Author: Marco Santoru
According to Menopause Support, approximately 13 million peri, current and post-menopausal people are living in the UK today.
This makes up a whole third of British women.
Despite making up such a large portion of society, a lot of women find themselves feeling ashamed, shunned or invisible due to their symptoms and the lack of discussion surrounding the subject of menopause.
What is menopause?
Menopause simply means no periods for 12 months and usually begins between the ages of 45-55, but it may start earlier. 80% of women are menopausal by the age of 54 years, so an average woman spends one third of her life being menopausal. In the lead up to menopause, women often experience symptoms of ‘perimenopause’. Changes in the menstrual cycle, hormonal fluctuations and ‘hot flashes’ can all occur as the ovaries begin to stop producing eggs. It is important to note that menopause is a natural transitionary period in life and is not a disease or illness.
What are the symptoms of menopause?
80% of women suffer some symptoms.
Meaning 20% of women have no symptoms at all, and of the 80 % who do suffer some symptoms, only 25% want or need treatment.
Some of the physical symptoms of menopause may include, but are not limited to:
- Night sweats
- Hot flushes
- Dizziness
- Fatigue
- Headaches
- Recurring UTIs
- Stiff joints, aches and pains
- Heavy periods
- Insomnia
- Itchy skin
- Osteoporosis
- Weight gain
Menopause is not only characterised by physical health symptoms, but mental health can also be affected by it too.
Some symptoms might include:
- Anxiety
- Memory loss
- Depression
- Reduced concentration
- Brain fog
How can I manage symptoms for menopause?
A healthy diet and regular exercise, alongside simple lifestyle changes, may improve some symptoms and are important parts of the toolkit in dealing with menopause. Reducing nicotine, alcohol and caffeine intake further assist in reducing symptoms as well.
‘Phytoestrogens’ also help, and these are found in foods like soya protein, beans, yams and nuts. These non-hormonal treatments should always be tried first before hormonal treatments like HRT, which top up hormone levels.
World Menopause Day
World Menopause Day is recognised every year on October 18th to attempt to break the stigma around menopause and highlight the support available to women when they’re experiencing symptoms.
This year’s theme is based on HRT and the various pros and cons.
