Month: August 2024
On 14th August 2024, the World Health Organization declared outbreaks of mpox in Africa to be a Public Health Emergency of International Concern.
What is mpox?
Mpox is a viral infection that was previously known as “monkeypox”.
It shares some similarities with smallpox, to the extent that smallpox vaccine may be cross-protective; however, the illness is much less severe. (Waning population immunity to smallpox, since vaccination programmes ended in 1980, is one possible reason for the increased tendency to outbreaks now.)
So far, there have been 14,000 cases reported in Africa, with 524 deaths. Sweden has just reported the first case of clade I mpox outside Africa in the current outbreak (see below).
Previously confined to central Africa, recent outbreaks have ultimately spread globally, which is why the WHO has now decided to urge a concerted global response.
How is it spread?
The infection is spread mainly by close direct / intimate contact with body fluids and secretions, and by sexual exposure.
It can also be spread by contact with animals, or their droppings, or by eating under-cooked contaminated meat – so-called “bush meat”. The animal reservoir of infection is mainly among rodents and non-human primates.
The illness
Infection may be symptomless, but in most cases, symptoms appear 7 to 14 days following exposure.
Mpox is characterised by blistering skin lesions that are often extremely painful (and highly infective to other people), occurring particularly on the skin, genitals and face. They can be sparse, or even single blisters.
Other symptoms include fever, chills, headache, muscle aches, fatigue and swollen lymph glands.
The blisters may appear first on the face, spreading to other parts of the body; or alternatively in the genital area if the infection was acquired by sexual contact. Extensive lesions around the mouth may make eating and drinking painful or impossible, requiring intravenous treatment.
The illness is considerably more serious in people with HIV infection or reduced immunity. Severity of infection is also linked to the degree of exposure.
Mpox strains
There are two strains (called clades – Clade I and Clade II) that differ in severity and ease of spread.
Clade II tends to be more severe (up to 1,000 times more virulent than clade II) and occurs in Central Africa, Clade II occurs mainly in West Africa and may sometimes be more easily transmissible. Mutations into sub-strains is also occurring, which makes testing more complicated, especially in countries where resources are poor.
Where are cases occurring?
It is important to bear in mind that official statistics generally underestimate true numbers of cases, since not everyone with symptoms seeks medical attention, and not all cases undergo full testing.
Laboratory-confirmed cases have been reported in:
- Burundi: over 100 cases (Clade Ib) throughout the country
- Central African Republic: 28 cases (Clade I) throughout the country
- Côte d’Ivoire: 6 cases (Clade II) in Abidjan and Bas-Sassandra districts
- Democratic Republic of the Congo: > 14,000 cases (Clades Ia and Ib) throughout the country, mainly in Équateur, Sankuru, South Kivu, and Sud Ubangi provinces
- Kenya: 1 case (Clade Ib) in Taita-Taveta County
- Republic of the Congo: > 120 cases (Clade I) throughout most of the country, mainly in Cuvette, Kouilou, Likouala, and Point-Noire departments
- Rwanda: 4 cases (Clade Ib); no specified locations
- South Africa: 24 cases (Clade IIb) in Gauteng (12 cases and 2 deaths), KwaZulu-Natal (11 cases and 1 death), and Western Cape (1 case) provinces
- Uganda: 2 cases (Clade Ib) in Kasese District; no secondary transmission has been reported
A previous outbreak in 2022 resulted in spread to over 40 countries – with over 30,000 cases in the USA, for example, mainly in the MSM community.
Are visitors at risk?
Although current news reports of mpox cases are alarming and intended to generate a global public health response, so as to raise awareness and help bring outbreaks under control, most tourists and travellers to Africa are not at risk.
Travel to Africa for the usual tourist activities (e.g. safari, outdoor activities, beach) should be unaffected by the outbreak.
Older travellers who have previously been vaccinated against smallpox may still have some additional cross-protection against mpox.
- Risk arises from close contact (especially sexual contact) with infected people.
- Those at highest risk are men who have sex with men (MSM).
