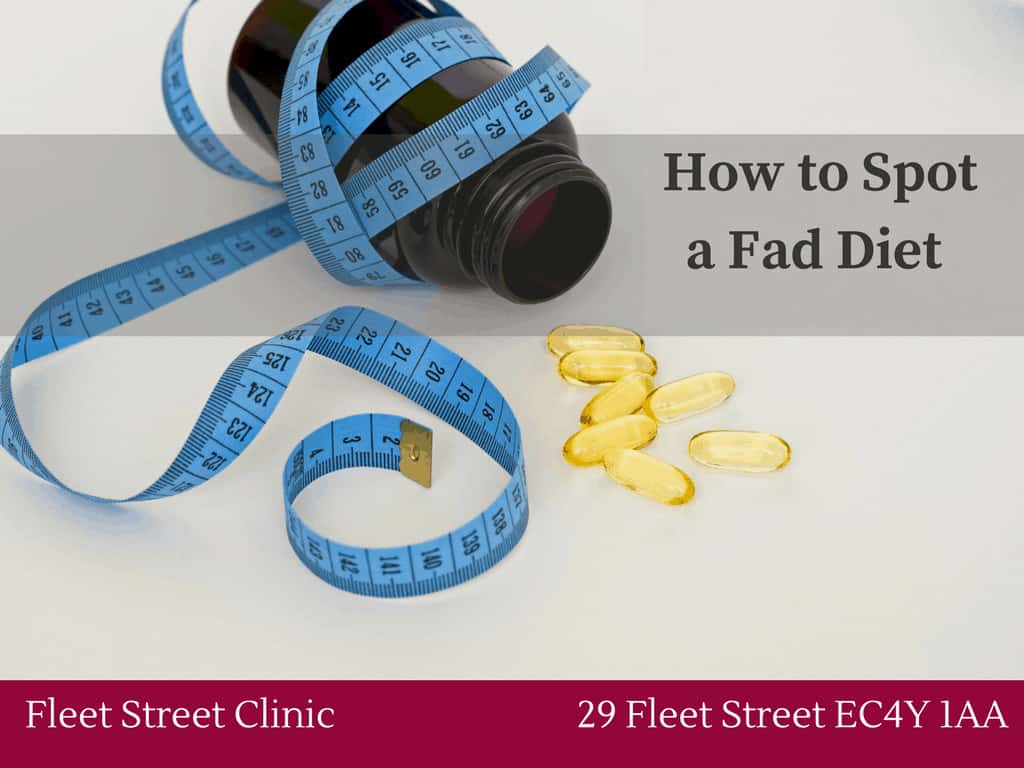
Category: General Health
Many people begin January feeling tired, more than they expected. After a busy December, disrupted sleep routines, richer food, travel, darker days and the pressure of returning to work, it’s normal for energy levels to dip. Most people recover within a week or two once routines settle.
However, persistent or unexplained fatigue is not something to ignore. At Fleet Street Clinic, we see fatigue regularly and for many patients it becomes clear that their tiredness is not simply “post-holiday sluggishness”, but a symptom of an underlying issue that needs attention.
Recognising the difference matters. Fatigue is one of the most common reasons people delay seeking help and one of the symptoms most likely to improve with early assessment.
Understanding what’s normal
Short-term fatigue at the start of the year usually has a clear cause: disrupted sleep, social overstimulation, poor hydration, irregular meals, increased alcohol intake or jet lag. Once life settles, most people notice gradual improvements in energy, concentration and sleep quality.
If your energy steadily improves day by day, this is generally reassuring.
When fatigue becomes a concern
Fatigue becomes medically significant when it persists, is worsening, or begins to affect normal functioning.
People often report:
- Difficulty concentrating or thinking clearly
- Struggling to wake up despite adequate sleep
- Feeling physically weak or drained
- Increased irritability or low mood
- Needing to rest more than usual
- Recurrent minor infections or slower recovery
These are often early signs that something in the body needs attention.
What many patients don’t realise is that fatigue is not a diagnosis, it’s a symptom. And that symptom may point to issues such as thyroid imbalance, iron deficiency, B12 deficiency, diabetes, chronic stress, post-viral changes, sleep disorders or hormone shifts. All of these are manageable, but only when identified.
Why a GP assessment is so important
When a patient comes to us with fatigue, our first step is to understand the full picture. That includes sleep patterns, diet, stress levels, recent infections, travel, menstrual cycles, medication and general health history.
From there, a targeted set of blood tests can reveal the underlying reason for tiredness. Depending on the individual, this can include:
- Iron and ferritin (iron deficiency is extremely common)
- Thyroid function
- Vitamin B12 and folate
- Vitamin D
- HbA1c to assess blood sugar regulation
- Full blood count
- Liver and kidney health markers
- Inflammation markers
Many fatigue related conditions present subtly, especially in the early stages. Blood tests allow us to identify issues before they progress and to create a tailored plan based on your physiology, not guesswork.
Fatigue that is left uninvestigated can gradually affect mood, memory, immunity, productivity and overall wellbeing. For some, fatigue is linked to a treatable deficiency; for others, it’s the first sign of hormonal changes or a developing metabolic issue. In most cases, once we identify the cause, meaningful improvement follows.
What recovery looks like
Treatment depends entirely on the cause. For some, correcting a nutritional deficiency restores energy quickly. For others, small adjustments to sleep timing, stress load, hydration or routine can make a significant difference. In certain cases, we may recommend specialist referrals, monitoring or lifestyle guidance tailored to the individual.
What matters most is that you don’t ignore persistent fatigue or assume it is “just January”. Your body is signalling something and it’s worth listening.
Book your GP Health Review at Fleet Street Clinic here: https://booking.fleetstreetclinic.com/medicals_and_health_screenings
January is a natural reset point for many of us. After the busyness of the festive season, it’s a good time to pause and check in on your health for the year ahead. At Fleet Street Clinic, we often see patients who want to improve their wellbeing but aren’t sure where to begin. An annual health review is an effective, structured way to understand what your body needs and what to prioritise.
Here’s our checklist to help you start the year feeling informed and supported.
1. Blood tests worth considering annually
Routine blood tests can identify changes long before symptoms develop. Depending on your medical history, your GP may recommend:
• Full blood count: Screens for anaemia, infection and several systemic issues
• Thyroid function: Evaluates unexplained fatigue, weight change, temperature sensitivity
• Vitamin D: Commonly low in winter months, affects immunity, energy, bone health
• B12 and folate: Important for energy production and neurological function
• Iron studies: Particularly relevant for women and anyone with fatigue
• HbA1c (diabetes screening): Identifies issues with blood sugar control
• Liver and kidney function: Important for overall metabolic health
Having a baseline each year helps track small changes early and target any underlying causes of fatigue, low mood or hormonal symptoms.
2. Review your cardiovascular health
High blood pressure and cholesterol can develop silently.
Your GP may recommend:
• Blood pressure monitoring
• Cholesterol & lipid panel
• ECG if there are symptoms or cardiovascular risk factors
Heart health should be reviewed annually for adults over 40 or earlier based on family history or symptoms.
3. Mental wellbeing check-in
January can affect mood for many reasons. The days are shorter, disrupted sleep routines and post-holiday pressure. A GP check-in can help identify early signs of:
• Stress overload
• Low mood
• Anxiety or sleep disturbance
• Hormone-related mood changes
Early support is always more effective than waiting until symptoms escalate.
4. Travel health for the year ahead
If you’re planning holidays or work travel this year, now is the time to review:
• Required or recommended vaccines
• Malaria risks
• Travel medications
• Family travel considerations
• Gut health / gastro kits for common travel illnesses
Early planning helps avoid last-minute stress and ensures wider vaccine coverage windows when needed.
5. Women’s and men’s health screens
Depending on age and medical history:
Women may review:
• Cervical screening (if due)
• Breast checks and breast pain concerns
• Hormone testing for fatigue, irregular cycles or perimenopause
• Iron levels
Men may review:
• Prostate symptoms or PSA testing if appropriate
• Testosterone concerns
• Cardiovascular risk factors
6. Immunisation updates
A GP can confirm whether you are up to date with:
• Flu (seasonal)
• Covid-19 boosters
• Tetanus
• HPV (available privately up to age 45)
• Travel vaccinations
Vaccination status is often overlooked but plays a big role in long-term prevention.
7. Build a personalised wellbeing plan
Once you’ve reviewed the essentials, your GP can help you map out a wellbeing plan that includes:
• Sleep support strategies
• Nutrition guidance
• Stress management
• Exercise routines based on your health profile
• Follow-up tests or referrals if needed
A personalised plan turns good intentions into actionable steps.
If you’re unsure where to start or feeling overwhelmed by symptoms, a GP consultation is an excellent first step. Early conversations give you clarity, reassurance and a tailored roadmap rather than waiting until symptoms impact daily life.
Book your GP Health Review at Fleet Street Clinic here: https://fleetstreetclinic.com/services/gp-services/screenings/
HAY FEVER: TIPS AND TEST
Are you one of the many millions in the UK suffering from hay fever at the moment? Learn more about the condition here.
WHAT CAUSES HAY FEVER?
Many allergens are in the air, where they come in contact with your eyes and nose. Airborne allergens include pollen, mould, dust and pet dander.
Other causes of allergies, such as certain foods or bee stings, do not typically affect the eyes the way airborne allergens do. Adverse reactions to certain cosmetics or drugs such as antibiotic eye drops also may cause eye allergies.
Some people actually are allergic to the preservatives in eye drops such as those used to lubricate dry eyes. There are now a wide range of preservative-free brands in unit (single) dose, novel multi-dose bottles and even sprays.
SUMMERTIME EYE ALLERGY TIPS
- Get an early start. See your optometrist before allergy symptoms start this year to learn how to reduce your sensitivity to allergens.
- Try to avoid what’s causing your eye allergies, whenever possible.
- Don’t rub your eyes if they itch! This will release more histamine and make your eye allergy symptoms worse.
- Use plenty of artificial tears to wash airborne allergens from your eyes. Ask your optometrist what they recommend.
- Reduce contact lens wear or switch to daily disposable lenses to reduce the build-up of allergens on your lenses.
- Consider purchasing an air purifier for your home, and purchase an allergen-trapping filter for your furnace.
QUIZ: HAY FEVER EYE ALLERGIES SELF-TEST
Take this quiz to see if you might have eye allergies. Always consult your optometrist / general practitioner if you suspect you have an eye condition needing care.
- Do your eyes often itch, particularly during spring pollen season?
- Are you allergic to certain animals, such as cats?
- Have you ever been diagnosed with “pink eye” (conjunctivitis)?
- Do allergies run in your family?
- Do or have you ever used antihistamines and/or decongestants to control sneezing, coughing and congestion?
- When pollen is in the air, are your eyes less red and itchy when you stay indoors under an air conditioner?
- Do your eyes begin tearing when you wear certain cosmetics or lotions, or when you’re around certain strong perfumes?
If you answered “yes” to most of these questions, then you may have eye allergies.
See here for more information.
Pollen Calendar

For the best course of action or if you have any concerns about the health of your eyes, you can make an appointment online here.
In today’s fast paced world, finding the time to visit a doctor can be challenging. Whether you are juggling a busy work schedule, looking after family, facing mobility issues, or travelling, accessing quality healthcare shouldn’t be difficult. This is where a home visit GP service in London can make all the difference. Fleet Street Clinic offers private GP home visits, ensuring that expert medical care comes directly to you, whenever and wherever you need it.
Why Home Visits Are Essential in London
1. Convenience at Your Doorstep
Navigating London’s traffic and packed public transport can make a short trip to the doctor extremely stressful. A GP home visit removes travel time, allowing you to receive expert medical care in the comfort of your home, office, or hotel.
2. Same-Day Appointments for Immediate Care
Waiting for a GP appointment at a busy surgery can take days, if not weeks. Often, NHS appointments require a registration process that can take several days. With same-day GP home visits in London, Fleet Street Clinic ensures you receive prompt medical attention when you need it most.
3. Personalised and Unhurried Care
Unlike traditional 15- or 30-minute clinic visits that may feel rushed, a private GP home visit allows for a more in-depth consultation. Your doctor can assess your condition in a familiar environment and provide tailored treatment plans suited to your lifestyle.
4. Ideal for Families, Elderly Patients, Busy Professionals, and Travellers
- Parents with young children can avoid exposing them to germs in waiting rooms.
- Elderly patients or those with mobility issues benefit from receiving care without the challenge of travelling.
- Professionals with demanding schedules can fit a GP consultation into their day without taking time off work.
- People travelling into London may need urgent medical attention before flights back home; home visits can also take place in hotels, airbnbs, or any other third party location.
5. Comprehensive Medical Services at Home
Fleet Street Clinic’s private doctor home visits cover a wide range of medical services, including:
- Diagnosis and treatment of illnesses. Prescriptions and medication advice.
- Vaccinations, including flu and travel vaccines. Health check-ups and screenings.
- Chronic disease management.
- Medical certificates and sick notes.
- Wide range of services including blood tests, urine samples, swabs, and more.
Book a GP Home Visit in London Today
If you need a home visit GP in London, Fleet Street Clinic is here to help. We provide professional, same-day medical care wherever you are, ensuring your health remains a priority without the hassle of travel.
Call us now at +44 207 353 5678 to book your appointment or schedule a home visit directly on our website. Take control of your health with the convenience of private GP home visits in London.
The summer holidays will fly by and be over as quickly as they began, much to your relief, but probably the disappointment of your kids! Unfortunately, alongside the general back to school chaos, September also brings with it the start of the flu season.
Flu season not only means that people have to take time off of work due to being ill themselves, but parents often have to take time off work to look after their children who have the flu, because schools are rife with superspreaders. It seems that the best solution to the frustrating effects of the flu on school and parenting life is to nip it in the bud early enough in the season for immunity to make a significant difference.
This is where the flu vaccine comes in.
The flu vaccine comes in two forms, the traditional syringe-administered jab, and a nasal spray vaccine. While the nasal spray vaccine may be the preferred administration tactic for parents of children who don’t like needles, supply issues have resulted in limited availability, and it may still be worth considering the alternative.
When might the jab be preferable?
The nasal spray vaccine is protective and an excellent choice, but is not suitable for everyone. It is a live vaccine, and so cannot be administered to children who are immunocompromised or who live with anyone who may be immunocompromised. It is also unsuitable for anyone with bad asthma, since it may trigger an attack. The injected vaccine is not a live vaccine and is an obvious solution for a lot of people.
The nasal spray vaccine contains traces of gelatine and egg, and so may be unsuitable for vegetarians, vegans, Muslims or those with a severe egg allergy. There is a cell-culture based injectable vaccine that is egg-free, which may be a more acceptable alternative.
The nasal spray vaccine can only be given from age two onwards. However, if there is a special reason for needing to vaccinate your child at a younger age than this, the standard injectable vaccine can be given from the age of 6 months. (The best way to protect babies younger than this is by vaccinating mums during pregnancy.)
For the past three winters, the nasal spray vaccine has been in limited supply. It has not been available privately but only through the NHS, and supply issues have resulted in extended delays. By contrast, injected vaccines have been available reliably from September onwards.
A well-timed dose of the injected vaccine, early in the season, may be a better option than the uncertainty of a delayed dose.
At the Fleet Street Clinic, we have been happy to offer the nasal spray vaccine previously but having been unable to obtain reliable supplies for the past three years, we will not be offering it this season.
If you decide to book the injected flu vaccine for your child this winter, you can rely on guaranteed supplies as well as our expertise in vaccinating babies and children of all ages.
__________________________
24/25 Winter Flu Vaccination Pricing:
Cell-Based Quadrivalent Flu Jab – £42 – Suitable from 2 years
Standard Quadrivalent Flu Jab – £20 (while stocks last) – Suitable from 6 months old
Book Your Flu Jab Online Today
Respiratory Syncytial Virus (RSV) is a common and highly contagious virus that primarily affects the respiratory tract, causing significant illness, particularly in infants.
It is present year-round but peaks during the winter months, and spreads through droplets from coughs and sneezes or via contact with contaminated surfaces. RSV is a virus, so antibiotics are not an effective treatment.
Each year, RSV poses a substantial health risk to infants and older adults worldwide.
In the UK, RSV accounts for approximately 33,500 hospitalisations annually in children aged 5 and under, resulting in 20 to 30 deaths per year. 75-80% of hospitalisations due to RSV happened during the first 6 months of life.
Is there a suitable RSV vaccine for pregnant woman?
Abrysvo is a recombinant vaccine for the prevention of severe lower respiratory tract disease caused by RSV in infants up to six months old. It is the only maternal RSV immunisation given to the pregnant woman between 28 – 36 weeks of pregnancy to help protect newborns. It can also be used for older adults over the age of 60 years, in preventing RSV that can lead to breathing difficulties and pneumonia.
Maternal vaccination involves administering vaccines to pregnant women to protect their newborns through the transfer of antibodies. This approach has been effectively used for diseases like whooping cough.
Vaccinating pregnant women against RSV provides passive immunity to their babies, safeguarding them against RSV until they can receive their own vaccines. The RSV vaccine should ideally be given at least 2 weeks apart from the whooping cough vaccine.
In the UK, the Joint Committee on Vaccination and Immunisation (JCVI) has assessed the impact of RSV and now recommends vaccination to protect vulnerable groups, including infants and older adults with the aim of reducing the incidence of RSV-related illnesses among infants, ultimately reducing RSV-related morbidity.
At Fleet Street Clinic, we can offer private RSV vaccination to protect you and your baby, ahead of the NHS roll out.
Abrysvo is an inactivated vaccine and only requires a single dose for protection.
Price: £296
Please contact our reception team to book by phone, +44 20 7353 5678 or by emailing info@fleetstreetclinic.com
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
I picked up Covid early in the pandemic and put my newly acquired immunity to good use by joining the Covid medical team at my local hospital for the weeks that followed. There was a side-effect however: a sense of invincibility that has perhaps made me take less care to protect myself from respiratory viruses ever since.
My luck ran out recently while looking after a group of patients with upper respiratory infections. Not all respiratory viruses are equal: we may call them “colds”, but some varieties are considerably more unpleasant than others.
Using PCR, we can now tell the difference between 22 different bugs with pinpoint accuracy, in about an hour. Mine turned out to be parainfluenza type 1 (there are four serotypes, who knew?) – a nasty virus, more common in the USA and among children.
My bout ranked alongside my experience with Covid: the symptoms lasted over three weeks and included a secondary lower respiratory infection requiring antibiotics to clear.
There’s no vaccine as yet against parainfluenza, but there are vaccines against other important respiratory infections – pneumococcal pneumonia, RSV, Covid-19, a newly-recommended adult top-up against whooping cough, and of course flu.
I shall be having all of these vaccines this winter and will take much greater care to protect myself when those around me have “colds”.
Trusted London clinic now offers private Covid-19 vaccines.
As a trusted name in healthcare for the past three decades, Fleet St. Clinic are proud to announce the expansion of our services to include private Covid-19 vaccination for individuals and businesses alike. We offer the most up-to-date Pfizer Covid vaccines at a cost of £115 per dose.
Covid Vaccinations for Individuals
Until now, Covid vaccination has only been available through the NHS, which has rightly prioritised access those most likely to suffer complications. However, coronavirus infection remains a hazard for everyone, and many other people also wish to be protected. Protection can be especially important for people keen to avoid illness abroad, for people in key occupations, and for those in close contact with vulnerable friends and relatives.
Covid vaccination will now be available year-round for all those who would like to be protected, including those who have not been eligible for NHS care. Whether you need a booster vaccination or would like to consider having the Covid vaccine for the first time, we can help.
Book your private covid vaccination here.
Covid Vaccinations for Businesses
Fleet St. Clinic has provided large-scale flu vaccination initiatives for businesses across the United Kingdom since 1995. These programmes are now being expanded to include long-awaited vaccination against Covid-19. Many of our clients have been keen to protect those in business-critical roles as well as to protect employee health and wellbeing more generally.
Workplace vaccination programmes are offered as a straightforward and fully-managed service, enabling employees to access vaccinations they might otherwise find challenging to obtain. Introducing vaccination against Covid-19 reflects our longstanding commitment to keeping companies and their employees healthy.
Book your private covid vaccination workplace programme here.
Fleet St. Clinic Medical Director, Dr Richard Dawood commented:
“We are delighted to be one of the first medical practices in the UK to offer Covid-19 vaccinations outside the NHS. Now that Covid has transitioned from being a pandemic to an endemic disease, it is important that vaccination against Covid should become as “normal” and accessible as vaccination against other infectious diseases.
As a private, multi-disciplinary medical practice, the Fleet St. Clinic has specialised in vaccines for three decades, delivering hundreds of thousands of doses. Through the pandemic, most of our doctors and nurses volunteered to deliver Covid-19 vaccines in the NHS. We are especially pleased that being vaccinated against Covid-19 can now be a matter of choice for individuals and businesses alike, no longer restricted to those in the most vulnerable groups.”
Pre-Book Your Covid Vaccine
Covid vaccination will become available in March, but you can pre-book your own Covid vaccine or a Workplace vaccination programme, from today. Fill in our online form and we will be in touch with more information.
Pre-book your private covid vaccination programme here.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Full Respiratory Panel PCR Test
There has been a huge rise in measles cases already this year inciting a national campaign to ensure that children and adults are adequately vaccinated against measles.
Measles is a highly contagious virus that can cause serious illness. Complications of the disease include pneumonia and meningitis. In some cases, the virus can be fatal.
The MMR vaccine is a highly safe and effective vaccine that not only offers protection against measles but also against mumps and rubella, as a 3-in-1 vaccine.
In the UK, the uptake of the MMR vaccination has declined significantly, resulting in an increase in measles infection. It is estimated that 3.4 million children under the age of 16 years remain unprotected against the disease.
The UK is not alone with rising cases of measles. The World Health Organization has reported a 30-fold increase of measles in Europe. Over 30,000 measles cases were reported by 40 of the Region’s 53 Member States between January and October 2023. Compared to 941 cases reported in all of 2022.
The MMR vaccination forms part of the national childhood schedule where the vaccinations are given at one year of age and then at 3 years of age.
