus is primarily transmitted through the bites of infected midges (Culicoides paraensis) and mosquitoes. The virus is mainly spread in tropical and subtropical regions where these vectors are prevalent.
Symptoms of Oropouche virus disease include:
- sudden-onset fever,
- severe headaches,
- muscle and joint pain,
- rash,
- eye pain,
- nausea,
- and dizziness.
While most cases are mild and self-limiting, lasting 3 to 7 days, some individuals may experience more severe symptoms like meningitis and encephalitis.
There is no specific antiviral treatment or vaccine for the disease, so care focuses on symptom relief, such as rest, hydration, and pain management.
How to protect yourself from Oropouche virus
Preventing Oropouche virus disease involves reducing exposure to vector bites. Unlike mosquitoes, the main vector (midges) lacks a proboscis, and so is unable to bite through clothing.
Covering up, and wearing long-sleeved clothing, is therefore a keyway of preventing infective bites.
Other key measures include using plenty of insect repellent, impregnating clothing with Permethrin insecticide, using bed nets, and staying indoors during peak biting times.
Eliminating standing water where vectors breed is an important public health measure.
Prevention is key!
With no vaccine available, prevention remains the best defence against Oropouche virus disease.
Personal protective measures against insect bites also help protect against dengue, yellow fever, Zika, chikungunya, malaria, and a wide range of other tropical insect-borne infections, and should be followed carefully by travellers to tropical countries.
Cases found in Europe
Spain, Italy and Germany reported infections in numerous patients who had recently travelled to Cuba and Brazil.
The European Centre for Disease Prevention and Control (ECDC) warned of a moderate threat to travellers visiting Brazil, Bolivia, Colombia, Peru and Cuba, where Oropouche virus (Orov) is currently spreading.
If you’ve recently travelled to a known outbreak area and are experiencing any of the symptoms mentioned above, it is important to mention this to your doctor. This will help them rule out an Oropouche virus infection.
Worried about your upcoming travel plans?
Schedule a travel consultation with one of our specialist travel nurses.
They will guide you through potential health risks and recommend the necessary preventive measures and vaccinations to ensure your safety while travelling.
For more information on:
ESSENTIAL CHICKENPOX VACCINE FACTS:
- The chickenpox vaccine is not currently given by the NHS, but is part of the childhood vaccination schedule in other countries
- Chickenpox is a highly contagious infection caused by the varicella zoster virus
- In the UK, it mostly affects children
- It can be itchy and uncomfortable, can leave scars, and can sometimes cause severe disease – adults may suffer more serious symptoms, including pneumonia
- Chickenpox is spread by inhaling droplets coughed up by people infected with the virus
- People with chickenpox become contagious about 2 days before the appearance of the rash, which can make it difficult to avoid infection
- The chickenpox vaccine (varicella vaccine) can be administered from the age of twelve months onwards
- Two doses of vaccine are needed, with a 4 week gap between doses
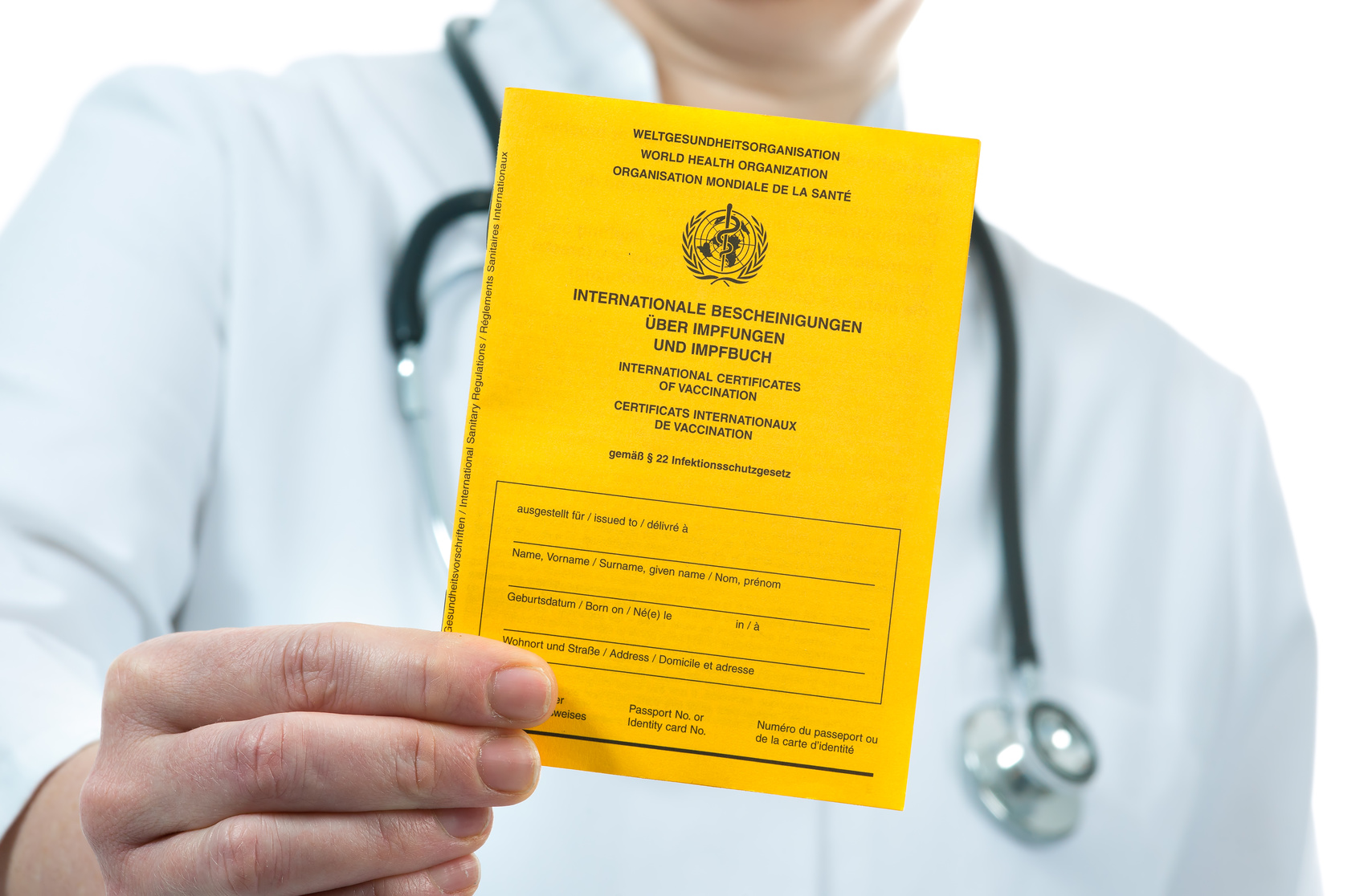
- If your child is receiving the MMR vaccination or a Yellow Fever vaccine, the varicella vaccination must either be given on the same day, or 4 weeks later
HOW TO BOOK A VACCINATION APPOINTMENT
Fleet Street Clinic is dedicated to maintaining a good supply of the chickenpox vaccine.
Our private chickenpox vaccine service is undertaken by doctors and nurses with long experience of vaccinating children. Our family friendly clinic is sympathetic to parents’ needs and concerns, and we welcome any vaccine-related queries. We operate a Saturday vaccination clinic once a month, the next will be held on Saturday April 8th.
To book your chickenpox vaccination for yourself or your child, you can book online now.
Recent media reports have raised awareness of the effects of Meningitis B and the importance of the meningitis vaccine (if your child is aged under 12 months, the vaccine still readily available via your NHS doctor). Less well-known is the fact that there are different strains of Meningitis, with different vaccines protecting against them.
