Month: March 2022
Chronic kidney disease (CKD) is a long-term condition where the kidneys don’t work as well as they should. In some circumstances, the loss of kidney function can get progressively worse over time but CKD only reaches an advanced stage in a small proportion of people. Although the damage is irreparable, sometimes if changes are made, CKD can be halted with no further damage occurring.
Chronic Kidney disease (CKD) is divided into 5 stages.
Stage 1 is the earliest stage whereby tests have indicated some level of kidney damage. It is important not to ignore a stage 1 diagnosis as this is the time to take action and make lifestyle changes so that the condition does not worsen. With every increase in stage, more kidney damage has been detected up until the last stage, stage 5. Stage 5 means the kidneys have lost almost all their function and it will be time for thinking about dialysis or a transplant.
What to do if your recent blood test shows a reduced kidney function.
Don’t panic, absorb the diagnosis and understand this doesn’t definitively mean your kidneys will stop working altogether. CKD should not be ignored as it can get worse over time but with careful monitoring and management it can be maintained and you can live long fulfilling lives without being unduly affected by the condition.
It is important to review your lifestyle and in particular, your diet. With early stage CKD (stages 1-3) it is paramount to be as healthy as possible and have a healthy balanced diet.
What do I mean by a healthy balanced diet?
This includes:
- Consistently eating freshly cooked food for every meal
- Limiting your intake of processed foods and avoid highly-processed foods
- Reducing your daily salt intake
- Having considered balanced meals – your lunch and dinner meals should contain proteins, carbohydrates and vegetables. Your portion size will depend on your weight and if you have diabetes
- Ensuring you have a minimum of 2-3 portions of fruits and vegetables each and every day
- Increasing your intake of plant based proteins such as beans, lentils, tofu, soya, seitan
- Drinking lots of water to remain well hydrated (ensure your urine runs clear)
- Being as active as physically possible for you