HRT works by replacing the hormones lost in the menopause process and can relieve symptoms of menopause to a manageable degree. Many women see it as a necessity for managing their menopause symptoms.
However, studies have shown that HRT can slightly increase the risk of breast cancer. This may sound concerning but the risk reduces when using oestrogen only HRT, rather than combined. HRT for managing menopause is an ongoing discussion in the medical field, but a lot of women experiencing menopause find the benefits outweigh the risks, and your GP will be able to advise whether HRT is the right solution for you.
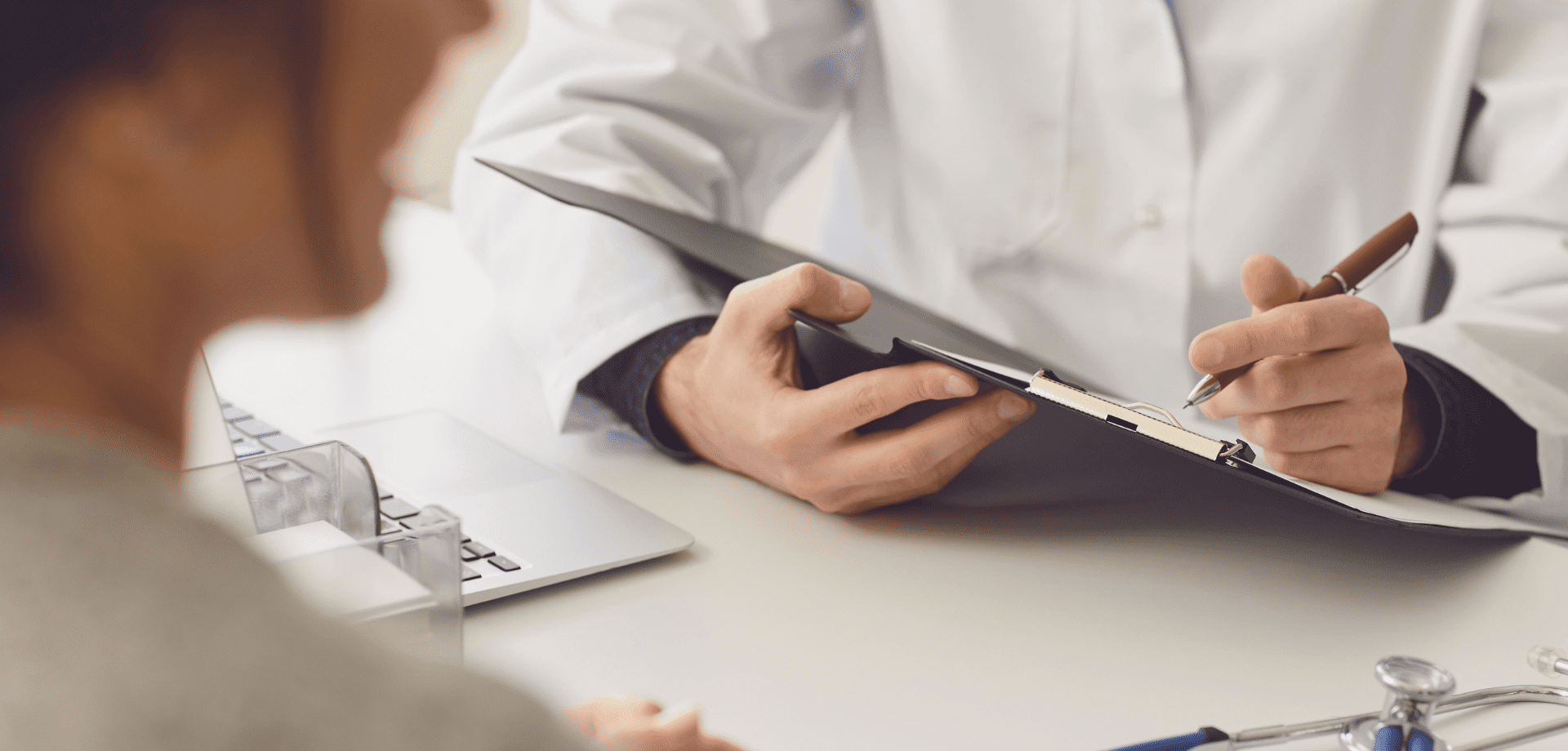
How can Fleet Street Clinic help me?
If you think that you are beginning to experience symptoms of perimenopause or are suffering with your current symptoms, it may be time to book a GP appointment to discuss your menopause and see how we can help you.
Menopause can be a scary transition, but we want to do everything we can to make it as easy as possible for you.
Book a GP appointment today and let us support you.
More information:
Here at Fleet Street Clinic, we have had many stool samples come through our laboratory. One recent clinical case using our in-house Full Gastrointestinal PCR Panel, presented unprecedented results.
Patient overview:
- 51-year-old patient
- Travelled to and from Pakistan for a trekking trip
- The patient presented with a history of severe diarrhoea
- Symptoms recorded: erratic bowel movement and weight loss.
Test results:
The PCR result came back quicky as positive for four pathogens:
- Cyclospora cayetanensis,
- Enteroaggregative E. coli (EAEC),
- Enteroinvasive E. coli (EIEC)/Shigella,
- and Enteropathogenic E. coli (EPEC)
This is highly unusual and it is little wonder why our patient was feeling so unwell with severe symptoms.
Our Biomedical Scientist, Jenny Reyes commented; “This is my first time in all of my time as a Biomedical Scientist to encounter such a result with four pathogens presenting all at once.”
Without our GI PCR test, this patient may have undergone many tests to identify the cause and may not have identified that the symptoms were the result of four simultaneous pathogens causing a mixed infection.
The advantage of a panel PCR test is its ability to identify the exact cause, enabling targeted treatment.
In this case, the clinician overseeing this patient’s care was able to tailor treatment to address all four identified pathogens simultaneously with precision.
Without this technology, diagnosing a mixed infection could have taken significantly longer, requiring multiple different tests to pinpoint each cause.