Strains and Meningitis Vaccines:
- Meningitis B: the protective single-strain meningitis B vaccine is Bexsero
- Meningitis A C W Y: the 4-strain vaccines Menquadfi and Nimenrix offer protection.
Meningococcal Meningitis and its Symptoms
Meningococcal meningitis is a bacterial infection that causes inflammation of the protective membranes surrounding the brain and spinal cord. It can affect people of any age, but those most commonly affected are children under 5, and teenagers and young adults heading off to university.
Initial symptoms may be similar to flu, progressing to:
- A high temperature/fever, with cold hands and feet
- Vomiting
- Refusal to eat
- Drowsiness
- Floppy and unresponsive
- Rapid breathing
- Neck stiffness
- Bright light sensitivity
- Pale, blotchy skin, and a red rash that doesn’t fade when a glass is rolled over it
- Convulsions or seizures
Further information: https://www.meningitisnow.org/meningitis-explained/
The specialists at the Fleet Street Clinic recommend getting your children vaccinated not just against Meningitis B, but against Meningitis A,C,W & Y strains as well (the vaccine is currently available and in stock).
Meningitis B Vaccines Availability
We currently have a good supply of Meningitis B vaccine, available on a first come, first served basis. You can book a Meningitis B vaccination appointment online.
From Sunday, June 12, 2022 at 12:01AM ET all COVID-19 testing entry requirements for international travellers to the United Stated were rescinded.
Arrivals no longer need to show proof of a negative Covid-19 test or documentation of recovery prior to boarding a flight to the U.S nor upon arrival.
The Centre For Disease Control (CDC) has reached the decision based on the high vaccine uptake and widespread population immunity.
In the statement they released, they explain; “The COVID-19 pandemic has now shifted to a new phase, due to the widespread uptake of highly effective COVID-19 vaccines, the availability of effective therapeutics, and the accrual of high rates of vaccine- and infection-induced immunity at the population level in the United States. Each of these measures has contributed to lower risk of severe disease and death across the United States. As a result, this requirement which was needed at an earlier stage in the pandemic may be withdrawn.”
Most countries, including the UK, have already abandoned testing requirements in a bid to return international travel to pre-Covid levels and it seems the CQC have decided it is now time for the U.S to do the same.
Does this mean that the COVID-19 pandemic has ended?
No, but it does signify a shift in the pandemic. As we see a worldwide reduction in covid cases and death rates, the CDC statement clarifies that whilst testing may not be necessary right now, they will continue to monitor the data and adapt accordingly.
They state; “CDC continues to evaluate the latest science and state of the pandemic and will reassess the need for a testing requirement if the situation changes”.
What about covid vaccinations…
Do I need to be vaccinated to travel to the U.S?
Yes, foreign travellers from outside of the U.S are required to be double vaccinated from COVID-19 to enter the country. But for people under the age of 18, U.S citizens/ nationals or lawful permanent residents will be exempt from vaccination requirements. Currently, the Covid Booster vaccination is not a requirement and there is no set expiry date on the first dose of vaccination.
Overall, the easing of the US Covid restrictions is welcome news to the travel and tourism industry and demonstrates the possibility of international travel returning back to its pre-covid levels.
However, the absence of masks, vaccines, or travel mandates does not mean that the risk of catching Covid-19 has gone away.
We strongly recommend:
- Having comprehensive travel health insurance for all travel to the USA – hospital care should you require treatment for Covid is very costly.
- Wearing a high filtration (N95 or FFP3) mask during your journey
- Practising all the usual hygiene recommendations during your journey (e.g. hand sanitisers, distancing where possible
- Having an early test and avoiding travel if you have even minor symptoms.
For more information on the covid testing services available at Fleet Street Clinic.
With monkeypox cases being recorded in over 20 countries across the globe, people are becoming increasingly concerned about its spread and transmission.
Following 2 years of the Covid-19 pandemic, this outbreak has reignited the public’s fear and uncertainty of infectious diseases.
Whilst the media coverage of the monkeypox outbreak is alarming, we would like to reassure our patients that as it stands, the risk is still very minimal and vaccination is not advised as a precautionary measure. Whilst vaccines will undoubtedly be a key part of containing the outbreak, for now, only people who may have been exposed are being offered vaccination.
Our Medical Director & Travel Medicine Specialist, Dr Richard Dawood explains;
“Lots of people have been getting in touch with us to ask about a monkeypox vaccination, but this is not available privately. It is currently only being offered to anyone identified as a direct, close contact of a confirmed case deemed to be at sufficient risk.
The current outbreak does, however, highlight the need to think about your vaccine protection more generally, whether for travel or simply to protect your health and well-being, taking advantage of the best vaccines currently available.”
In a more general sense, it is never too late to catch up on childhood vaccinations, incomplete vaccination courses or any required boosters.
Your immune system naturally decreases with age and certain diseases are also more prevalent in older adults so there may be new vaccinations which are now suitable for you to consider for preventable diseases. Some health conditions can also weaken the body’s immune response, making you more vulnerable to infectious diseases, complications and hospitalisation. Therefore, it is important to ask your GP which vaccinations would be suitable for keeping you healthy.
– For more information on wellness vaccinations.
If you are travelling soon and haven’t had a travel consultation with a travel nurse, perhaps it is time to consider one. Travel nurses are experts in travel health and will advise which travel vaccinations & medications you should consider based on the risk of where you are travelling to and your itinerary once there.
– For more information on travel consultations.
To conclude, we’d like to dismiss a couple of dangerous myths about monkeypox that are unnecessarily scaremongering the public:
Myth 1: Monkeypox is as contagious as COVID-19 or smallpox
Fact: Monkeypox is far less contagious compared to smallpox, measles, or COVID-19.Myth 2: Monkeypox is a new virus.
Fact: No, the monkeypox virus is not a novel virus. It’s a known virus and is generally seen in central and western African countries as localised outbreaks.In summary, we, like the rest of the medical field, will be keeping a close eye on the progression of the Monkeypox outbreak and should our advice change based on new information, we will update this statement accordingly.
For more information on Monkeypox.
Exercise More – Get Outdoors
Today is National Fitness Day. September is a great time to redress the balance after summer holidays and make a new exercise plan. Time to get out and get moving!
Regular exercise has many benefits – a healthier heart, increased well-being, and a better quality of life. Research shows that if you exercise with friends, you are more likely to continue to keep fit, as the social environment encourages positive associations with the activity.
Exercising outdoors can contribute to this feeling of wellbeing. Organised outdoor exercise groups have grown in popularity recently, with a wide range of community-based activities across the country. A few of the more popular outdoor exercise activities are detailed here:
Park Run – Over 1 million Britons have taken part in Park Run – the Saturday morning 5k run in local parks across the country.
Project Awesome – A free community exercise group based in London, Bristol and Edinburgh, Project Awesome is based on high-energy, early morning exercise classes designed to kick-start your day.
Good Gym – For those who’d like to combine voluntary work with exercise, Good Gym enables you to meet like-minded people to run and work together on community projects in your local area.
British Military Fitness – Operating in parks across the UK, British military fitness classes are run by serving or former members of the armed forces with recognised fitness training qualifications. Classes are graded by ability group and are for members of the public. They are designed for all abilities, from those just starting to exercise who want to lose weight, to the already very fit.
Open Air Swimming – If you’re a keen swimmer, have you ever tried swimming outdoors? There are many reported benefits to open-air swimming, which can be enjoyed all year round even in the UK, with or without wetsuits. Check Wild Swim for your nearest open-air swimming site.