- Avoiding non-steroidal medicines such as ibuprofen, naproxen etc.
What is a renal diet?
You may have heard of the term, renal diet. The term is used quite widely amongst those who have CKD, but personally, I am not a fan of this term. It doesn’t really mean much and can often be misused. People often think it means a diet of low protein, low salt, low potassium and low phosphate – which is pretty hard to do all at once and not always necessary.
People newly diagnosed with CKD in particular often restrict their diet in a panic unnecessarily and in combination with online resources not being clear enough, this can cause a lot of confusion.
My advice would be to seek guidance from someone like myself, a dietician who can look at your lifestyle and individual health and work out a personalised diet plan. This will be much more achievable and as well as not feeling so overwhelming, you’ll only have to limit the foods you absolutely need to.
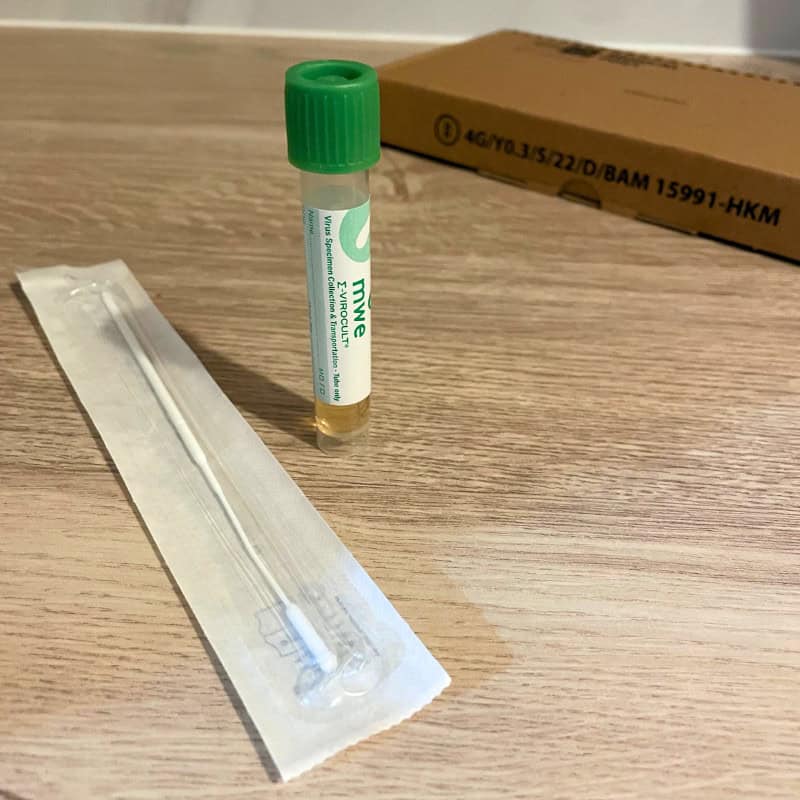
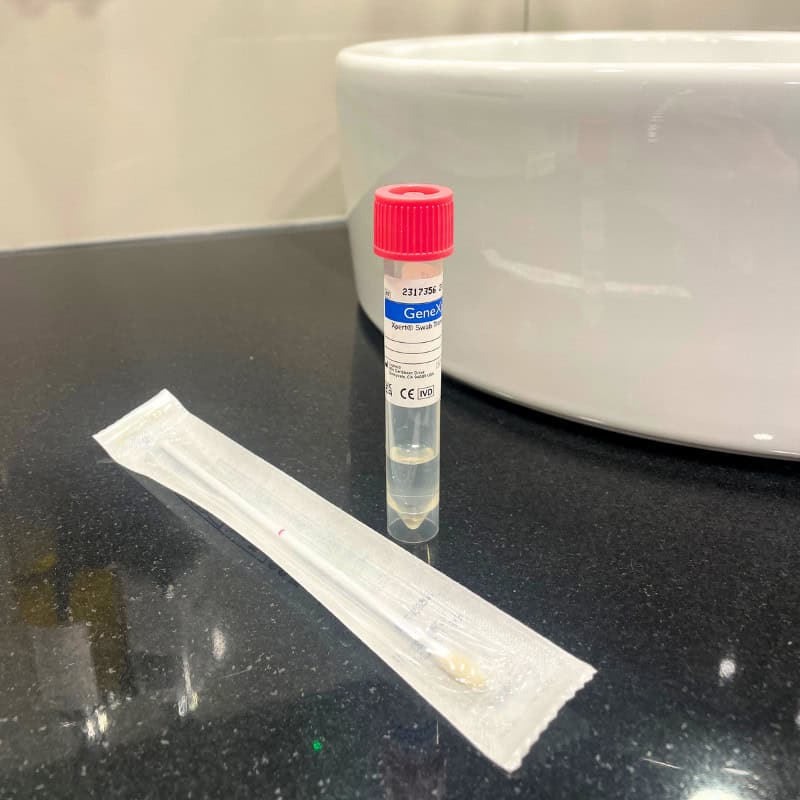
How do you monitor CKD?
The best way to monitor CKD is to have regular tests, either blood or urine. How often you require testing will be dictated by the stage of CKD. Your GP will determine what is best for you and it is best to ask them any medical and testing questions rather than your dietician who will focus solely on your lifestyle and diet.
______________
Ruth Kander is a kidney-specialist dietitian, to book an appointment with her please click here.
Women today lead incredibly busy lives. They run and organise homes and build successful careers, usually all whilst taking on the majority share of caring for their children and often their older relatives. It is therefore not uncommon for women to have little or no time to look after themselves, their health included.
In addition to not making time to prioritise their health, it seems that when women do put their health first and seek medical advice, they are less likely to feel heard and supported in comparison to their male counterparts.
A recent survey by The Department of Health and Social Care found that “more than 4 in 5 (84%) women they surveyed had experienced times when they (or the woman they had in mind) were not listened to by healthcare professionals.”