This would have increased the risk that only one pathogen would have been identified, leaving the symptoms caused by the others untreated even after addressing the diagnosed cause.
We encourage all patients with unexplainable gastrointestinal symptoms to consider the GI PCR Panel. It really does offer faster, more targeted care and can identify mixed infection with ease!
More information on our GI Panel:
Our Gastrointestinal Panel Test delivers accurate and reliable results quickly, often within a matter of hours.
It is capable of detecting any of the 23 commonest pathogens that cause diarrhoea – such as E. coli, campylobacter, norovirus salmonella, shigella and giardia, from a single stool sample – all that’s needed is a simple swab.
This supports our rapid diagnostic process, clinical management and educated treatment decisions which improve overall patient outcomes.
Learn more and book today
The summer holidays will fly by and be over as quickly as they began, much to your relief, but probably the disappointment of your kids! Unfortunately, alongside the general back to school chaos, September also brings with it the start of the flu season.
Flu season not only means that people have to take time off of work due to being ill themselves, but parents often have to take time off work to look after their children who have the flu, because schools are rife with superspreaders. It seems that the best solution to the frustrating effects of the flu on school and parenting life is to nip it in the bud early enough in the season for immunity to make a significant difference.
This is where the flu vaccine comes in.
The flu vaccine comes in two forms, the traditional syringe-administered jab, and a nasal spray vaccine. While the nasal spray vaccine may be the preferred administration tactic for parents of children who don’t like needles, supply issues have resulted in limited availability, and it may still be worth considering the alternative.
When might the jab be preferable?
The nasal spray vaccine is protective and an excellent choice, but is not suitable for everyone. It is a live vaccine, and so cannot be administered to children who are immunocompromised or who live with anyone who may be immunocompromised. It is also unsuitable for anyone with bad asthma, since it may trigger an attack. The injected vaccine is not a live vaccine and is an obvious solution for a lot of people.
The nasal spray vaccine contains traces of gelatine and egg, and so may be unsuitable for vegetarians, vegans, Muslims or those with a severe egg allergy. There is a cell-culture based injectable vaccine that is egg-free, which may be a more acceptable alternative.
The nasal spray vaccine can only be given from age two onwards. However, if there is a special reason for needing to vaccinate your child at a younger age than this, the standard injectable vaccine can be given from the age of 6 months. (The best way to protect babies younger than this is by vaccinating mums during pregnancy.)
For the past three winters, the nasal spray vaccine has been in limited supply. It has not been available privately but only through the NHS, and supply issues have resulted in extended delays. By contrast, injected vaccines have been available reliably from September onwards.
A well-timed dose of the injected vaccine, early in the season, may be a better option than the uncertainty of a delayed dose.
At the Fleet Street Clinic, we have been happy to offer the nasal spray vaccine previously but having been unable to obtain reliable supplies for the past three years, we will not be offering it this season.
If you decide to book the injected flu vaccine for your child this winter, you can rely on guaranteed supplies as well as our expertise in vaccinating babies and children of all ages.
