Month: April 2019
Uzbekistan is home to spellbinding architecture and ancient cities. In terms of sights alone, Uzbekistan is Central Asia’s biggest draw and most impressive showstopper. Fabulous mosques, medressas and mausoleums are just some of the pulls for tourists when visiting Uzbekistan while more eccentric views can be seen at the fast disappearing Aral Sea and Nuratau Mountains.
Travel Nurse, Anna, shares her top tips on how to stay healthy during your trip to Uzbekistan.
Vaccinations
Ensure you are up-to-date with your travel vaccinations. The minimum advised for a trip to Uzbekistan is diphtheria tetanus and polio, and Hepatitis A. Typhoid, Hepatitis B and Rabies can be considered by some travellers. It is advisable to attend for a pre-travel assessment with a travel nurse 6-weeks before your trip as some vaccinations requires several injections to complete the course.
Food and water
Precautions against the dreaded traveller’s diarrhoea should be taken to prevent an upset stomach ruining your trip. Do not drink tap water in Uzbekistan, stick to bottled water or water that has been boiled. If you are trekking or visiting remote areas it’s a good idea to take either a water bottle with a filter or some chlorine dioxide tablets to make water safe to drink, should you not be able to find a shop with bottled water.
Sour milk dishes dominate the Uzbek cuisine. Cue caution if you want to try ‘kurt’, the famous fermented cheese balls. There is a risk of a bacterial disease called brucellosis that can be spread through unpasteurised dairy products such as cheese and milk.
Travelling further afield
Uzbekistan forms one of the countries on the old silk route. If you plan on a tour of the ‘Stans’ or attempting the whole Beijing to Istanbul route, you may need to consider other travel health precautions. Depending on your route, and also the time of year you intend to travel, you may wish to consider vaccinations against Tick-Borne Encephalitis and Japanese Encephalitis.
Altitude
Khazret Sultan, Uzbekistan’s highest peak stands at 4643m. Many popular walking and hiking routes such as Big Chimgan exceed over 3000m, making altitude related illnesses a hazard. Tips for reducing altitude sickness include a slow ascent route, keeping hydrated, ensuring that your sleeping altitude doesn’t exceed 500m per day. Diamox (acetazolamide) is a prescription medication that can reduce the symptoms of altitude related illness.
Book your travel appointment today
By Anna Chapman | Travel Nurse | April 2019
Marrakesh is a former Imperial City and the heart of Morocco. Whether you plan on visiting the medinas of Marrakesh or branch out to the sands of the Sahara or the heights of the Atlas mountains, ensure you follow our top travel tips to stay healthy.
Vaccinations
All travellers should ensure they have received vaccinations against Hepaitis A and diphtheria-tetanus and polio. Vaccinations against typhoid should be considered for those who cannot guarantee safe food and water during their trip, Hepatitis B and Rabies vaccinations can be considered for some travellers, especially those travelling to more remote locations.
Water
Travellers should be careful when dining in Morocco. This will help to prevent food and water-borne illnesses. You should avoid drinking tap water, and stick to boiled water, or bottled sealed water. Those who are trekking may wish to take a water bottle with a filter or a supply of chlorine dioxide tablets to make water safe when in remote locations.
Food Safety
Stick to the mantra of cooking it, peel it, boil it, forget it. If you cannot cook, peel or boil what you plan to eat or drink, it is probably safest to avoid consuming. Food contaminated with local water, such as salads are considered high risk and best to be avoided. Ensure all food is cooked thoroughly and served straight away. Avoid buffet items which may have been sat for long periods of time and could be contaminated. You can also purchase our worldwide gastro kit.
First Aid
The availability of health care and first aid supplies are limited in Morocco. Whether you are visiting the median of Marrakesh or ambling around the Atlas, taking a good first aid kit with you is essential – click here to buy online now.
Basic provisions include pain relief, plasters and medication to treat an upset stomach, such as loperamide and oral rehydration salts. If you take prescription medication to ensure you pack enough and carry the prescription with you.
Altitude
The peak of Mount Toubkal exceeds 4,000m and can be summited in 5-7 hours. High altitude and fast ascent rates can put travellers at risk of altitude sickness and acute mountain sickness. The risk can be reduced by ensuring you stay hydrated, plan a slow ascent and factor in some acclimatisation days. Acetazolamide (Diamox) can be used to help aid the process, speak to a travel nurse about this at your pre-travel assessment.