Two doses of the vaccination provide over 99% protection against illness.
ADVICE
Although measles is a highly contagious illness, it can be easily prevented with vaccination.
MMR VACCINATION:
For full protection, ensure your child has received their routine childhood immunisations of 2 doses of the MMR vaccine.
Children at high risk of measles exposure can receive an accelerated vaccine schedule of MMR if they are high risk for contracting the disease, where two doses are given one month apart.
Infants at high risk contracting the disease can receive the MMR from as early as 9 months of age.
In some cases, a catch-up vaccination may be recommended for individuals who have not received the vaccine at the recommended ages.
Additionally, in certain situations, infants may receive an early dose of MMR, such as during outbreaks or if they will be traveling to areas where there is an increased risk of exposure.
Travellers who are visiting countries reporting outbreaks of measles should ensure that their routine immunisations against MMR have been completed. A simple blood test can confirm immunity if in doubt.
HOW MANY VACCINES ARE NEEDED?
Two doses of the MMR vaccine will provide lifetime immunity.
In the UK, these are normally given to a child around their first birthday. The second is normally given at around the age of three. If there is a risk of an outbreak or an infant is at higher risk to contract the disease, vaccines are sometimes given as early as 9 months of age.
You can easily book an MMR vaccine appointment online.
SHOULD I BE WORRIED?
Adults are also encouraged to check their own and their children’s vaccination status. This is especially important for those who are considered vulnerable or those travelling to countries that have reported outbreaks of measles.
In the first instance, you should call your GP for confirmation of your vaccination history. If you didn’t have the MMR vaccine or your course is incomplete, you can book your MMR catch up vaccinations online.
Alternatively, if you are unable to find your records, a simple blood test will be able to confirm if you are immune or not. If you were born before 1970, it is assumed you will be immune through natural infection with the disease.
DO YOU HAVE ANY ADVICE FOR PARENTS?
Yes, we wrote a separate blog for parents who are worried about measles. We cover symptoms of measles, what to do if you suspect your child has measles, what to do if your child has been exposed to measles, amongst other important information.
The take home message being that the risk to you child dramatically reduces if they have had the full course of the MMR vaccine. If they are part-way through the course or have missing vaccinations, we encourage you to consider catch up vaccinations for full protection and peace of mind.
Read our full blog on what to do if you think your child has measles and when you should keep them off school.
CAN ADULTS RECEIVE THE VACCINE?
Yes, it is perfectly safe to have catch up vaccinations if they are required.
If you are unsure of your vaccination status, we would recommend a blood test to check your antibody level first. If we discover that you are not immune, you will require two vaccine doses, given a month apart.
WERE THERE ANY WARNING SIGNS OF AN OUTBREAK?
In July last year, the UK Health Security Agency (UKHSA) issued a warning that, unless vaccination rates improve, London is at risk of a major measles outbreak. Even after that, the vaccination rates did not improve.
It is predicted that in some areas of the capital, up to forty per cent of children are not protected from measles by the time they start school. Young adults between the ages of nineteen and twenty-five are also particularly vulnerable. Referred to as the ‘Wakefield cohorts’ by UKHSA, this generation were exposed to misinformation published in the early 2000s and as a result, many were left unvaccinated.
In a bid to mitigate risk, councils wrote to households across the capital explaining the possibility of isolation requirements; Children who are identified as close contacts of a measles case, and who do not have an up-to-date vaccination record, may be required to self-isolate for up to twenty-one days. The NHS are therefore urging parents to check their children’s’ vaccination status. Records of their vaccines should be kept at their GP practice, or in their red book.
Book your MMR vaccination appointment today.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
CONTINUED READING ABOUT THE UK HEALTH SECURITY AGENCY (UKHSA) “ISOLATION WARNING FOR LONDON CHILDREN WITHOUT MEASLES JAB”
Read: Isolation warning for London children without measles jab
CONTINUED READING ABOUT THE LATEST MEASLES STATISTICS AND GUIDELINES (UKHSA) “LATEST MEASLES STATISTICS PUBLISHED” & “NATIONAL MEASLES GUIDELINES”
Read: Latest Measles Statistics Published
Read: National Measles Guidelines
What to do if you think your child has measles and when to keep them off school.
Measles cases are increasing throughout England, particularly among children. This highly contagious infection can lead to severe complications for some individuals.
Since there is no specific medical treatment for measles, obtaining vaccination is crucial for the best defence against serious illness. The measles, mumps, and rubella (MMR) vaccine is part of routine childhood vaccinations, meaning most children are already immunised against measles.
If your child has received both doses of the vaccine, it is unlikely that they will contract the virus.
Here, we’ll provide everything you need to know about measles, from ensuring your child’s vaccination to knowing when to keep them away from school.
What are the symptoms of measles?
Measles usually starts with cold-like symptoms, followed by a rash a few days later. Some people may also get small spots in their mouth.
Symptoms of measles usually start to appear 7-14 days after you become infected, which include:
- Runny/blocked nose
- Sneezing
- High temperature
- Sore, red eyes that may be sensitive to light
- Sore throat
- White spots inside the mouth
What does a measles rash look like?
Measles usually begins as flat red spots that appear on the face at the hairline and spread downward to the neck, body, arms, legs, and feet. Small, raised bumps may also appear on top of the flat red spots. The spots may become joined together as they spread from the head to the rest of the body.
What should you do if you think your child has measles?
If you suspect that you or your child might have measles, it’s important to request an immediate GP appointment or seek assistance from NHS 111.
Before visiting the GP or any healthcare facility, make sure to call ahead for guidance.
In the event of a measles diagnosis for your child by a doctor, it is advisable for them to refrain from attending nursery or school for a minimum of 4 days from the onset of the rash. Additionally, they should steer clear of close interactions with infants and individuals who are pregnant or have compromised immune systems.
What is the best way to protect against measles?
The best protection against measles for children and adults is to get both doses of the MMR vaccine.
MMR vaccination is available at Fleet Street Clinic for children and adults who would like catch-up on doses. If you or your child haven’t been vaccinated yet, or have an unfinished course of vaccines, either book an appointment online or contact our reception team on +44 20 7353 5678 to book an appointment.
We can usually accommodate same day appointments.
Alternatively, children receive the vaccine at no cost on the NHS at 12 months and then a second dose at 3 years and 4 months. You may find the NHS vaccination service has a longer wait time that us.
If you prefer a version of the MMR vaccine without pork products, please get in touch, explaining your preference and we will do our best to accommodate. It’s important to note that we would be ordering this product specially for you, so there may be a longer wait time for delivery and prepayment will be required. Either call our reception team on +44 20 7353 5678 or email info@fleetstreetclinic.com
Cold-like symptoms can be an early sign of measles. Should you still send your child to school?
If your child has been vaccinated, it’s very unlikely that they have measles. Check if they have a high temperature or a fever, and if not, we’d advise it’s fine to send your child to school.
Keep an eye on their symptoms and adapt accordingly if they worsen.
When should you keep your child off school or nursery and how long for?
If your child has measles, they should stay off nursery or school for at least 4 days from when the rash first appears and avoid close contact with babies and anyone who is pregnant or has a weakened immune system.
The school will let you know if your child has been in contact with someone who has measles and advise what you need to do.
They may advise people who are more susceptible to contracting the virus, such as unvaccinated siblings to stay away from school for the incubation period to be on the safe side.
The incubation period is the length of time it can take to develop the illness after being in contact with someone with measles. For measles, the incubation period can be up to 21 days.
Anyone, child or adult, who has been vaccinated is unlikely to be considered susceptible.
If you’re not sure whether your child is due a vaccination or has missed a vaccination, you can check their Red Book or contact your registered GP practice for confirmation.
If your child has missed their first or second dose of the MMR vaccine, we’d advise you book an appointment for catch up vaccines. You can book an appointment online.
Should you keep your child off school if another pupil has been diagnosed with measles?
Most children will be protected against measles and there is no need to keep your child off school if they have had both their MMR vaccinations.
Your school will let you know if your child has been in contact with someone with confirmed measles and will advise what the next steps are.
Can I still get my child vaccinated even if they’re older?
Yes. The MMR vaccine is suitable for adults and children, therefore, anyone who has not had 2 doses of the MMR vaccine can book an appointment for catch up vaccinations.
It’s best to have vaccines on time, but you can still catch up on most vaccines if you miss them. Two doses of the vaccine are needed to ensure full protection.
RELATED SERVICES AVAILABLE AT FLEET ST. CLINIC
Related Blogs:
Measles outbreak & isolation warning
Blue Monday happens every year on the third Monday of January. It is supposedly the most depressing day of the entire year, based on a crude calculation of bad weather, long nights, back to work dread and post-Christmas debt.
It does sound very plausible perhaps because we so familiar with the term “January Blues” but Blue Monday is in fact, a myth!
The phrase “Blue Monday” was coined by Sky Travel back in 2005 as a way to encourage people to book their next holiday as something to look forward too. They highlighted all the seasonal negatives to reinforce the benefits of booking a holiday – a clever marketing trick.
But can we really pinpoint the most depressing day of the year?
There is no actual scientific studies that have ever backed up any claims about Blue Monday being true or that there could even be a “most depressing day of the year”. This does make sense because this would be different for each and every one of us based on personal circumstances and the variables are extensive. It did, however, get use thinking about our mood, mental health and overall wellbeing at this time of year.
January is cold, often wet and everyone is trying to shake off the Christmas comedown and get excited about the new year ahead, but the January blues can creep in.
Remember you are not alone, and many people experience a dip in mood this time of year but it is important to identify when the January blues are actually symptoms of depression.
Depression is more than simply feeling unhappy, fed up or low for a few days. It can be long lasting and the symptoms range from mild to severe. Once accessed by a doctor, they will conclude the severity of your depression.
A simplified description follows:
Mild depression will have some impact on your daily life.
Moderate depression has a significant impact on your life.
Severe depression makes it almost impossible to get through daily life.
Sometimes there’s a trigger for depression. Life-changing events, such as bereavement, losing your job or giving birth, can bring it on. Other times, it can be linked with family history; people with family members who have depression are more likely to experience it themselves. But you can also become depressed for no obvious reason. It is quite complex and each person is unique.
There are many symptoms of depression and the combination is unpredictable.
They can be categorised at physiological, physical and social symptoms.
Some examples of psychological symptoms of depression include:
- continuous low mood or sadness
- feeling hopeless and helpless
- having low self-esteem
- feeling tearful
- feeling irritable and intolerant of others
- having no motivation or interest in things
- finding it difficult to make decisions
- not getting any enjoyment out of life
- feeling anxious or worried
- having suicidal thoughts or thoughts of harming yourself
Some examples of physical symptoms of depression include:
- moving or speaking slower than usual
- changes in appetite or weight (usually decreased, but sometimes increased)
- constipation
- unexplained aches and pains
- lack of energy
- low sex drive
- changes to your menstrual cycle
- disturbed sleep – for example, finding it difficult to fall asleep at night or waking up very early in the morning
Some examples of social symptoms of depression include:
- avoiding contact with friends and taking part in fewer social activities
- neglecting your hobbies and interests
- having difficulties in your home, work or family life
The most common symptoms of depression tend to be a low mood, feelings of hopelessness, low self-esteem, lack of energy, problems with sleep and a loss of interest in things you used to enjoy but it can be any number of symptoms listed above.
It’s important to seek help from a GP if you think you may be depressed. The sooner you see a doctor, the sooner you can be on the way to recovery.
For more information on GP services at Fleet Street Clinic, click here.
With every change of season comes a host of different medical issues, and winter can be one of the worst. With colder temperatures, shorter days, and seasonal illnesses circulating, it is one of the harder seasons to keep fit and healthy. There are certain conditions which are known to worsen in the colder months and so it is important to be aware of them and how you can best prepare yourself to keep healthy throughout winter.
These conditions include:
- Asthma
- COPD
- Circulatory disorders, such as claudication, Raynaud’s disease, and chilblains
- Ischaemic heart disease
- Hypothyroidism (if untreated)
- Osteoarthritis and any joint disorder to include rheumatoid arthritis
- Seasonal Affective disorder
- Allergic rhinitis
To reduce the increased risk associated with the above conditions, it is important to have a check up with your GP, ideally in the early Autumn before the Winter months. This will give you the best chance of getting ahead and allowing you to prepare for the coming season. But, if for whatever reason, you were unable to have a check up in Autumn, it is still beneficial to have a check up during the Winter months.
During a check up for asthma and COPD it’s advised to have a peak flow and lung function check. Asthma and COPD are worse in the dry, cold weather, so it is important to make sure you have plenty of your prescribed inhalers. It is best to be prepared rather than be taken unawares by an attack of wheezing. It is extremely important to see a doctor if you develop winter wheezing and are short of breath, especially during the night as this is when asthma and COPD attacks are most dangerous.
Circulatory disorders are worse in the cold weather as lower temperatures constrict blood vessels, increasing the likelihood of pain due to claudication (pain in the calves after walking a certain distance), Reynaud’s (discolouration of the fingertips due to constriction of the blood vessels) and chilblains (small, itchy, red patches on the skin). You can prepare for all of these conditions by obtaining prescriptions for treatment but most importantly, by keeping warm and preparing for the cold.
Ischaemic heart disease is also worse in the cold weather due to the effect of constricting blood vessels. It is important to have a cardiac check to include blood pressure, and if you suffer from angina, to ensure you have the medication to treat this painful condition which is likely to be much worse in the cold weather. Avoiding the extreme cold and wearing thermal clothing may also mitigate against the likelihood of a heart attack or myocardial infarction if you do suffer from Ischaemic heart disease.
If you suffer from Hypothyroidism, it is a good idea to have an annual blood test. Left untreated, hypothyroidism can cause increased sensitivity to cold, which can be particularly unpleasant in winter.
For those with arthritis of any kind, the best way to avoid pain and stiffness in the joints is to keep warm and keep the joints moving. Find more information on Arthritis in Winter here.
If your mood tends to be lower in the winter months, each year, you should have a check up with your GP to discuss Seasonal Affective Disorder (SAD). If you are diagnosed with SAD, consider CBT (Cognitive Behavioural Therapy) rather than medication if you can, and invest in a daylight lamp as these do help.
Allergic rhinitis is another ailment that tends to crop up a lot around winter time. This is diagnosed when you have a persistent nasal discharge. This can occur either as a result of pine or autumnal tree leaf mould, or due to house dust or mould which is often exacerbated by central heating. In this instance, nasal sprays and antihistamines are often required.
Finally, the Norovirus peaks in November until April. This is a really unpleasant vomiting virus which is picked up from contaminated surfaces or foods. To help avoid this nasty bug, always wash hands when handling food and make sure food is washed thoroughly before cooking or eating raw.
If you know or suspect that you might suffer from any of these conditions, please do visit your GP to help you keep prepared. Similarly, if anything new arises you should see your GP as soon as you can; the earlier a health condition is addressed, the easier it is to treat.
In general, an annual medical is a good way to give you a full-body overview of your health, as well as monitor the progression of any existing health conditions. A varied, balanced diet and regular exercise will also be crucial in keeping you generally fit and healthy throughout winter.
For more information on our GP Services.
Book a GP Appointment or an Annual Medical.
Arthritis is a common condition that causes pain and inflammation in joints. It is not a single disease but an informal way of referring to joint pain or joint disease. There are more than 100 types of arthritis and related conditions. There are thought to be 10 million people with some form of arthritis in the UK. It is the most common cause of disability in the UK and can affect people of all ages but it does occur more frequently as people get older.
Common arthritis joint symptoms include swelling, pain, stiffness and decreased range of motion. Symptoms can range dramatically from person to person, with some experiencing mild symptoms with occasional flare ups to those who experience constant debilitating pain everyday. The sad truth is that there is no cure for arthritis, so it is all about pain management and how to best reduce flare ups.
The impact of the weather on the symptoms of arthritis has been debated for many years and people tend to report more arthritis flare-ups in the winter, but the reason why is not specifically known.
Quite often sufferers will state that their symptoms get worse when the weather is damp and cold and some state they are able to tell when the weather is about to change based on their arteritis symptoms worsening.
Even if there is currently nothing to support this scientifically, this doesn’t remove the pain felt by sufferers and so rather than comment on where this is true or not, let’s look at ways to reduce flare ups in winter.
Our top 4 tips:
1. Stay warm
When the temperature drops both inside and outside, dress warmly. Make sure all arthritis prone areas are kept warm.
2. Stay hydrated
Drink plenty of water throughout the day. Even mild dehydration might make you more sensitive to pain.
3. Take warm baths
A warm bath or visiting a heated swimming pool will ease joint pain and comfort you. If you visit a heated swimming pool, gentle exercise will also help your mobility.
4. Stay active
It is now clear that active people experience less joint pain than those who are sedentary. If you are experiencing an arthritic flare then reduce your usual activity (but don’t stop altogether) and use simple anti-inflammatory medication such as ibuprofen if it is safe for you to do so.
Enjoy winter while taking the above precautions for Arthritis.
If you are facing extreme discomfort and pain in your joints due to arthritis, book an appointment with a GP to discuss your options.
In September 2021, Public Health England released new rules surrounding the timing of BCG vaccination, increasing the minimum age of vaccination to 28 days. This has been implemented in line with a pilot disease screening programme that tests eligible newborns for Severe Combined Immunodeficiency (SCID), the outcome of which becomes available by the time the baby is 6 weeks old. It is important that we wait for the result of this test before giving the BCG vaccine.
What is SCID screening?
All newborn babies in the UK are currently offered blood spot screening (heel prick test) that looks for 9 rare diseases, including sickle cell and cystic fibrosis. The NHS is considering introducing an additional test for Severe Immunodeficiency (SCID), a name given to a group of rare, inherited disorders that cause major abnormalities in the immune system. Affected infants have an increased risk of life-threatening infections and will normally become severely unwell in the first few months of life. Without treatment they will rarely live past their first birthday. About 14 babies a year are born in England with SCID.
The evaluation of this testing, which began on 6th September 2021, is taking place in 6 areas across England and will cover around 60% of new born babies. It is running alongside the existing blood spot screening and the intention is to roll it out nationally once the 2 year evaluation has been made.
Why does this affect the BCG vaccination?
Bacillus Calmette-Guérin (BCG) is a live attenuated vaccine that can cause problems if given to an immunocompromised person. Treatment for SCID is more complicated if the child has received the BCG vaccine, so it is important that if your child has been tested. We wait for a negative result before vaccinating.
What we need from you:
If your child was included in the SCID programme, you will need to provide a letter that confirms the negative result of screening.
If your child was born outside of the programme areas and therefore, not included in the SCID programme, we will need to see a letter confirming this.
In either case, please bring the letter with you to your appointment, as well as your child’s vaccination book.
Nb. If your child was born before 1st September 2021, before the programme was introduced, no letter will be needed.
For more information on:
Other Childhood Vaccinations
RSV is a common and highly contagious respiratory virus that is a leading cause of lung disease. RSV is seasonal, and like other respiratory viruses, its peak incidence is during the winter months each year. It spreads from person to person via droplets, or from infected surfaces or objects. RSV is a virus, so antibiotics are not effective.
Arexvy is a new vaccination designed to protect against lower respiratory tract disease caused by respiratory syncytial virus (RSV). It is an important advance, because no specific treatment for RSV is available, and infection is often severe.
Older adults, and those with underlying medical conditions such as diabetes, heart disease and lung diseases such as asthma and COPD are at the greatest risk of the infection. RSV can exacerbate these underlying conditions and lead to pneumonia.
In the UK, RSV causes more hospitalisations and deaths than flu in those over the age of 60. It is estimated that RSV causes14,000 hospitalisations and an estimated 8,000 deaths in adults 60 years of age and older each year.
Arexvy is a recombinant adjuvanted vaccine for the prevention of RSV is adults 60 years of age and above. It is the only licensed vaccination in the UK that has been authorised for use by the Medicines and Healthcare products Regulatory Agency, meaning at risk adults are now able to be vaccinated against the disease.
Arexvy is as in inactive vaccination and only requires single dose for protection. It can be administered at the same time as other vaccinations including flu, pneumococcal, and COVID.
We are among the first practices in the UK to offer it to adults needing protection.
If you have a heart condition you have a greater risk of becoming more seriously ill from flu (seasonal influenza) than the general population. In addition, having the flu can exacerbate pre-existing conditions like diabetes or asthma.
According to the NHS, “every year over 11,000 people in England die from complications caused by the flu virus. Many of these deaths could have been prevented by having the flu vaccination.”
Preventing the flu in the first place is the best option.
The best protection is to have a Flu Vaccine each winter.
What is the flu?
Many people think having influenza, also known as the flu, is like having a bad cold, but in reality flu is a nasty respiratory virus that can make you very unwell. Influenza causes inflammation in the body and can be very serious – sometimes leading to hospitalisation or even death.
There is evidence that heart attacks happen more often during or immediately after an acute inflammatory illness, such as flu.
A flu jab is the best protection against flu.
In general, the flu causes stress and inflammation on the body, increasing blood pressure, heart rate and heart function. This is not good for someone with heart or circulatory problems.
Flu vaccination is strongly recommended for anyone who has ever had a heart attack, stroke or has underlying heart disease. A previous diagnosis of heart or circulatory diseases is considered a high risk factor for complications or even another heart attack, for anyone who becomes ill with flu.
Does flu affect heart medication?
If you take warfarin, flu symptoms can affect your blood clotting rate (INR). You should speak to your doctor if this happens so they can monitor your situation closely. It does also mean if you do become unwell, it may take you longer to recover than the average person.
In addition, some over-the-counter flu medicines can’t be used when taking medicines for heart conditions, so contact your doctor before taking things like painkillers and cough medicines. It is better to check before beginning any new medications.
When is the best time to get the flu jab?
Flu vaccinations become available from mid to late September, and through the season until February. It’s best to get your flu vaccine in September or October. The peak time for catching flu runs from Christmas to Easter. The aim is to be vaccinated before flu transmission starts, and to allow at least a couple of weeks post-vaccination, for maximum immunity to develop. The sooner you have the vaccination, the sooner you will be protected.