Based on the data they collected, ‘not being listened to’ appears to be present at all stages of the healthcare pathway. Specifically, many women told them:
- their symptoms were not taken seriously and/or dismissed upon first contact with GPs and other health professionals
- they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years
- if they did secure a diagnosis, there were limited opportunities to discuss or ask questions about treatment options and their preferences were often ignored
Many women recalled their symptoms being dismissed upon first contact with GPs and other professionals; women felt they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years; and post-diagnosis, discussions about treatment options were often limited, and some said their preferences were ignored.
To make matters worse, there is some evidence that due to historical clinical trials being disproportionately male-orientated there is much less research into women-only health concerns and assumptions have been made that similar medical treatments will work for both sexes. The top reasons for the under-representation of women in trials were the belief that hormone fluctuations could influence results and concerns that fertility could be affected. A widely accepted negative repercussion, amongst others, being that women are much more likely to experience adverse side effects of medications because drug dosages have historically been based on clinical trials conducted on men.
A combination of these factors may explain why there is a gender gap in health outcomes, with women experiencing poorer health outcomes in comparison to men. We strongly believe in equality and ensuring health is a top priority for all.
Therefore, here are the top health symptoms women should never ignore:
1) Any change in bowel habit and/ or urination
This includes blood in the stools, unexplained persistent abdominal pain, weight loss, lumps around the anus, lack of appetite, blood in the urine or increased frequency of urination. These are all reasons for seeing your doctor ASAP as these symptoms could be due to bowel, bladder or ovarian cancer. All patients should have an annual faecal occult blood (FOB) test to exclude bowel cancer, which has increased in incidence in the UK for reasons unknown. Or if you are looking for a more in-depth investigation, you should request a colonoscopy which entails looking at the bowel with a colonoscopy. This is the gold standard, but an FOB is the next best thing and far less invasive as a first investigative option. It takes no time at all and is a good preventative check.
2) Any changes to the breast.
Any breast lumps, skin changes, nipple discharge, nipple changes or pain in the breast must be checked ASAP. Breast cancer is the most common type of cancer in the UK and often can present insidiously. Get to know what your breast feels like so that any subtle changes can be detected as early as possible.
3) Skin lesions that do not heal.
Any scab on the skin which does not heal, especially around the eyes, nose, ears and face should be checked. All these areas are the most sun-exposed, and, as such, are more at risk of skin cancer. If these lesions are picked up and treated early, scarring is minimal, but if left, then disfiguring scars and skin grafts may be necessary.
4) Bleeding after the menopause.
If you experience any bleeding after 1-year of your last menstrual period, you must visit your GP for further investigation. Bleeding after the menopause is not common and could be an indicator of cancer of the uterus, or the cervix. They will usually opt for a biopsy of the uterine lining to exclude both – don’t worry, this doesn’t hurt.
5) Always have regular cervical screens.
Most people don’t find cervical screens painful, although they can feel somewhat uncomfortable. If you are concerned about the pain or you have previously found the procedure painful with the NHS, you can opt to book a private appointment. It is important that you don’t miss your appointment.
6) Bleeding between periods.
At any age, you should never ignore bleeding between periods or after intercourse, as this can be a sign of cervical or uterine cancer. Whilst cervical cancer is monitored by regular screening, it is important to still get bleeding between periods checked out following a normal smear result. Cancer of the endometrium is becoming increasingly common in women who have not had children.
7) A persistent cough.
Regardless of gender, you should get a persistent cough checked out by your doctor, especially if you are coughing up discoloured sputum or blood.
8) Any unexplained changes to your body.
Any new indigestion, shortness of breath on exertion, neck or left arm pain requires follow up ASAP. Make sure a GP examines your chest and makes the appropriate investigations.
The same applies to calf pain or any pain in the chest. By taking a full history, examining you and doing quick and easy investigations, worrying conditions can be excluded, such as a pulmonary embolism or a heart attack.
Some recent examples of cases where other healthcare providers have failed our new female patients:
1) We saw a 36 year old who had not had a cervical screening for 5-years because the last one was so painful. The NHS advises a screening every 3-years but we advise yearly screenings to ensure any abnormalities are found as early as possible. 5-years is far too long!