It is always best to seek travel advice before any holiday. A pre-travel assessment is quick and easy, vaccinations and prescriptions can be given within a single appointment and any follow-up treatments to complete courses arranged for a convenient time straight away.
Book your travel appointment today
By Anna Chapman | Travel Nurse | April 2019
So you’re back to work and the tree’s on its way back to the loft. Time to come through on all the New Year’s resolution bravado. Here are a few tips about how to do just that.
Create a plan
Decide what it is you’re wanting to achieve and tailor your program towards it. Do you want to lose weight? Get fitter? Tone up? All three? Don’t just choose the new fitness regime trend, think what you enjoy to do and go with that! You stand much more chance of continuing if you do. Identify times of day when you can exercise and which days you will do it. It’s much harder to stick to a regime that is just squeezed in when and if you have the time (not to mention inclination!)
Determine your readiness
Make sure you are mentally and physically ready to start, and more importantly ready to stick to, a regime. Check with your GP if you have any concerns about your health before you start. A good proportion of my new patients come from people who have caused injuries in the first few weeks, or even days sometimes, of starting a new regime. If you have any niggles, get them treated, and get advice on how to prevent them from recurring.
Be realistic
Set goals that are achievable and realistic. To lose a stone or be able to run 10k by Easter are realistic. To decide you are going to the gym every day before breakfast probably won’t last long. Fitness needs to be built gradually with a good base. Get advice on what exercise you need to do. Just running will help cardiovascular fitness somewhat, but needs to be part of a balanced all-around program if you want to be healthier generally. To maintain it, alone, running will also soon start to cause musculoskeletal problems.
Talk a friend into joining you
There will probably be no shortage of people thinking along the same lines as you. Teaming up hugely increases the chances of you both sticking to a program and makes it much more fun and less painful than trying alone. Even just planning together and talking about what you’re doing, (even if diaries don’t allow actually exercising together), is really encouraging.
Think long-term
Don’t look at this as a quick fix just to drop a few pounds. Take it easy and don’t rush. Tailor your plan around becoming more fit and healthy permanently. If you do it will help with so many other things, from energy levels to less aching joints or back, to stress relief and better sleep.
By Andrew Doody | Osteopath
Andrew is available for pre-exercise assessment, advice on exercise/regime planning, and diagnosis/treatment of outstanding or new issues, as well as advice on injury prevention. You can book an osteopathy appointment online.
As it’s backcare awareness week, let’s talk about back pain at work.
Back pain can be the result of heavy lifting, repetitive movement or simply by sitting at your desk all day.
We know how hard it is to live and work in pain and back pain is no exception. By now I’m sure we all realise that sitting for long periods is bad for you. But just how bad have our habits become? And what can be done about it?
Sitting in an office chair for long periods of time can wreak havoc on your lower back. In addition to many other joints and muscles. Simply stated, our bodies weren’t made to sit for prolonged periods of time. In fact, our bodies developed a heck of a long time before chairs were around at all.
According to research, the average office worker spends an average of 5 hours and 41 minutes per day sitting at their desk. The same study also found that those who sit longer at work are more likely to sit more outside of work as well.
Overall, sedentary jobs have increased 83% since 1950. With physically active jobs now only make up about 25% of the workforce. That’s 50% less than in 1950. Additionally, the average working week is longer. We now work an average of 47 hours a week, 164 more hours a year than 20 years ago.
On top of the time spent sitting in the workplace, on average, we spend 7 hours sleeping and 4.5 hours watching tv a day.
So should we be standing?
A recent study in the European Journal of Preventive Cardiology found that standing for almost six hours a day instead of sitting not only prevents weight gain — it can help people shed pounds.
They calculated that standing burned 0.15 calories more per minute compared to sitting. If an average person stood for six hours a day instead of sitting, they would burn an extra 54 calories a day. Some studies had it even higher.
In addition, muscle activity from standing is also associated with lower risks for strokes and heart attacks. Quite a few studies have shown that a single day of breaking up sitting with standing or short walks seems to have a beneficial effect on health parameters. Which include blood sugar control, blood pressure, and feelings of pain and fatigue.
However, before we all decide to stand all day instead, let’s look at the downsides. There’s a confusing array of conclusions from recent studies involving the health implications of standing vs sitting for long amounts of time. There have been studies, for example, that have concluded that people who primarily stand for long periods of time during the day, instead of lowering their risk for heart disease, maybe up to twice as likely to develop it. Perhaps long periods of standing are not the answer either. It has also been pointed out that standing for extended periods of time isn’t safe for all people, such as those with joint or vascular issues.
