Month: September 2024
October is Breast Cancer Awareness Month
You may notice an increased amount of pink during this month, especially iconic pink ribbons, and it’s for a good reason: October is Breast Cancer Awareness Month.
This annual campaign aims to increase the awareness of the disease and to raise funds for research into its cause, prevention, diagnosis and treatment. With the hope that in the not too distant future, a cure will be found!
Breast Cancer is the most common cancer in the UK. 1 in 8 women in the UK will be diagnosed at some point in their lives.
In the UK, over 55,000 women each year are diagnosed with Breast Cancer which is the most common cancer. Thanks to research, more people are surviving breast cancer than ever before, yet there are still nearly 1,000 women who’ll die of breast cancer each month. Breast cancer is often thought of as something that only affects women, but men can get it in rare cases. It is important for males (especially those over 75 years with a high BMI) to check breast tissue for abnormalities as well.
We will be sharing important information on symptoms, causes and lifestyle alteration you can make to reduce your risk.
We are urging everyone, especially women, to check their breasts regularly and get checked out by a professional if something seems unusual for you.
REMEMBER: The earlier breast cancer is diagnosed, the easier it is to treat and the better the chance of successful treatment.
BREAST CANCER SYMPTOMS TO LOOK OUT FOR:
- a new lump or thickening in your breast, upper chest area or armpit
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
- Unexplained pain in your breast or armpit that’s there all or almost all the time
How to check your breasts
Checking your breasts yourself means you’ll get to know what is “normal” for you. As a society we are probably not that familiar with how our body currently is and so that makes it difficult to know what subtle changes happen. It’s most likely that unless a dramatic change has occurred a subtle change will go unnoticed.
So, how do you check your breasts?
There is no special technique and you don’t need any training to start checking your breasts. It may feel like you’re unsure what you’re doing but get to know your body and any breast check is better than no breast check.
The easiest and most accurate way is to divide the breasts into four quadrants; the upper outer quadrant, outer lower quadrant, inner lower quadrant and inner upper quadrant. Examine each quadrant with the flat of your hand. It is important to do this regularly so that you are familiar with what each breast feels like normally. That way, should you notice any changes, (hopefully not), you will pick them up straight away and changes won’t go unnoticed. It is important to remember to check your armpits as well. It is surprising how many breast lumps are discovered after an “axillary” or armpit lymph node is found and checked.
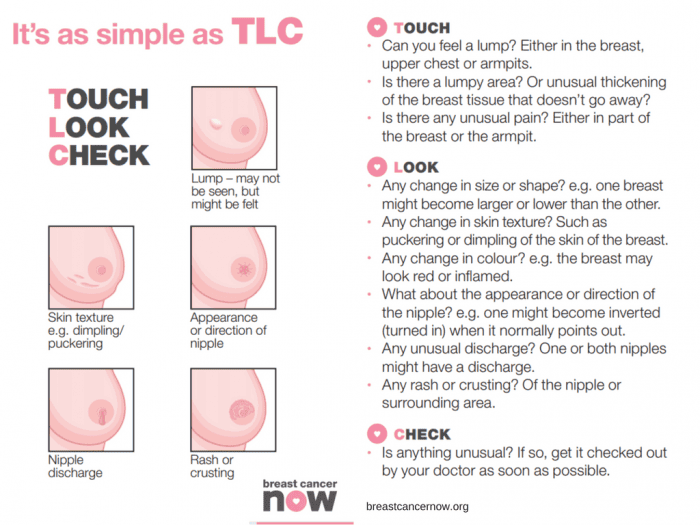
Breast Cancer Now advises the TLC method – “touch, look and check”.
Touch: Can you feel anything new or unusual?
Look: Does anything look different?
Check: Any changes with your GP
You should check your breasts Regularly
Get to know your “normal” by checking your breasts regularly. Get in the habit of checking your breasts at least every month. It can be easier whilst in the bath or shower.
Your breasts can change throughout your life for many reasons – like the menopause, pregnancy and breastfeeding, or puberty. So, if you check them regularly, you’ll be able to spot any new or unusual changes that should be checked out by a GP.
For young and pre-menopausal women it is advised to check mid-cycle (a week after their period finishes) if there are any changes this requires checking with your GP.