__________________________
24/25 Winter Flu Vaccination Pricing:
Cell-Based Quadrivalent Flu Jab – £42 – Suitable from 2 years
Standard Quadrivalent Flu Jab – £15 (while stocks last) – Suitable from 6 months old
Book Your Flu Jab Online Today
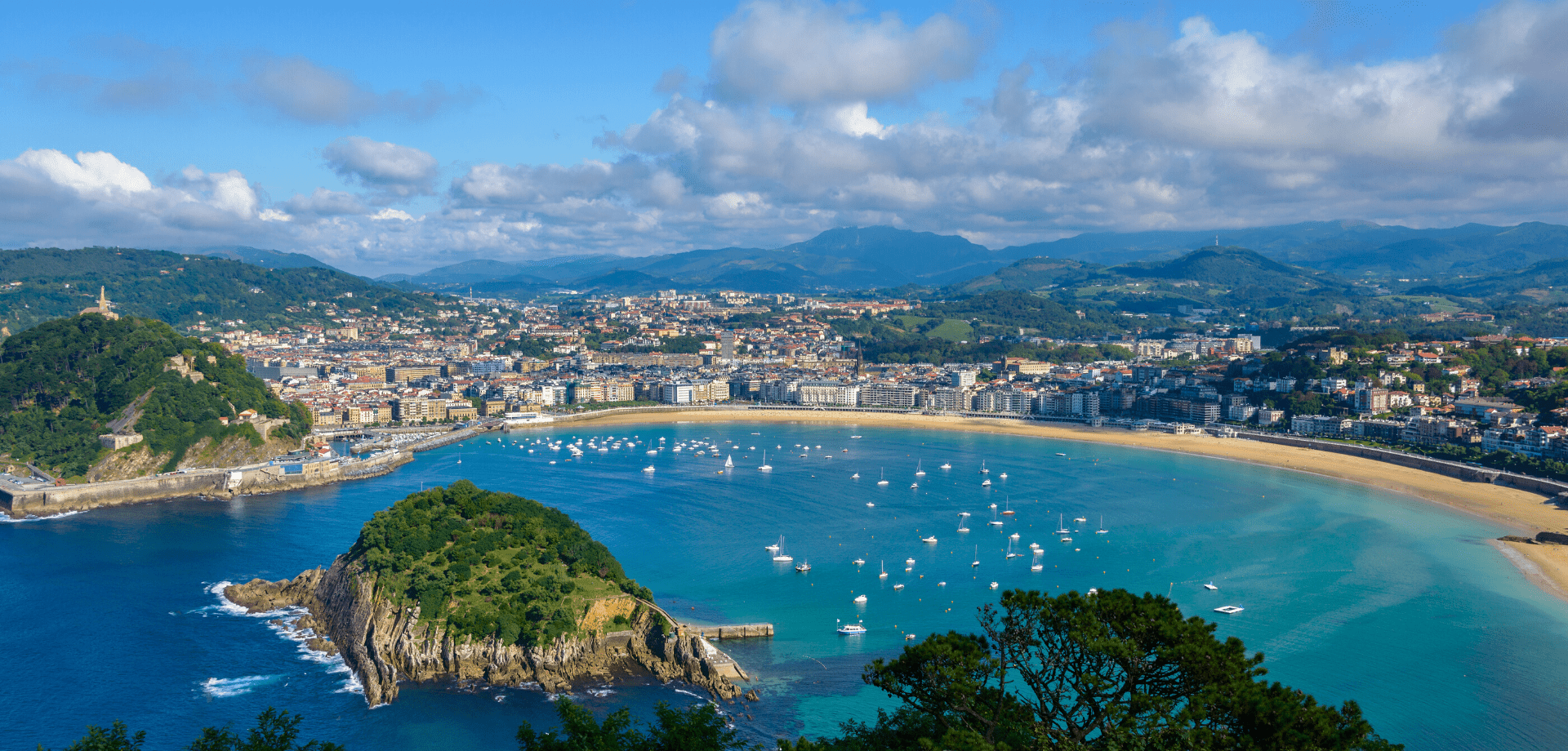
As a travel nurse based in London, I was concerned to hear the recent warning from health officials about the spread of tick-borne encephalitis (TBE) virus in several parts of the country. The UK Health Security Agency (UKHSA) has confirmed three cases of TBE virus in patients in Yorkshire, Norfolk, and on the border of Hampshire and Dorset. Further tests on ticks across the country have found that the disease, which was commonly found in parts of Europe and Asia until now, is now present in the UK. The experts have warned that it is unlikely that TBE virus will disappear, so it’s essential to establish a surveillance program.
Public health officials say the risk is low, but it’s essential for walkers to take precautions and seek medical help if they fall ill after being bitten, especially if by a tick.
As a clinic that specialises in travel, we are used to urging everyone to take precautions to protect themselves from tick bites anyway, but this news reinforces the importance of doing this at home as well as when travelling abroad. It is essential to cover your ankles and legs, apply insect repellent, and check clothes and your body for ticks, particularly when visiting areas with long grass such as woods, moorlands, and parks.
In most cases the TBE virus typically causes mild flu-like symptoms, but it can also lead to severe infection in the central nervous system resulting in meningitis or encephalitis a high fever with headache, neck stiffness, confusion, or reduced consciousness, and long-term impairment.