However, swapping out some sitting time for standing time is not only about heart disease.
One variable that makes sitting for extended periods damaging to the spine is the sustained contracture of the abdominal and hamstring muscles. This creates an imbalance. This, in turn, creates affecting the mechanics of the lower back. It also increases the load on the lumbar discs.
Using a standing desk, even for a portion of a workday, can minimise this imbalance. This helps maintain better spinal alignment and muscle symmetry.
So is a combination of sitting and standing the answer?
A recent study was performed where office workers of varying ages and body masses used a sit-stand desk where they alternated between sitting and standing throughout an 8-hour workday. The study found that the participants reported a 31.8% reduction in standing desk back pain when compared to sitting for the entire workday.
But just like sitting and leaning forward for extended periods can increase pressure on the back, the same applies to standing with poor ergonomics. Maintaining good posture and taking frequent breaks is the best way to ensure you’re standing or sitting optimally.
Try not to wear high heels (you can swap out for flats or slippers while at your desk if needed). Have the top of the computer screen at about eye level, and vary posture. When you’re in a sitting phase of your day make sure your chair and workstation have been fully ergonomically assessed. Discuss any conditions with your osteopath. They can advise how to adapt both the sitting and standing phases to suit you better. Have regular breaks from your desk altogether when you walk around the office.
And then of course if you really want to blow the budget there are treadmill desks…
If you’re experiencing back pain you can book an appointment with our Osteopath, Andrew Doody, online.
ADVICE ON TICK-BORNE DISEASE IN EUROPE
Tick-borne Encephalitis (TBE) is a viral disease that is spread by the bite of an infected Ixodes tick. It is estimated that the disease infects at least 13,000 people every year.
Symptoms can occur from 4-28 days post-bite and include fever, fatigue and muscle aches.
The virus can also go on to affect the brain and spinal cord, causing meningitis, with up to 20% of cases resulting in death. Unfortunately, there is no specific treatment for TBE.
TBE occurs in 3 main geographical locations:
European TBE – Western Europe
Siberian TBE – Urals, Siberia, Far-Eastern Russia and Finland
Far Eastern TBE – far Eastern Russia, China and Japan
Transmission of TBE occurs mainly during the summer months, mainly via wild vertebrate animals such as rodents. It can be transmitted either by ingestion of unpasteurised milk, or milk products from infected animals or by the bite of an infected tick.