You can book your flu jab online.
We have a range of flu vaccinations available, including the premium recombinant vaccine, cell-based vaccine, FluAd (for those aged 65 year and older), kids nasal spray and the standard flu jab.
It is important to have a flu jab every year because the flu virus can change. There are many strains of flu already and some are more dominant than others. Each year strains are analysed to determine which strains are likely to be the prevalent strains circulating that year. They can vary year to year so relying on a past vaccination for protection is risky. The previous year’s vaccine may not offer you the right protection against the strains in circulation this year.
In addition, immunity to flu decreases over time. Exposure to the flu virus strengthens the immune response and offers natural protection. With less flu circulating over the past few years due to covid restriction measures, natural immunity in the general population will have decreased.
A flu vaccine will boost immunity.
With most workers now returned to the office and social distancing restrictions long gone, there is a greater chance of the flu spreading and more people falling ill this winter. With both illnesses circulating around it is highly recommended to reduce the risk by getting the flu jab.
Protect yourself against the flu.
You can find more information on the types of flu vaccines available.
For more information on the premium recombinant flu jab.
_____________
Wanting to book a Workplace Flu Vaccination Programme?
Flujabs.org is part of Fleet Street Clinic and has been providing workplace flu vaccinations to UK businesses for many years.
Fill out the online form and one of our flu coordinators will get back to you with current availability and costs.
STUDENTS URGED TO GET VACCINATED BEFORE UNIVERSITY
The UK Health Security Agency (UKHSA), formerly known as Public Health England, is encouraging students to get vaccinated before they start/ return to University to protect themselves against a range of life-threatening illnesses.
Starting university and attending Fresher’s Week exposes students to a host of viruses and bacteria – some of which for the first time.
First year or returning students can be at increased risk of serious diseases such as meningitis, septicaemia and measles as they mix with large numbers of other students from around the country and overseas.
We strongly advise the following 3 vaccinations at a minimum for students:
Meningococcal ACWY (MenACWY)
– Protects against 4 common strains causing meningitis and septicaemia
Measles, Mumps and Rubella (MMR)
– Protects against measles, mumps, rubella
Human Papillomavirus (HPV)
– Protects against HPV-related cancers including cervical, penile & throat cancers, alongside protection against genital warts. HPV vaccination is estimated to prevent up to 90% of HPV-related cancers.
Meningitis Vaccinations:
– Meningococcal ACWY (MenACWY)
– Meningococcal B (MenB)
UKHSA vaccine coverage data shows around 1 in 8 new students going to college and university this year remain unprotected against these 4 strains of meningococcal bacteria, each of which can cause long term disability, serious health complications and can be life threatening.
The MenACWY vaccine is given by a single injection into the upper arm and protects against four different strains of the meningococcal bacteria that cause meningitis and blood poisoning (septicaemia): A, C, W, and Y. You can book online.
The MenB vaccine is also given as an injection to the upper arm but is a 2-dose course for full protection. It protects agains the B-strain of the meningococcal bacteria. You can book online.
Cases of meningitis, particularly virulent strain Men W & Men B, have been rapidly rising amongst students since 2009.
What is Meningitis W?
Meningitis is a bacterial infection of the protective membranes surrounding the brain and spinal cord. Meningococcal meningitis (Men W) is a highly serious form of bacterial meningitis that can lead to septicaemia. It is spread by droplets that come from a person who is infected with the bacteria.
Although the strain is most likely to affect babies, statistics reveal that older children, teenagers, and adults are also at risk. In recent times, cases amongst normally healthy teenagers have spiked and the fatality percentage is higher with Meningitis W than it is with the most common strains, Meningitis B and C.
Meningitis can progress quickly leading to blood poisoning (sepsis), which can kill within 24 hours. So, it is important to know the signs and symptoms of meningitis and septicaemia (sepsis).
Early symptoms of Meningitis include:
- headache
- a high temperature (fever)
- being sick (vomiting)
- a rash that does not fade when a glass is rolled over it (but a rash will not always develop)
- a stiff neck
- a dislike of bright lights
- cold feet and hands
- or muscular pain
Sepsis is a life-threatening reaction to an infection. It happens when your immune system overreacts to an infection and starts to damage your body’s own tissues and organs. Symptoms can be vague but include:
- acting confused, slurred speech or not making sense
- blue, pale or blotchy skin, lips or tongue
- a rash that does not fade when you roll a glass over it, the same as meningitis
- difficulty breathing, breathlessness or breathing very fast
Many people confuse the symptoms with just a hangover or freshers’ flu, which is one of the theories as to why students are so high-risk. So, check-in on your friends who are unwell. Symptoms can progress rapidly so urgent action in getting medical attention is critical – call NHS 111 straight away
Protection against this strain of Meningitis W is provided through the Meningitis ACWY vaccine. Only one dose is required.
We also carry an excellent stock of the Meningitis B vaccine and can provide both vaccinations at the same time should you require it.
Book your MenACWY & MenB vaccination appointment online
Measles, Mumps and Rubella (MMR) Vaccination
Mumps is a highly contagious viral infection which is spread in the same way as the flu. Coughing, sneezing and kissing can rapidly spread the infection, especially in the close quarters of student accommodation.
Measles is a very infectious viral infection which is also spread by coughing and sneezing. There have been multiple outbreaks of Measles around the world including the UK this year, so it’s important to make sure you are protected as you socialise with new peers.
Both Mumps and Measles can be prevented by safe and effective vaccination, MMR.
Book your MMR vaccination appointment online
Human Papillomavirus (HPV) Vaccination
HPV is a common virus that is passed on via genital contact. There are more than 100 HPV types which infect genital areas. Sometimes they cause no harm and the infection can go away on its own. However, the virus can persist and cause cells to change which can lead to some forms of cancers; cervical, head, neck & throat or genital warts. More information on HPV can be found here.
The HPV vaccine is offered at our clinic for girls and boys to protect against HPV-related cancers and genital warts. Book your HPV vaccination appointment online
Other vaccinations that we recommend for students starting/ returning to University are:
Fresher’s Flu:
Every year different flu strains circulate and infect millions of people. Being exposed to a new pool of infections in University accommodation can increase the risk of catching the flu. Having the flu jab before you go to University will help protect you against the flu and stop you getting sick.
Flu jabs become available from 3rd September and can be booked online.
BCG:
If you are from outside the UK, you should be vaccinated against tuberculosis (TB) before you enter the UK. A weakened strain of tuberculosis, the BCG Vaccine, is injected to protect against the infection. Those unsure of their immunity can have a simple Mantoux test to confirm.
Book your BCG vaccination or Mantoux Test appointment online
Tetanus:
Tetanus is a rare condition caused by bacteria entering a wound. We recommend making sure you are up to date with your DTP vaccinations and boosters before leaving for university. This vaccine protects against tetanus as well as Diptheria and Polio. Don’t let a cut or burn ruin your freshers week.
Book your Tetanus vaccination appointment online
Wellness VACCINATIONS AT FLEET STREET CLINIC
Fleet Street Clinic offers a friendly environment and a team of experienced medics to administer all wellness vaccinations. We meet rigorous quality management standards to ensure we offer you the highest standards of clinical care: you can feel confident you are in safe hands.
Secure your peace of mind by ensuring you are protected. Get your vaccines before university starts to receive protection in time.
Book your vaccination appointment today
_____________
For the full The UK Health Security Agency (UKHSA) statement, click here.
Recombinant Flu Jab – The Most Advanced Protection from Influenza
In a world constantly battling the threat of infectious diseases, the importance of vaccinations cannot be underestimated. Influenza – the flu – is a year-round, global respiratory threat that remains a constant concern, owing to the ability of flu viruses to mutate rapidly and cause seasonal epidemics.
As science advances, so does our ability to protect ourselves from flu. Applying recombinant technology to flu vaccines is a remarkable breakthrough that has created a new generation of premium vaccines, capable of delivering enhanced protection.
Why are recombinant flu vaccines the premium offering in comparison to other flu vaccines?
Traditional flu vaccines are created by growing influenza viruses in chicken eggs, allowing the viruses to replicate, and then inactivating or weakening them for use as vaccines. This process, while effective, presents several challenges, including the potential for the virus to mutate during replication in eggs.
Recombinant flu vaccines offer an innovative alternative to these traditional methods. Instead of using live viruses, these vaccines utilise genetic engineering techniques to produce specific proteins found on the surface of the influenza virus. These proteins are then harvested and used as the key components in the vaccine.
Notably, recombinant flu vaccines eliminate the need for egg-based production, thus addressing concerns related to egg allergies and the risk of viral mutations.
Key benefits
Precise Targeting: Recombinant flu vaccines consist only of precise copies of the surface antigen proteins that flu viruses use to enter our cells. This enables the immune system to recognise and remember them, ensuring the most robust immune response possible whenever flu viruses are encountered.
Enhanced Effectiveness: The genetic engineering process in recombinant vaccines ensures a high degree of consistency and purity in the vaccine components. This consistency translates to enhanced vaccine effectiveness, reducing the risk of a mismatch between the vaccine strains and the circulating flu viruses.
Reduced Allergic Reactions: Individuals with egg allergies often face a dilemma when considering traditional flu vaccines, as these vaccines are cultivated in eggs. Recombinant flu vaccines eliminate this concern, providing a safe option for those with egg allergies.
Forward-Thinking Defence: The adaptability of the flu virus demands a vaccination strategy that can keep up with its mutations. Recombinant vaccines, designed with a focus on the virus’s evolutionary genetics offers a forward-thinking defence by stimulating immunity against a broader range of potential viral strains.
Broader Accessibility: Traditional flu vaccine production is dependent on the availability of fertile chicken eggs and a lengthy production process. Recombinant vaccines overcome these limitations, allowing for more rapid production and distribution, even in situations where egg supplies are compromised.
So, why choose a recombinant flu jab over a traditional standard fu jab?
In the fight against influenza, staying ahead of the mutating virus requires cutting-edge solutions. Recombinant flu vaccinations represent a quantum leap in our approach to flu protection, offering a targeted, effective, and forward-looking defence against the ever-changing flu strains.
As technology continues to evolve, these vaccines hold the promise of becoming the gold standard in flu protection, providing individuals with a safer, more reliable shield against this seasonal threat.
So, when the flu season comes around, consider the power of recombinant flu vaccinations—the premium offering for your ultimate flu protection.
Private Patients
For more information on our flu vaccinations and pricing.
Workplace Flu Vaccination Programmes
Fill out the form below for a quote for flu jabs for your employees.
______________
RELATED SERVICES AVAILABLE AT FLEET STREET CLINIC
In today’s health-conscious era, prioritising well-being has become a central focus in our lives. However, understanding just how fit we truly are requires a comprehensive approach.
A medical check-up is the optimal method for obtaining a holistic view of your overall health. Familiarising yourself with essential health indicators can play a pivotal role in preventing potential illnesses and diseases.
Here’s a breakdown of key health numbers that can provide valuable insights into your well-being:
- Body Mass Index (BMI):
- BMI, frequently mentioned in the media, is a straightforward index of weight-for-height. It classifies individuals as underweight, overweight, or obese based on the ratio of their weight to the square of their height in meters.
- Resting Heart Rate:
- Your resting heart rate serves as an indicator of your basic fitness level and is a reliable predictor of cardiovascular health. Monitoring this metric can offer valuable insights into your overall well-being.
- Waist to Hip Ratio:
- The distribution of body fat, especially around the abdominal area, can impact health significantly. Research suggests that fat stored in this region may contribute to heart disease, obesity, and diabetes. Understanding your waist-to-hip ratio is crucial for assessing this risk.
- Cholesterol:
- Surprisingly, over half of all UK adults have elevated cholesterol levels, and a cholesterol test is the only definitive way to ascertain if you are affected. High cholesterol is linked to heart disease, a prevalent cause of mortality in the UK.
- Blood Pressure:
- Elevated blood pressure places additional strain on your arteries and heart, potentially leading to severe health issues such as heart attacks, strokes, kidney disease, or dementia. Regular blood pressure tests are essential for early detection and preventive measures.
- Blood Sugars:
- Monitoring your blood sugar levels is critical for identifying diabetes or the risk of developing it. For type 2 diabetes, often associated with lifestyle factors, early detection allows for dietary adjustments that may prevent the need for medication and even avert the onset of the disease.
- Bone Density:
- Bone density testing, a non-invasive procedure known as bone densitometry or a bone mineral density scan (BMD), provides insights into the strength of your bones. This assessment can reveal potential risks of osteoporosis, guiding proactive measures for bone health.
- Mammogram/Prostate Check:
- Depending on age, routine checks like mammograms for women and prostate checks for men are advised by healthcare professionals. These screenings are crucial for early detection of tumors or cancerous cells, significantly improving the chances of successful intervention.
If you’re interested in discovering your health numbers, consider booking a comprehensive medical check-up or consulting your GP to determine which medical is best suited for you.
Prioritising these assessments can empower you to take control of your well-being and make informed decisions about your lifestyle.
The UK is currently facing a rapidly escalating diabetes crisis.
What does that mean?
According to a recent report published by Diabetes UK, more than 5 million people are living with diabetes in the UK, and the number is only increasing. This figure is a combination of those who have been diagnosed with diabetes and an estimate of those who are currently unaware that they are diabetic.
As a private healthcare clinic in London, Fleet St. Clinic is committed to providing support and the highest quality of care to all our patients, especially those affected by this escalating crisis.
Diabetes is a chronic condition that affects how your body regulates blood sugar. There are two main types of diabetes:
Type 1 – which is usually diagnosed in childhood and is caused by the immune system attacking the cells in the pancreas that produce insulin,
Type 2 – which is usually diagnosed in adulthood and is caused by the body becoming resistant to insulin or not producing enough insulin.
Diabetes UK’s report shows that 4.3 million people have been diagnosed with diabetes in the UK. We know that approximately 90% of these diagnoses are of type 2 diabetes, and around 8% of diagnoses are type 1 diabetes, with the other forms of the condition making up the remaining 2% including gestational, neonatal, and monogenic diabetes.
In addition, Diabetes UK also estimates there are an additional 850,000 people living with diabetes who are yet to be diagnosed, bringing the overall UK-wide figure beyond 5 million.
Year-on-year the numbers for diabetes are increasing, a worrying trend, especially as most of the diagnosis are for type 2. Diabetes UK’s report states that 2.4 million people in the UK are considered at high-risk of developing type 2 diabetes and could already be pre-diabetic.
All types of diabetes can lead to serious complications, including heart disease, stroke, kidney disease, nerve damage, and blindness. With the right treatment and management, many people with diabetes can live full and active lives.
What are the symptoms of diabetes?
The 4Ts of diabetes include:
- Thirsty
- Tired
- Toilet (needing to urinate a lot, especially at night)
- Thinner (losing weight without trying)
At Fleet St. Clinic, we offer a range of services to support patients with diabetes, including regular check-ups, blood sugar monitoring, and dietary advice. Our team of experienced healthcare professionals, including doctors, nurses, and dietitians, work together to provide personalised care tailored to each patient’s needs.
Diagnosing Diabetes:
Our most non-invasive test is the instant HbA1C test which can be a standalone appointment with a nurse or suggested by your doctor during a GP appointment. This test is used to diagnose diabetes and only requires a finger prick of blood. It takes about 6 minutes to receive results meaning you can have the test and receive the result during your consultation.
We also offer specialist services for patients with diabetes-related complications, such as foot ulcers, which can be a serious problem for people with diabetes. Our podiatrist can provide expert advice and treatment to help prevent and manage foot ulcers, which can lead to amputation if left untreated.
Diabetes can have a major effect on your eye health and greatly increase your risk of certain eye conditions, so if diagnosed, it is very important that you have your eyes checked regularly. Our sister clinic, Whitby & Co. Optician, is also based at 29 Fleet St. London and offers eye examinations which include an OCT scan. OCT scans can be useful to diagnose and monitor diabetic eye conditions such as diabetic retinopathy.
In addition to our clinical services, we also offer support to help patients with diabetes manage their condition. Our doctors and dietitian can discuss topics such as healthy eating, exercise, and medication management with you.
At Fleet St. Clinic, we understand that living with diabetes can be challenging, but we are committed to providing the highest quality of care and support to our patients.
So, if you are living with diabetes or are at risk of developing the condition, please don’t hesitate to get in touch with us. We’re here to help you manage your diabetes and live your best life.
Read the full report by Diabetes UK
Diabetes UK: “Know your risk” online tool
Related Services at Fleet St. Clinic
As a travel nurse based in London, I was concerned to hear the recent warning from health officials about the spread of tick-borne encephalitis (TBE) virus in several parts of the country. The UK Health Security Agency (UKHSA) has confirmed three cases of TBE virus in patients in Yorkshire, Norfolk, and on the border of Hampshire and Dorset. Further tests on ticks across the country have found that the disease, which was commonly found in parts of Europe and Asia until now, is now present in the UK. The experts have warned that it is unlikely that TBE virus will disappear, so it’s essential to establish a surveillance program.
Public health officials say the risk is low, but it’s essential for walkers to take precautions and seek medical help if they fall ill after being bitten, especially if by a tick.
As a clinic that specialises in travel, we are used to urging everyone to take precautions to protect themselves from tick bites anyway, but this news reinforces the importance of doing this at home as well as when travelling abroad. It is essential to cover your ankles and legs, apply insect repellent, and check clothes and your body for ticks, particularly when visiting areas with long grass such as woods, moorlands, and parks.
In most cases the TBE virus typically causes mild flu-like symptoms, but it can also lead to severe infection in the central nervous system resulting in meningitis or encephalitis a high fever with headache, neck stiffness, confusion, or reduced consciousness, and long-term impairment.
As a travel nurse, I think it is really important to educate people about the symptoms of TBE to encourage them to seek medical help immediately if they experience any of these symptoms, but also to emphasise the fact that infections are preventable.
Ticks are becoming more common in parts of the UK, mainly due to increasing deer numbers. They live in undergrowth and latch on to humans when they walk through long grass. It is thought infected ticks may have arrived in the UK via migrating birds. Scientists had suspected the virus had arrived in the UK in 2019, following a couple of cases, but complexities involved in testing meant these could not be confirmed.
It’s crucial to emphasise the significance of vaccination for individuals who are considered of a higher risk. You are much more likely to catch TBE if you work outdoors or if you enjoy outdoor activities such as camping, hiking, dog-walking, countryside rambling and even jogging. Children playing outside may be especially vulnerable.
Vaccines can provide protection, and as there is currently no known cure for tick-borne encephalitis virus, those individuals who would be considered at higher risk are advised to be vaccinated as a precaution.
It’s worth noting that a vaccine is used routinely in areas of high incidence in Europe, and its advisable to consider vaccination for individuals with outdoor occupations in regions where the virus is prevalent.
For the general public the risk of contracting TBE is relatively low. Therefore, it’s essential to educate people about TBE and encourage them to take precautions to protect themselves from tick bites, particularly when travelling to areas where the virus is found.
Related services available at Fleet Street Clinic
Tick Borne Encephalitis Vaccination
For further reading, more news coverage can be found here:
Gov.uk – Tick Borne Encephalitis detection in England
The Times – Tick-borne encephalitis warning to walkers
The Telegraph – First cases of rare tick disease found in England
SPRING IS UPON US!
A time of longer days, shorter nights, flowers in bloom, and warmer weather allowing us to spend much more time enjoying the great outdoors.
This year, March 26th marks the start of British Summer Time when the clock springs forward 1 hour, increasing daylight, prolonging our evenings and our transition to Summer begins.
Spring is the time of year when we emerge from our winter hibernation and seek more time in the fresh air, the outdoors, in nature and with friends and family.
There are so many health benefits that Spring has on our physical and mental well-being.
But in what ways specifically is Spring good for our health?
1. Spring makes us feel more energised
There’s nothing quite like the feeling of the warm sunshine on our skin after a long, cold winter.
This small act of nature, in general, makes us feel more upbeat and positive and can quite literally give us a “spring in our step!”. Exposure to natural light is thought to increase the brain’s release of a hormone called serotonin. Serotonin is associated with boosting mood and helping a person feel calm and focused with a more optimistic outlook to life.
With sunlight and sunshine increasing, spring is a natural positive energiser.
2. Spring weather encourages us to be more active
With the weather improving and the temperature rising it encourages us to get outdoors and be more active. That doesn’t mean we’re all inspired to run a marathon, but time outdoors is good for your physical and mental health.
Time in the fresh air can really help you to switch off from your daily stresses, reduce your blood pressure and improve your mood.
Spring encourages us to take up a new sport, go out for walks and spend more time being active.
3. Spring sunshine tops up our vitamin D
Getting enough vitamin D is essential for the typical growth and development of our bones, teeth and muscle health, as well as improving our resistance to certain diseases.
Extra daylight gives you more time to spend outside and soak up the nutrients from the sunshine. In Spring and Summer, most people are able to make all the vitamin D they need from the sunlight on their skin without the need for supplements.
4. Spring encourages us to clean our home
Spring is the perfect time of year to air out our homes, clean out the grime that has built up over the winter and make a fresh, clean start.
There are many health benefits to giving your house a deep spring clean, such as:
- Reducing your risk of allergies and asthma from the accumulation of dust or pet dander.
- By removing germs and bacteria, especially from hard-to-reach places, you are reducing your risk of getting sick in general.
- Visual clutter leads to mental clutter; so, doing a big tidy-up should see improvements in your mental health and even increase your productivity.
Is it time to spring clean your health?
Related services available at Fleet Street Clinic.
Cholesterol is a type of fat that is found in the blood and plays an important role in our bodies. However, high levels of cholesterol can lead to serious health issues, such as heart disease, stroke, and other cardiovascular problems. Unfortunately, cholesterol is often referred to as a “silent killer” as there are usually no symptoms and the first indication that something is wrong may be a heart attack. That’s why it’s important to have your cholesterol levels checked regularly.
Instant cholesterol testing only requires a short nurse appointment that provides you with both the test and the results during the same appointment. This type of testing makes it easy and convenient for people to understand their cholesterol levels and take steps to keep them under control.