As a travel nurse, I think it is really important to educate people about the symptoms of TBE to encourage them to seek medical help immediately if they experience any of these symptoms, but also to emphasise the fact that infections are preventable.
Ticks are becoming more common in parts of the UK, mainly due to increasing deer numbers. They live in undergrowth and latch on to humans when they walk through long grass. It is thought infected ticks may have arrived in the UK via migrating birds. Scientists had suspected the virus had arrived in the UK in 2019, following a couple of cases, but complexities involved in testing meant these could not be confirmed.
It’s crucial to emphasise the significance of vaccination for individuals who are considered of a higher risk. You are much more likely to catch TBE if you work outdoors or if you enjoy outdoor activities such as camping, hiking, dog-walking, countryside rambling and even jogging. Children playing outside may be especially vulnerable.
Vaccines can provide protection, and as there is currently no known cure for tick-borne encephalitis virus, those individuals who would be considered at higher risk are advised to be vaccinated as a precaution.
It’s worth noting that a vaccine is used routinely in areas of high incidence in Europe, and its advisable to consider vaccination for individuals with outdoor occupations in regions where the virus is prevalent.
For the general public the risk of contracting TBE is relatively low. Therefore, it’s essential to educate people about TBE and encourage them to take precautions to protect themselves from tick bites, particularly when travelling to areas where the virus is found.
Related services available at Fleet Street Clinic
Tick Borne Encephalitis Vaccination
For further reading, more news coverage can be found here:
Gov.uk – Tick Borne Encephalitis detection in England
The Times – Tick-borne encephalitis warning to walkers
The Telegraph – First cases of rare tick disease found in England
SPRING IS UPON US!
A time of longer days, shorter nights, flowers in bloom, and warmer weather allowing us to spend much more time enjoying the great outdoors.
This year, March 26th marks the start of British Summer Time when the clock springs forward 1 hour, increasing daylight, prolonging our evenings and our transition to Summer begins.
Spring is the time of year when we emerge from our winter hibernation and seek more time in the fresh air, the outdoors, in nature and with friends and family.
There are so many health benefits that Spring has on our physical and mental well-being.
But in what ways specifically is Spring good for our health?
1. Spring makes us feel more energised
There’s nothing quite like the feeling of the warm sunshine on our skin after a long, cold winter.
This small act of nature, in general, makes us feel more upbeat and positive and can quite literally give us a “spring in our step!”. Exposure to natural light is thought to increase the brain’s release of a hormone called serotonin. Serotonin is associated with boosting mood and helping a person feel calm and focused with a more optimistic outlook to life.
With sunlight and sunshine increasing, spring is a natural positive energiser.
2. Spring weather encourages us to be more active
With the weather improving and the temperature rising it encourages us to get outdoors and be more active. That doesn’t mean we’re all inspired to run a marathon, but time outdoors is good for your physical and mental health.
Time in the fresh air can really help you to switch off from your daily stresses, reduce your blood pressure and improve your mood.
Spring encourages us to take up a new sport, go out for walks and spend more time being active.
3. Spring sunshine tops up our vitamin D
Getting enough vitamin D is essential for the typical growth and development of our bones, teeth and muscle health, as well as improving our resistance to certain diseases.
Extra daylight gives you more time to spend outside and soak up the nutrients from the sunshine. In Spring and Summer, most people are able to make all the vitamin D they need from the sunlight on their skin without the need for supplements.
4. Spring encourages us to clean our home
Spring is the perfect time of year to air out our homes, clean out the grime that has built up over the winter and make a fresh, clean start.
There are many health benefits to giving your house a deep spring clean, such as:
- Reducing your risk of allergies and asthma from the accumulation of dust or pet dander.
- By removing germs and bacteria, especially from hard-to-reach places, you are reducing your risk of getting sick in general.
- Visual clutter leads to mental clutter; so, doing a big tidy-up should see improvements in your mental health and even increase your productivity.
Is it time to spring clean your health?
Related services available at Fleet Street Clinic.