2) We saw a woman who had a suspicious lump at her anal margin, which her usual GP had told her was part of her bladder. She wanted a second opinion because it had grown in size and was now painful. The patient was referred for an urgent assessment to exclude cancer.
3) We saw an 88 year old patient who was disfigured by a large basal cell carcinoma on her forehead, about which she was embarrassed. The patient had been seen by a dermatologist who had frightened her about having the lesion removed by saying she might not survive an anaesthetic. The patient wished that she had taken the risk and asked to be referred back, as the skin lesion was disfiguring and ruining her quality of life.
** The outcomes of these patients are yet unknown, but they are all certainly serious health concerns that should have been properly addressed long before now.
We want to encourage women to take ownership over their health and be assertive when they feel that something has changed from our normal. If they feel like they are not being taken seriously or not being heard, they should seek a second opinion.
If you cannot get an appointment with your usual GP or through the NHS, rather than waiting for weeks and worrying about what it could be, make an appointment with a private GP who can usually see you on the same day!
Put your mind at ease with private healthcare.
Fear of flying, otherwise known as aerophobia, is an excessive worry about air travel. It is one of the most common forms of phobia and according to YouGov, around 24% of Brits have some form of anxiety about getting on a plane.
People suffering from fear of flying experience extremely anxious thoughts which are often so powerful they become physical symptoms. These can include shallow breathing, experiencing chest tightening, sweaty palms, feeling nauseated or lightheaded and sometimes these even develop into a panic attack, meaning many opt to avoid air travel altogether.
For some, it will have been a lifelong problem that has meant never flying at all. For others, who have flown many miles in their lifetime, it is a problem that slowly creeps up on them over time. In both circumstances, the fear can be debilitating and symptoms often trickle into other areas of life.
Like all phobias, there is little logic to support the anxiety that it causes – travel is in fact the safest form of transport and you are much more likely to die from a car accident than in a plane crash. Knowing that fact does little to ease the flying-related anxiety of an aerophobic sufferer.
So, what can be done to overcome our fear of flying?
Understand the reason why you’re a nervous flyer
Fear of flying is usually caused by a combination of factors. Understanding the root cause of your own phobia is perhaps the first step in overcoming it. Is it a fear of heights? Claustrophobia? Was it that film you watched as a child? Or has a particular world event sparked the fear? Many people suddenly developed a fear of flying after 9/11 for example. Figuring this out will then allow you to tackle it in the right way and using the appropriate techniques.
Fight fear with knowledge
Some experts suggest the first strategy for everyone suffering from a fear of flying is learning about the aeroplane and the science behind flight. Our anxiety is fed by ‘what if?’ catastrophic thoughts. Once you become knowledgeable, your ‘what if’ thoughts will be limited by the facts. There are professionally designed courses that will explain aspects like air traffic control, anti-terrorism measures, and what happens during turbulence. Some courses use Virtual Reality (VR) to simulate a flight, explaining everything along the way with the aim of injecting logic into an illogical fear.
Seek medical help for anxiety, fear and panic
From here, a form of therapy may help to identify and break anxiety cycles. There are many different types of therapy and choosing the right one for you will depend on your own needs and goals. Hypnotherapy and cognitive behavioural (CBT) are some of the most commonly used, but there are countless more to choose from. Deciding which is the most appropriate form of therapy can be daunting, so it may be helpful to seek advice from your GP or a travel nurse.
For those who manage to make it onto the plane, there are quite a few, simple personal techniques that can be used to calm your nerves.
Deep breathing techniques
Making a conscious effort to breathe slowly and deeply can interrupt panic. Deep breathing is known to trigger a comfort response and will help prevent hyperventilation.
Distract yourself
Reading a book or listening to a good podcast can refocus your mind and attention.Distracting yourself from the fact that you are flying can be a great way to keep calm if you’re a nervous flyer.. Time tends to pass much more quickly when adequately distracted.