Getting Fit with Fleet Street Clinic
Our podiatrists can offer advice on appropriate footwear for exercise and our dietician and osteopath can work with you to support your exercise regime, ensuring a holistic approach to achieving a long-term, healthier you.
Imagine you’re holidaying in a tropical paradise, walking barefoot on the beach. Would you consider this a health risk? What if this simple, carefree activity could turn your trip into a nightmare?
Unfortunately, this is what happened to a Canadian couple in the Dominican Republic, who contracted hookworm in Punta Cana after walking on the beach without shoes.
Fleet Street Clinic’s medical director, Dr Richard Dawood, is Telegraph Travel’s medical expert and shared his medical opinion on the case in a recent article.
The article details the story of the couple, who shared their plight on social media to raise awareness of the parasitic worm infection.
Hookworm can infect humans if soil contaminated with their larva comes into contact with bare skin. Most commonly, hookworm infection can occur in Africa, the Americas, China and south-east Asia, according to the NHS.
Dr Dawood explained to the Telegraph how you can spot a hookworm infection:
“Typically there is a linear rash that follows the track of the migrating larva. It can become almost unbearable itchy, much worse than an insect bite, which is an important clue. There’s a local allergic reaction, which can then blister, making the line pattern harder to spot.”
And how to treat: “There are a number of different anti-parasitic treatments that work, either taken as tablets, or made into a cream and applied locally. The larvae can sometimes also be killed using cryotherapy to freeze them. Blisters or scratching can easily lead to infection, necessitating antibiotic treatment.”
To avoid hookworm, avoid coming into contact with soil or sand that could be contaminated. If walking on the beach, it’s advisable to wear shoes at all times!
Dr Richard Dawood at Fleet Street Clinic
Dr Richard Dawood is founder of Fleet Street Clinic in London and has practiced for over 35 years. He was one of the first doctors in the UK to establish Travel Medicine as a distinct speciality. Richard is the most senior UK travel medicine specialist working exclusively in a private setting.
You can book a travel consultation appointment online.
How to Cope During a Heatwave
The UK is currently experiencing a heatwave with temperatures rising to 35 degrees in some parts of the country this week. While sunshine is welcome and the vitamin D is much needed, too much heat can lead to illness. To avoid any heat-related sickness, make sure you are well-prepared! Follow Fleet Street Clinic’s tips to help keep safe during the hot weather.
Risks During the Heat:
- Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes causing rapid dehydration. This can result in heat exhaustion or heatstroke which can be life threatening if not dealt with promptly.
- The highest risk groups are the elderly, babies, children and those with pre-existing medical conditions.
- If you engage in strenuous physical activity this will increase the risk of illness related to the heat.
Top 7 Tips For Beating the Heat
- Seek shelter and shade during the middle of the day (11am -3pm).
- If you are outside, ensure you protect your skin against the sun with a high factor sun cream, hat and sunglasses.
- Wear loose fitting, light-weight and light colour clothing.
- Keep hydrated by drinking plenty of fluids and eating food with a high water content (such as fruit).
- Ensure you are taking in sufficient salt in your diet (sweating leads to electrolyte and salt depletion).
- Avoid caffeine and alcohol, which can worsen heat-related illness.
- Heat stroke can be a life-threatening emergency and medical help should be sought.
About Fleet Street Clinic
Fleet Street Clinic is an independent healthcare practice in London. For more advice or to book an appointment with our expert medical team, you can book online.
What is HPV?
Human Papillomavirus, or HPV, is the name of a group of viruses with around 200 different types, that is most commonly passed on via genital contact.
Although HPV is highly common, 90% of HPV infections go away by themselves and do not cause any harm. Most people with HPV never develop symptoms or health problems.
However, it is possible for HPV infections to persist and cause cellular change in your body. This can lead to:
- Cancer of the cervix, vulva, and vagina in women
- Precancerous lesions in men and women
- Genital warts in men and women
- Head and neck cancers in men and women
HPV vaccines have a well-established role in preventing cervical cancers as well as these other aforementioned conditions.
Who Should Be Vaccinated against HPV?
In theory, HPV vaccines are best given to young people before they become sexually active, and therefore before they can be exposed to HPV.
Individuals who are already sexually active might also benefit as they may not have yet acquired all of the HPV strains covered by the vaccine. Patients aged under 16 can only be vaccinated with their parents present.
Why Boys should receive the HPV Vaccine
- About 15% of UK girls who are eligible for vaccination are currently not receiving both doses. This figure is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries which have no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high: treating anogenital warts alone in the UK is estimated to cost £58 million a year, while the additional cost of vaccinating boys has been estimated to cost about £20 million a year
Source: HPV Action
To book an HPV vaccination for yourself or your child, you can book an appointment online. Or find out more information about HPV here.
We are very sorry to hear that Interhealth is ceasing to trade. As a hugely respected health practice, it is a great loss for Travel Medicine in the UK.
Fleet Street Clinic is in contact with Interhealth to offer support and provide continuity of medical care for existing individual and corporate Interhealth clients as required.
If you are looking for continuity with Interhealth services as an individual, or if you require corporate services such as Occupational Health and Travel Healthcare including travel vaccinations, please get in touch.
For more information please call Fleet Street Clinic on 0207 353 5678 or email at info@fleetstreetclinic.com
Stoptober is a good time to reflect on smoking habits and how to improve health issues related to tobacco use.
Quitting smoking is one of the most effective ways you can improve your health and the benefits start almost immediately. And remember, it’s never too late to quit!
The benefits of stopping smoking
After 20 minutes
Blood pressure and pulse are normalised, blood circulation improves.
After 8 hours
Levels of carbon monoxide in the blood decrease.
After 48 hours
Your sense of smell and taste are improving.
After 2 to 3 days
Less or no phlegm in the throat, fewer breathing difficulties.
After 5 to 7 days
Your breath is fresher, your teeth are cleaner and energy levels higher.
After 2 to 3 weeks
Physical withdrawal symptoms will stop, and you can now go several hours without thinking about smoking. Your risk of blood clots (thrombosis) is reduced.
After 4 weeks
Coughing, blocked sinuses and breathing difficulties should subside. The lungs are better able to resist infection.
After 2 to 3 months
Lung function improves by 5%.
After 1 year
The risk of developing cardiovascular disease is halved.
After 2 to 3 years
The risk of developing severe pneumonia or flu is the same as for a non-smoker. Your risk of heart disease, angina (chest pains) and stroke continues to fall.
After 5 years
The risk of throat, oesophageal and bladder cancer is halved.
After 5 to 10 years
The risk of developing cardiovascular disease or thrombosis is the same as for a non-smoker.
After 10 years
The risk of lung cancer is halved. The risk of developing osteoporosis decreases.
After 15 to 20 years
The risk of lung, throat, oesophageal or bladder cancer is the same as for a non-smoker. But heavy smokers (20 a day) have double the risk of lung cancer for the rest of their lives.
Help with quitting
If you need any advice or help to stop smoking, you can book an appointment with one of our GPs.
Measles Outbreak – What You Need to Know
The WHO has issued a warning about recent outbreaks of measles in Europe and the USA. Cases of measles have risen rapidly in recent months in Italy, Romania and most recently in US.
Measles is a highly contagious virus with potential for serious complications.
Initial symptoms can include:
- Runny nose
- High Temperature
- Spots in the mouth
- Aches and pains
- Sore eyes and swollen eyelids
A rash appears after 2-4 days which can present as blotchy spots, often starting at the head and progressing down.