Cholesterol is a type of fat that is found in the blood and plays an important role in our bodies. However, high levels of cholesterol can lead to serious health issues, such as heart disease, stroke, and other cardiovascular problems. Unfortunately, cholesterol is often referred to as a “silent killer” as there are usually no symptoms and the first indication that something is wrong may be a heart attack. That’s why it’s important to have your cholesterol levels checked regularly.
Instant cholesterol testing only requires a short nurse appointment that provides you with both the test and the results during the same appointment. This type of testing makes it easy and convenient for people to understand their cholesterol levels and take steps to keep them under control.
Statistics from the National Institute for Health and Care Excellence (NICE) show that cardiovascular disease (CVD) is the leading cause of death in the United Kingdom, accounting for around 26% of all deaths. The most common type of CVD is coronary heart disease, which is caused by a build-up of fatty deposits in the arteries leading to the heart. High cholesterol levels can contribute to the formation of these fatty deposits.
By knowing your cholesterol numbers through instant testing, you can understand your risk of developing CVD and take the necessary steps to keep your levels under control. NICE recommends that all adults in the UK should have their cholesterol levels checked at least once every five years, or more frequently if they are at increased risk of CVD. Those at increased risk include people with a family history of CVD, smokers, people with high blood pressure, and people with diabetes.
To keep your cholesterol levels under control, it is important to make changes to your diet. This includes eating more fruits, vegetables, whole grains, and lean proteins, and reducing your intake of saturated and trans fats. You should also aim to maintain a healthy weight and be physically active for at least 30 minutes a day.
If lifestyle changes are not enough, medication may be required. The most common type of cholesterol-lowering medication is statins, which work by reducing the production of cholesterol in the liver. Statins are widely used in the UK and are safe and effective.
The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
Further reading on “NICE recommends wider use of statins for prevention of cardiovascular disease (CVD)”.
In conclusion, instant cholesterol testing provides an easy and convenient way to understand your cholesterol levels and take steps to keep them under control. Regular testing is important for everyone in the UK, especially those who are at increased risk of CVD. By knowing your numbers, making changes to your diet, maintaining a healthy weight, and being physically active, you can help keep your cholesterol levels in the healthy range and reduce your risk of developing serious health problems.
Related services available at Fleet Street Clinic:
Instant Cholesterol Testing with a nurse
Blood Tests at Fleet St. Clinic
Well Person Medical
GP Services
As a private healthcare clinic, our goal is to provide the best protection against pneumonia for our patients. One of the key tools in this fight is the pneumococcal vaccine. One of the latest advancements in this area is the Apexxnar vaccine. This 20-valent vaccine provides protection against 20 different serotypes of the pneumococcal bacteria, offering a more comprehensive defence against pneumonia.
We understand that choosing the right vaccine can be complex and that different patients may require different solutions. That’s why we recommend speaking with one of our healthcare providers to determine which vaccine, including Apexxnar, is best for you. They will consider risk factors such as your age, underlying health conditions, and previous vaccinations, to ensure you receive the most effective protection against pneumonia.
At Fleet St. Clinic, we believe in the power of prevention, and that the right vaccine can make all the difference. So, if you’re looking for the best defence against pneumonia, consider talking to us about the Apexxnar vaccine today.
Information about Pneumonia:
Pneumonia is a lung infection that can cause a range of symptoms, including:
- Cough: A persistent cough that produces mucus or phlegm is a common symptom of pneumonia. The cough may be dry or productive, and the mucus or phlegm may be green, yellow, or rust-coloured.
- Fever: Pneumonia often causes a high fever, which may be accompanied by chills and sweats.
- Shortness of breath: Pneumonia can cause difficulty breathing, especially during physical activity. The shortness of breath may be accompanied by chest pain or tightness.
- Fatigue: Pneumonia can cause extreme tiredness and weakness, making it difficult to carry out normal daily activities.
- Muscle aches: Pneumonia can cause muscle aches and joint pain, which may be mistaken for the flu.
- Chest pain: Pneumonia can cause chest pain, especially when breathing deeply or coughing.
- Nausea and vomiting: Some people with pneumonia may experience nausea and vomiting, especially if the infection is caused by a type of bacteria known as Legionella.
