Tag: Africa
Egypt has long been a fascinating destination for travellers with its ancient monuments, rich culture, and vibrant landscapes. Now, there’s even more reason to consider Egypt as a travel destination: the World Health Organization (WHO) has officially declared the country malaria-free.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, said “Malaria is as old as Egyptian civilisation itself, but the disease that plagued pharaohs now belongs to its history and not its future.
This is a significant milestone in public health and brings an added layer of safety and assurance to travellers planning to visit.
Here’s what you need to know about this important achievement and what it means for your health when traveling to Egypt.
What does it mean to be “Malaria-Free”
To be certified as malaria-free, a country must demonstrate that it has interrupted local transmission of malaria for at least three consecutive years. Egypt met this requirement, showing consistent results in controlling the disease, improving healthcare infrastructure, and reducing the risk of reintroduction.
According to the WHO, Malaria in Egypt has been traced as far back as 4000 B.C.E., with genetic evidence of the disease found in Tutankhamun and other ancient Egyptian mummies.
Egypt is one of the latest countries to receive this certification, contributing to a global push toward eradicating malaria worldwide.
What does it mean for travellers?
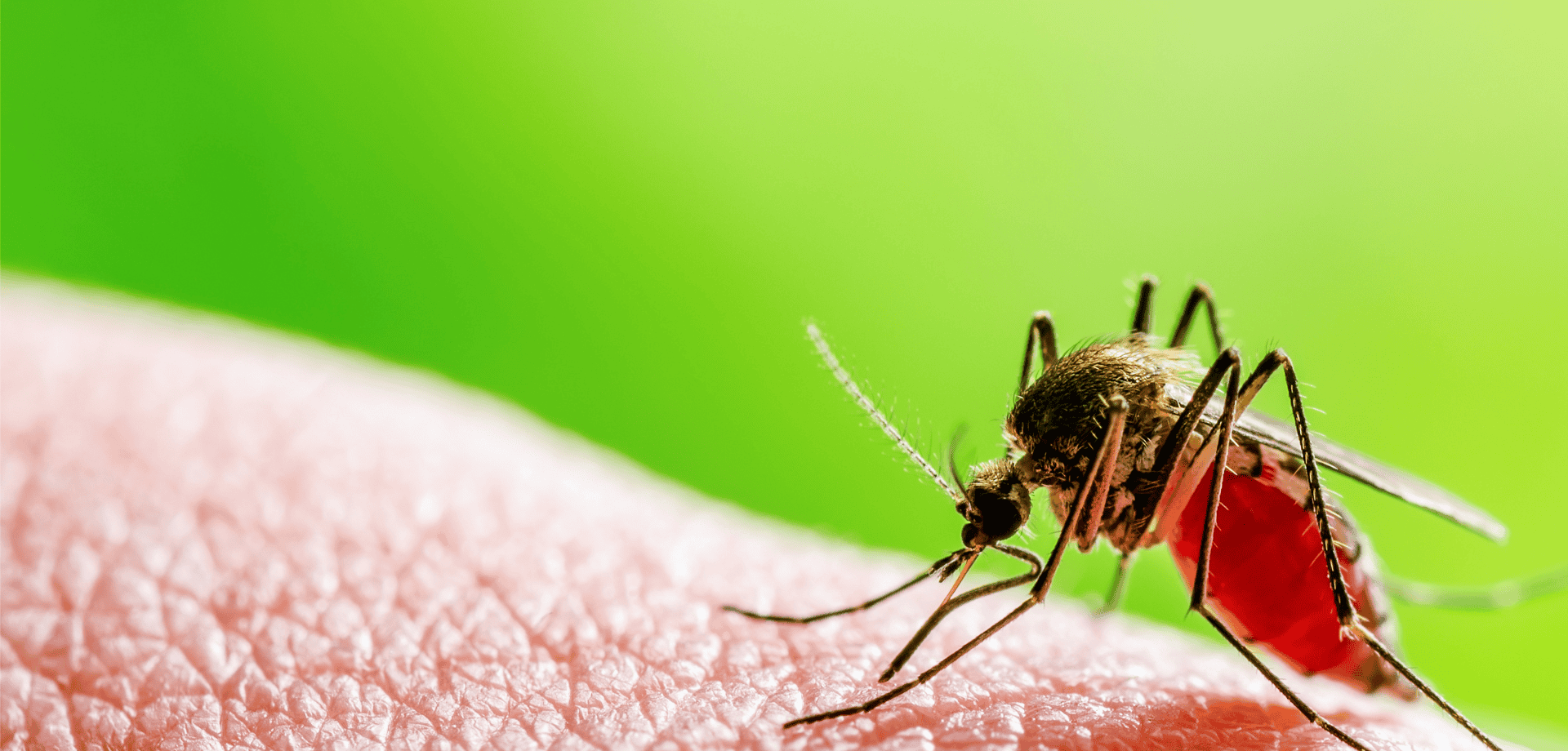
Malaria has long been a concern in various tropical and subtropical regions, causing severe illness, fever, and sometimes even death.
Travellers often must take preventative steps, such as antimalarial medication and mosquito avoidance measures, when visiting areas where malaria is prevalent.
Egypt’s certification as malaria-free means travellers now have one less health risk to consider when planning their holiday.