Medical Advice for Measles
If you think you may be suffering from measles, or are concerned about risk of infection when travelling, please see your doctor straight away.
Travelling to areas with a risk of measles
Make sure you are up-to-date with your vaccinations before you travel, including the measles, mumps and rubella (MMR) vaccine. If your child will be travelling, the MMR can be given from 6 months of age. If you have not had measles or if you have not had two doses of MMR, you may be at risk. Measles is easily passed from person to person and can be a serious illness in adults as well as children. It is never too late to have the vaccine.
Call Fleet Street Clinic for medical assistance, advice on vaccinations and travel precautions on 0207 353 5678 email info@fleetstreetclinic.com or book online now.
FINISHING THE LONDON MARATHON
The 2018 London Marathon is just around the corner! Are you preparing for the run this year? If so, you’ll be very aware of the struggle ahead. A challenge like a marathon is incredibly rewarding but also tough on the body. Increasing your exercise capacity to this level pushes the limits of endurance both physically and mentally.
But even though this can feel torturous at times, you should not ignore recurrent pain or discomfort that persists after adequate rest. A common mistake is to push through and wait until pain prevents training before seeking care. By then, prolonged time off is often necessary to heal. It is estimated that 50 to 70 percent of first-time marathon runners drop out before their race.
If you do pick up an injury:
- First and foremost, stop and get it assessed.
- Maintain your strength and endurance as much as possible while recovering from your injury. If it prevents you from running, low-impact cardio exercise such as swimming, cycling or pool running can continue to improve exercise tolerance.
- Don’t be over-anxious to return to running, a good indicator of readiness is once you can walk for 30 minutes without pain during or after, you can begin a slow, careful return to pain-free running.
- Do not push through the pain.
Moving forward
As you increase your training and running, consider a biomechanical assessment. Slight problems in gait caused by many issues from footwear to posture to old injuries can cause new injuries (knees are particularly susceptible), or cause you to have to slow your pace or walk during the race.
Listen and respond to your body throughout training and recovery, and that finish line is waiting for you!
Post race
As you can imagine, a marathon takes its toll on the body in many ways. A post race assessment is well worth it, to identify any issues caused, not to mention a treatment to work out some of that lactic acid and to restore full function to the joints and muscles.
Our osteopath Andrew Doody and podiatrist George Hill can help with any marathon-related complaints. For more training tips and advice, or marathon injury treatment you can book an appointment online.
Ask the average person what viral disease they think claims the most lives, and HIV might be the likely response. However, this is not so, according to research in the Lancet. The research suggests that viral hepatitis caused 1.45m deaths in 2013 compared to 1.2m lives claimed by AIDS in 2014. What is Hepatitis?
Hepatitis is best defined as an inflammation of the liver caused by the hepatitis virus. There are 5 types of hepatitis virus called; A,B,C,D and E. Contaminated food is usually the cause of virus types A and E. Types B, C and D are spread via infected bodily fluid contact. Virus types B and C lead to the most deaths.
Prevention
Hepatitis A and B are vaccine preventable. Many countries offer these vaccines routinely on the childhood schedule but this is not the case in the UK.
Hepatitis Vaccination at the Fleet Street Clinic
Vaccinations are needed to give protection against hepatitis A and B and they currently are not part of the childhood vaccination schedule in the UK. At the Fleet Street Clinic, we make it a priority to have a good supply of hepatitis A and B vaccines for children all year round. The hepatitis vaccinations can be given individually, or as a combined injection. For long lasting protection, several doses are required. Our vaccination team are highly trained, well-qualified and have dozens of years’ experience between them. Our vaccination service takes place in a clean, comfortable and safe environment.
You can learn more about our vaccinations here.
While hepatitis is causing millions of fatalities across the globe, you can take steps towards protection against the virus by booking an appointment for hepatitis vaccinations at Fleet Street Clinic today.
Cases of measles reported in the UK
A number of cases of measles have been reported in Liverpool and Leeds. Recent outbreaks in Europe, where countries such as Romania and Italy have been affected, are believed to have caused the increase in UK cases. To date, 17 cases in Leeds and 8 cases in Liverpool have been reported.
Measles virus
Measles is a highly infectious virus which can be transmitted to anyone who is not vaccinated, most commonly to young children. To prevent outbreaks, it is recommended that 95% of the population is vaccinated.
Initial symptoms can be similar to a cold and include:
- Runny nose
- High Temperature
- Spots in the mouth
- Aches and pains
- Sore eyes and swollen eyelids
A rash appears after 2-4 days which can present as blotchy spots, often starting at the head and progressing down. MEDICAL ADVICE FOR MEASLES
If you think you may be suffering from measles, or are concerned about the risk of infection, please see your doctor straight away.
Vaccination against MEASLES
Make sure you are up-to-date with your vaccinations including the measles, mumps and rubella (MMR) vaccine. Although the NHS immunisation schedule offers the vaccine to children from 12 months of age, the MMR can be given from 6 months. If you have not had measles or if you have not had two doses of MMR, you may be at risk. Measles is easily passed from person to person and can be a serious illness in adults as well as children. In 2012 there were 122,000 deaths worldwide caused by measles. It is never too late to have the vaccine.
MMR Vaccination at Fleet Street Clinic
You can book an MMR vaccination online.
Measles Vaccination
Public Health England has implemented emergency measures to ensure the Hepatitis B vaccine is protected for those who need it most, due to severe shortages in the supply of the vaccine.
The UK is a low-risk country for Hepatitis B those most at risk are babies. The Hepatitis B vaccination has recently been added to the standard NHS immunisation schedule, which is not affected by the current shortage.
Individuals can reduce their risk of contracting hepatitis B through avoiding unprotected sex and injecting drugs, avoiding getting tattoos, piercings or acupuncture when overseas, and avoiding medical or dental care in high risk countries unless absolutely necessary.
A spokesperson for Public Health England said “We think there will be shortages until early 2018 so we are urging people to make sure they are taking the right precautions while the shortage is ongoing.”
For all those needing vaccination and immunisation support, Fleet Street Clinic offers expert travel advice, occupational health assessments and a dedicated vaccination clinic with expert medics for all those needing vaccination and immunisation support.
Our Travel Clinic can provide you with all the vaccines you need.
All of our travel and wellness vaccination appointments are available to book online.
Fleet Street Clinic’s monthly Saturday Clinic will be held on Saturday, August 12th, 9am -1pm. Patients have access to all nurse services – including travel jabs and childhood immunisations.
We have good stocks of vaccines which are in short supply at the moment, such as Hepatitis A and Hepatitis B.
If you’d like to bring your children for their immunisations or if you’re travelling over the holidays and need some last-minute vaccines, we can help.
You can book an appointment online.
HPV vaccine unavailable to boys on the NHS
The HPV vaccine is now offered to girls aged 12-18 years in the UK for free by the NHS.
Since its introduction in 2008, it has already shown to be very effective in reducing the cases of cervical cancer in females*. But the HPV virus doesn’t only cause cervical cancer, it can lead to other cancers such as anal, head, neck and throat cancers. Men are as much at risk of these cancers as women, so why are boys ineligible to receive the HPV vaccine as part of the NHS vaccination schedule?
The BBC has reported the case of Jamie Rae today, to highlight the issue. Mr Rae is campaigning for the HPV vaccine to be introduced, after undergoing radiotherapy for his throat cancer which he believes could have been prevented if an HPV vaccine had been available.
The article also reports that Professor Francis Vaz, a head and neck surgeon at University College London Hospital, paid privately to vaccinate his three sons, to protect them from certain cancers like anus, penis, mouth and throat. He said he saw on a daily basis that cancers driven by the HPV virus had been increasing in the past decade.