- Confusion or disorientation: Pneumonia can cause confusion or disorientation, especially in older adults and people with underlying health conditions.
It’s important to seek medical attention if you experience any of these symptoms, as pneumonia can be a serious and potentially life-threatening condition.
More information on pneumonia.
Who is considered “high-risk”?
Individuals considered to be at high risk for hospitalisation due to pneumonia include the elderly, young children, people with weakened immune systems (including people who have had their spleen removed), and individuals with underlying health conditions such as chronic heart or lung diseases, diabetes, and liver or kidney problems.
At the Fleet St. Clinic, we also regard anyone who has had a previous significant episode of pneumonia as likely to benefit from being vaccinated.
When is the best time for a pneumonia vaccine?
The best time to vaccinate against pneumonia depends on various factors such as the type of vaccine, the individual’s age, and underlying health conditions.
The pneumonia vaccine is not the same as the flu vaccine, as it doesn’t need to be given at a certain time of year.
For the pneumococcal vaccine, it is generally recommended to receive the vaccine once in a lifetime for most adults. Some individuals may need a booster shot, and this is determined by a healthcare provider such as a doctor or nurse.
How to book an appointment?
Booking an appointment is easy. If you are on the go, you can book online through our online booking system, pre-payment is required.
If you would like to discuss anything further or would like to book with our reception team, you can call them on +44 207 353 5678 or email us at info@fleetstreetclinic.com
Related services available at Fleet Street Clinic:
Ovarian cancer is a disease that affects thousands of women worldwide each year and is often referred to as the silent killer due to its silent symptoms, including bloating, abdominal pain, and changes in bowel habits, which are often mistaken for other conditions. Despite advances in treatment, the disease remains a major public health concern due to its high mortality rate. However, new data from a study funded by Cancer Research UK (CRUK) suggests that a seemingly unlikely tool – supermarket loyalty card surveillance – could help spot ovarian cancer early, when it is most treatable.
The study, which was published in JMIR Public Health and Surveillance, analysed data from supermarket loyalty card programs and found that changes in purchasing behaviour could be used to detect early signs of ovarian cancer.
Researchers found that women with ovarian cancer often experience a decline in their appetite and energy levels, which can result in changes in their grocery shopping habits. By monitoring these changes in real-time, it may be possible to detect the disease early and improve the chances of successful treatment.
This is an exciting development in the fight against ovarian cancer, and one that has the potential to revolutionise the way we detect and treat the disease. By leveraging the vast amounts of data generated by supermarket card programs, healthcare providers and public health officials could identify women who may be at risk of ovarian cancer and encourage them to seek early medical attention. This could help to improve the outcomes of treatment and reduce the overall impact of the disease on society.
One of the key benefits of supermarket card surveillance is that it allows for continuous monitoring of women’s purchasing behaviour. This means that healthcare providers can receive real-time alerts when changes occur, allowing them to act quickly and effectively. This level of monitoring is not possible with traditional screening methods, which are typically performed only once or twice per year and may miss early signs of the disease.
Additionally, supermarket card surveillance is a cost-effective way to monitor the population for signs of ovarian cancer. Unlike other screening methods, it does not require specialised equipment or trained personnel, and the cost of monitoring is negligible compared to the cost of treatment. This could make it possible to implement large-scale screening programs, even in resource-limited settings, and reach a greater number of women who may be at risk of ovarian cancer.
Of course, it’s important to keep in mind that supermarket card surveillance is not a substitute for traditional screening methods, such as ultrasound or CA-125 tests, or for regular self-reporting and awareness of symptoms. However, it could be used as an adjunct to these methods, helping to improve the accuracy of screening and reduce the number of missed cases.
Another important consideration is the privacy of women whose purchasing behaviour is being monitored. While supermarket card surveillance has the potential to help detect ovarian cancer early, it is important to ensure that women’s privacy is protected and that the data collected is used only for medical purposes. Healthcare providers and public health officials should work together to ensure that any monitoring programs are transparent, secure, and in compliance with privacy regulations.