If you’re travelling to affected countries during the transmission period, you are most at risk if you are doing outdoor activities such as hiking, camping and walking in forested areas where ticks are abundant.
Take the following precautions to avoid infection:
Wear long trousers and sleeves. Impregnating clothing with permethrin and using insect repellents such as DEET are also good ways of preventing tick bites.
Get vaccinated. Ticovac (and Ticovac Junior for children) is advised for travellers who may be at risk. It requires two vaccinations prior to travel, and the third dose after a year can provide up to 5 years protection.
Check your body for ticks -especially in the armpits, groin and behind the knees.
Remove ticks promptly and correctly and clean the bite site with antiseptic.
Fast Facts
| What | Tick-Borne Encephalitis |
| Where | Eastern Europe, Scandinavia, Siberia |
| When | Summer Months |
| How | Infected bite of a tick |
| Can it be prevented? | Yes – Vaccination and tick-prevention |
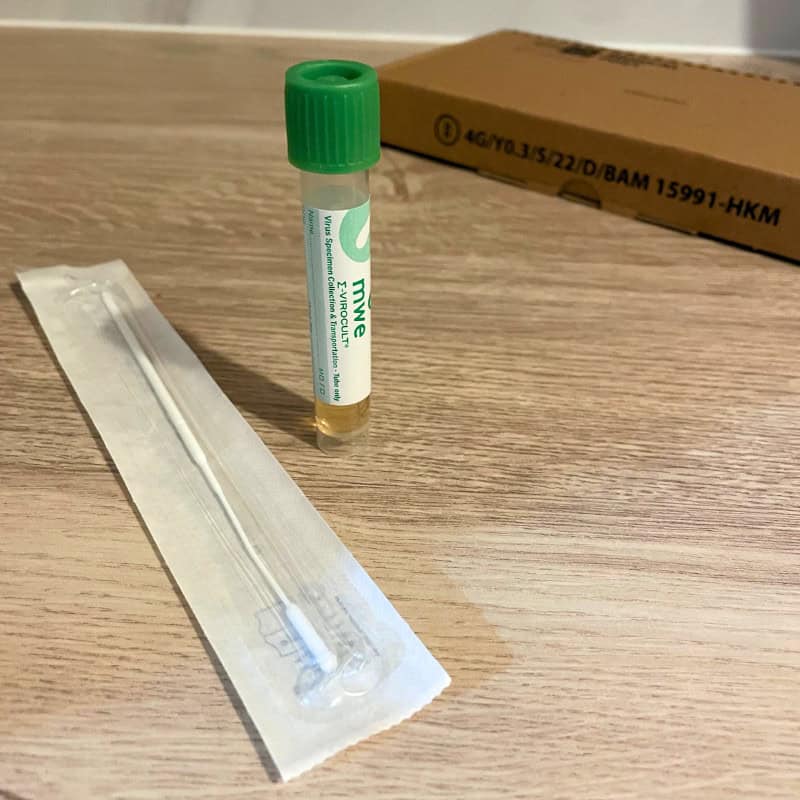
Tick Removal Tips
If you find a tick embedded on your skin you need to remove it, asap:
To remove a tick follow these steps :
- Use a pair of fine tweezers or a tick-remover
- Grasp the tick head as close the skin as possible
- Pull upwards at right-angles to the skin
Top tip: Avoid putting pressure on the body to avoid incomplete removal which may cause infection.
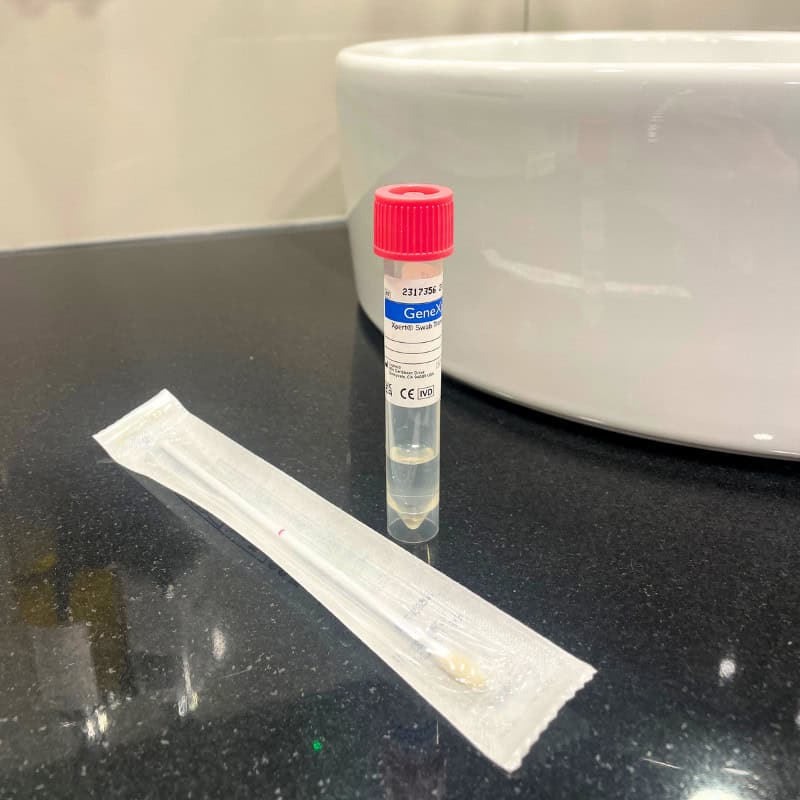
TICK-BORNE ENCEPHALITIS VACCINATION
There is a vaccination against tick-borne encephalitis (Ticovac and Ticovac Junior) which is highly effective against TBE. The primary schedule requires two vaccinations to be given 14 days apart, and a third dose to be given one year later. A booster vaccination is recommended after 3 years. The vaccination is suitable for adults and children over the age of one-year-old.
You can book a travel consultation appointment online to find out if you beed a tick-borne encephalitis vaccine for your next trip.
MUMPS OUTBREAKS IN UK UNIVERSITIES:
CASES OF MUMPS REPORTED AT A NUMBER OF UK UNIVERSITIES
Public Health England has confirmed they are urging students to get MMR vaccinations.
A number of cases of mumps have been reported in Nottingham and Exeter. The recent rise in teenagers and young adults who have not had two doses of the MMR vaccine are believed to have caused an increase in UK cases. Unprotected students are particularly vulnerable due to close living conditions. Students are being urged to ensure they have received the full two-dose MMR vaccine course to protect themselves against mumps.
A total of 241 suspected cases were reported, with 52 confirmed, across Nottingham Trent University and the University of Nottingham and 7 confirmed cases at Exeter University.
MUMPS VIRUS
Mumps is a contagious viral infection which causes swelling of the parotid glands.
Initial symptoms can be similar to a cold and include:
- Headache
- High Temperature
- Joint Pain
- Feeling Sick
- Tiredness
- Loss of Appetite
- Swelling of the face/neck
Mumps can result in some serious complications. It can cause temporary hearing loss in 1 in 20 people. Mumps can cause a rare but potential risk of encephalitis, which affects 1 in 1,000 sufferers and requires hospitalisation.
It is spread in the same way as colds and flu – through infected droplets of saliva that can be inhaled or picked up from surfaces and transferred into the mouth or nose.
A person is most contagious a few days before the symptoms develop and for a few days afterwards.
Some people suffer complications that can include inflammation of the pancreas, viral meningitis (inflammation of the brain), inflamed and swollen testicles in men and ovaries in women.
MEDICAL ADVICE FOR MUMPS
If you think you may be suffering from mumps, or are concerned about the risk of infection, please see your doctor straight away.
Those who have not had the MMR vaccine – or have only received one dose – regardless of age, should ensure they receive two doses of the MMR (measles, mumps and rubella) vaccine.
In order to keep virus’ such as mumps from spreading, a certain proportion of the population must be immunised, this is called the ‘herd immunity’.
Herd immunity is particularly important as not everyone can get vaccinated, but those who can are able to help people those who can’t. Some people are unable to get vaccinated because they’re too ill, too young or have an impaired immune system. When we vaccinate, we protect not only ourselves but also the most vulnerable members of our communities.
VACCINATION AGAINST MUMPS
The disease can be easily prevented with two doses of the MMR vaccine, that has safely and efficiently been in use since the late 1980s’.
Make sure you are up-to-date with your measles, mumps and rubella (MMR) vaccine. Although the NHS immunisation schedule offers the vaccine to children from 12 months of age, the MMR can be given from 6 months. If you have not had measles, mumps or rubella or if you have not had two doses of MMR, you may be at risk. Measles mumps and rubella are easily passed from person to person and can be a serious illness in adults as well as children. It is never too late to have the vaccine.
You can book an MMR vaccine online.
Links:
There is no denying that a marathon is an extraordinarily long distance to run and the effects it has on the body can be enormous.
No part of the body is more affected than your feet.
From the intense training regime to the 26.2 miles of constant pounding on hard concrete, it is crucial you look after your feet before and after the London Marathon.
There are many injuries that can be picked up whilst training such as blisters, callus build-up, cracks in the heal and ingrown toenails. Vigorous long-distance running can amplify these injuries but also cause nail damage and even loss of a toenail.
Caring for your feet post marathon is extremely important and visiting a podiatrist is advised to reduce the possibility of long-term damage which could be irreversible.
The key to post-race recovery starts with putting your feet up, relax them with some rest and then think about booking a podiatrist appointment roughly 3 days after your marathon. This will allow any soft tissue that has become inflamed to reduce.
If you have nail damage:
It is important that any pain caused by nail damage be investigated by a podiatrist, this could be from a loose nail to a build-up of pressure from a blood blister under the nail. Following trauma never force the removal of a nail or attempt ‘home-surgery’ as you are likely to create a nail bed infection and increase the risk of causing more long-term damage – leave this to a podiatrist.
If the nail damage isn’t significant nor causing any pain, you can protect it to reduce any further damage and monitor it’s healing. If the area doesn’t heal or begins to become painful it is advisable to book in with a podiatrist for medical help.
If you have excessive swelling and bruising:
These two symptoms can be a key indicator of a fracture, even in the absence of noticeable pain.
In some cases, adrenaline from running the marathon can conceal the pain caused by the fracture and the runner will push on and either ignore the warning signs or simply not register the pain. If swelling occurs for a prolonged period of time or a new bruise develops up to a couple of days post marathon, it is recommended that you seek advice from a podiatrist or visit a GP.
Post race foot care is an extremely important part of your post-race aftercare and will speed up your recovery time and in turn, will mean you can begin training for your next marathon quicker and with healthy feet.
If you would like to incorporate a podiatry appointment into your marathon training or book in for a post-marathon foot care appointment, you can book an appointment online.