“I regularly see the bad end of that spectrum, so I thought the vaccination would be suitable for my sons,”
– he said.
“It’s just unfortunate it wasn’t available for them on the NHS. I was happy to pay for it because I think it’s a good vaccine.”
Why boys should receive the HPV vaccine
- About 15% of UK girls eligible for vaccination are currently not receiving both doses, a figure which is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries with no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high – treating anogenital warts alone in the UK is estimated to cost £58m a year, while the additional cost of vaccinating boys has been estimated at about £20m a year
Source: HPV Action
Our HPV vaccine page explains how get an HPV vaccine at Fleet Street Clinic.
FLEET STREET CLINIC – SPECIALIST VACCINE CLINIC
Fleet Street Clinic is a specialist vaccination clinic offering all vaccinations from travel jabs, to childhood immunisations to flu vaccinations programmes.
TO BOOK
You can book an appointment online.
Around 8 in 10 people don’t know what encephalitis is and so World Encephalitis Day aims to raise awareness of this illness, which causes brain inflammation and affects 6,000 people a year in the UK and has a high mortality rate.
Symptoms of Encephalitis
Infectious encephalitis usually begins with a ‘flu-like illness’ or a headache. Typically more serious symptoms follow hours to days, or sometimes weeks later. The most serious finding is an alteration in the level of consciousness. This can range from mild confusion or drowsiness to loss of consciousness and coma. Other symptoms include a high temperature, seizures (fits), aversion to bright lights, inability to speak or control movement, sensory changes, neck stiffness or uncharacteristic behaviour.
Autoimmune encephalitis often has a longer onset. Symptoms will vary depending on the type of encephalitis related antibody but may include: confusion, altered personality or behaviour, psychosis, movement disorders, seizures, hallucinations, memory loss, or sleep disturbances.
WHAT IS ENCEPHALITIS?
Encephalitis is an inflammation of the brain. It is caused either by an infection invading the brain (infectious encephalitis) or through the immune system attacking the brain in error (post-infectious or autoimmune encephalitis).
Anyone at any age can get encephalitis. There are up to 6,000 cases in the UK each year and potentially hundreds of thousands worldwide. In the USA there were approximately 250,000 patients admitted to hospital with a diagnosis of encephalitis in the last decade.
CAUSES OF ENCEPHALITIS?
The inflammation is caused either by an infection invading the brain (infectious encephalitis) or through the immune system attacking the brain in error (post-infectious or autoimmune encephalitis). Viruses are the most frequently identified cause of infectious encephalitis (e.g. herpes viruses, enteroviruses, West Nile, Japanese encephalitis, La Crosse, St. Louis, Western equine, Eastern equine viruses and tick-borne viruses). Any virus has the potential to produce encephalitis, but not everybody who is infected with these viruses will develop encephalitis. Very rarely, bacteria, fungus or parasites can also cause encephalitis.
SYMPTOMS OF ENCEPHALITIS
Infectious encephalitis usually begins with a ‘flu-like illness’ or a headache. Typically more serious symptoms follow hours to days, or sometimes weeks later. The most serious finding is an alteration in the level of consciousness. This can range from mild confusion or drowsiness to loss of consciousness and coma. Other symptoms include a high temperature, seizures (fits), aversion to bright lights, inability to speak or control movement, sensory changes, neck stiffness or uncharacteristic behaviour.
Autoimmune encephalitis often has a longer onset. Symptoms will vary depending on the type of encephalitis related antibody but may include: confusion, altered personality or behaviour, psychosis, movement disorders, seizures, hallucinations, memory loss, or sleep disturbances.
DIAGNOSIS OF ENCEPHALITIS
Symptoms alone often do not allow sufficient ability to distinguish between the many diseases that can mimic encephalitis. Therefore, doctors perform a variety of hospital tests – it is important that investigations are carried out as soon as possible as prompt diagnosis reduces mortality and improves the outcomes.
With increasing numbers of people travelling worldwide, it is important to highlight the risk of infectious encephalitis which can be spread by mosquitoes (Japanese encephalitis ), ticks (Tick-borne encephalitis,) or other animals (Rabies).
If you are concerned about travelling to an area with the possibility of encephalitis infection, please visit our country vaccination guide for specific advice on your destination.
Information from The Encephalitis Society
You can protect yourself from Japanese Encephalitis and Tick-borne Encephalitis with vaccinations. Book your travel vaccination appointment today.
HEPATITIS A and Hepatitis B VACCINES AT FLEET STREET CLINIC LONDON
Although Hepatitis A and Hepatitis B vaccinations are currently in short supply in the UK and globally, Fleet Street Clinic is committed to maintaining the stock of all vaccines and currently has a good supply of both.
Hepatitis A
Hepatitis A is a viral infection that is spread through food and water contaminated with the virus. It occurs world wide including Central and South America, Africa, Eastern Europe, Middle-East, Asia, and the Indian Subcontinent.
Hepatitis A affects the liver causing jaundice, and whilst most people make a full recovery, it can result in chronic liver disease and be fatal.
HEPATITIS A VACCINATION
Hepatitis A is easily preventable through vaccination, and there are several types of vaccination available in the UK that offer protection. The vaccination is available to adults and children over the age of 1 year. It can be given alone (Avaxim, Vaqta) or in combination with typhoid (Viatim), whereby a single injection provides protection for 12 months. A second injection given 6 months later will provide 25 years of protection against Hepatitis A.
The vaccination is available to adults and children over the age of 1 year. It can be given alone (Avaxim, Vaqta) or in combination with typhoid (Viatim), whereby a single injection provides protection for 12 months. A second injection given 6 months later will afford 25 years of protection against Hepatitis A.
It is also possible to receive Hepatitis A in combination with Hepatitis B (TwinRix or Ambirix) whereby 2 or 3 doses of the vaccination can be given between 3 weeks or 6 months.
In addition to the vaccination, travellers should exercise caution with food and water by:-
- Ensuring all food is cooked thoroughly and served hot
- Sticking to bottled water only with a seal or boiled water– no tap water
- Avoiding ice
- Only consuming fruit that can be peeled or sliced without contamination (such as bananas)
- Avoiding high-risk food such as shellfish, raw or rare meat, salad, buffet food, reheated food
HEPATITIS B
- Hepatitis B is a viral infection spread by contaminated blood and bodily fluids.
- 350 million people worldwide are carriers of the Hepatitis B virus.
- The highest risk countries for Hepatitis B infection are central, western and southern Africa and south-east Asia.
- Chronic infection with Hepatitis B can cause liver disease and liver cancer.
Hepatitis B is contracted through contact with infected blood or bodily fluids. These can include:
- Mother to baby transmission at the time of birth
- Unprotected sexual intercourse
- Through contaminated blood products (such as unscreened blood transfusion)
- Contaminated medical equipment (such as needles and syringes)
- Contaminated tattoo or body piercing equipment
- Through contaminated needles and syringes from injecting drug use
VACCINATION AGAINST HEPATITIS B IS ADVISED FOR:
- Those who are at occupational risk (such as health care workers, aid workers where their job puts them at risk of injury)
- Travellers who visit high-risk areas, or those who travel frequently or for longer periods
- Travellers who have pre-existing conditions whereby their condition may make it more likely for them to need medical attention
- Travellers who carry out activities associated with risk (adventure sports, body piercing, tattoos)
- Those who participate in lifestyle behaviours that may increase the risk (such as, unprotected sex and injecting drug use)
A Hepatitis B vaccine is available and can be given from birth. It requires a primary course of 3 vaccinations to be given over a 6 month period (0, 1 months, 6 months) with a booster dose given 5 years later. Those who require the vaccinations to be given more quickly, such as last-minute travellers, can receive the primary course over a shortened 3 week period. Hepatitis B can also be given in combination with Hepatitis A when protection against both diseases is required. TwinRix is available for both adults and children and adheres to the vaccination schedule outlined above. Ambirix is licenced for children under the age of 15 years and requires 2 doses 6 months apart.
BCG Vaccine Shortage in the UK
As the media has reported, the UK is in short supply of the BCG vaccine, impacted by global shortages.
The BCG vaccination gives worthwhile protection against tuberculosis, a serious infection spread by coughs and sneezes. In 2014, more than 6,500 TB cases were reported in the UK. Babies most at risk of contracting TB are those living in London and the Midlands, so if you live in these areas it is strongly recommended to have your baby inoculated.
At the Fleet Street Clinic, we have over 20 years experience as a specialist vaccination centre. We have a good supply of the BCG vaccine and run a designated BCG clinic for babies and children on Wednesday’s each week. All our vaccines are administered by highly qualified nurses or doctors, who will be happy to answer any queries or concerns.
What is TB?
TB is a bacterial infection spread through coughs and sneezes and affects the lungs, lymph glands, bones, and nervous system.
Where is the clinic?
The Fleet Street Clinic is located in Central London. Our address is 29 Fleet Street, London EC4Y 1AA.
How to Book?
With the new football season in full swing, it’s apt time to address one of the most common football injuries; hamstring pulls.
Hamstring Injury
This injury occurs when there’s a tear or strain to the muscles at the back of the thigh. By definition, hamstrings are a set of three muscles at the back of the thigh that all cross both the knee and hip joint, with only half of one (the biceps femoris) originating from the thighbone. Rapid acceleration movement is the main course of hamstrings getting injured. With football being a sport that relies heavily on quick movement in this area of the body, it is an injury your favourite footballer is highly likely to suffer from this season. There are three levels of severity to hamstring injuries. These are:
- Grade 1 – a minor strain
- Grade 2 – a partial tearing of the muscle
- Grade 3 – a complete tearing of the muscle
Symptoms of Hamstring Injury
This depends on what grade of the injury the player has.
- Grade 1 injury – consists of tenderness and sudden pain at the back of the thighs. Muscle strength will likely remain the same, but moving the leg might be painful.
- Grade 2 injury – more painful and more tender. Some bruising and swelling could occur in the area. There will also be a loss of strength in the leg.
- Grade 3 injury – have grade 1 and 2 symptoms at a more severe level. A popping or snapping sensation may be felt. The injured person may struggle to even be able to stand.
Treatment
There are initial steps that can be taken to treat hamstring injuries including compression, applying ice, elevation and good rest. Taking painkillers such as paracetamol can help reduce pain. Full recovery time will depend on the grade of injury. Professional footballers have access to equipment and health professionals that can help speed up recovery. Although self-treatment is an option for the everyday person, seeing a healthcare professional is advised if you’re concerned the injury is severe, the symptoms worsen or healing is very slow.
Osteopathy Treatment for Hamstring Injuries
Osteopathy is a medical specialty focused on musculo-skeletal problems. An osteopath deals with diagnosing, management and treatment of these types of injuries. If you’re concerned that you might be suffering from a hamstring injury or your self-treatment is not working out, book an appointment online and we can book you a session with Andrew Doody, our osteopath.
Prevention of Hamstring injury
There’s no surefire way of preventing an hamstring injury but there are steps that can be taken to reduce the likelihood. These include;
- Gentle stretching the hamstring area after exercise
- Warming up
- A longer warm-up period in cold weather
- If you feel any tightness, you might want to stop as this could be a signal that a tear might occur
BCG Vaccine for Children
At the Fleet Street Clinic in Central London, we have been providing specialist vaccination services for over 20 years. Our excellent relationship with a range of suppliers enables us to maintain good stock levels of vaccines, even where there may be supply shortages elsewhere.
We run a BCG clinic once a week for babies and children under the age of 6. Our baby/child BCG clinic runs on Wednesday’s.
Why have the BCG Vaccine?
The BCG vaccine protects against tuberculosis. TB is a bacterial infection that affects the lungs in most cases but can affect other parts of the body such as the bones and kidneys. Typical of many bacterial infections, tuberculosis can be spread through long-lasting exposure to an infected person via sneezing or coughing. The BCG vaccine is a proven way to ensure protection against the tuberculosis bacteria.
Vaccination for Babies and Children Under 6 years of age
The BCG vaccination is not offered to all children by the National Health Service. Some NHS boroughs do offer it as routine but are unable to supply at present due to the national shortage. The TB vaccination has to be sourced privately instead. With two decades of experience providing vaccination services, the Fleet Street Clinic provides a safe, child-friendly environment and the guarantee of an expert medical support service.
To protect your baby with the BCG Vaccine, you can book an appointment online.
There is currently an outbreak of Cyclospora related to travel in Mexico.
A Public Health England Health Protection Report highlights 204 confirmed cases since June 1st, 2016.
The cases are mainly associated with travel to Mexico, specifically the Riviera Maya Coast. The average incubation period is a week and infection is characterised by watery diarrhoea, fatigue, muscle pain, weight loss, nausea and low-grade fever. The foods previously involved in cyclospora outbreaks include soft fruits, such as raspberries, and salad products such as coriander, basil and lettuce. If untreated the illness can last for several weeks.
The Fleet Street Clinic can run a stool sample test that can diagnose Cyclosporiasis among many other causes of diarrhoea in returning travellers, and you will get your reults back in an hour of the test being done. If you are worried about any symptoms you have post travel to Mexico or any other country then call our reception team on 02073535678.
Or you can book an appointment online.
Bowel Cancer in the UK
The beginning of April marked the start of Bowel Cancer Awareness month. Bowel cancer is very treatable and one of the most common cancers in the UK.
40,000 cases are diagnosed every year. 1 in every 20 people will develop bowel cancer in their life time.
Symptoms of bowel cancer are often ones that you may find difficult to talk about or explain to your doctor. Nobody enjoys an uncomfortable conversation, especially when it comes to being candidly honest about something so private but the earlier it’s diagnosed, the greater the chance of survival is. It’s difficult, but let’s talk about it.
WHAT ARE THE SIGNS AND SYMPTOMS?
- Bleeding from your bottom and/or blood in your bowel movements
- A change in your bowel habits that lasts three weeks or longer
- Sudden and unexplained weight loss
- Extreme tiredness for no obvious reason
- A pain or a lump in your stomach
AM I AT RISK OF BOWEL CANCER?
Currently we do not know what causes this cancer. We have been able to identify some factors that can increase your risk of getting the disease:
- Aged over 50
- A strong family history of bowel cancer
- Being overweight or obese
- Lack of exercise and being inactive
- Longstanding inflammatory bowel disease such as Crohn’s disease or ulcerative colitis
HOW CAN I HELP PREVENT BOWEL CANCER?
There is no way to 100% prevent bowel cancer unfortunately. Things like family history, you cannot change.
However, there are some ways you can help yourself as recommended by the NHS.
- Improve your diet – eat less processed foods and red meat, eat more fish and fibre
- It is recommended that adults exercise for at least 2.5 hours a week
- Making sure you are a ‘healthy’ weight
- Stop smoking
- Cut down on alcohol
You can read all about these tips here on the NHS website.