In conclusion, the findings of this study are a major step forward in the fight against ovarian cancer. By leveraging supermarket card surveillance, it may be possible to detect the disease early, when it is most treatable, and improve the outcomes of treatment for women around the world. However, it is important to carefully consider the privacy implications of monitoring purchasing behaviour and to ensure that any programs implemented are transparent, secure, and in compliance with privacy regulations. The early detection of ovarian cancer is a critical goal, and we hope that this research will help to pave the way for new and innovative approaches to screening and treatment. Additionally, women should be encouraged to seek medical attention if they notice any changes.
Reference Source: https://publichealth.jmir.org/2023/1/e41762
Related services available at Fleet Street Clinic:
Is there such a thing as testing too early for STIs?
Yes, in fact, if you test too soon after exposure to an STI aka during the “window period”, you may not get an accurate result.
The ‘window period’ is the length of time it can take between catching an infection and when it will show in a test. It’s important to note that if you are tested earlier than the “window period”, some tests may not detect the STI, even though an individual is infected.
The timing of STI testing after potential exposure varies depending on the specific infection. In general, it is best to wait until a sufficient amount of time has passed for the infection to be detectable, but not so long that the infection has already caused damage.
The “window period” for common STIs:
Chlamydia and Gonorrhoea
– These bacterial infections can be detected 2 weeks after exposure. Symptoms can appear before this so those with symptoms shouldn’t delay testing.
HIV
– Antibody tests can be taken 4 weeks after exposure, whilst instant antibody tests are suitable for use 90 days post contact. Early detection RNA tests can be taken from 10 days after potential exposure. Your healthcare provider will be able to advise which test is most suitable for you.
Syphilis
– Antibody tests for syphilis can be detected 12-weeks after a suspected exposure. Symptoms can appear before this so those with symptoms shouldn’t delay testing, as alternative tests can be taken to diagnose.
If you have been exposed to an STI and are concerned about potential infection, it is recommended to have a sexual health consultation at the earliest opportunity. Your healthcare professional will be able to discuss your risk factors, and then advise the appropriate time interval for tests based on the type of test being used. Your healthcare provider can help you determine which test is right for you, and when to get tested. They will discuss this with you during your sexual health consultation.
It is important to note that some STIs, such as herpes and human papillomavirus (HPV), can have no symptoms, so it is possible to have an infection and not know it. Regular STI testing is the only way to diagnose and treat an infection early, which can prevent complications and reduce the risk of transmission to others.
If you have been sexually active and have concerns about potential STI exposure, it is best to consult with a healthcare provider. They can help you determine the best course of action, including when to get tested and which tests to have.
What STIs can we test for?
Fleet St. Clinic offers testing and treatment for several different STIs including:
– HIV
– Gonorrhoea
– Syphilis
– Chlamydia
– Herpes
– HPV – Genital Warts
Additional tests for symptomatic patients include:
– Mycoplasma
– Ureaplasma
– Trichomoniasis
Results
Rapid results are available for most of our STI checks meaning we can provide you with answers on the same day as your tests. Most swabs are analysed within our onsite laboratory so we can provide you with answers as soon as possible.
Remove unnecessary worry by selecting our fastest turnaround times. These vary for each type of STI, so discuss this with your nurse or doctor during your sexual health consultation.
How regularly should I be getting tested?
Getting tested for sexually transmitted infections (STIs) is an important part of maintaining sexual health. There is no one-size-fits-all answer to when to get tested, as the frequency and timing of STI testing depend on several factors, including:
1. Sexual behaviour: Individuals who engage in higher-risk sexual behaviours, such as unprotected sex, multiple sexual partners, or sexual contact with someone who has an STI, should get tested more frequently.
2. Personal health history: Individuals who have a history of STIs or other health conditions that affect sexual health should get tested more frequently.
3. Age: Young people and older adults may be at higher risk for STIs and should consider getting tested more often.
4. Pregnancy: Pregnant women should be tested for STIs during their first prenatal visit, as well as any other time during their pregnancy as recommended by their healthcare provider.
It is also important to note that some STIs can have no symptoms, so it is possible to have an infection and not know it. Regular STI testing is the only way to diagnose and treat an infection early, which can prevent complications and reduce the risk of transmission to others.
Related services available at Fleet Street Clinic: