Tag: Women’s Health
According to Menopause Support, approximately 13 million peri, current and post-menopausal people are living in the UK today.
This makes up a whole third of British women.
Despite making up such a large portion of society, a lot of women find themselves feeling ashamed, shunned or invisible due to their symptoms and the lack of discussion surrounding the subject of menopause.
What is menopause?
Menopause simply means no periods for 12 months and usually begins between the ages of 45-55, but it may start earlier. 80% of women are menopausal by the age of 54 years, so an average woman spends one third of her life being menopausal. In the lead up to menopause, women often experience symptoms of ‘perimenopause’. Changes in the menstrual cycle, hormonal fluctuations and ‘hot flashes’ can all occur as the ovaries begin to stop producing eggs. It is important to note that menopause is a natural transitionary period in life and is not a disease or illness.
What are the symptoms of menopause?
80% of women suffer some symptoms.
Meaning 20% of women have no symptoms at all, and of the 80 % who do suffer some symptoms, only 25% want or need treatment.
Some of the physical symptoms of menopause may include, but are not limited to:
- Night sweats
- Hot flushes
- Dizziness
- Fatigue
- Headaches
- Recurring UTIs
- Stiff joints, aches and pains
- Heavy periods
- Insomnia
- Itchy skin
- Osteoporosis
- Weight gain
Menopause is not only characterised by physical health symptoms, but mental health can also be affected by it too.
Some symptoms might include:
- Anxiety
- Memory loss
- Depression
- Reduced concentration
- Brain fog
How can I manage symptoms for menopause?
A healthy diet and regular exercise, alongside simple lifestyle changes, may improve some symptoms and are important parts of the toolkit in dealing with menopause. Reducing nicotine, alcohol and caffeine intake further assist in reducing symptoms as well.
‘Phytoestrogens’ also help, and these are found in foods like soya protein, beans, yams and nuts. These non-hormonal treatments should always be tried first before hormonal treatments like HRT, which top up hormone levels.
World Menopause Day
World Menopause Day is recognised every year on October 18th to attempt to break the stigma around menopause and highlight the support available to women when they’re experiencing symptoms.
This year’s theme is based on HRT and the various pros and cons.
HRT works by replacing the hormones lost in the menopause process and can relieve symptoms of menopause to a manageable degree. Many women see it as a necessity for managing their menopause symptoms.
However, studies have shown that HRT can slightly increase the risk of breast cancer. This may sound concerning but the risk reduces when using oestrogen only HRT, rather than combined. HRT for managing menopause is an ongoing discussion in the medical field, but a lot of women experiencing menopause find the benefits outweigh the risks, and your GP will be able to advise whether HRT is the right solution for you.
How can Fleet Street Clinic help me?
If you think that you are beginning to experience symptoms of perimenopause or are suffering with your current symptoms, it may be time to book a GP appointment to discuss your menopause and see how we can help you.
Menopause can be a scary transition, but we want to do everything we can to make it as easy as possible for you.
Book a GP appointment today and let us support you.
More information:
October is Breast Cancer Awareness Month
You may notice an increased amount of pink during this month, especially iconic pink ribbons, and it’s for a good reason: October is Breast Cancer Awareness Month.
This annual campaign aims to increase the awareness of the disease and to raise funds for research into its cause, prevention, diagnosis and treatment. With the hope that in the not too distant future, a cure will be found!
Breast Cancer is the most common cancer in the UK. 1 in 8 women in the UK will be diagnosed at some point in their lives.
In the UK, over 55,000 women each year are diagnosed with Breast Cancer which is the most common cancer. Thanks to research, more people are surviving breast cancer than ever before, yet there are still nearly 1,000 women who’ll die of breast cancer each month. Breast cancer is often thought of as something that only affects women, but men can get it in rare cases. It is important for males (especially those over 75 years with a high BMI) to check breast tissue for abnormalities as well.
We will be sharing important information on symptoms, causes and lifestyle alteration you can make to reduce your risk.
We are urging everyone, especially women, to check their breasts regularly and get checked out by a professional if something seems unusual for you.
REMEMBER: The earlier breast cancer is diagnosed, the easier it is to treat and the better the chance of successful treatment.