GET SCREENED FOR BOWEL CANCER
If you are concerned about possible symptoms and are not eligible for NHS screening (aged between 60 – 74 and registered with a GP), you can make an appointment to speak with one of our experienced GPs (male or female GP’s).
If you need advice, get in touch with our expert GP’s and dietician at Fleet Street Clinic.
To book an appointment, head to our online booking system here. Alternatively, call us on 020 7353 5678 or email us at info@fleestreetclinic.com.
The Zika Virus has been making headlines recently for it’s frightening links to rare birth defects. Brazil has even gone as far as to warn women to avoid falling pregnant whilst an epidemic is rife. The link between 400 cases of new-borns with microcephaly in the north-east of Brazil is being investigate by health authorities.
The increase in microcephaly, a neurological disorder that stunts the growth of the baby’s cranium, limiting it to a circumference of less than 33cm, has increased in Brazil from 59 cases in 2014, rising to 1,248 cases throughout 2015. Typically, life expectancy for babies born with the condition is reduced. In 90% of cases, brain function is also reduced. There are currently no travel restrictions in affected areas.
How is the virus contracted?
The Zika virus is spread to people through the bite of an infected mosquito. Outbreaks have been seen across Africa, Asia, Central and South America.
What are the the symptoms and treatment?
The common symptoms, usually mild and often lasting from a few days to one week, can be a rash, fever, joint pain, and conjunctivitis. There is currently no vaccine to prevent or medicine to treat the virus. Pain killers can be used to alleviate these symptoms which often go mistaken as a fever, and can easily be missed, especially in the early stages of pregnancy.
Is there a way to reduce my risk?
Insect bite precautions is paramount, especially for pregnant women in the affected areas. The NHS travel website, Fit For Travel, recommends:
- Covering up – wearing long sleeved tops and long trousers
- Spraying thinner clothing with insect repellent
- Burning pyrethroid coils and heating insecticide impregnated tablets
- Sleeping in a screened room where possible or using a treated mosquito net
If you are travelling to Brazil or any of the infected areas, book an appointment with one of our dedicated Travel Clinic nurses for information on vaccines and travel wellbeing now on 020 7353 5678.
Zika Virus – Additional Resources
Zika virus: medical advice for travellers – The Telegraph – Richard Dawood
Zika Virus – Video
Watch Fleet Street Clinic’s Dr Richard Dawood discuss Zika Virus on Victoria Derbyshire.
The popular Thai tourist resorts of Krabi and Phuket are reporting high incidences of dengue fever this year.
Since January 2015 over 400 cases of dengue fever have been reported, resulting in one fatality.
Cases of dengue fever also soared in Malaysia with over 40,000 reported cases this year. It is estimated between 6-10 cases of dengue are diagnosed each day – double the rate of last year. The most dramatic increases have been seen in Penang, Johor and the state of Selangor.
Dengue Fever Advice for Travellers
Unfortunately, there is no vaccine or medication that can prevent dengue. The only way to reduce the risk is to prevent mosquito bites, particularly during daylight hours.
If you are off on an Asian adventure this summer, follow these simple steps to reduce the risk of dengue fever:
- Cover up with clothing
- Use insect repellents containing a minimum of 50% DEET on any exposed skin
- Consider treating clothes with permethrin
- Sleep under bed nets and use insect screens on doors.
- Reduce mosquito breeding sites by removing any water containers from outdoor areas
- Use air-conditioning
- Consider the use of plug-in electrical vaporisers which deter mosquitoes
Our Ultimate Bug Kit contains everything you need to help keep mosquitos at bay and is available to purchase online.
Fleet Street Clinic
For more information on Dengue or any other travel-related topic, you can book travel consultation appointment online.
India is currently experiencing a heat wave, with temperatures exceeding 47 degrees Celsius. The heat wave has now spread westwards, with temperatures in Pakistan and the Middle East reaching 50 °C. The highest temperature ever recorded was in Sweihan, Abu Dhabi at 50.5 °C.
Up to 2000 people have died in India as a result of sunstroke and dehydration related to the heat. It is expected that heat waves will continue through summer with Eastern Europe and the Balkans expecting temperatures exceeding 38 °C throughout July and august.
Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes causing rapid dehydration. This can result in heat exhaustion or heatstroke which can be life threatening if not dealt with promptly.
Any traveller can be at risk of sun and heat related injuries, but the highest risk is in the elderly, babies, children and those with pre-existing medical conditions.
Travellers who perform strenuous physical activity will increase the risk of illness related to the heat.
It can take the body up to 10 days to acclimatize to the heat, so it is important that travellers are prepared to prevent heat related illness.
What can travellers do?
*Seek shelter and shade during the middle of the day (11am -3pm) when temperatures are at their hottest
*If you are outside, ensure you protect your skin against the sun with a high factor sun cream
*Wear lose fitting light weight and light colour clothing
*Keep hydrated by drinking plenty of fluids and eating food with a high water content (such as fruit)
*Ensure you are taking in sufficient salt in your diet (sweating leads to electrolyte and salt depletion).
*Avoid caffeine and alcohol, which can worsen heat related illness
Heat stroke can be a life-threatening emergency and medical help should be sought.
http://www.aljazeera.com/news/2015/06/heat-wave-spreads-pakistan-gulf-150603102018356.html
World Malaria Day
Reaching the zero Malaria target
How You can Prevent Malaria
- Using antimalarial medication
- Spraying indoor walls and your clothing with insecticides
- Using insecticide-treated nets and window screens
- Wear light-coloured, long sleeve clothing
- Get rid of any stagnant water
Since 2017, the World Health Organization has supported a group of 21 malaria-eliminating countries through a special initiative called the “E-2020”. This report charts their progress towards a common goal: eliminating malaria within the 2020 timeline. According to this report, 8 E-2020 member countries reported zero indigenous cases of malaria in 2020, a remarkable achievement in view of the ongoing global COVID-19 pandemic. Maintaining zero cases is a testament to their commitment to protect hard-won gains and keep the disease at bay. You can find more on this report here.
More Information
Read more about malaria and how to you can prevent it.
For further information and a consultation with an experienced member of our travel team, you can book an appointment online here.
Measles on the rise:
The World Health Organisation (WHO), has reported that measles cases are on the rise worldwide and in Europe alone, outbreaks have surged to a 20-year high.
The WHO states that reported measles cases (provided by each country) currently show that about 229,000 cases have already been reported, compared with 170,000 for 2017. Worryingly the 2018 number is likely to rise as the reporting deadline ends April ’19.
With a 50% increase in measles cases last year, it is important to understand the benefits of vaccinating against measles:
Dr Richard Dawood, our Medical Director explains;
“I recently heard about a patient suffering a bad attack of shingles. She didn’t believe in doctors, medicines or vaccines, I was told, and was languishing at home, with a dreadful, crusted rash across her body, and burning with pain. She had stuck to her beliefs and refused to take antiviral medication that could have aborted the attack or reduced the probability of ending up with long term nerve damage and lingering pain. Shingles can strike more than once, but since she doesn’t believe in vaccines (there is a good one that is 95% effective) she will have to take her chances of a recurrence in future. I disagree with her opinions, but her latest actions will harm nobody but herself.
But measles is different: when it comes to vaccination, personal choices and opinions have a direct impact on the health and wellbeing of others – individually as well as for entire communities. Measles vaccination is a major public health issue. Memories of the past outbreaks, epidemics, tragic disability and loss of life that drove research and ground-breaking vaccine development now belong to a previous generation. In these days of “fake news”, “influencers” and social networks, it has become too easy to undermine confidence in matters of public health. In the case of measles, concerns about vaccine safety are down to the “fake research” of Andrew Wakefield, who was struck off the medical register for concocting a spurious link with autism in the 1990s. But the damage was long-lasting.