As older women are of a higher risk of breast cancer, due to age, it is advised they check even more frequently. Older women should check on a monthly basis without exception. It is advised for men to check also.
Any lump requires attention and checking with your GP immediately.
In addition to regular self-checks, it is important to never miss a mammogram appointment. They may be painful and momentarily uncomfortable, but a mammogram can save your life. If you have a long wait for a mammogram, are unable to access an appointment or just want an additional check, contact the Fleet Street Clinic and we should be pleased to help.
What are the causes of breast cancer?
There are several factors that contribute to increasing your risk of developing breast cancer. There is no single cause, and has to do with our lifestyle, environment and genetics. There are factors which we simply cannot control such as getting older, family history, inherited genes, dense breast tissue, hormones and age at which period started and stopped. However, there are some lifestyle choices that if altered can reduce your risk of breast cancer.
Lifestyle change that will reduce your risk of breast cancer
1. Your weight
Being overweight or obese has a high risk of breast cancer in both men and women (especially after menopause). You can work out your ideal weight using a BMI (Body Mass Index) calculator, this checks your height and weight to see if you are at a healthy weight. For the majority of adults an ideal BMI ranges from 18.5 to 24.9. A BMI between 25 – 30 means overweight. Obesity means a BMI of 30 and above.
2. How much alcohol you drink
Alcohol consumption increases the risk of breast cancer. The risk is greater with each extra unit per day, the latest UK guidelines state no more than 14 units a week.
3. How much exercise you do
Being inactive contributes to a small increased risk of breast cancer, this qualifies as doing less than 150min of moderate activity on a weekly basis. This does not necessarily mean sport and exercise, anything that makes you warmer and out of breath counts.
Throughout October we’ll be highlighting the reasons to support this campaign across our social media platforms. We will be sharing inspirational stories from those who have survived the disease and those who are currently battling. We will also hear from those who have supported a suffering loved one during treatment. Sharing these stories humanises the disease and can provide support/tips for those who may be struggling with a current diagnosis. We will be sharing ways of checking for early warning signs. We’ll also be encouraging all to undertake a Well-Woman or Well-Man health checks. Both of which contain a breast examination.
At Fleet Street Clinic, we specialise in women’s health and have four female GPs on-site to facilitate well-woman health checks. Our Executive Well Woman medical is focused on protecting your well-being and involves a full examination including breast examinations and cervical screen tests. Our comprehensive medical is designed to screen for health problems at the earliest possible stage.
Book Your Well Woman Medical Online. Or if you notice any changes to your breast or have any concerns, you should book a GP appointment as soon as possible.
_______________
To find out more from Breast Cancer Now, visit breastcancernow.org
Here at Fleet Street Clinic, we have had many stool samples come through our laboratory. One recent clinical case using our in-house Full Gastrointestinal PCR Panel, presented unprecedented results.
Patient overview:
- 51-year-old patient
- Travelled to and from Pakistan for a trekking trip
- The patient presented with a history of severe diarrhoea
- Symptoms recorded: erratic bowel movement and weight loss.
Test results:
The PCR result came back quicky as positive for four pathogens:
- Cyclospora cayetanensis,
- Enteroaggregative E. coli (EAEC),
- Enteroinvasive E. coli (EIEC)/Shigella,
- and Enteropathogenic E. coli (EPEC)
This is highly unusual and it is little wonder why our patient was feeling so unwell with severe symptoms.
Our Biomedical Scientist, Jenny Reyes commented; “This is my first time in all of my time as a Biomedical Scientist to encounter such a result with four pathogens presenting all at once.”
Without our GI PCR test, this patient may have undergone many tests to identify the cause and may not have identified that the symptoms were the result of four simultaneous pathogens causing a mixed infection.
The advantage of a panel PCR test is its ability to identify the exact cause, enabling targeted treatment.
In this case, the clinician overseeing this patient’s care was able to tailor treatment to address all four identified pathogens simultaneously with precision.
Without this technology, diagnosing a mixed infection could have taken significantly longer, requiring multiple different tests to pinpoint each cause.
This would have increased the risk that only one pathogen would have been identified, leaving the symptoms caused by the others untreated even after addressing the diagnosed cause.
We encourage all patients with unexplainable gastrointestinal symptoms to consider the GI PCR Panel. It really does offer faster, more targeted care and can identify mixed infection with ease!