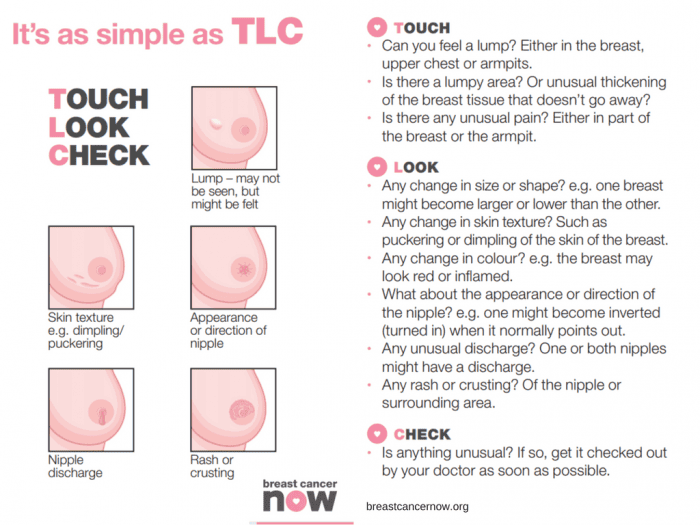
BREAST CANCER SYMPTOMS TO LOOK OUT FOR:
- a new lump or thickening in your breast, upper chest area or armpit
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
- Unexplained pain in your breast or armpit that’s there all or almost all the time
How to check your breasts
Checking your breasts yourself means you’ll get to know what is “normal” for you. As a society we are probably not that familiar with how our body currently is and so that makes it difficult to know what subtle changes happen. It’s most likely that unless a dramatic change has occurred a subtle change will go unnoticed.
So, how do you check your breasts?
There is no special technique and you don’t need any training to start checking your breasts. It may feel like you’re unsure what you’re doing but get to know your body and any breast check is better than no breast check.
The easiest and most accurate way is to divide the breasts into four quadrants; the upper outer quadrant, outer lower quadrant, inner lower quadrant and inner upper quadrant. Examine each quadrant with the flat of your hand. It is important to do this regularly so that you are familiar with what each breast feels like normally. That way, should you notice any changes, (hopefully not), you will pick them up straight away and changes won’t go unnoticed. It is important to remember to check your armpits as well. It is surprising how many breast lumps are discovered after an “axillary” or armpit lymph node is found and checked.
Breast Cancer Now advises the TLC method – “touch, look and check”.
Touch: Can you feel anything new or unusual?
Look: Does anything look different?
Check: Any changes with your GP
You should check your breasts Regularly
Get to know your “normal” by checking your breasts regularly. Get in the habit of checking your breasts at least every month. It can be easier whilst in the bath or shower.
Your breasts can change throughout your life for many reasons – like the menopause, pregnancy and breastfeeding, or puberty. So, if you check them regularly, you’ll be able to spot any new or unusual changes that should be checked out by a GP.
For young and pre-menopausal women it is advised to check mid-cycle (a week after their period finishes) if there are any changes this requires checking with your GP.
As older women are of a higher risk of breast cancer, due to age, it is advised they check even more frequently. Older women should check on a monthly basis without exception. It is advised for men to check also.
Any lump requires attention and checking with your GP immediately.
In addition to regular self-checks, it is important to never miss a mammogram appointment. They may be painful and momentarily uncomfortable, but a mammogram can save your life. If you have a long wait for a mammogram, are unable to access an appointment or just want an additional check, contact the Fleet Street Clinic and we should be pleased to help.
What are the causes of breast cancer?
There are several factors that contribute to increasing your risk of developing breast cancer. There is no single cause, and has to do with our lifestyle, environment and genetics. There are factors which we simply cannot control such as getting older, family history, inherited genes, dense breast tissue, hormones and age at which period started and stopped. However, there are some lifestyle choices that if altered can reduce your risk of breast cancer.
Lifestyle change that will reduce your risk of breast cancer
1. Your weight
Being overweight or obese has a high risk of breast cancer in both men and women (especially after menopause). You can work out your ideal weight using a BMI (Body Mass Index) calculator, this checks your height and weight to see if you are at a healthy weight. For the majority of adults an ideal BMI ranges from 18.5 to 24.9. A BMI between 25 – 30 means overweight. Obesity means a BMI of 30 and above.
2. How much alcohol you drink
Alcohol consumption increases the risk of breast cancer. The risk is greater with each extra unit per day, the latest UK guidelines state no more than 14 units a week.