Tell the flight attendants
Alerting the flight attendants of a nervous flyer could also help – with their training and expertise, they are ideally placed to provide reassurance and will regularly check in on you during the flight.
Avoid coffee and wine
Nervous flyers in general should avoid drinking coffee and wine before and whilst flying. Both can leave you more dehydrated than normal. The extra caffeine in coffee can aggravate anxiety issues and the Dutch courage wine offers will pass leaving you more susceptible to jet lag. Stick with water where possible.
Tea really does help
It’s very British to recommend tea to make everything better, but there are many different herbal teas available which can help with relaxation, reducing stress and calming anxiety. Peppermint, camomile, lemon balm and lavender teas are the most commonly used.
We advise nervous flyers and people with aerophobia to seek further information and guidance from their GP who will be able to make a formal diagnosis and treatment options.
For more advice and information you can book a travel consultation appointment.
Ageing is an inevitable part of living. As we age, many physical and psychological changes affect our overall health and these vary from person to person.
The general myth is that as you age, you become more fragile and that this is unavoidable. This is most certainly not the case. There are always things we can do to help keep healthy in our older years and these changes can slow down or even prevent certain health conditions from developing.
The term “fragile” is defined as not “strong or sturdy; delicate and vulnerable” and is most often used to describe older ladies. One particular age-related health issue that supports this description would be osteoporosis.
Osteoporosis is a degenerative disease that weakens and thins the bones which makes them fragile and more likely to break and is becoming increasingly common. It is much more prevalent in women than men due to the menopause directly affecting hormone balances and this directly affects bone density. It is important to prevent osteoporosis as we age as 75% of fractures due to osteoporosis occur in people aged 65 and over.
There are several things you can do to help prevent osteoporosis:
1) Do regular, weight bearing physical activity.
The lack of regular exercise will result in loss of bone and muscle, so adults who are inactive are more likely to have a hip fracture than those who are more active. Adults should aim to do at least two and a half hours of moderate-intensity exercise every week. Weight bearing and resistance training are a particularly great way of improving bone density and helping to prevent osteoporosis.
2) Eat plenty of calcium and Vitamin D containing foods.
Your diet is very important and the nutrients we get from the food we consume will affect how strong our body is. Eat plenty of dairy, seeds, eggs, oily fish, protein, fruit and vegetables. Additionally, try to get at least 15-minutes of sun exposure per day to increase your Vitamin D intake. As we know in the UK, such sun exposure is not always possible during the winter months and, if this is the case, taking a daily Vitamin D supplement is advised.
3) Maintain a healthy weight.
As you get older, you start to lose lean body mass like muscle and bone density and this can start to happen yearly from the age of 30. Being underweight weakens your bones so it is important to keep your weight in a healthy range. A good indication, although not exact, is your BMI. For most adults, a healthy BMI range is between 18.5 and 24.9, so try not to let your BMI fall below 19.
Those who suffer from eating disorders such as anorexia and bulimia are at a higher risk of fragility due to the conditions causing further bone density loss. This can happen to anorexic and bulimic sufferers of all ages.
Older people should aim to consume a varied diet, consisting of enough calories for maintaining a healthy weight.
4) Limit your consumption of alcohol.
We’d recommend that you drink no more than a maximum of 2 units of alcohol per day. Any more than this has been demonstrated to increase the risk of bone fracture. Alcohol abuse has detrimental effects on bone health and increases a person’s risk of developing osteoporosis.
5) Stop smoking and definitely don’t start!
Smoking is a known risk factor for osteoporosis as it increases bone mass loss. In fact, smoking doubles the risk of hip fracture.
Generally, being healthy is the key to avoiding fragility and in particular preventing osteoporosis as we age. Having an annual health medical can highlight any areas of concern. They can monitor the progression of any pre-existing health issues, as well as detect arising conditions in the early stages. You can book your annual medical online
In addition to making healthy lifestyle choices, it is also important to book a doctor’s appointment should you notice any changes to your health. The sooner a health concern is addressed, the easier it is to treat. You can book a GP appointment online.