More information on our GI Panel:
Our Gastrointestinal Panel Test delivers accurate and reliable results quickly, often within a matter of hours.
It is capable of detecting any of the 23 commonest pathogens that cause diarrhoea – such as E. coli, campylobacter, norovirus salmonella, shigella and giardia, from a single stool sample – all that’s needed is a simple swab.
This supports our rapid diagnostic process, clinical management and educated treatment decisions which improve overall patient outcomes.
Learn more and book today
Dengue has been declared an epidemic in the state of Karnataka in India.
Dengue fever is an unpleasant viral infection spread by the bites from infected Aedes mosquitoes. Unlike the mosquitoes that transmit malaria and are active at dusk, Aedes mosquitoes are most active during daylight hours, making dengue prevention more challenging.
As of this week, Karnataka has reported 25,589 cases and 12 deaths so far, with a staggering 15,000 new cases in the last 45 days alone—the highest in a decade.
Bengaluru, one of the hardest-hit cities, has recorded over 11,500 cases, driven by the rainy season that has created ideal mosquito breeding conditions.
To combat this, the government is enforcing strict measures, including penalties for property owners who allow mosquito breeding. However, personal protection remains critical, especially for those planning to travel to India.
At Fleet Street Clinic, we offer Qdenga®, the newest dengue vaccine. As a live vaccine, it’s not suitable for everyone, so we recommend booking a consultation with one of our specialist travel nurses to determine if it’s right for you.
Safety Tips:
In addition to vaccination, follow these safety tips:
- Cover up, wear long sleeves and trousers when there are mosquitoes around.
- Use mosquito repellent creams, coils, and sprays.
- Use a mosquito net at night
- If you experience symptoms like fever, muscle aches, nausea, or vomiting, seek medical attention.
If you’re planning to travel, ensuring your vaccinations are up-to-date is essential for your safety. To determine if the Qdenga® vaccine is right for you, we recommend booking an online consultation with one of our expert travel nurses.
The Qdenga® vaccine requires two doses, with each dose priced at £148. Our specialists will provide personalised advice and help you navigate your vaccination needs.
Click to book your appointment.
For more information on:
Dengue Epidemic in Karnataka, India
Karnataka declares Dengue an Epidemic
Holidays are a time to relax, unwind and have fun!
However, this excitement can lead to us making decisions we may not usually make when we are at home. If you have unprotected sex whilst abroad whether it is oral, vaginal or anal you are at risk of catching sexually transmitted infections.
You could be at risk of catching these common STIs: HIV, chlamydia, HPV, herpes, syphilis and gonorrhoea.
What can you do to prevent an STI?
Abstaining from sex is the most reliable way to avoid infection. However, if you wish to be sexually active follow some of the tips below:
- Use a condom from start to finish every time during sex including oral, vaginal and anal.
- Get vaccinated to protect against diseases such as Hepatitis B and HPV.
- Do not assume that your partner is STI-free. Talk openly and discuss your sexual health histories.
- Taking drugs and/or alcohol can lead to bad decisions. Be cautious when having sex whilst inebriated as you are more likely to take risks. These include not wearing a condom or having sex with someone you usually would not.
What are the symptoms of an STI?
Symptoms are different depending on the infection. Some diseases also do not cause any symptoms which makes them very hard to spot. If symptoms do occur, they could be some of the following:
- Pain when you urinate or have sex
- Discharge from the vagina, penis, or anus
- Unexplained rash, sore, or ulcer on your skin, genitals, or throat
- Jaundice (yellow colour of the skin and eyes)
What do you do if you think you have an STI?
Having an open and honest conversation, discussing your sexual health with your doctor is a good start to help guide you towards any tests or medication that you may need.
Long-term problems can be prevented by testing for STIs early and also prevent the spreading to other partners.
If you are worried that you may have an STI you should:
- Not have sex with anyone. This will reduce the risk of spreading the disease to anyone else.
- See a doctor or nurse as soon as possible.
- Discuss your sexual history and international travel with the doctor or nurse as some diseases are more common in some countries.
- If you have a positive result notify your recent partners. They may also be infected and unaware.
Fleet Street Clinic offers a discreet and trusted sexual health service including confidential sexual health advice, instant testing, and comprehensive STI screening.
You can book a sexual health appointment online.