For the tourism and travel health sectors, this achievement reassures visitors that Egypt is safe from malaria transmission, especially in rural areas and near water sources, which are typically high-risk locations for malaria-carrying mosquitoes.
Are there any precautionary measures still needed?
While Egypt’s malaria-free status is excellent news, it’s still essential to practice general travel health precautions to stay safe.
Here are some tips:
- Protect Against Other Mosquito-Borne Diseases: While malaria may not be a concern, other mosquito-borne illnesses, such as West Nile Virus and Dengue Fever, can still pose risks. Use insect repellent, wear long sleeves, sleep under a mosquito net and consider vaccinations where possible, like Qdenga for Dengue Fever.
- Stay Up-to-Date on Vaccinations: Egypt does require certain vaccinations for travellers, such as Rabies, Hepatitis A, Hepatitis B, and Typhoid. Make sure you are aware of any health advisories and have up-to-date vaccinations before your trip.
- Practice General Travel Hygiene: Staying hydrated, avoiding untreated water, and being cautious with food preparation are essential for staying healthy on your travels.
Is a travel consultation still necessary?
Yes, whilst it is fantastic news that Egypt is now malaria-free, there are other health risks to consider when travelling and it is still important to seek travel health advice from an expert.
We advise booking a travel consultation at least 4-6 weeks before your departure date to allow enough time for any necessary vaccinations, medications, and preventive advice to take full effect.
If you’re planning a last-minute trip, don’t worry! Book a consultation as soon as possible; even a brief appointment can provide valuable advice, essential vaccinations, and immediate preventive tips to keep you safe during your travels.
The Future of Malaria Control in the Region
Egypt’s success in eradicating malaria is a hopeful indicator for neighbouring regions where malaria is still a concern. The country’s strategies and investments in healthcare could serve as a model for other nations aiming to reduce or eliminate malaria.
Planning Your Malaria-Free Trip to Egypt
Whether exploring the pyramids, cruising the Nile, or enjoying the coastal resorts, travellers to Egypt now have added peace of mind regarding malaria. However, consulting with a travel health specialist before your trip remains important to ensure your overall health and safety. By staying informed and prepared, you can focus on enjoying the cultural and natural wonders Egypt has to offer.
As always, our travel health experts are here to provide personalised advice, vaccination guidance, and preventive health tips to make sure your journey is as safe and enjoyable as possible.
Book a travel consultation to discuss your upcoming trip to Egypt.
Related services at Fleet Street Clinic
Specialist Travel Clinic
Travel Vaccinations
Dengue Fever
Rabies Vaccination
Antimalarials
On 14th August 2024, the World Health Organization declared outbreaks of mpox in Africa to be a Public Health Emergency of International Concern.
What is mpox?
Mpox is a viral infection that was previously known as “monkeypox”.
It shares some similarities with smallpox, to the extent that smallpox vaccine may be cross-protective; however, the illness is much less severe. (Waning population immunity to smallpox, since vaccination programmes ended in 1980, is one possible reason for the increased tendency to outbreaks now.)
So far, there have been 14,000 cases reported in Africa, with 524 deaths. Sweden has just reported the first case of clade I mpox outside Africa in the current outbreak (see below).
Previously confined to central Africa, recent outbreaks have ultimately spread globally, which is why the WHO has now decided to urge a concerted global response.
How is it spread?
The infection is spread mainly by close direct / intimate contact with body fluids and secretions, and by sexual exposure.
It can also be spread by contact with animals, or their droppings, or by eating under-cooked contaminated meat – so-called “bush meat”. The animal reservoir of infection is mainly among rodents and non-human primates.
The illness
Infection may be symptomless, but in most cases, symptoms appear 7 to 14 days following exposure.
Mpox is characterised by blistering skin lesions that are often extremely painful (and highly infective to other people), occurring particularly on the skin, genitals and face. They can be sparse, or even single blisters.
Other symptoms include fever, chills, headache, muscle aches, fatigue and swollen lymph glands.
The blisters may appear first on the face, spreading to other parts of the body; or alternatively in the genital area if the infection was acquired by sexual contact. Extensive lesions around the mouth may make eating and drinking painful or impossible, requiring intravenous treatment.
The illness is considerably more serious in people with HIV infection or reduced immunity. Severity of infection is also linked to the degree of exposure.
Mpox strains
There are two strains (called clades – Clade I and Clade II) that differ in severity and ease of spread.
Clade II tends to be more severe (up to 1,000 times more virulent than clade II) and occurs in Central Africa, Clade II occurs mainly in West Africa and may sometimes be more easily transmissible. Mutations into sub-strains is also occurring, which makes testing more complicated, especially in countries where resources are poor.
Where are cases occurring?
It is important to bear in mind that official statistics generally underestimate true numbers of cases, since not everyone with symptoms seeks medical attention, and not all cases undergo full testing.
Laboratory-confirmed cases have been reported in:
- Burundi: over 100 cases (Clade Ib) throughout the country
- Central African Republic: 28 cases (Clade I) throughout the country
- Côte d’Ivoire: 6 cases (Clade II) in Abidjan and Bas-Sassandra districts
- Democratic Republic of the Congo: > 14,000 cases (Clades Ia and Ib) throughout the country, mainly in Équateur, Sankuru, South Kivu, and Sud Ubangi provinces
- Kenya: 1 case (Clade Ib) in Taita-Taveta County
- Republic of the Congo: > 120 cases (Clade I) throughout most of the country, mainly in Cuvette, Kouilou, Likouala, and Point-Noire departments
- Rwanda: 4 cases (Clade Ib); no specified locations
- South Africa: 24 cases (Clade IIb) in Gauteng (12 cases and 2 deaths), KwaZulu-Natal (11 cases and 1 death), and Western Cape (1 case) provinces
- Uganda: 2 cases (Clade Ib) in Kasese District; no secondary transmission has been reported
A previous outbreak in 2022 resulted in spread to over 40 countries – with over 30,000 cases in the USA, for example, mainly in the MSM community.
Are visitors at risk?
Although current news reports of mpox cases are alarming and intended to generate a global public health response, so as to raise awareness and help bring outbreaks under control, most tourists and travellers to Africa are not at risk.
Travel to Africa for the usual tourist activities (e.g. safari, outdoor activities, beach) should be unaffected by the outbreak.
Older travellers who have previously been vaccinated against smallpox may still have some additional cross-protection against mpox.
- Risk arises from close contact (especially sexual contact) with infected people.
- Those at highest risk are men who have sex with men (MSM).
- High-risk behaviour is easily avoided, and safe-sex precautions reduce the risk of infection.
- Risk also arises from close physical contact with infected animals, or by eating under-cooked bush meat – which should be avoided. (Thorough cooking kills the virus.)
- Healthcare workers may be at risk if caring for people who are ill with mpox
- Journalists and news media personnel should avoid physical contact, keep their distance and observe the usual hygiene precautions when reporting on the evolving mpox outbreak situation
Mpox vaccines and treatment
- In the UK, vaccination is available for MSM and healthcare workers via the NHS.
- Current vaccines protect against all strains.
- Vaccination within 14 days of possible exposure also appears to confer protection (post-exposure protection).
- Several antiviral drugs can provide benefit in the most severe cases.
More information:
In the months since its release in the UK, we have seen a huge demand for the new Dengue vaccine, Qdenga.
For those with experience of the disease, the news of its licensing has been much anticipated and we are proud to be one of the first clinics in the UK to offer the vaccine.
What is Dengue Fever?
Dengue is a viral infection that is spread through the bite of an infected aedes mosquito, a species easily recognisable by its striped legs. It occurs in over 120 countries worldwide, mainly in the tropics and sub-tropics, and is the second most common cause of fever in the returning traveller.
The most seriously impacted regions are the Americas, South-East Asia, and Western Pacific, with Asia accounting for around 70% of the world’s disease burden.
It is also spreading to new areas, including Europe, where outbreaks have been increasing in recent years. Read more about this in our recent blog, Dengue Fever in Europe: Temperature Risk.
Since it is transmitted from person to person, via the mosquito vector, it is of particular concern in populated, urban areas.
What are the symptoms of Dengue Fever?
Whilst most cases are asymptomatic, some will develop a severe flu like illness that can require hospitalisation. In rare cases, this will be life threatening.
Common symptoms include;
a high fever,
severe headache,
pain behind the eyes,
muscle ache,
joint pains,
nausea,
vomiting and rash.
There are four serotypes of Dengue virus; for those infected by one type, a subsequent infection is more likely to be life threatening. The severe type of Dengue usually starts a few days after the initial symptoms began. After feeling a bit better, symptoms suddenly return and can include severe abdominal pain, persistent vomiting and bleeding.
Approximately 1 in 20 patients with Dengue will progress into the severe form of the disease.
Dengue Fever Vaccination
Historically, the only protection we could provide was advice surrounding mosquito bite avoidance. With the arrival of Qdenga, we now have the option of a vaccination which provides safe and effective protection.
Studies have shown Qdenga to offer 80% protection from the first dose, with long term immunity achieved after the second.
Who should get vaccinated?
Qdenga can be safely given to those who have previously had the disease, and it is especially important for this group. We would also encourage frequent or long stay travellers to consider the vaccine. The vaccine is licensed for the prevention of Dengue in individuals from 4 years of age and requires two doses, to be given three months apart.
It is a live vaccine, so it’s not suitable for everyone. To discuss your suitability with one of our specialist travel nurses, please book a travel consultation online, or call our reception team on +44 20 7353 5678.
We can usually accommodate same day bookings and suitable vaccinations can be given within the same appointment.
Related services available at Fleet Street Clinic
Travellers’ Diarrhoea Online Consultation
For further reading
Tanzania is the perfect haven for adventurous travellers. Not only does it boast three of Africa’s Seven Natural Wonders, but it is home to the ancient nomadic stewards, the iconic, Maasai people. It is also the perfect place for an African safari adventure, with it’s 16 national parks accounting for more than 30% of the country.
Tanzania is blessed with the highest peak in Africa. Mount Kilimanjaro beckons visitors from all over the world. It is the world’s highest free-standing volcano and gets an estimated 30,000 travellers attempting to summit the peak each year. Climbers by the thousands venture here to challenge themselves on its muddy slopes, rocky trails and slippery scree.
It’s crowning jewel is the island, Zanzibar. The island is famous for its mix of exotic white sand beaches, dense palm trees and coral seas. A true paradise. It hosts famous spice plantations and is rich with diverse culture. Unguja (the main island in Zanzibar) is also home to many endangered species including the red colobus monkey and green turtle.
Whether you are visiting for an action-packed safari, challenging yourself to reach the peak of Mt. Kilimanjaro or relaxing on the island of Zanzibar, ensure you follow our top travel tips to stay healthy in Tanzania.
Vaccines
All travellers should ensure they are in date with all their routine immunisations, including diphtheria, tetanus and polio (DTP), and measles, mumps and rubella (MMR).
You should consider specialist travel vaccinations prior to travel. Hepatitis A and Typhoid are highly recommended. Furthermore, some travellers may also wish to be vaccinated against Rabies, Hepatitis B and Cholera for extra precautions. Especially if travelling to more rural areas.
For more information on our vaccines, please visit our travel and wellness vaccination pages.
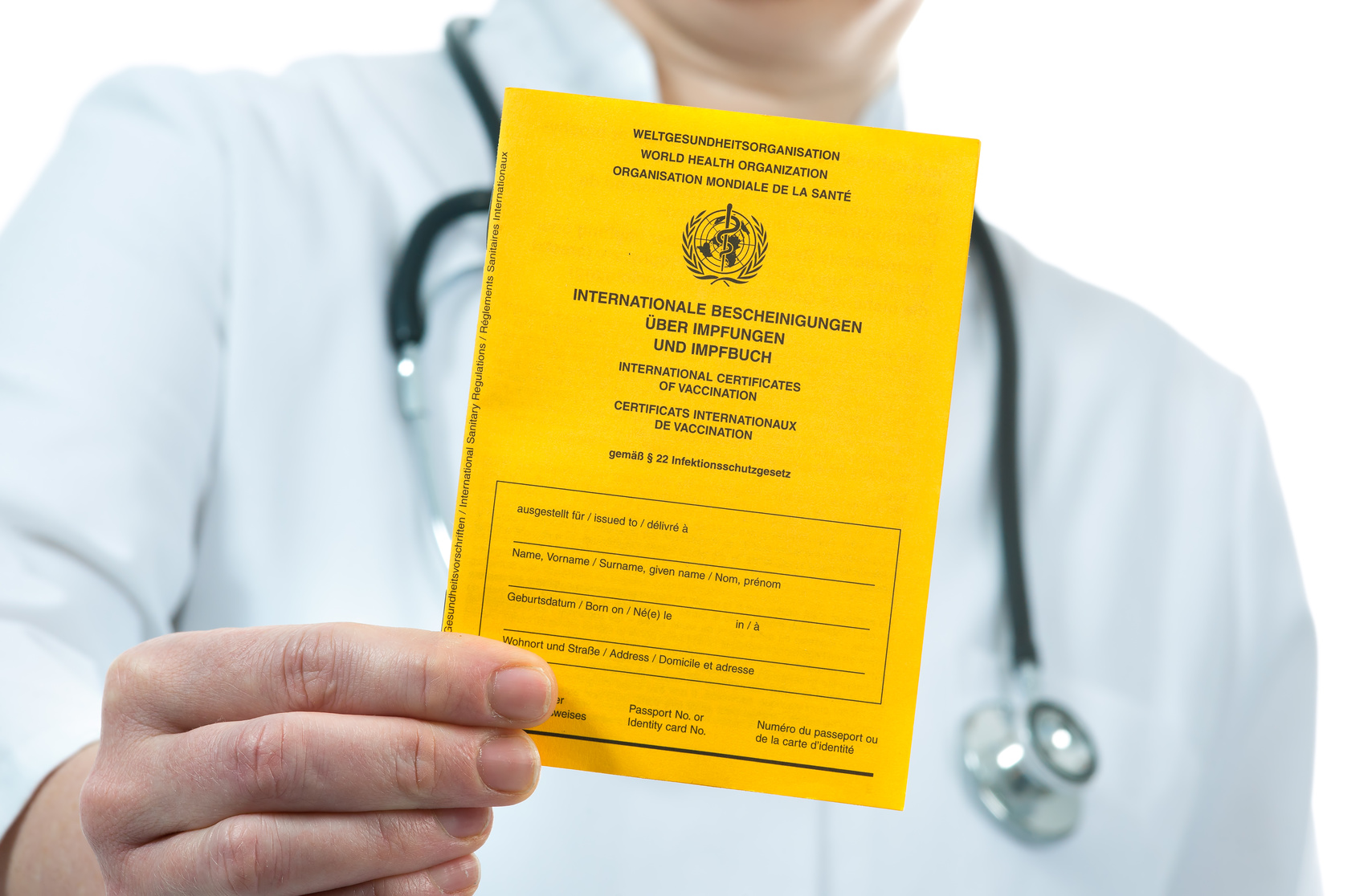
Yellow Fever
In Tanzania, there is no risk of yellow fever. If you are only travelling directly from the UK and back, it generally isn’t advised to have yellow fever vaccine. There is, however, a requirement for travellers to have a certificate of vaccination if they enter Tanzania from another country that has Yellow Fever. Bordering countries such as Kenya, Uganda, Rwanda, Burundi & DRC would all require a certificate. In this instance, a vaccination or a waiver certificate may be advised. It is best to speak with a specialist travel nurse, who will look at your route and access what vaccinations and certificates you would require.
Prevent Malaria
Whether you plan to visit Zanzibar or the mainland, all areas of Tanzania have a risk of malaria. Therefore, you should take anti-malarial medication. Malaria is spread by mosquitoes that are most active between dusk and dawn. A common question is whether or not you need to take them if you plan to trek Mount Kilimanjaro. Even though the risk of malaria is low in areas above 2,500m, the start and finish of the trek take you well below this altitude. In short, you should take medication to prevent it. You should take precautions to reduce the risk of being bitten in the first place.
Precautions include:
- Wear long, loose clothing
- Wear plenty of mosquito repellent with a minimum of 50% DEET
- Use clothes spray containing permethrin – you can spray before you travel for short-duration trips
- Sleep under a mosquito net
See our Ultimate Bug Kit for everything you need to keep the mosquitos at bay.
Climbing Kilimanjaro
If you are trekking Kilimanjaro, make sure your pre-travel plans take this into account. Trekking is physically demanding and exposes you to the risk of altitude sickness. The summit of the peak is 5,895m and treks can take anything from 5-9 days. Altitude sickness is unpleasant. Not only this but it can develop into something more serious and become life-threatening. Take time to acclimatise. This will reduce your risk of developing altitude sickness. Ideally, choose a longer trek. A slower ascent over more days will reduce your risk considerably. Alternatively, you can get a prescription of acetazolamide (Diamox) to aid the process. Speak to a specialist travel nurse about this at your pre-travel consultation. Don’t let altitude sickness ruin your trip.
Book your travel appointment today
By Anna Chapman | Travel Nurse | August 2019
The Southern African nation, Mozambique is gaining popularity amongst the adventure traveller community. Often referred to as ‘The Pearl of the Indian Ocean’, it is well off the usual tourist trail of Africa. Mozambique offers rustic beaches, delightful architecture, superb national parks, and plenty of diving opportunities.
Many choose to start their adventure exploring the capital city, Maputo. It is easy to understand why. It is rich in culture with beautifully preserved Portuguese colonial architecture. You could easily spend a week enjoying the hospitality of the friendly locals, eating the delicious food and partying the night away. Maputo is a largely-underestimated African capital city.
Mozambique is also known for having some of the most pristine dive sites in the world. Tofo is arguably one of the greatest places on Earth to see megafauna marine life. Crystal clear water provides perfect visibility to view the abundant marine life. The beautiful tropical Islands of the Bazaruto and Quirimbas Archipelagos are some of the most romantic and secluded beach destinations in the world – ideal for honeymooners.
Whatever your holiday entails, ensure you read out top travel tips to stay healthy in Mozambique.
Vaccinations
Travellers should ensure they are up-to-date with their routine immunisations including measles, mumps and rubella (MMR) and diphtheria-tetanus and polio (DTP). Additional travel vaccinations are advised including hepatitis A, typhoid, rabies and hepatitis B. It’s best to speak with a travel nurse about any specific travel vaccinations you may need in a pre-travel consultation.
For more information on our vaccines, please visit our, travel and wellness vaccination pages.
…What about Yellow Fever?
Yellow Fever is a viral haemorrhagic illness spread from the infected bite of the Aedes mosquito. Whilst it can occur in parts of Africa, there is no risk of Yellow Fever in Mozambique. Therefore, travellers do not need to be vaccinated.
The only exception to this will be for travellers who are entering Mozambique from a country which does have a risk of the illness. In this case, it is best to speak to a travel nurse to see if you require the vaccine. If you do, you will need to be in possession of a Yellow Fever Vaccination certificate as a condition of entry. Ask your travel health specialist for advice.
…And Polio?
Polio is a viral infection. As it is contagious, you can get polio from contact with an infected person. In addition, consuming food or water that has been contaminated by a person with poliovirus also puts you at risk. There has been a worldwide effort to eliminate polio, which is proving highly successful. However, Mozambique still remains at risk due to vaccinate-derived circulating strains. All travellers should ensure they are up-to-date with their polio immunisation. The polio vaccine is a combination vaccination, given with diphtheria and tetanus. It provides protection for 10 years.
If you plan to stay for longer than 4 consecutive weeks, it’s advised that your polio vaccine be administered within the last 12-months. You should also have the dose recorded on an International certificate of vaccination prophylaxis card as proof of immunisation. Furthermore, long-term travellers to Mozambique may be required to show this when they leave the country, as proof they have been immunised.
Malaria
All of Mozambique has a risk of malaria. Malaria is an infection spread by the Anopheles mosquitoes which are most active during dusk till dawn. You should take strict precautions against mosquito bites. This includes wearing long loose clothing and using an insect repellent with a minimum of 50% DEET. You can reduce the risk of indoor mosquito activity with the use of plug-in vaporisers. Plus, sleeping under a mosquito net can help reduce night-time bites.
We recommend taking antimalarial medication for the duration of your trip. As there are different options available, it’s best to speak to a travel nurse to find the best option for you and your family.
See our Ultimate Bug Kit.
Special precautions post-Cyclone Idai
Cyclone Idai battered the coast of Mozambique on the 9th March 2019. The storms brought heavy rains, winds and flooding. As a result of the initial impact alone, there were hundreds of fatalities. The storm created many serious health risks. Firstly, like most natural disasters, the storm has displaced a huge number of local people. Which as a result, will increase the risk of diseases spreading. Secondly, it has placed a strain on the countries structural and health infrastructure. Which as a result, and can lead to further flooding and increases the risk of water-borne infections such as cholera. Thirdly, the increase of water has led to an increase in breeding sites for mosquitoes. Therefore, there is an increased risk of malaria and other mosquito-transferred diseases.
Although the risk for tourists will be much lower than that of the local population, extra precautions to avoid infectious diseases should be taken. You should pay extra attention to the food and water hygiene you consume. This will minimise the risk of you getting a diarrhoeal illness.
If you are travelling to an area with a known outbreak, the Cholera vaccine can be considered. Similarly, those undertaking humanitarian work or those with inadequate access to safe water and sanitation should also consider the vaccine.
Book your travel appointment today
By Anna Chapman | Travel Nurse | July 2019
Marrakesh is a former Imperial City and the heart of Morocco. Whether you plan on visiting the medinas of Marrakesh or branch out to the sands of the Sahara or the heights of the Atlas mountains, ensure you follow our top travel tips to stay healthy.
Vaccinations
All travellers should ensure they have received vaccinations against Hepaitis A and diphtheria-tetanus and polio. Vaccinations against typhoid should be considered for those who cannot guarantee safe food and water during their trip, Hepatitis B and Rabies vaccinations can be considered for some travellers, especially those travelling to more remote locations.
Water
Travellers should be careful when dining in Morocco. This will help to prevent food and water-borne illnesses. You should avoid drinking tap water, and stick to boiled water, or bottled sealed water. Those who are trekking may wish to take a water bottle with a filter or a supply of chlorine dioxide tablets to make water safe when in remote locations.
Food Safety
Stick to the mantra of cooking it, peel it, boil it, forget it. If you cannot cook, peel or boil what you plan to eat or drink, it is probably safest to avoid consuming. Food contaminated with local water, such as salads are considered high risk and best to be avoided. Ensure all food is cooked thoroughly and served straight away. Avoid buffet items which may have been sat for long periods of time and could be contaminated. You can also purchase our worldwide gastro kit.
First Aid
The availability of health care and first aid supplies are limited in Morocco. Whether you are visiting the median of Marrakesh or ambling around the Atlas, taking a good first aid kit with you is essential – click here to buy online now.
Basic provisions include pain relief, plasters and medication to treat an upset stomach, such as loperamide and oral rehydration salts. If you take prescription medication to ensure you pack enough and carry the prescription with you.
Altitude
The peak of Mount Toubkal exceeds 4,000m and can be summited in 5-7 hours. High altitude and fast ascent rates can put travellers at risk of altitude sickness and acute mountain sickness. The risk can be reduced by ensuring you stay hydrated, plan a slow ascent and factor in some acclimatisation days. Acetazolamide (Diamox) can be used to help aid the process, speak to a travel nurse about this at your pre-travel assessment.
It is always best to seek travel advice before any holiday. A pre-travel assessment is quick and easy, vaccinations and prescriptions can be given within a single appointment and any follow-up treatments to complete courses arranged for a convenient time straight away.
Book your travel appointment today
By Anna Chapman | Travel Nurse | April 2019
Senegal is one of West Africa’s most visited countries; it is considered one of the most stable democracies in Africa, which is probably why it is more popular than it’s neighbouring countries. Senegal offers the hustle and bustle of Dakar, the sand dunes of the Lompul Desert, the clear waters of the Casamance and tropical backwaters of the Sine-Saloum Delta. Unfortunately, a tropical environment comes with tropical diseases, especially ones that fly!
Don’t wing it with your health, follow our top travel tips to stay healthy and have a bug-free break …
Sleeping Sickness
Sleeping sickness, also known as “human African trypanosomiasis”, is caused by the tsetse fly, which is native to the African continent and generally active during the day. If an infected tsetse fly, which is carrying the parasite, bites you, it can cause acute trypanosomiasis. Sleeping sickness infects the brain causing confusion, disturbed sleep (hence the name) and can be fatal if not treated.
Malaria
Malaria is prevalent throughout the whole of West Africa, including Senegal. It is spread by the bite of an infected Anopheles mosquito. Generally, these mosquitos bite most often during dusk til dawn. All travellers to Senegal should take anti-malarial medication and take preventative measures against mosquitoes.
Yellow Fever
Yellow Fever is a virus spread by the Aedes mosquito, that is most active from dawn till dusk. Catching Yellow Fever can be fatal but can be prevented by vaccination. The vaccination gives a lifetime of protection, however, it is not suitable for everyone and a comprehensive risk assessment should be sought from a travel clinic. Additionally, there is a requirement to be in possession of a valid Yellow Fever certificate when entering Senegal from another infected country, especially those who plan onwards travel to Gambia or Guinea-Bissau.
Zika Virus
Zika Virus is spread by the Aedes mosquito which commonly bites during the day in urban settings, such as Dakar and St Louis. The majority of people who are infected with Zika virus have no symptoms, but if contracted during pregnancy or close to conception it can cause Congenital Zika Syndrome. Currently, there is no vaccination nor cure for Zika virus infection and strict precautions against mosquitoes should be taken.
Best prevention to banish those bugs?
- Wear long loose clothing and cover-up. If the insects can’t bite you, they can’t transmit their diseases to you.
- Use a minimum of 50% DEET spray on any exposed areas of skin and reapply regularly
- Sleep under a mosquito net
- Treat clothes with permethrin
- Ensure you receive a travel consultation prior to departure to receive the appropriate pre-travel vaccinations and medications against malaria and Yellow Fever
- You can purchase one of our Ultimate Bug Kits to help protect yourself
Book your travel appointment today
By Anna Chapman | Travel Nurse | February 2019
With Ebola remaining a cause for concern in the Democratic Republic of Congo (DRC), Johanna, one of our travel nurses who’s had first-hand experience during the 2014 outbreak, looks at the differences between the current outbreak compared to her experience.
During the 2014 outbreak, I was stationed in an Ebola treatment centre in Sierra Leone. The UK government responded to the Ebola outbreak by sending out British medical professionals to help support the Ebola response unit. It was a time in my life when I didn’t have responsibilities that tied me to a fixed geographic location, alongside having the necessary skills that could make a difference, so there really didn’t seem a reason not to go to help out.
The current outbreak is happening in the Democratic Republic of the Congo (DRC).
The General-Director of the World Health Organisation recently visited Ebola-affected areas in the DRC and reported:
‘Since the outbreak began in August 2018, there have been 608 cases and 368 deaths in North Kivu and Ituri provinces. To date, more than 54,000 high-risk contacts and frontline responders have been vaccinated, and almost every new patient receives one of four investigational treatments, something which was never previously possible during an Ebola outbreak.
The main challenges are the security environment, pockets of mistrust among affected populations, and poor infection prevention and control in many public and private health facilities. Under the government’s leadership and working collaboratively with UN and NGO partners, WHO is committed to addressing these challenges and ending the outbreak.
There are many factors that make this current outbreak vastly different to the 2014 outbreak:
- Regional Stability
The political situation in the DRC is unstable which has led to less infrastructure to support relief efforts and virus control activities. Healthcare providers may be at risk of violence which makes a difficult job even harder. Civil unrest has lead to more than 1 million people being forced to leave their homes to escape potential violence, this mass movement of people means the spread of the virus is harder to control. This creates a very different context to the one we were facing in Sierra Leone.
Source: The New England Journal of Medicine: New tools in the Ebola arsenal, United Nations High Commissioner for Refugees: Spiralling violence puts millions at risk in Ebola-hit eastern DRC. August 24, 2018
- Public Awareness
At the beginning of the 2015 outbreak, there was very limited public awareness of the Ebola virus and how it is spread. The understanding of Ebola transmission was minimal and communities were unaware that some traditional practices could be increasing the risk of infection. The outbreak in 2015 involved a very steep learning curve for all involved. The many lessons learnt then will mean that there is more knowledge, resources and information to fight the virus this time around.
According to The Lancet:
In 2016, Guinea, Liberia, and Sierra Leone succeeded in interrupting the longest epidemic of Ebola virus disease in global history…Control of the epidemic was primarily achieved by implementation of effective and coordinated public health measures that involved rapid identification, isolation of cases, contact tracing, and isolation of contacts.
Source: The Lancet: Prevention of Ebola virus disease through vaccination: where we are in 2018
- Ebola Vaccine
One of the major developments in the armoury of tools to fight Ebola is the development of an Ebola vaccine. This was only a dream in the 2015 outbreak but it is a reality for the healthcare professionals currently working in the DRC. Although still in its early stages, the Ebola vaccine in use in the DRC is showing very promising results. In May and June of 2018 more than 3,000 people were vaccinated as part of the WHO response to the Ebola virus.
Source: The Lancet: Prevention of Ebola virus disease through vaccination: where we are in 2018
- Safer working conditions
Treating patients in the 2015 outbreak was very difficult for many reasons. One of the hardest things was finding a balance between safety from infection and being able to provide effective and compassionate care. Working in the hazmat suits kept us safe from transmission of the disease, but working in 40-degree heat wrapped up in layers of plastic was very inconvenient for many reasons. Being so hot meant that we could not spend as much time with our patients as we would have liked because there were limits to how much time we could spend in the Red Zone for our own safety. Being so covered up also made it harder to form human relationships with our patients (which is the cornerstone of nursing practice) because it was difficult for our patients to distinguish between us and any chance of communication through facial expressions was impossible.
The current outbreak has seen the introduction of air-conditioned Ebola treatment cubicles which eliminates the need for such restrictive time constraints whilst also offering a healthier environment for medical professionals.
According to the New England Journal of Medicine:
With such cubicles, health care workers can provide intravenous fluids and therapeutics through specialized ports and are thus freed from the burdensome personal protective equipment used during the 2014 West African outbreak to spend more time with their patients. Medcins sans Frontieres (MSF, or Doctors without Borders) continues to be a leader in developing safe care for patients with EVD provided in structures that can be rapidly erected using local resources.
Sources: The New England Journal of Medicine: New tools in the Ebola arsenal
- Containment of the outbreak
This outbreak is considered a contained case with little spread outside of the outbreak origin. The 2015 outbreak quickly moved across international borders and therefore was a cause of much concern for the international community. People are obviously anxious about the spread of Ebola, however, at this stage, the risk is minimal within Europe. There are many precautions taken by all those returning to the UK from affected areas.
When returning from Sierre Leone, I was subject to 3-week quarantine monitored by Public Health England during which I had to report my temperature to them twice a day and there were numerous restrictions on what I could and couldn’t do such as, I couldn’t work in hospitals, I could get my hair cut but not shaved, I couldn’t get a pedicure nor go to places with large amounts of people including football matches and music concerts. Everything was extremely well monitored and the public was kept incredibly safe from infection. These practices are no-doubt to be in place for this current outbreak as well.
______________________________
If you have any concerns about travelling to parts of Africa, you can book a travel consultation for the latest travel health advice for your destination.
By Johanna Bosowski | Travel Nurse | February 2019
Our travel clinic nurse, Anna Chapman, has just returned from an amazing two weeks travelling around South Africa.
Many items were ticked off her bucket list including a stay in Cape Town, a visit to the Winelands of Franschhoek and Stellenbosch and a stopover in Hermanus and Touwsrivier in the Western Cape. It was a busy trip!
Anna shares her top travel health tips for staying healthy on the road.
TRAVEL VACCINATIONS ARE A MUST!
Make sure you get your travel vaccinations in plenty of time prior to travelling. Book a travel consultation appointment 4-6 weeks before your flight to discuss health safety and vaccination recommendations. Travellers with a pre-existing health problem should book an appointment with a GP even earlier. Often vaccines are left to the last minute and not prioritised but it is important to protect yourself against life-threatening diseases.
South Africa is a huge country and the vaccinations you need will depend on exactly where you plan to stay, visit and what you plan to do. Depending on where you enter the country, high-risk areas may require you to provide proof of yellow fever vaccination on entering.
The far eastern provinces and game parks of South Africa pose a risk of malaria. If you are planning a safari, find out which reserve you will be visiting to determine if you will require anti-malarial medication. There are numerous game parks in the east and centre of the country which are malaria free. We also recommend our Ultimate Bug Kit to help protect you from mosquitos.
Other vaccinations to consider; hepatitis A, polio and typhoid.
BE MINDFUL OF THE WATER DROUGHT
There has been a severe drought in South Africa, particularly in the Western Cape. At present, there are active water restrictions in place throughout. You should be mindful of water consumption and comply with local restrictions.
As a result, many toilets no longer have running water to wash your hands with and instead offer hand sanitiser. Make sure you take your own hand sanitiser with you just in case the public facilities run out. Good hand hygiene is key to preventing upset stomachs otherwise known as travellers’ diarrhoea. Travellers should consider booking the drinkable vaccination, Dukoral, which protects against cholera and travellers’ diarrhoea. It would probably be worthwhile in taking a diarrhoea treatment pack with you on your travel as well.
TRAVEL SICKNESS
The Western Cape and the Cape of Good Hope is known for stormy seas. If you are prone to travel sickness and plan on taking any boat trips, make sure you pack seasickness medication. Whale watching is a popular tourist activity, and even the short boat ride from Cape Town to Robben Island can be rough enough to make those susceptible to seasickness feel queasy.
OVERNIGHT FLIGHT RISKS
Most travellers enter South Africa in a direct overnight flight from the UK. With only an hour time difference from the UK, people use this flight to catch up on sleep before they land. Sitting immobile for prolonged periods can put you at risk of a deep vein thrombosis. Minimise the risk by staying hydrated, keeping mobile and wearing compression stockings throughout the flight
IMPORTANT AFTER TRAVEL APPOINTMENTS
Travellers returning with diarrhoea should seek medical care if symptoms do not improve within three days. At Fleet Street Clinic, we have an on-site PCR machine which is able to identify the cause of travellers’ diarrhoea to produce a rapid report. Our GP’s can identify the exact cause, provide an accurate diagnosis and prescribe the correct treatment.
Medical advice should be sought earlier for those who are elderly, children and other vulnerable travellers if they are showing signs of dehydration.
______________________________
Our experience team of travel nurses can help advise with any queries or more information on South Africa.
Book your travel appointment today
By Anna Chapman | Travel Nurse | September 2018
Madagascar
Madagascar is a large country off the south east coast of Africa. It is well known for its rainforests, hiking and diving, beaches and reefs.
Make sure you are aware of what you need, such as visas, vaccines and other medical requirements.
Check your flight route
You may need a Yellow Fever certificate. Whilst most flights involve a change of plane in Paris, some flights route via Nairobi, Kenya. If you have a long lay over in Nairobi you will be required to provide on entry to Madagasgar, a valid Yellow Fever certificate.
Don’t risk rabies
Rabies is a virus found in mammals and is fatal if not treated promptly. Treating rabies can be difficult in Madagascar, but is made much simpler for those who receive rabies vaccinations prior to travel. If the focus of your trip is the mammals of Madagascar, rabies vaccinations pre-trip is strongly recommended.
Banish the bites
Make sure you wear plenty of insect repellent whilst away as Madagascar has several diseases that can be spread via the bite of a mosquito or fly. Insect repellent should contain at least 50% DEET. Anti-malarial medication is always advised for Madagascar. Protect yourself from mosquitos with our Ultimate Bug Kits.
Travel with Insurance
Ensure you take out comprehensive travel insurance before you go to Madagascar, and ensure that it covers you any activities you may have planned (such as scuba diving).
FLEET STREET TRAVEL CLINIC
Book your travel appointment today
By Anna Chapman | Travel Nurse | August 2018