- High-risk behaviour is easily avoided, and safe-sex precautions reduce the risk of infection.
- Risk also arises from close physical contact with infected animals, or by eating under-cooked bush meat – which should be avoided. (Thorough cooking kills the virus.)
- Healthcare workers may be at risk if caring for people who are ill with mpox
- Journalists and news media personnel should avoid physical contact, keep their distance and observe the usual hygiene precautions when reporting on the evolving mpox outbreak situation
Mpox vaccines and treatment
- In the UK, vaccination is available for MSM and healthcare workers via the NHS.
- Current vaccines protect against all strains.
- Vaccination within 14 days of possible exposure also appears to confer protection (post-exposure protection).
- Several antiviral drugs can provide benefit in the most severe cases.
More information:
Oropouche Virus Disease: A growing concern in Central and South America.
As of mid-2024, Central and South America are experiencing a significant outbreak of Oropouche virus disease, impacting countries such as Brazil, Bolivia, Colombia, Peru, and Cuba.
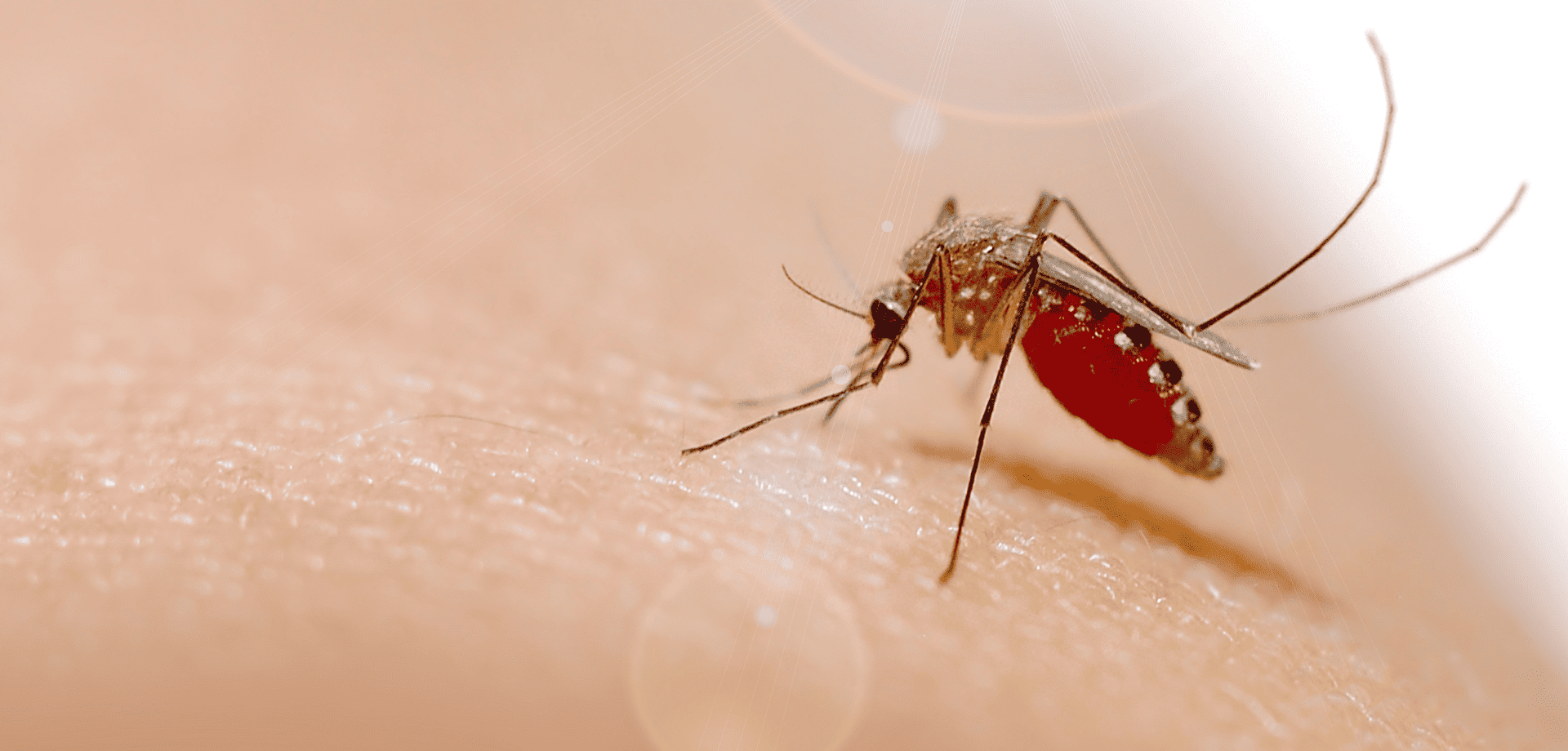
The Oropouche virus is primarily transmitted through the bites of infected midges (Culicoides paraensis) and mosquitoes. The virus is mainly spread in tropical and subtropical regions where these vectors are prevalent.
Symptoms of Oropouche virus disease include:
- sudden-onset fever,
- severe headaches,
- muscle and joint pain,
- rash,
- eye pain,
- nausea,
- and dizziness.
While most cases are mild and self-limiting, lasting 3 to 7 days, some individuals may experience more severe symptoms like meningitis and encephalitis.
There is no specific antiviral treatment or vaccine for the disease, so care focuses on symptom relief, such as rest, hydration, and pain management.
How to protect yourself from Oropouche virus
Preventing Oropouche virus disease involves reducing exposure to vector bites. Unlike mosquitoes, the main vector (midges) lacks a proboscis, and so is unable to bite through clothing.
Covering up, and wearing long-sleeved clothing, is therefore a keyway of preventing infective bites.
Other key measures include using plenty of insect repellent, impregnating clothing with Permethrin insecticide, using bed nets, and staying indoors during peak biting times.
Eliminating standing water where vectors breed is an important public health measure.
Prevention is key!
With no vaccine available, prevention remains the best defence against Oropouche virus disease.
Personal protective measures against insect bites also help protect against dengue, yellow fever, Zika, chikungunya, malaria, and a wide range of other tropical insect-borne infections, and should be followed carefully by travellers to tropical countries.
Cases found in Europe
Spain, Italy and Germany reported infections in numerous patients who had recently travelled to Cuba and Brazil.
The European Centre for Disease Prevention and Control (ECDC) warned of a moderate threat to travellers visiting Brazil, Bolivia, Colombia, Peru and Cuba, where Oropouche virus (Orov) is currently spreading.
If you’ve recently travelled to a known outbreak area and are experiencing any of the symptoms mentioned above, it is important to mention this to your doctor. This will help them rule out an Oropouche virus infection.
Worried about your upcoming travel plans?
Schedule a travel consultation with one of our specialist travel nurses.
They will guide you through potential health risks and recommend the necessary preventive measures and vaccinations to ensure your safety while travelling.
For more information on:
If caught and symptoms develop, rabies is almost invariably fatal.
Rabies is spread through the saliva of an infected animal and is present in over 150 countries worldwide. Up to 100 children die each day from rabies, and more than 55,000 people a year are killed from the disease, mainly in Asia and Africa.
If bitten or scratched by an infected animal you need to act quickly. Your pre-exposure vaccines simplify medical care in case of a potential rabies exposure, reducing the number of post-exposure vaccine doses needed and providing more time to seek medical care because your antibodies will start to respond. This is crucial when traveling to remote areas with limited access to medical facilities.
If you haven’t had pre-travel vaccinations, the treatment is much more complicated; it is also expensive and can be hard to access in lower income countries. If treatment is given correctly and promptly after exposure, it is 100% preventable.
It is extremely important that if you are travelling somewhere with a known risks of rabies it only seems sensible to protect yourself against it. Rabies is a vaccine-preventable disease, so make sure you get vaccinated before you travel.
For more information on rabies and travel health, visit our rabies page here.
The Fleet Street Clinic is passionate about travel. We have provided rabies vaccinations for over 20 years. Our team of expert travel medical professionals provide advice and detailed consultations to ensure you have a healthy trip.
You can book a travel consultation or rabies vaccination appointment online.
ESSENTIAL CHICKENPOX VACCINE FACTS:
- The chickenpox vaccine is not currently given by the NHS, but is part of the childhood vaccination schedule in other countries
- Chickenpox is a highly contagious infection caused by the varicella zoster virus
- In the UK, it mostly affects children
- It can be itchy and uncomfortable, can leave scars, and can sometimes cause severe disease – adults may suffer more serious symptoms, including pneumonia
- Chickenpox is spread by inhaling droplets coughed up by people infected with the virus
- People with chickenpox become contagious about 2 days before the appearance of the rash, which can make it difficult to avoid infection
- The chickenpox vaccine (varicella vaccine) can be administered from the age of twelve months onwards
- Two doses of vaccine are needed, with a 4 week gap between doses
- If your child is receiving the MMR vaccination or a Yellow Fever vaccine, the varicella vaccination must either be given on the same day, or 4 weeks later
HOW TO BOOK A VACCINATION APPOINTMENT
Fleet Street Clinic is dedicated to maintaining a good supply of the chickenpox vaccine.
Our private chickenpox vaccine service is undertaken by doctors and nurses with long experience of vaccinating children. Our family friendly clinic is sympathetic to parents’ needs and concerns, and we welcome any vaccine-related queries. We operate a Saturday vaccination clinic once a month, the next will be held on Saturday April 8th.
To book your chickenpox vaccination for yourself or your child, you can book online now.
The summer holidays will fly by and be over as quickly as they began, much to your relief, but probably the disappointment of your kids! Unfortunately, alongside the general back to school chaos, September also brings with it the start of the flu season.
Flu season not only means that people have to take time off of work due to being ill themselves, but parents often have to take time off work to look after their children who have the flu, because schools are rife with superspreaders. It seems that the best solution to the frustrating effects of the flu on school and parenting life is to nip it in the bud early enough in the season for immunity to make a significant difference.
This is where the flu vaccine comes in.
The flu vaccine comes in two forms, the traditional syringe-administered jab, and a nasal spray vaccine. While the nasal spray vaccine may be the preferred administration tactic for parents of children who don’t like needles, supply issues have resulted in limited availability, and it may still be worth considering the alternative.
When might the jab be preferable?
The nasal spray vaccine is protective and an excellent choice, but is not suitable for everyone. It is a live vaccine, and so cannot be administered to children who are immunocompromised or who live with anyone who may be immunocompromised. It is also unsuitable for anyone with bad asthma, since it may trigger an attack. The injected vaccine is not a live vaccine and is an obvious solution for a lot of people.
The nasal spray vaccine contains traces of gelatine and egg, and so may be unsuitable for vegetarians, vegans, Muslims or those with a severe egg allergy. There is a cell-culture based injectable vaccine that is egg-free, which may be a more acceptable alternative.
The nasal spray vaccine can only be given from age two onwards. However, if there is a special reason for needing to vaccinate your child at a younger age than this, the standard injectable vaccine can be given from the age of 6 months. (The best way to protect babies younger than this is by vaccinating mums during pregnancy.)
For the past three winters, the nasal spray vaccine has been in limited supply. It has not been available privately but only through the NHS, and supply issues have resulted in extended delays. By contrast, injected vaccines have been available reliably from September onwards.
A well-timed dose of the injected vaccine, early in the season, may be a better option than the uncertainty of a delayed dose.
At the Fleet Street Clinic, we have been happy to offer the nasal spray vaccine previously but having been unable to obtain reliable supplies for the past three years, we will not be offering it this season.
If you decide to book the injected flu vaccine for your child this winter, you can rely on guaranteed supplies as well as our expertise in vaccinating babies and children of all ages.
__________________________
24/25 Winter Flu Vaccination Pricing:
Cell-Based Quadrivalent Flu Jab – £42 – Suitable from 2 years
Standard Quadrivalent Flu Jab – £30 – Suitable from 6 months old