The complications of measles are most severe in babies who are not yet old enough to be vaccinated, and children with reduced immunity. When the rate of vaccination in the general population falls below 95%, outbreaks occur and can easily spread, with the highest impact on those most vulnerable populations, undermining years of hard work around the world to bring measles under control.
That is what is happening now”.
VACCINATION AGAINST MEASLES
‘The highly contagious disease can cause severe diarrhoea, pneumonia and vision loss. It can be fatal in some cases and remains an important cause of death among young children”, according to the WHO.
The disease can be easily prevented with two doses of a safe and efficient vaccine that has been in use since the 1960s’.
Make sure you are up-to-date with your vaccinations including the measles, mumps and rubella (MMR) vaccine. Although the NHS immunisation schedule offers the vaccine to children from 12 months of age, the MMR can be given from 6 months. If you have not had measles or if you have not had two doses of MMR, you may be at risk. Measles is easily passed from person to person and can be a serious illness in adults as well as children. It is never too late to have the vaccine.
Staying Healthy on the Slopes
Ski season is upon us, and it’s time to prepare yourself physically for your adventures on the slopes!
Skiing once a year can easily lead to injury – no surprise for such an intense activity, involving a range of muscle groups. And it’s not just skiing that’s physical; lifting skis, boots and using lifts can all take their toll on your body! In order to stay healthy this ski season, a little preparation is all that’s required.
Our Consultant Osteopath, Andrew Doody BSc (Hons), gives advice on how to avoid injuries so that you enjoy your holiday on the slopes.
Before your holiday:
- Build up your fitness gradually – walking quickly to work or weekend sessions on a cross-trainer will help you to prepare your muscles
- Start a stretching programme. Concentrate on quads, hamstrings and calves
- Don’t ignore any twinges you have – get yourself checked out by a professional before you travel
- Work on your balance – yoga postures will help
- Check your alignment; most skiers find turning one way easier than the other, which may be caused by either one-sidedness or muscle weakness
- Get professional advice on the best products to support a problem back, knees, ankles, or wrists
On the Slopes and Après Ski
- Ensure ski-boots are properly fitted. Ill-fitting boots can impact on your posture when skiing
- Warm up before you start and stop to stretch, especially at the end of the day
- Make sure to keep hydrated – easy to forget in the cold weather
- Beware when you’re walking with you ski gear! Lots of ski injuries come from carrying kit badly or slipping on ice away from the slopes
On Your Return
- Consider ways to improve your fitness level throughout the year and be well prepared for the 2018 season
- If you have any lasting pains, make sure to have a professional health check
Book an Appointment at Fleet Street Clinic
Want more professional support and advice before your ski trip?
Book an appointment to see Fleet Street Clinic’s Consultant Osteopath Andrew online.
The Fleet Street Clinic is committed to keeping journalists safe and well in high risk environments abroad.
The aim of this seminar is to provide a briefing for newsgatherers on the current crisis in West Africa, plus a hands-on training in biohazard protection.
Frontline Club, 13 Norfolk Place, London W2 1QJ
Thursday 2nd October 2014
9:30 – 14:30
The current outbreak of Ebola virus disease is unprecedented in scale and severity. The affected countries of West Africa do not have the resources or the public health infrastructure necessary to bring the outbreak under control, and massive external intervention will be needed. How long might it continue? How will it be covered as a news story? Will the need for news put newsgatherers at risk, and if so, how can risks be minimised? How should Ebola be reported upon? What impact is news reporting having upon the regional economy, and the global response?
These are some of the questions we hope to address in a special seminar aimed at print and broadcast media: bureaux chiefs, health & safety managers, and frontline news crew themselves, with a briefing from an internationally renowned expert in the field, and a practical, hands-on training session conducted by an expert in biohazard protection.
The event is free to attend, but places are limited, so please let us know if you would like to attend.
Programme
| 9:30 | Coffee, registration | |
| 10:00 | Ebola: background and analysis of the current West African outbreak | Prof David Heymann |
| 10:45 | Q&A / Discussion | |
| 11:15 | Coffee break | |
| 11:30 | Protecting News Media Personnel in a High Risk Environment: Introduction | Dr Richard Dawood |
| 11:45 | Biohazards: Principles of Personal Protection | Ian Samson |
| 12:15 | Lunch | |
| 12:45 | Biohazards: Personal Protection – Practical session | Ian Samson |
| 14:30 | Finish |
Speakers:
Professor David Heymann, CBE
David is Professor of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine; head of the Centre on Global Health Security at Chatham House, London; and chairman of Public Health England, UK. He has frontline experience of working with Ebola in Africa, having personally investigated some of the original outbreaks in central Africa going back to 1976. He is actively involved in the current international response.
Ian Samson
Ian is the EMEA Regional Training Specialist for DuPont Personal Protection. DuPont is currently supplying personal protective equipment to the WHO, MSF and other public health and aid agencies, including tens of thousands of coveralls. Ian’s expertise in this field is well known, and he has previously trained news media personnel during other public health emergencies, such as during news coverage of avian flu in Asia, in 2005/6.
Dr Richard Dawood
Richard is the medical director of the Fleet Street Clinic, a specialist in Travel Medicine, and a consultant to several news media organisations.
Personal Protective equipment will be available for delegate training, supplied by courtesy of DuPont and CES Ltd.
A new medical paper in Lancet Infectious Diseases has highlighted some of the countries at the highest risk for a major Zika virus outbreak. The study looked at air traffic between countries in the Americas, where Zika is already established, and places in Africa and Asia where the Aedes mosquitoes, the mosquitoes that can spread Zika, are most prevalent. The study also took other factors into account such as seasonality of transmission, population density, and economics to come up with a “hit list” of countries where Zika could potentially have the biggest impact.
Countries with larger volumes of travellers arriving from Zika virus-affected areas of the Americas and large populations at risk include:
- India (67,422 travellers arriving per year; 1.2 billion residents in potential Zika transmission areas)
- China (23,8415 travellers arriving per year; 242 million residents in potential Zika transmission areas)
- Indonesia (13,865 travellers arriving per year; 197 million residents in potential Zika transmission areas)
- The Philippines (35,635 travellers arriving per year; 70 million residents in potential Zika transmission areas)
- Thailand (29,241 travellers arriving per year; 59 million residents in potential Zika transmission areas).
Of the countries with the largest at risk populations, the authors suggested that India, the Philippines, Indonesia, Nigeria, Vietnam, Pakistan, and Bangladesh might be most vulnerable to impact because of their limited per capita health resources.
Dr Richard Dawood, Medical Director and co-founder of the Fleet Street Clinic, discussed the paper with one of its authors, as well as the current situation faced by travellers, on the Victoria Derbyshire programme on BBC2 on 2nd September.
“We have always known Zika could spread everywhere Aedes mosquitoes abound,” Dr Dawood told the programme. “This study tells us about the seasonality of risk of spread, and when/where it might take root, but does not model travel/risk of spread within Africa or Asia – so more studies are still needed.”
The study’s publication coincided with the arrival of Zika in Singapore – a major hub for Asian travel and Malaysia, with clear implications for further spread. With this news came the new evidence that Aedes aegypti mosquitoes are capable of passing the infection on to their offspring.
There is currently no vaccination available for the Zika Virus. If you have any questions and would like some more information and advice, please contact the Fleet Street Clinic on 020 7353 5678 or you can book a travel consultation appointment.