Statistics from the National Institute for Health and Care Excellence (NICE) show that cardiovascular disease (CVD) is the leading cause of death in the United Kingdom, accounting for around 26% of all deaths. The most common type of CVD is coronary heart disease, which is caused by a build-up of fatty deposits in the arteries leading to the heart. High cholesterol levels can contribute to the formation of these fatty deposits.
By knowing your cholesterol numbers through instant testing, you can understand your risk of developing CVD and take the necessary steps to keep your levels under control. NICE recommends that all adults in the UK should have their cholesterol levels checked at least once every five years, or more frequently if they are at increased risk of CVD. Those at increased risk include people with a family history of CVD, smokers, people with high blood pressure, and people with diabetes.
To keep your cholesterol levels under control, it is important to make changes to your diet. This includes eating more fruits, vegetables, whole grains, and lean proteins, and reducing your intake of saturated and trans fats. You should also aim to maintain a healthy weight and be physically active for at least 30 minutes a day.
If lifestyle changes are not enough, medication may be required. The most common type of cholesterol-lowering medication is statins, which work by reducing the production of cholesterol in the liver. Statins are widely used in the UK and are safe and effective.
The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
Further reading on “NICE recommends wider use of statins for prevention of cardiovascular disease (CVD)”.
In conclusion, instant cholesterol testing provides an easy and convenient way to understand your cholesterol levels and take steps to keep them under control. Regular testing is important for everyone in the UK, especially those who are at increased risk of CVD. By knowing your numbers, making changes to your diet, maintaining a healthy weight, and being physically active, you can help keep your cholesterol levels in the healthy range and reduce your risk of developing serious health problems.
Related services available at Fleet Street Clinic:
Instant Cholesterol Testing with a nurse
Blood Tests at Fleet St. Clinic
Well Person Medical
GP Services
As a private healthcare clinic, our goal is to provide the best protection against pneumonia for our patients. One of the key tools in this fight is the pneumococcal vaccine. One of the latest advancements in this area is the Apexxnar vaccine. This 20-valent vaccine provides protection against 20 different serotypes of the pneumococcal bacteria, offering a more comprehensive defence against pneumonia.
We understand that choosing the right vaccine can be complex and that different patients may require different solutions. That’s why we recommend speaking with one of our healthcare providers to determine which vaccine, including Apexxnar, is best for you. They will consider risk factors such as your age, underlying health conditions, and previous vaccinations, to ensure you receive the most effective protection against pneumonia.
At Fleet St. Clinic, we believe in the power of prevention, and that the right vaccine can make all the difference. So, if you’re looking for the best defence against pneumonia, consider talking to us about the Apexxnar vaccine today.
Information about Pneumonia:
Pneumonia is a lung infection that can cause a range of symptoms, including:
- Cough: A persistent cough that produces mucus or phlegm is a common symptom of pneumonia. The cough may be dry or productive, and the mucus or phlegm may be green, yellow, or rust-coloured.
- Fever: Pneumonia often causes a high fever, which may be accompanied by chills and sweats.
- Shortness of breath: Pneumonia can cause difficulty breathing, especially during physical activity. The shortness of breath may be accompanied by chest pain or tightness.
- Fatigue: Pneumonia can cause extreme tiredness and weakness, making it difficult to carry out normal daily activities.
- Muscle aches: Pneumonia can cause muscle aches and joint pain, which may be mistaken for the flu.
- Chest pain: Pneumonia can cause chest pain, especially when breathing deeply or coughing.
- Nausea and vomiting: Some people with pneumonia may experience nausea and vomiting, especially if the infection is caused by a type of bacteria known as Legionella.
- Confusion or disorientation: Pneumonia can cause confusion or disorientation, especially in older adults and people with underlying health conditions.
It’s important to seek medical attention if you experience any of these symptoms, as pneumonia can be a serious and potentially life-threatening condition.
More information on pneumonia.
Who is considered “high-risk”?
Individuals considered to be at high risk for hospitalisation due to pneumonia include the elderly, young children, people with weakened immune systems (including people who have had their spleen removed), and individuals with underlying health conditions such as chronic heart or lung diseases, diabetes, and liver or kidney problems.
At the Fleet St. Clinic, we also regard anyone who has had a previous significant episode of pneumonia as likely to benefit from being vaccinated.
When is the best time for a pneumonia vaccine?
The best time to vaccinate against pneumonia depends on various factors such as the type of vaccine, the individual’s age, and underlying health conditions.
The pneumonia vaccine is not the same as the flu vaccine, as it doesn’t need to be given at a certain time of year.
For the pneumococcal vaccine, it is generally recommended to receive the vaccine once in a lifetime for most adults. Some individuals may need a booster shot, and this is determined by a healthcare provider such as a doctor or nurse.
How to book an appointment?
Booking an appointment is easy. If you are on the go, you can book online through our online booking system, pre-payment is required.
If you would like to discuss anything further or would like to book with our reception team, you can call them on +44 207 353 5678 or email us at info@fleetstreetclinic.com
Related services available at Fleet Street Clinic:
Statins are a widely prescribed class of drugs used to lower cholesterol levels and prevent cardiovascular events such as heart disease and strokes. The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
This decision was made after the independent committee updating the NICE guideline on cardiovascular disease (CVD) risk assessment and reduction considered new evidence on the safety and side effects of statins, meaning more people could be given them.
The draft guideline recommends that doctors should consider statins for people who haven’t had a CVD event (called ‘primary prevention’) with a 10-year CVD risk score of less than 10%. The committee agreed that if more people took statins there would be a greater reduction in the incidence of heart disease and strokes.
In addition to being prescribed by National Health Service GP’s, statins can also be prescribed by private healthcare providers, such as us, Fleet Street Clinic. In fact, private GP’s can play an important role in the management of cardiovascular disease risk by offering statins as part of a comprehensive treatment plan for patients at high risk.
People can be at risk from CVD because of factors they cannot change including their age, sex, ethnicity and family history but it’s important to note that certain lifestyle changes can reduce the risk. These include stopping smoking, reducing alcohol consumption, introducing or increasing exercise and eating a healthy diet.
Therefore, the decision to take a statin should be made in consultation with a healthcare professional and should take into account the individual’s values and priorities as well as the potential risks and benefits of treatment.
With the British Heart Foundation noting that “there are around 7.6 million people living with heart and circulatory diseases in the UK” and that they “estimate that in the UK more than half of us will get a heart or circulatory condition in our lifetime” this is likely to be an impactful change in the landscape of CVD and statins.
To conclude, Paul Chrisp, director of the Centre for Guidelines at NICE, said:
“What we’re saying is that, for people with a less than 10% risk over 10 years of a first heart attack or stroke, the decision to take a statin should be left to individual patients after an informed discussion of benefits and risks.
“The evidence is clear, in our view, that for people with a risk of 10% or less over 10 years, statins are an appropriate choice to reduce that risk.
“We are not advocating that statins are used alone. The draft guideline continues to say that it is only if lifestyle changes on their own are not sufficient, and that other risk factors such as hypertension are also managed, that people who are still at risk can be offered the opportunity to use a statin, if they want to. They don’t have to, and their decision should be informed by an understanding of the risks and tailored to their values and priorities.”
Reference Source: https://www.nice.org.uk/guidance/indevelopment/gid-ng10178/documents
Related services available at Fleet Street Clinic:
Sleep plays a crucial role in maintaining overall health and well-being, and recent research has revealed a strong link between sleep and cardiovascular health. A study conducted by the University of Warwick in the UK found that individuals who get 7-9 hours of sleep per night have a lower risk of cardiovascular disease (CVD) and mortality compared to those who sleep less or more than the recommended range.
The study, published in the Journal of the American College of Cardiology, analysed data from over 116,000 participants in the UK Biobank study and found that those who slept less than 6 hours or more than 9 hours had a higher risk of CVD and mortality. These findings add to the growing body of evidence that suggests a link between sleep duration and cardiovascular health.
The exact mechanisms by which sleep affects cardiovascular health are not fully understood, but researchers suggest that it may be related to the impact of sleep on cardiovascular regulation, inflammation, and metabolic function.
It is important to prioritize sleep and aim for the recommended range of 7-9 hours to maintain cardiovascular health.
It’s worth noting that these findings are observational, and more research is needed to fully understand the relationship between sleep and cardiovascular health, but it’s a good indication that sleep plays a vital role in maintaining a healthy cardiovascular system.
To read the full study, continue reading here:
medscape.co.uk – Does sleep duration influence cvd and mortality risk?
Related services available at Fleet Street Clinic:
Dry January grows in popularity year on year.
The campaign by Alcohol Change UK, encourages participants to give up alcohol for the entire month of January.
The dry January one-month booze-free challenge can have a significantly positive impact on your health.
Alcohol has proven to increase the risk of developing a range of health problems (including cancers of the mouth, throat and breast) and that risk increases the more you drink on a regular basis.
Ruth Kander, our dietitian, looks at what is considered a safe amount of alcohol consumption.
The UK Chief Medical Officers’ (CMOs) guideline for keeping health risks from alcohol to a low level for both men and women states that:
- It is safest not to drink more than 14 units a week on a regular basis.
- Regularly drinking as much as 14 units per week, it’s best to spread your drinking evenly over three or more days.
– If you have one or two heavy drinking episodes a week, you increase your risk of death from long-term illness and injuries. - Cutting down the amount you drink, a smart way to help achieve this is to have several drink-free days a week.
A useful website for more information about alcohol is www.drinkaware.co.uk
What is a unit of alcohol?

How long does alcohol stay in your body?
On average, it takes about one hour for your body to break down one unit of alcohol, however, this can vary, depending on:
- Your weight
- Whether you’re male or female
- Your age
- Your metabolism – how quickly or slowly your body turns food into energy
- How much food you have eaten
- The type and strength of the alcohol you have consumed
- Whether you’re taking medication and, if so, what type
- It can also take longer if your liver isn’t functioning normally
If I am on medicines can I drink alcohol?
People taking sedative drugs (like diazepam/valium) or antidepressants (like fluoxetine/Prozac) should avoid alcohol altogether.
There are some antibiotics; metronidazole and tinidazole which just do not mix with alcohol – drinking with these will make you sick. But for most commonly prescribed antibiotics, drinking is unlikely to cause problems so long as it is within the low-risk alcohol unit guidelines.
People taking long-term medications should be careful about drinking, as alcohol can make some drugs less effective and long-term conditions could get worse. Examples of long-term medications include drugs for epilepsy, diabetes, or drugs like warfarin to thin the blood.
(From www.drinkaware.co.uk)
What are the consequences of drinking too much alcohol?
- Low mood/mood swings
- Liver problems
- Heart problems
- Cancers (mouth, tongue, throat, oesophagus)
- Weight gain
- Poor sleep
- Blood pressure instability
By Ruth Kander BSc(Hons)RD | Dietitian
If you wish to discuss ways to maintain a healthy diet and reduce your alcohol consumption, Ruth holds a virtual clinic every Friday from 9am-2pm. Please call our reception team on 020 7353 5678 if you would like to request a face-to-face appointment
Cases of Strep A infections amongst children are on the rise and tragically at least 9 children are known to have died in the UK as a result.
What is Strep A?
Group A streptococcus (GAS) is a common bacteria. Lots of us carry it in our throats and on our skin and it doesn’t always result in illness. However, GAS does cause a number of infections, some mild and some more serious.
Strep A causes infections in the skin, soft tissue and respiratory tract. It’s responsible for infections such as tonsillitis, pharyngitis, scarlet fever, impetigo and cellulitis among others.
Strep A Infections are not common but it is important for parents to lookout for symptoms and consult a GP as soon as possible for early diagnosis and treatment. Strep A infections are treatable if caught early.
Symptoms of Strep A
The first symptoms to appear are fever, chills, muscle aches and sore throat with difficulty swallowing.
Later, a rash may develop and the tongue may become red and inflamed. There may be pus on the tonsils which can be seen as white exudates. The disease affects the neck as well as it becomes tender due to the enlargement of the lymph nodes.
Small children may also present with headaches and abdominal pain in addition to the above symptoms, plus even nausea and vomiting.
How does the disease spread?
School children are in the close contact with each other and hence, they are more likely to spread the disease. In the past, GPs have been advised not to prescribe antibiotics if avoidable.
Strep A needs treatment with Penicillin or an alternative antibiotic in the case of penicillin allergy.
Children with strep A must stay at home until recovered to avoid spreading the bacteria.
How can you protect your child
It is very important for carers to stay vigilant and lookout for any symptoms that their child might have. If there is any suspicion of Strep A, make sure that the child is treated with antibiotics or an alternative just to be safe.
To limit the risk of infection, parents must not send children to school with tonsillitis, so that the spread of the disease can be reduced.
If your child develops symptoms:
- consult your GP for proper medical advice
- do not leave it until your child is seriously unwell to get treatment
Call 999 or go to A&E for emergency help if your child:
- develops difficulty breathing
- pauses between breaths
- will not wake or stay awake
- their skin, tongue or lips change colour to blue
The number of cases can be reduced if proper care is taken for Strep A and its symptoms.
_____________________________
We are a family friendly health clinic – if your child needs to see a GP – book online.
________
Dr Belinda Griffith’s comments in the UK news:
Independent Online: How can I protect my child from Strep A?
Yahoo! News: Health: How can I protect my child from Strep A?
The Herald Scotland: How can I protect my child from Strep A?
Flu cases in the UK have increased earlier this winter than usual, perhaps by over a month.
Other unpleasant respiratory infections such as RSV are also on the rise.
Information from around the world can help us predict what might type of flu season might be heading our way.
- Australia has just come to the end of a bad flu season, with a dramatic increase in flu cases and hospitalisations relative to the mild season it experienced last year, in a pattern likely to be replicated in the UK.
- In the USA, by the end of November 2022 there had already been more than 6.2 million flu cases, with 53,000 hospitalisations, and 2,900 deaths from flu.
- Across Europe as a whole, the flu season has commenced earlier than in the 4 previous seasons, and the proportion of positive tests from sentinel locations has exceeded the technical threshold for consideration as an epidemic.
Meanwhile, UK vaccination rates have so far been low: by the end of November, when the flu vaccination campaign should be largely complete, fewer than 40% of “at risk” adults under 65 had been vaccinated, fewer than 25% of healthy adults aged 50 to 64, and fewer than 30% of pregnant women.
So this winter’s flu season is likely to be more severe, and not enough people will be protected.
What can you do to keep well this winter?
Get Vaccinated . Get Tested . Get Treatment
Get Vaccinated
The good news is that circulating flu strains have so far been a good match with this year’s flu vaccines. It is not too late to be vaccinated. Vaccines are still available. At this point in the season, our preferred vaccine for adults is our premium recombinant vaccine, Supemtek, which is known to be highly immunogenic.
Flu cases in children are rising but the nasal spray vaccine has so far been in restricted supply. If your child has not yet been able to obtain the flu spray, injected flu vaccines are at least as effective and should be given without further delay.
You can easily book your flu jabs online.
For family or groups bookings, it may be more convenient for you to book by phone or email.
Get Tested
At the Fleet Street Clinic, we can test quickly and accurately for a full panel of respiratory viruses in our own laboratory. It is helpful to know whether you are suffering from flu, covid, or another circulating virus such as RSV or metapneumovirus. We can tailor treatment to the result, help you know how long symptoms will last, and can help you prevent spreading it to others – especially important over the Christmas period when socialising in high at work and amongst family and friends.
Get Treatment
Flu is treatable with anti-viral drugs, which reduce symptoms and speed recovery. Preventive treatment for close contacts and other members of your family is also something we can help with, available from our GPs. Knowing for certain that you have a viral infection can also help avoid unnecessary antibiotic treatment.
___________________________
For more information on Flu Jabs available at Fleet Street Clinic.
Other recommended winter vaccinations are the shingles vaccine & the pneumonia vaccine.
We can also provide onsite Workplace Flu Vaccinations for companies in the UK – for more information.
Complete the below form for a quote:
Mental Health Awareness Week: What Is Stress?
Look around your office, do you know if anyone is struggling?
You may think those around you – fellow colleagues or your staff – are completely fine. But mental health affects us all and problems in the workplace are actually very common.
According to mental health charity Mind, at least one in six workers are experiencing common mental health problems, including anxiety and depression.
Nowadays, there is increasing recognition of stress and mental health problems, both within the workplace and in everyday life. Currently, following Stress Awareness Month in April, we are approaching Mental Health Awareness Week, which takes place from 13-19th May.
We thought it might be helpful to focus on some positive strategies to help, in terms of stress management and resilience. Whilst being particularly useful and relevant within the workplace, these can all be used in everyday life as well.
WHAT IS STRESS?
In its purest form, stress is the body’s reaction to something it perceives as dangerous or threatening. When we feel under attack, our bodies respond by producing a mixture of hormones such as adrenaline and cortisol. These prepare us for physical action by diverting blood away from our core and into our limbs. It also temporarily shuts down some less vital bodily functions such as digestion.
For immediate, short-term situations, stress can be beneficial to your health, by helping you cope with potentially serious situations.
Yet if your stress response continues, and stress levels stay elevated far longer than necessary, it can take a toll on your health.
WHY IS IT IMPORTANT TO TACKLE STRESS?
Chronic stress can cause a variety of symptoms, contribute to many health problems (such as high blood pressure, heart disease, obesity and diabetes, anxiety and depression) and affect your overall well-being.
Reducing stress can help prevent these harmful effects on both mind and body.
Looking after yourself and ensuring you have good mental health has many benefits – not just for you as an individual, but for the business too. Employees are generally more productive, passionate and motivated when in good health. Even if they’re experiencing mental health problems, knowing they are supported by their employer can help in the recovery process.
STRESS PREVENTION IS BETTER THAN STRESS MANAGEMENT
Ultimately, the best way to manage stress is through prevention rather than cure.
Research shows that those who are better informed about the practical ways in which they can lower their stress levels are far better able to tackle difficult situations with emotional resilience and determination.
Within the workplace, employers are encouraged to make promoting the wellbeing of their employees a core element of the company’s internal operations. Some examples of a proactive approach to stress-management might be:
- To invite people to take active breaks away from their desks
- Offering lunchtime yoga classes or mindfulness sessions
- Group walks in the fresh air.
So what can help you reduce stress? Continue reading our stress, with Our Top Tips For Reducing Stress.
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch. Or if you are an individual who needs help with stress management, you can book a GP appointment online.
Feeling stressed?
Everyone feels stressed from time to time. In small doses, stress can actually be quite useful; motivating us to achieve our goals. But for some, stress is chronic. Meaning it is debilitating and negatively impacts their mood, their health and wellbeing, their relationships and their work.
Experiencing a lot of stress over a long period of time can also lead to a feeling of physical, mental and emotional exhaustion, often called burnout. It is, therefore, easy to see why reducing stress across all areas of your life would be important. Stress management tips are a good place to start.
Learning how to manage your stress takes practice and time.
Here are our top 10 ways on managing and reducing stress.
10 TIPS TO REDUCE STRESS:
-
Prioritise your health
– make decisions which will benefit your physical, mental and emotional wellbeing. For example, go alcohol-free a few nights each week or allow yourself time for a hobby you enjoy. These small steps for a healthier lifestyle will help in reducing stress levels.
-
Get a good night’s sleep (regularly)
– research clearly shows that sleep deprivation amplifies the symptoms associated with stress. Aim for between 7-9 hours of good quality sleep every night.
-
Practice deep breathing
– when our bodies are stressed, the muscles that help us breathe tighten. By focussing on taking several deep breaths we can quickly and effectively relieve physical symptoms associated with feeling stressed or anxious. Try to do this regularly throughout the day.
-
Drink enough water
– being dehydrated (however mild) causes our cortisol levels to rise, which automatically makes us feel stressed. Your body is already dehydrated if you’re feeling thirsty. So try to avoid reaching this point by hydrating yourself regularly. Aim for 2-3 litres per day, more in hot weather or when exercising.
-
Eat a balanced diet
– dieticians stress how certain foods have stress-relieving properties. For example, dark chocolate is rich in antioxidants, whilst avocados and oily fish are high in omega-3 fatty acids (both of which are proven to help lower anxiety levels).
-
Exercise regularly
– physical activity causes our brains to release mood-improving chemicals called endorphins. These help us to cope with potentially challenging situations. Both Public Health England and the World Health Organisation recommend at least 150 minutes of moderate intensity physical activity each week, in bouts of 10 minutes or more. Choose activities you enjoy to achieve maximum benefit for the mind as well as the body.
-
Adopt a positive mindset
– research suggests that making a conscious effort to think positively can help protect us against a whole host of physical and mental issues, including stress.
-
Manage your time and tasks effectively
– by giving ourselves enough time in which to complete a given task, and by making sure that we don’t try and accomplish too many stressful things at once, we can reduce the likelihood of feeling overwhelmed.
-
Spend less time online
– many studies have found a strong positive correlation between internet usage and stress levels. Spending less time on our computers and phones is a simple way to practice self-care. Having screen-free time for at least an hour before bedtime has also been shown to improve sleep.
-
Learn to say no
– in a culture that demands we take on more and more responsibilities, having the confidence to say “no” will only become more important. This final tip takes us back to the start, by reiterating the importance of prioritising our health above unrealistic social pressures, and brings us onto developing an essential tool – resilience.
Continue reading about Resilience or read What is Stress?
If you are interested in how Fleet Street Clinic can assist your workplace with stress management and resilience training, get in touch.
Or if you are an individual who needs help managing stress, you can book a GP appointment online. Our doctors will be able to talk through your thoughts, symptoms and emotions and set you on the right path to diagnosis. They will also be able to recommend relevant support services for stress, if appropriate.
Mental Health Awareness Week: Resilience
WHAT IS RESILIENCE?
Resilience is the ability to recover from adversity, hardships, or significant sources of stress.
It means “bouncing back” from difficult experiences, feeling stronger and more capable to cope than before. With life becoming more stressful than ever, it is an important skill to develop which can make a big difference between surviving and thriving within work and general life.
HOW RESILIENT AM I?
Research has shown that resilience is ordinary, not extraordinary, and is not simply a trait we either have or do not have.
So here’s the good news! Resilience can be developed. It involves behaviours, thoughts and actions which can be learned and developed in anyone.
SO HOW CAN I DEVELOP RESILIENCE?
Many studies show that the primary factor in developing resilience is having caring and supportive relationships within and outside the family, including at work. Relationships fostering trust, provide role models and offer encouragement and reassurance help bolster resilience.
Several additional factors are associated with resilience, including:
- The capacity to make realistic plans and take steps to carry them out.
- A positive view of yourself and confidence in your strengths and abilities.
- Skills in communication and problem-solving.
- The capacity to manage strong feelings and impulses.
These are all factors you can develop in yourself, and which can be fostered within the work environment by employers taking an active interest in employees’ wellbeing.
TOP TIPS FOR DEVELOPING RESILIENCE
Here are a few things you could try, to develop your resilience.
Please don’t feel you need to tackle them all at once – trying one or two at a time may be enough to make a big difference!
1) Create connections
– good relationships with family, friends and colleagues are crucial. Accepting help and support from those who will listen to and care about you strengthens resilience. Assisting others in their time of need can benefit you in return.
2) Accept that change is fundamentally part of living
– accepting circumstances that cannot be changed can help you deal with these more effectively whilst focussing on circumstances that you can alter.
3) Avoid seeing stressful events as insurmountable problems
– try to look beyond the present towards how future circumstances may be a little better. Take note of any subtle ways in which you might already feel better as you deal with difficult situations – signs of good progress.
4) Take decisive action
– this can assist you in giving some control over your response to challenging situations
5) Pursue your goals
– making them small but achievable and most importantly realistic. Each day, ask yourself “What’s one thing I know I can accomplish today which will help me move in the direction I want to go? Take baby steps in the right direction!
6) Nurture a positive outlook
– developing confidence in your ability to solve problems and trusting your instincts helps build resilience.
7) Keep things in perspective
– retaining an optimistic outlook and visualising what you want, rather than worrying about what you don’t want, can all help the brain engage with this.
8) Practice mindfulness and meditation
– Mindfulness means paying more attention to the present moment – to your own thoughts and feelings, and to the world around you. Meditation involves the use of techniques such as mindfulness to train attention and awareness. Mindfulness and meditation are believed to relax and calm the brain, tackling sources of stress while improving clarity focus and even sleep. According to mentalhealth.org.uk, those practising mindfulness have shown increased activity in the area of the brain associated with positive emotions.
9) Take opportunities for self-discovery and personal growth
– by learning something about themselves, people may find that they have grown in some respect. Many people who have experienced tragedies and hardship have reported better relationships, a greater sense of strength even while feeling vulnerable, increased sense of self-worth, a more developed spirituality and heightened appreciation for life.
10) Take good care of yourself
– pay attention to your own needs and feelings. Engage in activities that you enjoy and find relaxing. Exercise regularly. Taking care of yourself helps to keep your mind and body primed to deal with situations requiring resilience.
If you would like further help and support in resilience training in your workplace, get in touch with our Corporate Health department.
Stress: Are we coping?
We all feel the effects of stress in daily life, whether it’s managing children or dealing with a problem at work. Stress is a normal response, in fact, in small doses, stress can be useful. The problems arise when you start to have a ‘fight or flight’ stress response to situations in everyday life. This can lead to illness, both mentally and physically.
The first step is to recognise symptoms of stress:
- Nail biting and fidgeting
- Over-eating or loss of appetite
- Irritability with other people
- Substance abuse, including alcohol and smoking
- Lack of concentration
- Increased and suppressed anger
- Feeling out of control
- Excessive emotion & crying
- Lack of interest in anything
- Permanently tired even after sleep
By identifying stress-related problems as early as possible, action can be taken to avoid any serious stress-related illness. For Mental Health Awareness week, which runs from 14-18 May, here are some tips to help manage your own personal stress:
- Be active – 30 minutes a day can reduce the emotions and let you take the time to think more clearly
- Take control – you are your own worst enemy, but you are also the key to empowerment!
- Find support – Connect with your family and friends, the more help the better the solutions
- Take time for yourself – remember to have time for yourself as well. Read, relax and get things done on your to do list that may be holding you back
- Create challenges for yourself – Setting achievable goals, little or big can help build confidence in your abilities
- Avoid unhealthy habits – Cut down on caffeine, smoking, and alcohol. These can enhance the feeling of stress in the long run
- Be positive – Instead of looking at problems negatively, try to see what you can get out of it to help you grow. Be grateful!
- Acceptance – Take ownership of mistakes, or acceptance of things you can’t control.
Our Occupational Health team at the Fleet Street Clinic are able to provide a full range of work health assessments to address the occupational health needs of your staff. Click here for more information.
To book an appointment with one of our friendly doctors, or for further details on what we can offer for our Occupational Health, call us today on 0207 353 5678 email info@fleetstreetclinic.com or book online now.

Cutting back on alcohol can be a really effective way to improve your health, boost your energy, loose weight and save money.
In 2016, the Chief Medical Officers in the UK reduced the recommended amount of alcohol you should consume a week due to concerns about the risk of cancer. New research confirmed that even drinking a small amount of alcohol per week can cause an increase in risk of cancer.
From then onwards, it has been recommended that men and women have the same weekly intake of units per week. According to the UK low risk drinking guidelines, you should drink no more than 14 units a week, make sure you have several drink-free days, and never binge drink.
What does 14 units of alcohol look like?
Because alcoholic drinks come in different strengths and sizes, units are a way to tell how strong your drink is. 14 units is equivalent to six pints of average strength beer or six medium (175ml) glasses of average strength wine.

It’s safest for both men and women to drink no more than 14 units a week, spread over three or more days with several drink-free days, and no bingeing.
Your risk of death from long term illness, accident or injury, is increased if you ‘binge drink’ 1 or more times a week.
How long does alcohol stay in your body:
On average, it takes about one hour for your body to break down one unit of alcohol. However, this can vary, depending on:
- Your weight
- Whether you’re male or female
- Your age
- How quickly or slowly your body turns food into energy (your metabolism)
- How much food you have eaten
What are the consequences of drinking too much alcohol:
- Low mood/mood swings
- Liver problems
- Heart problems
- Cancers (mouth, tongue, throat, oesophagus)
- Weight gain
- Poor sleep
- Blood pressure instability
What are the benefits to cutting down on alcohol?
Short-term benefits:
- waking up in a better mood
- being less tired and more energetic throughout the day
- healthier looking skin
- saving some money
Long-term benefits:
- lower your blood pressure
- lower the risk of diseases including cancer, stroke, hypertension and liver disease
- lower your cholesterol levels
- your memory will improve
- better quality of sleep
- help with weight management*
* Did you know? Alcoholic drinks are high in calories, so cutting back on the amount you drink can really help to reduce your calorie intake.
According to our GP & Occupation Health Physician, Dr Claire Braham;
“When you drink alcohol, you lose around 4 times as much fluid as you drink.
It is therefore easy to understand why dehydration often occurs. Dehydration symptoms are much like your classic hangover symptoms and will include headache, nausea and fatigue. These symptoms will become present when you are about 2-percent dehydrated, which is about when you start to feel thirst.
Avoiding alcohol means better hydration and sleep which will reduce hangovers and headaches, reduce tiredness, reduce sickness, increase your concentration and improve your overall control over emotions and behaviour. This leads to more productivity, better decision making and overall less accidents, regrets and more enjoyment.
It is not advised to drink more than 14 units a week, which is the equivalent of 6 pints of beer. That converts to 1,092 calories in total and would need 109 minutes of running to burn off those additional consumed calories. Abstinence is an easy way to avoid festivity weight gain.
Nowadays it is very easy to cut down or cut out alcohol. There is a wide variety of alcohol-free beer, wine, prosecco, gin, vodka, whisky and other spirits available on the market. These include some which are vegan and gluten-free as well as often free from sugar and artificial sweeteners. So you can still enjoy a ‘drink’, without the alcohol and high-sugar but with health benefits.”
For further detail of how alcohol can have a negative impact on your health, head to drinkaware.co.uk for more information and advice on drinking.
If you have concerns about the amount of alcohol you are drinking or about your health you should speak to a GP. You can book an appointment online.
More information on our GP service can be found here.
Urgent polio boosters advised for London children
UK Health Security Agency (UKHSA) has announced that all children aged 1-9 years regardless of previous immunisation status are recommended a polio vaccine booster from all London boroughs.
The virus, which can cause paralysis, has been found 116 times in London’s waste water between February and July this year.
In the UK, the overall risk of paralytic polio is considered low because most people are protected from this by vaccination. However, due to the recent discovery of type 2 vaccine-derived poliovirus in sewage in multiple locations in London, the Joint Committee on Vaccination and Immunisation (JCVI) have advised that booster vaccinations in all children aged 1-9 years is an appropriate course of action.
The UKHSA says most of the samples detected are the safe vaccine form of polio, but “a few” have mutated enough to be considered dangerous.
Parents should seek the polio vaccine booster as soon as possible – even if their child is up-to-date with their childhood vaccinations.
The aim is two-fold; to ensure a high level of protection from polio paralysis and help reduce further spread of the polio virus across London and beyond.
Booster Polio Vaccinations at Fleet Street Clinic
We offer two vaccinations in-clinic that offer protection from Polio:
Revaxis Vaccine: Suitable for children from 6 years and above
Protects against: Diphtheria, Tetanus, Polio
Cost: £49 + £28 appointment fee
Call to book
Repevax Vaccine: Suitable for children from 3 years and above
Protects against: Diphtheria, Tetanus, Polio & Whooping Cough
Cost: £105 + £28 appointment fee
Call to book
Both of these vaccinations are inactivated, and given by injection. They are both licensed as booster doses, and are not intended for primary immunisation.
More information on the Polio vaccines available at Fleet Street Clinic, click here.
Primary Polio Vaccination
Unfortunately, we do not offer the infant/ baby vaccination for Polio – in the UK this would be the Infanrix-Hexa, the 6-in-1 vaccine. We have no suitable vaccination for children under the age of 3, or for those requiring their primary immunisation against Polio.
Please contact your NHS doctor or an alternative provider to see if they can help you further.
Dr Vanessa Saliba, Consultant Epidemiologist at UKHSA, said:
“It is vital parents ensure their children are fully vaccinated for their age. Following JCVI advice all children aged 1 to 9 years in London need to have a dose of polio vaccine now – whether it’s an extra booster dose or just to catch up with their routine vaccinations. It will ensure a high level of protection from paralysis. This may also help stop the virus spreading further.”
______________________
More information on Polio and the emerging London findings:
What is Polio?
Polio is a serious viral infection that is transmitted through the stool’s of an infected person through contaminated water, food or surfaces. It can cause unpleasant flu-like symptoms and in severe cases, cause paralysis.
What are the symptoms of Polio?
The majority of people with the infection have no symptoms but some feel as if they have the flu, with:
- high temperature
- sore throat
- headache
- abdominal pain
- sickness
In severe cases of polio, the virus can attack the nerves in the spine and brain which can cause paralysis. In some cases, it can cause persistent or lifelong difficulties and even be life-threatening.
Where has Polio been found?
According to the UKHSA statement, in addition to the findings earlier this year of type 2 poliovirus (PV2) collected from the Beckton sewage treatment works, further upstream sampling undertaken by the UK Health Security Agency (UKHSA) and the Medicines and Healthcare products Regulatory Agency (MHRA) has now identified at least one positive sample of the poliovirus, currently present in parts of the following boroughs:
- Barnet
- Brent
- Camden
- Enfield
- Hackney
- Haringey
- Islington
- Waltham Forest
The sampling has also detected the virus in lower concentrations and frequency in areas adjacent to the Beckton catchment area to the South (immediately below the Thames) and to the east of Beckton. However, it is not clear whether the virus has established itself in these areas or if the detections are due to people from the affected area visiting these neighbouring areas.
How many cases of Polio have been identified?
To date, again based on the UKHSA statement, ‘a total of 116 PV2 isolates have been identified in 19 sewage samples collected in London between 8 February and 5 July this year’.
A further 15 sites in London will start sewage sampling in mid-August, and 10 to 15 sites will be stood up nationally to determine if poliovirus is spreading outside of London.
To book your child’s Polio Booster Vaccination, call +44 20 7353 5678 today.
WHAT IS DIABETES?
Diabetes is a lifelong condition that occurs when the body is unable to properly regulate the amount of glucose (sugar) in your blood. Poor control of diabetes can lead to high blood sugar levels and cause long term damage to your overall health and organs.
WHAT HEALTH PROBLEMS DOES IT CAUSE?
High blood sugar levels can cause a lot of damage to your body and if not managed correctly, may lead to many diabetic complications. This will cause long term health problems, especially if they go untreated.
HOW DOES DIABETES AFFECT OTHER PARTS OF YOUR BODY?
Eyes: Retinopathy is a complication of diabetes caused by high blood sugar levels damaging the retina, often leading to vision impairment. It is the leading cause of blindness among working-age adults in the UK. As a consequence of diabetic retinopathy, swelling can take place, called diabetic macular oedema. People with diabetes are also more prone to develop cataracts and glaucoma at an earlier age, contributing to vision reduction.
Feet: Foot health is often a neglected area anyway but high blood glucose levels can lead to insensitivity in the foot and lower limbs, which means you lose the ability to feel pain and distinguish hot or cold. It can also lead to less blood supply to your feet leading to poor circulation.
Loss of sensitivity means that you may not notice if you have a minor cut, sore or wound and poor circulation means if you do get a cut or sore, it will take longer to heal and open wounds are more likely to become infected. This combination is why there is an increase in risk of amputation for those who are diabetic. Regular podiatry appointments are the best way to look after your foot health.
Heart: High blood sugar levels can also cause problems to your blood vessels which can sometimes lead to serious problems such as heart attacks and strokes.
Kidneys: High blood sugar levels creates more difficulty for the kidneys to clear waste. This may lead to Diabetic Nephropathy, the deterioration of the kidneys.
HOW CAN DIABETES BE TREATED?
There is currently no cure for diabetes, therefore, the best way to deal with diabetes is to get it properly managed and controlled. If you are diagnosed with type 1 diabetes, you must either inject or pump insulin into body to treat your diabetes. If you have type 2 diabetes, you may also have to use insulin, however, it can be managed through diet and lifestyle changes.
HOW CAN YOU TEST FOR DIABETES?
An instant HbA1c test can confirm if you’re within the recommended range, or are considered pre-diabetic or confirm that you have diabetes. Using a small blood sample it will measure how well your blood sugar has been controlled over the last 3 months and provide a numerical reading.
As the HbA1c test provides 3-months insight, it is an important blood test for diagnosed diabetics. It provides a good indication of how well they are managing their diabetes..
Many people are more familiar with the glucose blood test – it measures the concentration of glucose molecules in your blood at a single point in time. The amount of glucose in your blood could also indicate whether you could be diabetic or not. People with diabetes can also use this test to manage their condition on a daily basis alongside regular HbA1C testing.
You can book an instant HbA1C test online at a cost of £59.50.
WHAT ARE THE SYMPTOMS?
When it comes to diabetes the symptoms are not always obvious and can often go unnoticed for long periods of time before being diagnosed.
The most common symptoms include:
- Feeling constantly thirsty or dehydrated
- Unintentional loss of weight and increased appetite (type 1)
- Vision begins to blur
- Numbness in your hands or feet (type 2)
- Fatigue
- Urinating more frequently
WHO IS AT RISK?
In the UK, type 2 diabetes is the most common type of diabetes, affecting over 90% of sufferers. The symptoms of diabetes are often mild, therefore, it’s important to be aware of the risk factors that could make you more susceptible to diabetes in the future.
According to Diabetes UK, type 2 diabetes is twice more likely in people of African descent in comparison to people of European descent and six times more likely in South Asian communities, making them a high risk category in developing diabetes. Additionally, people of African – Caribbean and South Asian descent are also at risk of type 2 diabetes much earlier, usually over the age of 25. On the other hand, for Europeans the risk increases when over the age of 40. Other factors contributing to diabetes include being overweight, high blood pressure and genetics.
Other general risk factors include:
- Having high blood pressure
- Carrying extra weight around your middle
- Smoking
- Polycystic Ovary Syndrome (PCOS) sufferers
- Those with a sedentary lifestyle
- Drinking too much alcohol
- Those with disturbed sleep – this includes those who do not get enough sleep and those whose sleep too much
If you have symptoms of diabetes or general concerns about your diabetic risk, you can book a GP appointment to discuss in more detail.
Alternatively, you can book in for an instant HbA1c test with a nurse.
With monkeypox cases being recorded in over 20 countries across the globe, people are becoming increasingly concerned about its spread and transmission.
Following 2 years of the Covid-19 pandemic, this outbreak has reignited the public’s fear and uncertainty of infectious diseases.
Whilst the media coverage of the monkeypox outbreak is alarming, we would like to reassure our patients that as it stands, the risk is still very minimal and vaccination is not advised as a precautionary measure. Whilst vaccines will undoubtedly be a key part of containing the outbreak, for now, only people who may have been exposed are being offered vaccination.
Our Medical Director & Travel Medicine Specialist, Dr Richard Dawood explains;
“Lots of people have been getting in touch with us to ask about a monkeypox vaccination, but this is not available privately. It is currently only being offered to anyone identified as a direct, close contact of a confirmed case deemed to be at sufficient risk.
The current outbreak does, however, highlight the need to think about your vaccine protection more generally, whether for travel or simply to protect your health and well-being, taking advantage of the best vaccines currently available.”
In a more general sense, it is never too late to catch up on childhood vaccinations, incomplete vaccination courses or any required boosters.
Your immune system naturally decreases with age and certain diseases are also more prevalent in older adults so there may be new vaccinations which are now suitable for you to consider for preventable diseases. Some health conditions can also weaken the body’s immune response, making you more vulnerable to infectious diseases, complications and hospitalisation. Therefore, it is important to ask your GP which vaccinations would be suitable for keeping you healthy.
– For more information on wellness vaccinations.
If you are travelling soon and haven’t had a travel consultation with a travel nurse, perhaps it is time to consider one. Travel nurses are experts in travel health and will advise which travel vaccinations & medications you should consider based on the risk of where you are travelling to and your itinerary once there.
– For more information on travel consultations.
To conclude, we’d like to dismiss a couple of dangerous myths about monkeypox that are unnecessarily scaremongering the public:
Myth 1: Monkeypox is as contagious as COVID-19 or smallpox
Fact: Monkeypox is far less contagious compared to smallpox, measles, or COVID-19.Myth 2: Monkeypox is a new virus.
Fact: No, the monkeypox virus is not a novel virus. It’s a known virus and is generally seen in central and western African countries as localised outbreaks.In summary, we, like the rest of the medical field, will be keeping a close eye on the progression of the Monkeypox outbreak and should our advice change based on new information, we will update this statement accordingly.
For more information on Monkeypox.
Chronic kidney disease (CKD) is a long-term condition where the kidneys don’t work as well as they should. In some circumstances, the loss of kidney function can get progressively worse over time but CKD only reaches an advanced stage in a small proportion of people. Although the damage is irreparable, sometimes if changes are made, CKD can be halted with no further damage occurring.
Chronic Kidney disease (CKD) is divided into 5 stages.
Stage 1 is the earliest stage whereby tests have indicated some level of kidney damage. It is important not to ignore a stage 1 diagnosis as this is the time to take action and make lifestyle changes so that the condition does not worsen. With every increase in stage, more kidney damage has been detected up until the last stage, stage 5. Stage 5 means the kidneys have lost almost all their function and it will be time for thinking about dialysis or a transplant.
What to do if your recent blood test shows a reduced kidney function.
Don’t panic, absorb the diagnosis and understand this doesn’t definitively mean your kidneys will stop working altogether. CKD should not be ignored as it can get worse over time but with careful monitoring and management it can be maintained and you can live long fulfilling lives without being unduly affected by the condition.
It is important to review your lifestyle and in particular, your diet. With early stage CKD (stages 1-3) it is paramount to be as healthy as possible and have a healthy balanced diet.
What do I mean by a healthy balanced diet?
This includes:
- Consistently eating freshly cooked food for every meal
- Limiting your intake of processed foods and avoid highly-processed foods
- Reducing your daily salt intake
- Having considered balanced meals – your lunch and dinner meals should contain proteins, carbohydrates and vegetables. Your portion size will depend on your weight and if you have diabetes
- Ensuring you have a minimum of 2-3 portions of fruits and vegetables each and every day
- Increasing your intake of plant based proteins such as beans, lentils, tofu, soya, seitan
- Drinking lots of water to remain well hydrated (ensure your urine runs clear)
- Being as active as physically possible for you
- Avoiding non-steroidal medicines such as ibuprofen, naproxen etc.
What is a renal diet?
You may have heard of the term, renal diet. The term is used quite widely amongst those who have CKD, but personally, I am not a fan of this term. It doesn’t really mean much and can often be misused. People often think it means a diet of low protein, low salt, low potassium and low phosphate – which is pretty hard to do all at once and not always necessary.
People newly diagnosed with CKD in particular often restrict their diet in a panic unnecessarily and in combination with online resources not being clear enough, this can cause a lot of confusion.
My advice would be to seek guidance from someone like myself, a dietician who can look at your lifestyle and individual health and work out a personalised diet plan. This will be much more achievable and as well as not feeling so overwhelming, you’ll only have to limit the foods you absolutely need to.
How do you monitor CKD?
The best way to monitor CKD is to have regular tests, either blood or urine. How often you require testing will be dictated by the stage of CKD. Your GP will determine what is best for you and it is best to ask them any medical and testing questions rather than your dietician who will focus solely on your lifestyle and diet.
______________
Ruth Kander is a kidney-specialist dietitian, to book an appointment with her please click here.
Women today lead incredibly busy lives. They run and organise homes and build successful careers, usually all whilst taking on the majority share of caring for their children and often their older relatives. It is therefore not uncommon for women to have little or no time to look after themselves, their health included.
In addition to not making time to prioritise their health, it seems that when women do put their health first and seek medical advice, they are less likely to feel heard and supported in comparison to their male counterparts.
A recent survey by The Department of Health and Social Care found that “more than 4 in 5 (84%) women they surveyed had experienced times when they (or the woman they had in mind) were not listened to by healthcare professionals.”
Based on the data they collected, ‘not being listened to’ appears to be present at all stages of the healthcare pathway. Specifically, many women told them:
- their symptoms were not taken seriously and/or dismissed upon first contact with GPs and other health professionals
- they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years
- if they did secure a diagnosis, there were limited opportunities to discuss or ask questions about treatment options and their preferences were often ignored
Many women recalled their symptoms being dismissed upon first contact with GPs and other professionals; women felt they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years; and post-diagnosis, discussions about treatment options were often limited, and some said their preferences were ignored.
To make matters worse, there is some evidence that due to historical clinical trials being disproportionately male-orientated there is much less research into women-only health concerns and assumptions have been made that similar medical treatments will work for both sexes. The top reasons for the under-representation of women in trials were the belief that hormone fluctuations could influence results and concerns that fertility could be affected. A widely accepted negative repercussion, amongst others, being that women are much more likely to experience adverse side effects of medications because drug dosages have historically been based on clinical trials conducted on men.
A combination of these factors may explain why there is a gender gap in health outcomes, with women experiencing poorer health outcomes in comparison to men. We strongly believe in equality and ensuring health is a top priority for all.
Therefore, here are the top health symptoms women should never ignore:
1) Any change in bowel habit and/ or urination
This includes blood in the stools, unexplained persistent abdominal pain, weight loss, lumps around the anus, lack of appetite, blood in the urine or increased frequency of urination. These are all reasons for seeing your doctor ASAP as these symptoms could be due to bowel, bladder or ovarian cancer. All patients should have an annual faecal occult blood (FOB) test to exclude bowel cancer, which has increased in incidence in the UK for reasons unknown. Or if you are looking for a more in-depth investigation, you should request a colonoscopy which entails looking at the bowel with a colonoscopy. This is the gold standard, but an FOB is the next best thing and far less invasive as a first investigative option. It takes no time at all and is a good preventative check.
2) Any changes to the breast.
Any breast lumps, skin changes, nipple discharge, nipple changes or pain in the breast must be checked ASAP. Breast cancer is the most common type of cancer in the UK and often can present insidiously. Get to know what your breast feels like so that any subtle changes can be detected as early as possible.
3) Skin lesions that do not heal.
Any scab on the skin which does not heal, especially around the eyes, nose, ears and face should be checked. All these areas are the most sun-exposed, and, as such, are more at risk of skin cancer. If these lesions are picked up and treated early, scarring is minimal, but if left, then disfiguring scars and skin grafts may be necessary.
4) Bleeding after the menopause.
If you experience any bleeding after 1-year of your last menstrual period, you must visit your GP for further investigation. Bleeding after the menopause is not common and could be an indicator of cancer of the uterus, or the cervix. They will usually opt for a biopsy of the uterine lining to exclude both – don’t worry, this doesn’t hurt.
5) Always have regular cervical screens.
Most people don’t find cervical screens painful, although they can feel somewhat uncomfortable. If you are concerned about the pain or you have previously found the procedure painful with the NHS, you can opt to book a private appointment. It is important that you don’t miss your appointment.
6) Bleeding between periods.
At any age, you should never ignore bleeding between periods or after intercourse, as this can be a sign of cervical or uterine cancer. Whilst cervical cancer is monitored by regular screening, it is important to still get bleeding between periods checked out following a normal smear result. Cancer of the endometrium is becoming increasingly common in women who have not had children.
7) A persistent cough.
Regardless of gender, you should get a persistent cough checked out by your doctor, especially if you are coughing up discoloured sputum or blood.
8) Any unexplained changes to your body.
Any new indigestion, shortness of breath on exertion, neck or left arm pain requires follow up ASAP. Make sure a GP examines your chest and makes the appropriate investigations.
The same applies to calf pain or any pain in the chest. By taking a full history, examining you and doing quick and easy investigations, worrying conditions can be excluded, such as a pulmonary embolism or a heart attack.
Some recent examples of cases where other healthcare providers have failed our new female patients:
1) We saw a 36 year old who had not had a cervical screening for 5-years because the last one was so painful. The NHS advises a screening every 3-years but we advise yearly screenings to ensure any abnormalities are found as early as possible. 5-years is far too long!
2) We saw a woman who had a suspicious lump at her anal margin, which her usual GP had told her was part of her bladder. She wanted a second opinion because it had grown in size and was now painful. The patient was referred for an urgent assessment to exclude cancer.
3) We saw an 88 year old patient who was disfigured by a large basal cell carcinoma on her forehead, about which she was embarrassed. The patient had been seen by a dermatologist who had frightened her about having the lesion removed by saying she might not survive an anaesthetic. The patient wished that she had taken the risk and asked to be referred back, as the skin lesion was disfiguring and ruining her quality of life.
** The outcomes of these patients are yet unknown, but they are all certainly serious health concerns that should have been properly addressed long before now.
We want to encourage women to take ownership over their health and be assertive when they feel that something has changed from our normal. If they feel like they are not being taken seriously or not being heard, they should seek a second opinion.
If you cannot get an appointment with your usual GP or through the NHS, rather than waiting for weeks and worrying about what it could be, make an appointment with a private GP who can usually see you on the same day!
Put your mind at ease with private healthcare.
Ageing is an inevitable part of living. As we age, many physical and psychological changes affect our overall health and these vary from person to person.
The general myth is that as you age, you become more fragile and that this is unavoidable. This is most certainly not the case. There are always things we can do to help keep healthy in our older years and these changes can slow down or even prevent certain health conditions from developing.
The term “fragile” is defined as not “strong or sturdy; delicate and vulnerable” and is most often used to describe older ladies. One particular age-related health issue that supports this description would be osteoporosis.
Osteoporosis is a degenerative disease that weakens and thins the bones which makes them fragile and more likely to break and is becoming increasingly common. It is much more prevalent in women than men due to the menopause directly affecting hormone balances and this directly affects bone density. It is important to prevent osteoporosis as we age as 75% of fractures due to osteoporosis occur in people aged 65 and over.
There are several things you can do to help prevent osteoporosis:
1) Do regular, weight bearing physical activity.
The lack of regular exercise will result in loss of bone and muscle, so adults who are inactive are more likely to have a hip fracture than those who are more active. Adults should aim to do at least two and a half hours of moderate-intensity exercise every week. Weight bearing and resistance training are a particularly great way of improving bone density and helping to prevent osteoporosis.
2) Eat plenty of calcium and Vitamin D containing foods.
Your diet is very important and the nutrients we get from the food we consume will affect how strong our body is. Eat plenty of dairy, seeds, eggs, oily fish, protein, fruit and vegetables. Additionally, try to get at least 15-minutes of sun exposure per day to increase your Vitamin D intake. As we know in the UK, such sun exposure is not always possible during the winter months and, if this is the case, taking a daily Vitamin D supplement is advised.
3) Maintain a healthy weight.
As you get older, you start to lose lean body mass like muscle and bone density and this can start to happen yearly from the age of 30. Being underweight weakens your bones so it is important to keep your weight in a healthy range. A good indication, although not exact, is your BMI. For most adults, a healthy BMI range is between 18.5 and 24.9, so try not to let your BMI fall below 19.
Those who suffer from eating disorders such as anorexia and bulimia are at a higher risk of fragility due to the conditions causing further bone density loss. This can happen to anorexic and bulimic sufferers of all ages.
Older people should aim to consume a varied diet, consisting of enough calories for maintaining a healthy weight.
4) Limit your consumption of alcohol.
We’d recommend that you drink no more than a maximum of 2 units of alcohol per day. Any more than this has been demonstrated to increase the risk of bone fracture. Alcohol abuse has detrimental effects on bone health and increases a person’s risk of developing osteoporosis.
5) Stop smoking and definitely don’t start!
Smoking is a known risk factor for osteoporosis as it increases bone mass loss. In fact, smoking doubles the risk of hip fracture.
Generally, being healthy is the key to avoiding fragility and in particular preventing osteoporosis as we age. Having an annual health medical can highlight any areas of concern. They can monitor the progression of any pre-existing health issues, as well as detect arising conditions in the early stages. You can book your annual medical online
In addition to making healthy lifestyle choices, it is also important to book a doctor’s appointment should you notice any changes to your health. The sooner a health concern is addressed, the easier it is to treat. You can book a GP appointment online.
Weight loss has become a thriving industry and we’re bombarded constantly with unhealthy FAD diets, weight loss programmes, influencers selling teas and pills all promising to help us lose weight. Many of these are promoting quick fixes which are not advised by doctors or dieticians. It can be really hard to know what information to trust. To help navigate the sea of information (and misinformation!) surrounding weight loss, we have asked one of our GPs, Dr Belinda Griffiths, and our dietitian, Ruth Kander, their advice on how to lose weight safely and successfully.
Firstly, it is important to note that weight loss should be consistent and gradual as it can be dangerous to lose too much weight too quickly. Dr Griffiths suggests that “a safe weight loss is 1-2 lbs or 0.5-1kg per week… Greater weight loss than this per week can lead to malnutrition, exhaustion, increased risk of gout and gallstones.” There is also an increased risk of developing an unhealthy relationship with food which, in extreme circumstances, could lead to eating disorders.
Ruth added, “Losing weight gradually and at a healthy rate is key.” Remember, it’s all about consistency! Perseverance will amount to healthy lifestyle changes which will allow you to achieve your weight loss goal.
Don’t underestimate diet
Both Dr Griffiths and Ruth agree that diet is the most important factor when it comes to weight loss. As Ruth explains; “having a healthy balanced diet that is lower in calories than our body uses is a good way to start the weight loss journey. If we don’t reduce calorie intake, one won’t lose weight:.” – this is known as being in a calorie deficit. The amount of calories that will result in weight loss will vary from person to person and depend on the amount of exercise the individual does. In order to lose weight, you will need to burn more calories than are consumed and therefore restricting your calorie intake is the simplest way of losing weight.
Foods to focus on
Ruth recommends that “people should focus on a variety of foods when trying to lose weight”. While Dr Griffiths suggests, “focusing on a range of lean proteins (including meat and fish), vegetables, high fibre foods (such as quinoa, bran flakes etc) and fruit in moderation”. Vegetarians can substitute in lentils, nuts, beans and tofu instead of meat and fish. In general, high calorie foods such as fried food, cakes, biscuits, chocolate and sugary drinks should be avoided.
Let’s get physical!
Although weight loss is still achievable without much exercise, incorporating exercise into your lifestyle will not only aid weight loss, but will generally improve your overall health. Any exercise is better than none whether it be tennis, swimming, or even walking, “whatever you are capable of, just do it!” is Dr Griffiths advice. Ideally, a combination of exercise is best for weight loss – this includes cardio / fat burning and resistance or weight training. Get those steps in! An easy way to incorporate more exercise into your daily routine is by aiming to walk at least 10,000 steps per day. This easy change can make a big difference and remember, as Dr Griffiths says “the more exercise you do, the greater calories are burned” – it’s as simple as that!
Don’t forget about NEAT movements!
NEAT (or Non-exercise activity thermogenesis) movement refers to the physical movement we do day-to-day that isn’t necessarily planned exercise and “encompasses the energy that we expend by simply living”.This includes the calories we burn breathing, eating, sleeping etc. Dr Griffiths suggests that “you can increase NEAT movement easily in your everyday life by making simple changes such as taking the stairs rather than the lift, by standing rather than sitting, by walking instead of taking the train/ bus/ tube or even by carrying bags rather than having items delivered”. It all adds up! These simple swaps will increase the number of calories you burn and help facilitate weight loss.
What to do when you plateau
The first stint of weight loss can make it seem a little too easy as you tend to lose weight more easily in the beginning, but a common issue lots of people face is when weight loss reaches a plateau. This is where you stop losing weight to the same extent you were before, or stop losing weight for a period of time. This can feel disheartening and more often than not, people tend to give up at this stage. Dr Griffiths states at this point “it is a case of persevering with calorie restriction and regular exercise and gradually weight loss will resume.” If it doesn’t, Ruth suggests “ looking at what you’re eating to see if anything has slipped”. She states “maybe you’re not taking into consideration extra calories here and there” but they all add up. See if there are any areas of your diet where you could be a little stricter, or consider starting or upping your exercise.
Sleep and Stress
A good night’s sleep and keeping your stress levels down will be your friend when it comes to weight loss. “In order to lose weight, you need to be in the correct frame of mind and life circumstances” says Ruth. Research has shown that you tend to eat more and make poorer food choices, including seeking comfort food, when you are sleep deprived. This is because not getting enough sleep “disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite” says Dr Griffiths.
Stress can also play a part in weight loss as Dr Griffiths explains that “stress increases cortisol levels which increases gastric acid output and makes you feel anxious and hungry”. Ruth adds “there is also a theory that being stressed can limit weight loss in terms of hormonal activity in the hypothalamic-pituitary axis which can lead to the release of hormones that can limit weight loss”. Keeping it simple, “to lose weight, good sleep and minimal stress would be ideal”.
Final thoughts
Trying to lose weight can seem complicated, confusing and difficult, but when you really break it down, the ingredients to losing weight successfully are actually very straightforward. If you stick to these simple rules and you are patient and consistent, the weight will come off and you will achieve your goals.
If you feel that you are doing everything right and you still aren’t losing weight, or are even putting weight on, there could be something else causing this. You may have an undiagnosed underlying medical condition and we’d advise you to visit your GP to make sure everything is well.
If you would like any extra support with your weight loss, why not book an appointment with Ruth. Or if you have any concerns over your health, please book an appointment with one of our GPs.
If you are feeling sad at the start of the year, don’t worry, you are not alone.
Although it comes around every year, we always seem to be caught off-guard by what has now commonly become known as “The January Blues”.
The January blues is another name for situational depression and is associated with the way we think and feel. Around this time of year, the weather is cold and gloomy, the days are shorter and the nights are longer, plus you may be experiencing post-Christmas exhaustion, debt and perhaps even dread going back to work.
Symptoms of the January blues are things such as low mood and sadness, lack of motivation, tiredness and low energy. These are all normal feelings, if temporary.
Most likely, your negative mood will be brought on by the anticlimax of reality after the exciting events of December & the New Year. Ever heard that old phrase, “don’t cry because it has ended, but smile because it happened”? Find comfort in knowing that you are absolutely not alone in feeling blue in January. In fact, many people in the UK feel especially down in January but the good news is that the January Blues are temporary and typically only last a couple of weeks. You don’t need to take any medication as your thoughts and feelings should naturally return to normal.
If it doesn’t and you are experiencing prolonged or worsening thoughts and feelings, you may actually have Seasonal Affective Disorder or SAD, which is different. SAD is clinical depression caused by a person’s biology. It is much longer-lasting, sometimes months on end and likely to occur every year in winter. You should see a doctor to discuss your symptoms as if you have SAD, a range of treatments are available to assist recovery. More information on SAD can be found here.
Remember, please be kind to yourself and know that you’re not alone.
For more information on our GP Services.
To book a GP appointment online, click here.
Most people experience fluctuations with their weight and it is common to gain weight naturally as we age. For the most part, diet changes, eating more or reducing exercise are the main causes for gaining weight. However, if a person gains weight in a short period of time for no reason, this could be the sign of an undiagnosed, underlying health condition. There are several conditions and circumstances that are known to cause weight gain, some of which can be serious and require medical attention.
Here are just some medical conditions which can cause sudden weight gain:
Polycystic ovary syndrome (PCOS)
This is a hormonal condition which affects the way a woman’s ovaries work. A common symptom of PCOS is weight gain, particularly around one’s middle. Weight gain is rarely the sole symptom, it is usually part of multiple symptoms including acne, excessive hair, irregular periods and/ or thinning hair. PCOS makes women less sensitive to insulin or cause insulin-resistance which can lead to weight gain and secondary conditions such as diabetes.
Hypothyroidism
A common cause of unexplained weight gain in men and women comes from having an underactive thyroid. This is because when a thyroid is underactive it doesn’t produce enough thyroid hormones, which in turn affects your metabolism, slowing it down. Hypothyroidism can be diagnosed with a thyroid function test and if diagnosed, it can be easily treated with a replacement hormonal tablets.
Cushing’s syndrome
This is a rare hormonal disorder which is caused by elevated levels of cortisol in the body. Cortisol is responsible for regulating metabolism and appetite, which means elevated levels can slow down your metabolism as well as increase hunger, both of which can cause weight gain.
Insomnia / chronic lack of sleep
Being sleep deprived can result in making poor food choices, including seeking unhealthy foods and eating more than usual. This is thought to be because a lack of sleep disrupts the hormones in the brain (Leptin and Ghrelin) that are responsible for appetite.
Medication
Certain medications affect metabolism which can cause weight gain and weight loss. Medications such as steroid medication can cause weight gain, bloating and swelling due to water retention.
Lipoedema
This is a problem caused by an issue with the lymphatic system that causes an abnormal build-up of fat in the legs and sometimes the arms. This usually results in the upper body being generally a much smaller size compared to the lower half of the body but typically affects both sides of the body equally. This condition can also be painful and cause tenderness or heaviness in the limbs. Lipoedema mainly affects women and it is rare in men.
Chronic stress, depression and/ or anxiety
Mental health issues can sometimes cause people to turn to food as a coping mechanism, often triggering compulsive eating behaviours. Additionally, higher cortisol levels are often found in people with depression which is known to increase appetite and the motivation to eat. Antidepressant medication can also increase hunger as they interfere with serotonin levels – a neurotransmitter that regulates appetite.
Menopause
Women going through the menopause often experience weight gain. Changing hormone levels affect the way the body stores fat and can cause women’s bodies to store, rather than burn, calories. Women also generally need less calories after the menopause, and so, if you do not adjust your calorie intake, you are likely to put on weight.
PMS
During PMS (premenstrual syndrome), progesterone levels surge and dip which are known to increase appetite (the cause of which are unknown). PMS can also cause weight gain as a result of water retention.
While many of these causes are rare, they are possible and anyone experiencing unexplained weight gain should visit their GP to rule out anything that may require medical care or treatment. It’s always best to be on the safe side! And if everything is normal, your GP can provide you with tips and advice on how to manage your weight gain.
If you are experiencing unexplained or sudden weight gain, or think you might be displaying symptoms of the conditions mentioned above, please book a GP appointment today.
Sleep is one of our greatest allies when it comes to health and wellbeing. It is associated with a number of health benefits which can have a huge positive impact on our daily lives.
Conversely, a lack of sleep can be detrimental – research has even found that not getting enough sleep can negatively impact some aspects of brain function to a similar degree as alcohol intoxication!
Dr Belinda Griffiths discusses some of the mental and physical health benefits of getting a good night’s sleep.
Immune System
During sleep, your body releases cytokines, which are essential for the regulation of the immune system. Cytokines are required in increased amounts when you are attacked by a pathogen (when you’re ill) or under stress. The level of cytokines increases during sleep, and therefore lack of sleep hinders the body’s ability to fight infections. This is also the reason why the body tends to sleep more while suffering from an infection.
Weight Control
When you’re well-rested, you’re less hungry. Being sleep deprived disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite.
With those out of balance, your resistance to the temptation of unhealthy foods goes way down. And when you’re tired, you’re less likely to want to get up and move your body. Together, it’s a recipe for putting on the pounds!
Athletic Achievement
If your sport requires quick bursts of energy, like wrestling or weightlifting, sleep loss may not affect you as much as endurance sports like running, swimming, and biking. But you’re not doing yourself any favours. Besides robbing you of your energy and time for muscle repair, lack of sleep saps your motivation, which is what gets you across the finish line. You’ll face a harder mental and physical challenge – and see slower reaction times. Proper rest sets you up for your best performance.
Memory
When you’re tired, you can have difficulty recalling information. That’s because sleep plays a big part in both learning and memory. Without sufficient sleep, the brain finds it difficult to focus and take in new information in the first place and then doesn’t have enough time to properly store information as short-term memories. Sleep helps enable you to retain memories and store information.
Sleep also allows for your mind to rest, repair and rebuild, the same way it does for your body. As you sleep, your brain begins to organise and process all the information you’ve taken in during the day. It converts these short-term memories into long-term memories – this helps you to learn.
Concentration
Not sleeping properly can mean that both your body and brain don’t function properly the next day. It can impair your attention span, concentration, strategic thinking, risk assessment, reaction times and problem-solving skills. This is particularly important if you have a big decision to make, are driving, or are operating heavy machinery. So, getting plenty of sleep can help you stay sharp and focused all day long.
Mood
Another thing your brain does while you sleep is process your emotions. Your mind needs this time in order to recognise and react in the right way. When you cut that short, you tend to have more negative emotional reactions and fewer positive ones. Lack of sleep can cause bad temper and anxiety, so the better you sleep, the better your ability to stay calm, controlled and reasonable.
Chronic lack of sleep can also raise your chance of having a mood disorder. One large study found that people with insomnia were five times more likely to develop depression, and the odds of having anxiety or panic disorders are even greater.
A refreshing slumber helps you hit the reset button on a bad day, improve your outlook on life, and be better prepared to meet the challenges of the next day.
Heart Health
While you sleep, your blood pressure goes down giving your heart and blood vessels a bit of a rest. The less sleep you get, the longer your blood pressure stays up during a 24-hour cycle. High blood pressure can lead to heart disease and strokes. Therefore, it is important to keep your blood pressure down.
Pain Threshold
Poor sleep and pain mutually reinforce each other. Sleep deprivation increases pain sensitivity and reduces pain tolerance. Therefore, something will feel more painful when you’re tired.
It is clear that sleep is an essential part of helping us stay physically and mentally healthy. What better excuse to have a few extra hours of sleep a day!
If have any concerns about your health, book a GP appointment today.
The health of both our planet and its people is, without doubt, one of the most important issues of our time. Maintaining healthy wellbeing has been in the public eye for some time now, particularly the topic of how to achieve good mental health. Chinese medical thought and acupuncture treatment can help us understand what we can do to help ourselves to achieve and maintain good health. Its teachings encourage us to inhabit our body, to connect to and to nourish our physical self and the physical world around us. This physical basis provides the root of our mental and emotional well-being.
A holistic treatment
Where Western Scientific Medicine has gone down the microscope to discover the minutiae workings of the human body (cells, biochemicals, genes), the understandings of Chinese Medicine, developed over thousands of years, have focused on how the body systems work together. It observes a person in their environment, their lifestyle, their posture… to understand the causes of ill-health, and the symptoms that arise to alert us to this. The whole body-mind is considered, and treated, to bring us back to good health and well-being.
A leap of faith for our Western minds
Acupuncture is a leap of faith for our Western minds. The concepts on which it is based do not exist in Western thought. You can’t cut open the body and find the meridians which form the energetic framework of the human body, or the Qi (pronounced ‘chee’, meaning energy) which flows through this network to motivate our physiological processes. Similarly, you can’t cut open a light bulb and find electricity. Likewise, you cannot cut open a computer and find cyberspace. It doesn’t mean that these things don’t exist. Proof of their existence lies in their application and the same is true of acupuncture treatment. Only through experiencing acupuncture for yourself will you be able to judge its true value.
Acupuncture helps reduce stress
Acupuncture is often described as incredibly relaxing, regardless of what a person seeks treatment for. Furthermore, most patients report an improvement in energy levels, sleep and a feeling of general well-being.
Acupuncture helps calm the nervous system. As a result, it helps switch off the ‘Fight-Flight’ stress response. Fuelled by adrenaline to keep us alert and primed for action, the stress response helps us to achieve. It is a useful tool for success. If the stress reaction is prolonged and not switched off, problems start to arise.
Heart rate increases, breathing quickens, muscles tighten, blood pressure rises .. it is perhaps not surprising that stress-related ailments are estimated to account for 75-90% of all doctor’s visits. By calming the body and promoting parasympathetic activity, Acupuncture helps improve circulation and reduce general muscle tension. This enhances all body functions not concerned with immediate survival – immunity, digestion, fertility, rest, recovery, repair. Generally speaking, the results note an overall feeling of relaxation and well-being.
Acupuncture helps manage day-to-day ailments
Our Acupuncturist, Diane, has 25 years experience in Chinese Medicine. She treats a wide variety of day-to-day ailments. Including headaches, IBS, anxiety, infertility. As well as the musculoskeletal pain, which acupuncture is most famous for. Why not book an appointment today to see how acupuncture can help you improve your health and well-being?
If you think you could benefit from acupuncture, you can book your appointment online.
By Diane Timewell | Acupuncturist | July 2019
THE WORLD HEALTH ORGANISATION (WHO), HAS REPORTED THAT POPULATION EXPOSURE TO HEAT IS INCREASING DUE TO CLIMATE CHANGE.
The WHO states, ‘global temperatures and the frequency and intensity of heatwaves will rise in the 21st century as a result of climate change’. Extended periods of heat exposure during the day and night time can increase the amount of physiological stress on the human body.’
The stress caused by heat exposure exacerbates the top causes of death globally. This includes respiratory and cardiovascular diseases, diabetes mellitus and renal disease.
They go on to state, ‘Exposure to excessive heat has wide-ranging physiological impacts for all humans, often amplifying existing conditions and resulting in premature death and disability.’
With the temperature said to continue rising, the WHO also states, ‘Awareness remains insufficient of the health risks posed by heatwaves and prolonged exposure to increased temperatures.’
So, who is most affected by heat exposure and how will it impact your health?
Who is affected?
Rising temperatures affect the whole population. However, some populations are more vulnerable to exposure to excessive heat. Those include:
- Elderly people
- Infants and children
- Pregnant women
- Outdoor and manual workers
- Athletes
- Poorer communities
How does heat impact health?
With rapid increases in external temperatures, the body will struggle to regulate our internal temperatures. The knock-on effect of this can result in a number of heat-related illnesses such as heat cramps, heat exhaustion, heatstroke, and hyperthermia. Reported small differences in the seasonal changes have been reported to have increased the number of heat-related illness and even death. Rising temperatures can also worsen chronic conditions such as cardiovascular, respiratory, and cerebrovascular disease and diabetes-related conditions.
What actions can you take to stay cool?
- Aim to keep your living space cool. WHO suggests ‘below 32 °C during the day and 24 °C during the night’
- If it is safe, open your windows at night time to cool your living space.
- Stay out of the heat by staying in the shade and avoiding going outside during the hottest part of the day.
- Take cool showers and wear loose-fitting clothing.
- Drink regularly and avoid alcohol and caffeine.
- Check on vulnerable family members who may be affected by the heat.
What to do if someone shows signs of a heat emergency?
It is extremely important to know what to do when someone is showing signs of heat illness. Everyone should know how to respond to heat emergencies, this can be learnt in first aid courses.
If one of your family members or someone you assist is showing signs of hot dry skin and delirium, convulsions and/or unconsciousness, call a doctor/ambulance immediately.
Whilst you are waiting for help to arrive place them in a cool place in a horizontal position and elevate their legs. It is now important to initiate external cooling.
This can be done by:
- Removing clothing
- Placing cold packs on the neck and groin
- Spraying cool water on their skin
- Fanning them
- If they are unconscious, place them on their side
If you or someone you are with is displaying mild signs of heat illness that is not considered an emergency, you might want to consider a same-day GP appointment. You can book an appointment online.
How to Cope During a Heatwave
The UK is currently experiencing a heatwave with temperatures rising to 35 degrees in some parts of the country this week. While sunshine is welcome and the vitamin D is much needed, too much heat can lead to illness. To avoid any heat-related sickness, make sure you are well-prepared! Follow Fleet Street Clinic’s tips to help keep safe during the hot weather.
Risks During the Heat:
- Exposure to such high temperatures increases sweating, and results in loss of fluid and electrolytes causing rapid dehydration. This can result in heat exhaustion or heatstroke which can be life threatening if not dealt with promptly.
- The highest risk groups are the elderly, babies, children and those with pre-existing medical conditions.
- If you engage in strenuous physical activity this will increase the risk of illness related to the heat.
Top 7 Tips For Beating the Heat
- Seek shelter and shade during the middle of the day (11am -3pm).
- If you are outside, ensure you protect your skin against the sun with a high factor sun cream, hat and sunglasses.
- Wear loose fitting, light-weight and light colour clothing.
- Keep hydrated by drinking plenty of fluids and eating food with a high water content (such as fruit).
- Ensure you are taking in sufficient salt in your diet (sweating leads to electrolyte and salt depletion).
- Avoid caffeine and alcohol, which can worsen heat-related illness.
- Heat stroke can be a life-threatening emergency and medical help should be sought.
About Fleet Street Clinic
Fleet Street Clinic is an independent healthcare practice in London. For more advice or to book an appointment with our expert medical team, you can book online.
Glastonbury has been going for over 50 years and is back this year following a fallow year last year.
Whether you are a festival first-timer or a seasoned Glastonbury veteran, make sure you follow our top tips on how to stay healthy during festival season.
First things first, facilities…
A major part of festival fun is the back to nature approach to living, so do expect basic living facilities. Facilities at festivals are confined to porta-loos, long drops and communal showers; a perfect breeding ground for bugs. Dodge the diarrhoea by following some simple rules. Wash your hands where possible, especially before eating and always after the toilet. If running water isn’t available, use hand wipes or hand sanitiser. Pack your own pocket-size alcohol hand gel for when you are on the go.
The Vaccines…
Don’t be fooled into thinking vaccinations are only for those far-flung destinations. Glastonbury is the largest greenfield festival in the world and over the course of a week, home to over 175,000 people. Crowded spaces and shared living areas increase the risk of infectious diseases spreading. Many of which are entirely vaccine preventable. Measles and mumps cases have been on the rise in the UK, so festival goers should check they have received at least 2 doses of the MMR vaccination to ensure they are protected. If there is any doubt you can get immunity tested to put your mind at ease. Young adults and children can also be particularly vulnerable to meningitis, so if you are in this group, make sure that you have also received the recommended Meningitis ACWY vaccination.
You can find more information on all our vaccinations here.
Eat, drink and be merry…
It is estimated that an average festival goer burns around 9,000 calories and walks over 15 miles. Make sure you fuel your festival by eating plenty, especially if you are drinking alcohol. Keep hydrated and ensure you drink plenty of water to prevent dehydration, especially on those (potentially) hot days.
Come rain or shine…
Glastonbury has seen it all: heatwaves, rain, floods, cloudless skies. The Great British weather is never predictable and exposure to extreme weather can cause anything from hypothermia to heat stroke. Be prepared for all eventualities. Take warm waterproof clothes that will dry quickly in case of wet weather. Pack cool, light coloured clothing to help you keep cool in the sun. Pack a hat and some good suncream and make sure you wear it! Shady areas are few and far between if you are centre stage for the day, and without sun protection you could end up with sunburn, or worse, heat stroke. You can lean more about staying safe in the heat here.
STI’s
Don’t run the risk of sexually transmitted infections if you decide to go beyond social intercourse. The best way to prevent infections such as chlamydia and gonorrhoea is to use condoms. Some STI’s can take several weeks to present themselves, and in some cases are asymptomatic (display no symptoms at all). It is quick and easy to get checked for STI’s, so if you have any concerns when the festival is over, make sure you get tested.
You can book appointments for all our services online.
What is HPV?
Human Papillomavirus, or HPV, is the name of a group of viruses with around 200 different types, that is most commonly passed on via genital contact.
Although HPV is highly common, 90% of HPV infections go away by themselves and do not cause any harm. Most people with HPV never develop symptoms or health problems.
However, it is possible for HPV infections to persist and cause cellular change in your body. This can lead to:
- Cancer of the cervix, vulva, and vagina in women
- Precancerous lesions in men and women
- Genital warts in men and women
- Head and neck cancers in men and women
HPV vaccines have a well-established role in preventing cervical cancers as well as these other aforementioned conditions.
Who Should Be Vaccinated against HPV?
In theory, HPV vaccines are best given to young people before they become sexually active, and therefore before they can be exposed to HPV.
Individuals who are already sexually active might also benefit as they may not have yet acquired all of the HPV strains covered by the vaccine. Patients aged under 16 can only be vaccinated with their parents present.
Why Boys should receive the HPV Vaccine
- About 15% of UK girls who are eligible for vaccination are currently not receiving both doses. This figure is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries which have no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high: treating anogenital warts alone in the UK is estimated to cost £58 million a year, while the additional cost of vaccinating boys has been estimated to cost about £20 million a year
Source: HPV Action
To book an HPV vaccination for yourself or your child, you can book an appointment online. Or find out more information about HPV here.
Sepsis Signs:
World Sepsis Day – 13 September
Sepsis is a global health crisis and affects 27 to 30 million people every year. Out of those affected, 7 to 9 million dies. That’s one death every 3.5 seconds.
Sometimes called the silent killer, Sepsis is a bacterial infection of the blood which can become life-threatening. It is very hard to detect in the early stages, with symptoms similar to many other conditions and illnesses. In the UK alone, around 37,000 people die from sepsis each year.
Thankfully, due to public awareness increasing due to medical bodies and health campaigns, sepsis is being talked about more. As a result, parents and doctors have the condition forefront-of-their mind. The condition is treatable with early recognition and care.
Causes of Sepsis
Bacterial infections are the most common causes of Sepsis. However, Sepsis can also be caused by infections like seasonal influenza viruses, dengue viruses, and highly transmissible pathogens.
Children under 1, the elderly and those with chronic diseases and a weakened immune system are most at risk of sepsis.
Symptoms of Sepsis
Sepsis can display in a variety of ways including:
-
Slurred speech or confusion
-
Extreme shivering or muscle pain or fever
-
Passing no urine all-day
-
Severe breathlessness
-
It feels like you’re going to die
-
Skin mottled or discoloured
If someone is ill and is getting progressively worse with two or more of the above symptoms, then it is advised for you to go to A & E without delay.
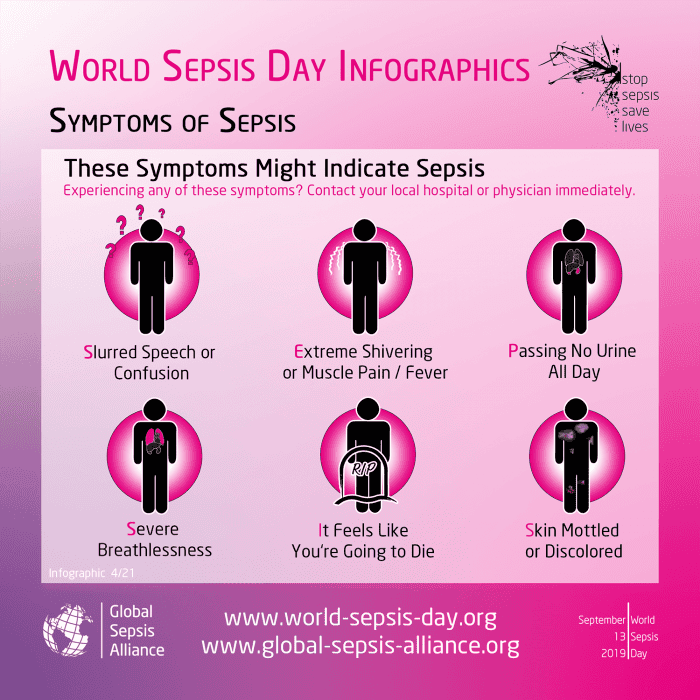
Preventing Sepsis
Preventing infection in the first place is the best way to prevent Sepsis from occurring.
This can be done by:
- Vaccinations – protect yourself from diseases which if serious, could lead to Sepsis.
- Hand Hygiene – reduce the spread of diseases and infections.
- Safe Childbirth – reducing infection to the mother and baby.
- Awareness of Sepsis– knowing the causes and symptoms can save lives.
If you think you are experiencing symptoms of sepsis, you should call 111 as you may require immediate medial attention.
For general GP health checks or vaccinations, you can book an appointment online.
So you’re back to work and the tree’s on its way back to the loft. Time to come through on all the New Year’s resolution bravado. Here are a few tips about how to do just that.
Create a plan
Decide what it is you’re wanting to achieve and tailor your program towards it. Do you want to lose weight? Get fitter? Tone up? All three? Don’t just choose the new fitness regime trend, think what you enjoy to do and go with that! You stand much more chance of continuing if you do. Identify times of day when you can exercise and which days you will do it. It’s much harder to stick to a regime that is just squeezed in when and if you have the time (not to mention inclination!)
Determine your readiness
Make sure you are mentally and physically ready to start, and more importantly ready to stick to, a regime. Check with your GP if you have any concerns about your health before you start. A good proportion of my new patients come from people who have caused injuries in the first few weeks, or even days sometimes, of starting a new regime. If you have any niggles, get them treated, and get advice on how to prevent them from recurring.
Be realistic
Set goals that are achievable and realistic. To lose a stone or be able to run 10k by Easter are realistic. To decide you are going to the gym every day before breakfast probably won’t last long. Fitness needs to be built gradually with a good base. Get advice on what exercise you need to do. Just running will help cardiovascular fitness somewhat, but needs to be part of a balanced all-around program if you want to be healthier generally. To maintain it, alone, running will also soon start to cause musculoskeletal problems.
Talk a friend into joining you
There will probably be no shortage of people thinking along the same lines as you. Teaming up hugely increases the chances of you both sticking to a program and makes it much more fun and less painful than trying alone. Even just planning together and talking about what you’re doing, (even if diaries don’t allow actually exercising together), is really encouraging.
Think long-term
Don’t look at this as a quick fix just to drop a few pounds. Take it easy and don’t rush. Tailor your plan around becoming more fit and healthy permanently. If you do it will help with so many other things, from energy levels to less aching joints or back, to stress relief and better sleep.
By Andrew Doody | Osteopath
Andrew is available for pre-exercise assessment, advice on exercise/regime planning, and diagnosis/treatment of outstanding or new issues, as well as advice on injury prevention. You can book an osteopathy appointment online.
MUMPS OUTBREAKS IN UK UNIVERSITIES:
CASES OF MUMPS REPORTED AT A NUMBER OF UK UNIVERSITIES
Public Health England has confirmed they are urging students to get MMR vaccinations.
A number of cases of mumps have been reported in Nottingham and Exeter. The recent rise in teenagers and young adults who have not had two doses of the MMR vaccine are believed to have caused an increase in UK cases. Unprotected students are particularly vulnerable due to close living conditions. Students are being urged to ensure they have received the full two-dose MMR vaccine course to protect themselves against mumps.
A total of 241 suspected cases were reported, with 52 confirmed, across Nottingham Trent University and the University of Nottingham and 7 confirmed cases at Exeter University.
MUMPS VIRUS
Mumps is a contagious viral infection which causes swelling of the parotid glands.
Initial symptoms can be similar to a cold and include:
- Headache
- High Temperature
- Joint Pain
- Feeling Sick
- Tiredness
- Loss of Appetite
- Swelling of the face/neck
Mumps can result in some serious complications. It can cause temporary hearing loss in 1 in 20 people. Mumps can cause a rare but potential risk of encephalitis, which affects 1 in 1,000 sufferers and requires hospitalisation.
It is spread in the same way as colds and flu – through infected droplets of saliva that can be inhaled or picked up from surfaces and transferred into the mouth or nose.
A person is most contagious a few days before the symptoms develop and for a few days afterwards.
Some people suffer complications that can include inflammation of the pancreas, viral meningitis (inflammation of the brain), inflamed and swollen testicles in men and ovaries in women.
MEDICAL ADVICE FOR MUMPS
If you think you may be suffering from mumps, or are concerned about the risk of infection, please see your doctor straight away.
Those who have not had the MMR vaccine – or have only received one dose – regardless of age, should ensure they receive two doses of the MMR (measles, mumps and rubella) vaccine.
In order to keep virus’ such as mumps from spreading, a certain proportion of the population must be immunised, this is called the ‘herd immunity’.
Herd immunity is particularly important as not everyone can get vaccinated, but those who can are able to help people those who can’t. Some people are unable to get vaccinated because they’re too ill, too young or have an impaired immune system. When we vaccinate, we protect not only ourselves but also the most vulnerable members of our communities.
VACCINATION AGAINST MUMPS
The disease can be easily prevented with two doses of the MMR vaccine, that has safely and efficiently been in use since the late 1980s’.
Make sure you are up-to-date with your measles, mumps and rubella (MMR) vaccine. Although the NHS immunisation schedule offers the vaccine to children from 12 months of age, the MMR can be given from 6 months. If you have not had measles, mumps or rubella or if you have not had two doses of MMR, you may be at risk. Measles mumps and rubella are easily passed from person to person and can be a serious illness in adults as well as children. It is never too late to have the vaccine.
You can book an MMR vaccine online.
Links:
This week is Cervical Cancer Prevention Week (#CCPW) and we’d like to remind all our patients that cervical cancer can be fatal – It is the most common cancer in women aged 35 and under.
Current UK statistics state:
> 2 women lose their lives to the disease every day
> 9 women are diagnosed with cervical cancer every day
> 75% of cervical cancers can be prevented by a smear test
Thousands of lives can be saved every year with better awareness and understanding of the symptoms of cervical cancer. Regular smear tests and having the HPV vaccine can dramatically decrease your chances of developing cervical cancer and will also assist in early detection.
Smear tests are extremely important and a major contributing factor to lowering the number of cervical cancer cases seen each year. On average, cervical screening helps save the lives of approximately 4,500 women in England every year, however, 1 in 4 women still don’t attend their smear test.

Smear tests are a method of detecting abnormal cells on the cervix, (the entrance to the womb). The detection and removal of abnormal cells can prevent cervical cancer from developing. As with all cancers, the earlier a problem is detected, the better the patient’s outcome.
Information on Cervical Cancer
Cervical cancer is not thought to be hereditary.
Cervical screening is not a test for cancer as screening programmes help to prevent cancer by detecting early abnormalities in the cervix, so they can be treated. If these abnormalities are left untreated they can lead to cancer of the cervix (the neck of the womb).
Symptoms:

For more information: www.jostrust.org.uk
At present, there is currently a shortage of Hepatitis B vaccine available in the United Kingdom and across the world.
Despite current global shortages, Fleet Street Clinic maintains good stock levels of the Hepatitis B vaccine.
The Hepatitis B virus is one of the most prevalent blood-borne viruses worldwide and is a major cause of chronic liver disease and liver cancer. In the majority of cases, Hepatitis B is asymptomatic – without symptoms. It is easily preventable through vaccination, and we strongly believe this vaccine should be offered more widely – all young, sexually active adults ought to be protected.
Although the overall risk for travellers is low, Hepatitis B immunisation is recommended for travellers travelling to East Asia and Sub Saharan Africa where between 5 – 10 % of the adult population is estimated to have persistent Hepatitis B infection. High rates of infection are also found in the Amazon, southern parts of eastern and central Europe, the Middle East and Indian subcontinents. The risk understandable increases for long-stay travellers in high-risk areas.
Certain behaviours and activities put individuals at higher risk, such as unprotected sex, adventure sports, body piercing, tattoos and injected drug usage.
Receiving medical or dental care in high-risk countries will also increase your risk and it is advised to avoid unless absolutely necessary. Travellers who have pre-existing conditions which may make it more likely for them to need medical attention should definitely consider the Hepatitis vaccination prior to travelling.
It’s the 30th anniversary of the MMR vaccine! To commemorate this scientific breakthrough, we wanted to share some information about the MMR vaccine and why it remains as important as ever for people, especially children, to be vaccinated.
The MMR vaccine is a combined vaccination that protects against three highly infectious diseases: measles, mumps and rubella (german measles). All three of which can be very serious and have the potential to cause long-lasting and severe health complications such as significant hearing loss, lung infection (pneumonia), brain infection (encephalitis), viral meningitis and even death.
Thankfully, the MMR vaccine is a highly safe and effective way of providing protection against measles, mumps and rubella. After 2 doses of the MMR vaccine, it is around 99% effective at protecting against measles and rubella and 97% effective at protecting against mumps.
Some people may not remember but before the MMR vaccine rollout in 1988, measles, mumps and rubella were all relatively common illnesses in the UK, especially among children. It is only thanks to a successful NHS vaccination programme with support by the private healthcare sector that cases dropped drastically after this time. And while this is great, the target of 95% of babies being vaccinated is still not being met and there continues to be outbreaks among unvaccinated children and adults. As a result, there is a push from the medical community for even more adults, as well as children to be vaccinated in order to prevent such outbreaks.
Didn’t have the vaccine as a child? That’s okay, there’s still time! It is really important to remember that it is never too late to catch up on childhood vaccinations. There is no upper age limit for receiving the MMR vaccine and so if you missed out on being immunised, it is strongly recommended that you have a “catch up” vaccine. This is especially important for anyone starting college or university, travelling abroad, planning a pregnancy or if you are a frontline health or care worker as your risk of exposure or serious health complications is increased.
As the 30th anniversary of the MMR vaccine is honoured, England’s top doctor and Chief Medical Officer (CMO), Prof Dame Sally Davies, has expressed her concerns that the uptake of the vaccine is “not good enough” and explains the dangers of children not receiving the vaccine.
She suggests that the reason some people are not having their children vaccinated is the result of people listening to anti-vaccine propaganda “myths” and “social media fake news”. She stresses the importance of listening to the science that provides clear evidence that the MMR vaccine is both safe and effective, and has helped “save millions of lives”.
Many of the false concerns over the MMR vaccine originated from a now-discredited study by former doctor, Andrew Wakefield, who incorrectly linked the MMR vaccine to autism back in 1998. This research has since been completely discredited and as a result, Andrew Wakefield was struck off the medical register for professional misconduct. Ever since, the medical community has worked hard to alleviate any lingering concerns over the safety of the MMR vaccine.
Our wonderful nurses at Fleet Street Clinic have been administering the MMR vaccine to our patients for over 25 years and we strongly believe in protecting all our patients with safe and effective vaccinations.
To read the full article, please click the link.
Some viruses thrive in the winter and are easily spread during cold weather. The lack of sunlight also means there is less Vitamin D in your body during winter, which can lower your immune system. This makes it harder for the body to fight off infections, resulting in a higher chance of sickness, even amongst the healthy.
If you’re planning on avoiding the flu this year, going on holiday, starting University, having a child or just living a healthy lifestyle in general, then there are a number of extremely important vaccines you should know about.
1. Flu Vaccine:
Now is the perfect time to have your flu jab, to ensure protection for the entire winter. Our adult flu vaccines are already in stock including Quadrivalent, FluAd and egg-free. Due to distribution delays, needle-free Quadrivalent vaccines for kids will be arriving soon.
– Find out more about the Flu Vaccine
2. MMR – Measles, Mumps and Rubella:
Many people who are now adults have never been vaccinated against measles, mumps or rubella, either from concerns over misinformation during the 1990s or because they simply missed out on getting protected. As a result, there has been an alarming rise in cases and outbreaks, with several deaths. Unfortunately, this year the UK also lost its ‘Measles Free’ status. Two doses are needed for protection, and it is never too late to be vaccinated!
– Find out more about the MMR Vaccine
3. Chickenpox:
There’s no need for any child to go through the misery of the chickenpox. It is entirely preventable with a vaccine that is still not yet available on the NHS, Varicella. This vaccine can be given to children over the age of one year. 2 doses are recommended for full protection.
– Find out more about the Chickenpox Vaccine
4. Shingles:
Shingles is a horrible reactivation of the chickenpox virus in adults who have had chickenpox during childhood. It consists of a painful, blistering rash. The pain can linger for months or years but it is also preventable. Shingrix is a relatively new vaccine which provides the best protection against Shingles. It offers up to 90% immunity. Supplies worldwide are limited but The Fleet Street Clinic is one of the first medical practices in the UK to make it consistently available.
– Find out more about the Shingles Vaccine, Shingrix
5. HPV (Human Papilloma Virus) Vaccine:
HPV is the leading cause of cervical cancer but also causes other genital, head & neck cancers. The national programme offers all 12- and 13-year-olds in school the Gardasil HPV vaccine. HPV-4 protects against 4 types of HPV. There is no “catch-up” programme for older children and adolescents.
At Fleet Street Clinic, we offer Gardasil 9. It offers greater protection against 5 additional types of HPV. In our opinion, if you have not received the HPV vaccine yet, you are better to get the HPV- Gardasil 9 vaccine to benefit from the extra protection it offers.
– Find out more about the HPV Vaccine, Gardasil 9
6. Whooping Cough:
Childhood vaccination does not give lifelong protection, and newborns are especially vulnerable. Vaccination is recommended during pregnancy, and may also be advisable if you have a close family member who is pregnant, or if you’re likely to be in close contact with their newborn baby.
– Find out more about Whooping Cough
7. Meningitis:
We offer Meningitis ACWY and Meningitis B vaccines. This vaccine is recommended to all those who fall outside the age groups currently targeted by the NHS or have an important deadline for protection.
– Find out more about Meningitis ACWY and Meningitis B vaccines
8. Hepatitis B:
Hepatitis B is spread by blood and body fluids. In most other developed countries, it has been a standard part of the childhood vaccination schedule for many years, but in the UK it has only just been added to the schedule at birth and infancy. There is no “catch-up” programme for older children and adolescents. We strongly believe this vaccine should be offered more widely – all young, sexually active adults ought to be protected.
– Find out more about Hepatitis B
9. Pneumonia:
We strongly recommend the Prevenar pneumonia vaccine for those aged 65 and over. Pneumonia can affect people of any age, but it’s more common and can be more serious, in certain groups of people, such as the very young or the elderly. Anyone with a past history of pneumonia, asthma or lung disease should also consider this vaccine. Anyone can get a pneumococcal infection, but not everyone is offered the pneumococcal vaccine on the NHS. Prevenar pneumonia vaccine protects against 13 of the most common strains of Streptococcus pneumoniae bacteria.
– Find out more about the Pneumonia Vaccine
10. Rabies:
At the Fleet Street Clinic, we are well known for offering the full range of travel vaccines, always in stock. But if I had to pick just one vaccine I would never want to be without, it would be rabies. Protection is cheap, easy, safe and long-lasting – but expensive and hard to find if you are ever unlucky enough to be bitten abroad. I was once attacked by a dog in a remote part of Peru, and have had to look after dozens of travellers who have been in similar situations.
– Find out more about the Rabies Vaccine
Get in touch…
If you would like more information or require any of these vaccinations, please give us a call to arrange an appointment or book your appointment online today
Exposure to high temperatures increases sweating and results in loss of fluid and electrolytes causing rapid dehydration. This can result in heat exhaustion or heatstroke which can be life threatening if not dealt with promptly.
Any traveller can be at risk of sun and heat related injuries but the highest risk is in the elderly, babies, children and those with pre-existing medical conditions.
Travellers who perform strenuous physical activity will increase the risk of illness related to the heat.
It can take the body up to 10 days to acclimatize to the heat, so it is important that travellers are prepared to prevent heat related illness.
What can travellers do?
*Seek shelter and shade during the middle of the day (11am -3pm) when temperatures are at their hottest
*If you are outside, ensure you protect your skin against the sun with a high factor sun cream
*Wear lose fitting light weight and light colour clothing
*Keep hydrated by drinking plenty of fluids and eating food with a high water content (such as fruit)
*Ensure you are taking in sufficient salt in your diet (sweating leads to electrolyte and salt depletion).
*Avoid caffeine and alcohol, which can worsen heat related illness
Heat stroke can be a life-threatening emergency and medical help should be sought.
For more travel health advice, you can book a travel consultation appointment with one of our nurses.
Measles: Don’t Get Caught Out
Cases of measles have risen rapidly in recent months in Europe, United Kingdom but most recently, Brazil. Measles is a highly contagious virus with potential for serious complications. It is a serious viral infection, spread by airborne droplets and is highly infectious. It is recommended that two doses of the measles vaccination should be given to individuals to prevent infection. Although many countries include the vaccination as part of the routine childhood immunisation schedule, international travellers should check that they are immune before departure.
Most UK citizens will have immunity in one of two ways:
Natural immunity can be assumed for those born before 1970, where individuals would have been exposed to the infection naturally.
Having received two doses of vaccination against measles. The vaccination was introduced in 1970 and is usually given in combination with rubella and mumps as the MMR vaccine.
Initial symptoms can include:
- Runny nose
- High Temperature
- Spots in the mouth
- Aches and pains
- Sore eyes and swollen eyelids
A rash appears after 2-4 days which can present as blotchy spots, often starting at the head and progressing down.
Advice for Adults
If you are in doubt about whether you have immunity to measles, a simple blood test can be taken to determine your immunity status. If you have no immunity to measles, you can be offered the MMR vaccination.
Advice for Children
Infants normally receive the MMR vaccination at 13 months old, as part of the national schedule. However, if you are travelling to a country where there is a significant risk of infection, the vaccination can be given to infants from 6 months.
Medical Advice
If you think you may be suffering from measles, or are concerned about the risk of infection when travelling, please see your doctor straight away.
The Fleet Street Clinic stocks travel sickness medication, travel vaccines and medical travel kits. Our experienced travel clinic nurses can help advise with any queries or more information on Measles.
Fleet Street Travel Clinic
Shringrix now in stock
We are pleased to say we have secured a limited stock of Shingrix at Fleet Street Clinic. These are the first doses to become available in the UK and have been specifically imported from other EU markets.
Globally, this vaccine is in extremely short supply and full supply is unlikely to be able to meet the demand for a number of years. This is even the case in the USA, where the vaccine was first launched since the vaccine has been recommended for routine use in over 50’s. There is unlikely to be an NHS program for the foreseeable future.
‘We believe we are the first medical practice in the UK to be able to offer our patients the new Shingrix vaccine, which provides powerful protection against a deeply unpleasant disease. As a full service medical practice with a longstanding commitment to cutting edge care, this follows an established tradition of UK vaccine “firsts” – including HPV for both sexes, Meningitis B, Zostavax, and Quadrivalent Flu.’
– Richard Dawood, Medical Director
What is Shingles?
Shingles, also called herpes zoster, is a painful skin rash caused by the chickenpox virus (varicella-zoster virus).
After you’ve recovered from chickenpox, the varicella-zoster virus lies dormant in your nerve cells and can reactivate at a later stage when your immune system is weakened. Anyone who has had chickenpox can get shingles.
Who can get Shingles?
While you can get shingles at any age, the odds start climbing at 50, then more sharply with each decade. As your immune system weakens with age, that puts you at an increased risk for shingles.
Your risk for shingles increases as you age. Previously we had recommended the Zostavax vaccination for shingles; which is still available. The difference in vaccinations being, Zostavax is only around 50% effective in preventing shingles, but Shingrix efficacy is up to 90% in preventing shingles and it’s complications.
Shingrix Vaccination Schedule…
The primary vaccination schedule consists of two doses of 0.5 ml each: an initial dose followed by a second dose 2 months later. If flexibility in the vaccination schedule is necessary, the second dose can be administered between 2 and 6 months after the first dose.
> Due to the scarcity of the vaccine, we recommend all those having the Shringrix vaccination to prepay for the second dose in advance.
HPV vaccine unavailable to boys on the NHS
The HPV vaccine is now offered to girls aged 12-18 years in the UK for free by the NHS.
Since its introduction in 2008, it has already shown to be very effective in reducing the cases of cervical cancer in females*. But the HPV virus doesn’t only cause cervical cancer, it can lead to other cancers such as anal, head, neck and throat cancers. Men are as much at risk of these cancers as women, so why are boys ineligible to receive the HPV vaccine as part of the NHS vaccination schedule?
The BBC has reported the case of Jamie Rae today, to highlight the issue. Mr Rae is campaigning for the HPV vaccine to be introduced, after undergoing radiotherapy for his throat cancer which he believes could have been prevented if an HPV vaccine had been available.
The article also reports that Professor Francis Vaz, a head and neck surgeon at University College London Hospital, paid privately to vaccinate his three sons, to protect them from certain cancers like anus, penis, mouth and throat. He said he saw on a daily basis that cancers driven by the HPV virus had been increasing in the past decade.
“I regularly see the bad end of that spectrum, so I thought the vaccination would be suitable for my sons,”
– he said.
“It’s just unfortunate it wasn’t available for them on the NHS. I was happy to pay for it because I think it’s a good vaccine.”
Why boys should receive the HPV vaccine
- About 15% of UK girls eligible for vaccination are currently not receiving both doses, a figure which is much higher in some areas
- Most older women in the UK have not had the HPV vaccination
- Men may have sex with women from other countries with no vaccination programme
- Men who have sex with men are not protected by the girls’ programme
- The cost of treating HPV-related diseases is high – treating anogenital warts alone in the UK is estimated to cost £58m a year, while the additional cost of vaccinating boys has been estimated at about £20m a year
Source: HPV Action
Our HPV vaccine page explains how get an HPV vaccine at Fleet Street Clinic.
FLEET STREET CLINIC – SPECIALIST VACCINE CLINIC
Fleet Street Clinic is a specialist vaccination clinic offering all vaccinations from travel jabs, to childhood immunisations to flu vaccinations programmes.
TO BOOK
You can book an appointment online.
Our InBody scanner lets you take control of your health
Do you want to take steps to manage your weight? Are you looking to lose weight or gain muscle? If so, the first step to changing your body is to get accurate measurements of your current stats.
Here at the Fleet Street Clinic, our Inbody scanner provides you with a detailed analysis of your body’s composition. This gives you an accurate way to measure your weight g oals.
You can use the InBody scanner by booking an appointment. Our nurse will measure your height, document your age and the scanner does the rest! Accurately measuring your weight, body fat, muscle mass, BMI and basal metabolic rate, the InBody scanner tells you if you are above, below or in the normal range for your age and height. You’ll receive your results as a one-page analysis, which we will talk through with you. From this, you can set your achievable long-term health goals.
Look for more help with your health goals?
If you’re looking to get some more direction on how to achieve your health goals, our dietitian provides weight management advice to improve your health to optimal levels.
Many people in the UK view tuberculosis as a Victorian disease, but in fact even today, 5000 people a year are affected by TB.
World TB day gives the opportunity to raise awareness of tuberculosis and lead to fewer cases. An easy way to help stop the spread TB is by having a BCG vaccine, which can be given to newborn babies soon after birth.
In some parts of London, the BCG is not readily available on the NHS, in which case you might consider getting the BCG vaccine privately.
BCG Vaccine for Children
At the Fleet Street Clinic in Central London, we have been providing specialist vaccination services for over 20 years.
We run a BCG clinic once a week for babies and children under the age of 6. Our baby/child BCG clinic runs on Wednesday’s.
Why have the BCG Vaccine?
The BCG vaccine protects against tuberculosis. TB is a bacterial infection that affects the lungs in most cases but can affect other parts of the body such as the bones and kidneys. Typical of many bacterial infections, tuberculosis can be spread through long-lasting exposure to an infected person via sneezing or coughing. The BCG vaccine is a proven way to ensure protection against the tuberculosis bacteria.
Meningitis Now Offers Advice for World Meningitis Day, to spread the word about meningitis, how to spot it and what causes it, as well as the importance of vaccines.
The theme for World Meningitis Day 2018 is #AllMeningitisMatters.
There are several different causes of meningitis and vaccines can help protect against certain strains of bacterial and viral meningitis.
The key messages for this year are:
- Meningitis is a potentially deadly disease that can kill within 24 hours.
- Bacterial meningitis can be caused by many different types of bacteria.
- There are safe and effective vaccines that protect against the most common causes of bacterial and viral meningitis.
- Not all strains of meningitis are vaccine preventable, so being able to recognise the symptoms is crucial.
Measles on the rise:
The World Health Organisation (WHO), has reported that measles cases are on the rise worldwide and in Europe alone, outbreaks have surged to a 20-year high.
The WHO states that reported measles cases (provided by each country) currently show that about 229,000 cases have already been reported, compared with 170,000 for 2017. Worryingly the 2018 number is likely to rise as the reporting deadline ends April ’19.
With a 50% increase in measles cases last year, it is important to understand the benefits of vaccinating against measles:
Dr Richard Dawood, our Medical Director explains;
“I recently heard about a patient suffering a bad attack of shingles. She didn’t believe in doctors, medicines or vaccines, I was told, and was languishing at home, with a dreadful, crusted rash across her body, and burning with pain. She had stuck to her beliefs and refused to take antiviral medication that could have aborted the attack or reduced the probability of ending up with long term nerve damage and lingering pain. Shingles can strike more than once, but since she doesn’t believe in vaccines (there is a good one that is 95% effective) she will have to take her chances of a recurrence in future. I disagree with her opinions, but her latest actions will harm nobody but herself.
But measles is different: when it comes to vaccination, personal choices and opinions have a direct impact on the health and wellbeing of others – individually as well as for entire communities. Measles vaccination is a major public health issue. Memories of the past outbreaks, epidemics, tragic disability and loss of life that drove research and ground-breaking vaccine development now belong to a previous generation. In these days of “fake news”, “influencers” and social networks, it has become too easy to undermine confidence in matters of public health. In the case of measles, concerns about vaccine safety are down to the “fake research” of Andrew Wakefield, who was struck off the medical register for concocting a spurious link with autism in the 1990s. But the damage was long-lasting.
The complications of measles are most severe in babies who are not yet old enough to be vaccinated, and children with reduced immunity. When the rate of vaccination in the general population falls below 95%, outbreaks occur and can easily spread, with the highest impact on those most vulnerable populations, undermining years of hard work around the world to bring measles under control.
That is what is happening now”.
VACCINATION AGAINST MEASLES
‘The highly contagious disease can cause severe diarrhoea, pneumonia and vision loss. It can be fatal in some cases and remains an important cause of death among young children”, according to the WHO.
The disease can be easily prevented with two doses of a safe and efficient vaccine that has been in use since the 1960s’.
Make sure you are up-to-date with your vaccinations including the measles, mumps and rubella (MMR) vaccine. Although the NHS immunisation schedule offers the vaccine to children from 12 months of age, the MMR can be given from 6 months. If you have not had measles or if you have not had two doses of MMR, you may be at risk. Measles is easily passed from person to person and can be a serious illness in adults as well as children. It is never too late to have the vaccine.
The HPV Vaccine, Gardasil 9, is back in stock at Fleet Street Clinic.
The vaccine is available to men and women. It protects against a range of cancers including cervical, head and neck cancer and other HPV-related diseases including genital warts.
5 facts about the HPV (Human papillomavirus) :
- Nearly all cases of cervical and anal cancer and 70% of oropharyngeal cancers are related to HPV.
- HPV is one of the most common sexually-transmitted diseases, so common in fact that most sexually active men and women will have HPV at some point in their life.
- There are different strains of the virus and they can be categorised into low-risk and high-risk HPV.
- There is no cure for HPV; some people fight off the virus without any knowledge of having been infected, whilst the virus can lie dormant in others, remaining undetected for many years.
- The virus can eventually cause abnormal cell growth – cervical abnormalities in women, which is why regular cervical screening is so important.
In order to protect against the virus, the HPV vaccine is strongly recommended. For more information, visit our HPV Vaccine page.
BOOKING A Vaccination APPOINTMENT
You can book an HPV appointment online.
Asthma – affecting millions around the globe
Today is World Asthma Day. Asthma is a very common respiratory condition, with 300 million people affected globally. And the numbers of asthma sufferers is increasing each year.
At Fleet Street Clinic we deal with asthma-related complaints on a regular basis and stock medication for dealing with symptoms.
What is Asthma?
Asthma is caused by inflammation in the airways, which narrow and can become blocked with mucus, leading to breathing difficulties.
Some may grow out of asthma, whilst others will have to manage the condition for life.
Asthma sufferers may notice wheezing, coughing, breathlessness and a tight chest. Severe symptoms may leave sufferers struggling to breathe which results in an asthma attack.
Treatment can be provided with inhalers and various steps can be taken to deal with asthma triggers to lessen symptoms.

Managing Your Asthma
Managing your asthma is very important to maintaining your health. Keep a diary of asthma flare-ups to see if you notice any particular triggers and visit your doctor regularly for check-ups. If your symptoms worsen, make sure to seek medical help without delay.
Travel and Asthma
If you are travelling, make sure to check you have the medication necessary for your trip. Remember hayfever seasons can vary around the world. Fleet Street Clinic stock necessary medication to cover any last-minute requirements.
If you think you may have asthma, book a GP appointment today.
What is Coeliac disease anyway?
Coeliac disease is an auto-immune condition, defined as
a disease in which the small intestine is hypersensitive to gluten, leading to difficulty in digesting food.
We’ve all heard the term “gluten free” of late, something that has become synonymous with the fad diet of the moment, but for suffers of this fairly common disease, what does being a coeliac actually mean?
Gluten is a type of protein found in many types of food. Let’s be clear, being a coeliac does not mean that you have a gluten intolerance. When you are a coeliac, your immune system responds to the gluten in your food like it is a threat and attacks it. This in-turn damages the lining of the small intestine and hinders your body’s ability to digest nutrients from food properly.
What food can gluten be found in?
Any food containing:
- Wheat
- Barley
- Rye
The most common food with gluten in:
- Pasta
- Cake
- Breakfast cereal/bars
- Bread
- Bottled sauces
- Beer
What are the symptoms of coeliac disease?
There are many varied symptoms of being a coeliac but some of the most common symptoms are:
- Diarrhoea
- Bloating and passing wind more regularly
- Pains in your abdomen
- Feeling tired all the time
How do you treat coeliac disease?
Although there is no cure for being a coeliac, you will need to follow a gluten free diet to appease the symptoms. With a little time and effort, most sufferers can follow the diet and carry on about their regular life with no further complications from the illness.
This can be tricky at first as there are so many products you would pick up from your local supermarket that contain gluten. It’s best to speak with an expert for advice on how to manage your diet. At Fleet Street Clinic we can screen for many food intolerances as well as assisting you in every step of the way should your tests coming back positive for an allergy.
If you have any concerns regarding coeliac disease or any other type of food intolerance, please book an appointment online. Or you can contact on 020 7353 5678 for more information.