3. How much exercise you do
Being inactive contributes to a small increased risk of breast cancer, this qualifies as doing less than 150min of moderate activity on a weekly basis. This does not necessarily mean sport and exercise, anything that makes you warmer and out of breath counts.
Throughout October we’ll be highlighting the reasons to support this campaign across our social media platforms. We will be sharing inspirational stories from those who have survived the disease and those who are currently battling. We will also hear from those who have supported a suffering loved one during treatment. Sharing these stories humanises the disease and can provide support/tips for those who may be struggling with a current diagnosis. We will be sharing ways of checking for early warning signs. We’ll also be encouraging all to undertake a Well-Woman or Well-Man health checks. Both of which contain a breast examination.
At Fleet Street Clinic, we specialise in women’s health and have four female GPs on-site to facilitate well-woman health checks. Our Executive Well Woman medical is focused on protecting your well-being and involves a full examination including breast examinations and cervical screen tests. Our comprehensive medical is designed to screen for health problems at the earliest possible stage.
Book Your Well Woman Medical Online. Or if you notice any changes to your breast or have any concerns, you should book a GP appointment as soon as possible.
_______________
To find out more from Breast Cancer Now, visit breastcancernow.org
Women between the ages of 25 and 64 are invited for regular cervical screenings where a healthcare professional looks at the health of the cervix to detect any cell changes or abnormalities. However, in 2022-2023, the number of women who attended their cervical screen fell. Nearly a third of the women invited to do their cervical screen didn’t attend their appointments, this is around 4.6 million women, a deeply concerning number, as over 3000 women are diagnosed with cervical cancer each year and 99.8% of those cases are preventable. Prevention is better than curing, and the earlier you are aware of any cell changes, the easier it is to treat.
Why do some women not attend their cervical screenings?
One of our general practitioners, Dr Belinda Griffiths, has found that in her experience women don’t attend their cervical screenings for a number of reasons including: difficulties with taking time off work for a GP appointment, fear of embarrassment, and fear of the process being uncomfortable or painful.
However, to combat these concerns, the NHS has launched at-home HPV kits. Dr Griffiths explains how they work – “The HPV test is highly sensitive so it separates out those who are HPV-positive and HPV-negative. Those who are HPV-negative will be considered ‘low risk’ for cervical cancer and will be asked to do a future test. Those who are HPV-positive will be deemed ‘high risk’ and be asked to attend for follow-up with a clinician whereby they will conduct a cervical screening to check the health of their cervix and investigate if any abnormal cells are present.”
These new tests are the same process as at-home STI tests whereby a simple swab collects the sample from the vagina. Having the option of this sort of test at home removes the fear some women may have surrounding the slightly more intrusive cervical screen.
What is HPV?
HPV (human papillomavirus) is a common virus passed on via skin-to-skin contact, usually through genital contact. There are many types of HPV, most of which are harmless, don’t usually cause any symptoms and the infection will go away on its own. However, others are deemed ‘high risk’ as they can persist and cause cell changes which can lead to cancer. It is thought that these ‘high risk’ HPV strains are responsible for around 80% of cervical cancer cases, making the detection of HPV all the more important.
How can you prevent HPV?
You can be protected from certain HPV strains through vaccination. There are two HPV vaccines currently available in the UK: Gardasil which protects against 4 strains of HPV used in the NHS and the vaccine used here at the Fleet Street Clinic, Gardasil-9, which protects against 9 of the high-risk HPV strains.
When can you be vaccinated against HPV?
The NHS now routinely offers the Gardasil vaccine to girls and boys around age 12/13, before the age people generally become sexually active. However, the vaccination programme only came into full force in 2019, meaning many people are currently unvaccinated. It should be pointed out that adults can get vaccinated at any age and even if you have already been exposed to HPV, the vaccine can still offer protection against other strains to which you have not yet been exposed.
It is a particularly good idea for people to get vaccinated before they attend university or before they go travelling on a ‘gap year’, as these are typically times where young people are more sexually active and therefore more likely to be exposed to HPV.
It is important to note that getting the HPV vaccination most certainly doesn’t mean missing or not participating in HPV tests or cervical screenings. A combination of these preventative measures gives you the highest possible chance of preventing cervical cancer.
Book your Cervical Screen or HPV vaccine online today.
Ovarian cancer is a disease that affects thousands of women worldwide each year and is often referred to as the silent killer due to its silent symptoms, including bloating, abdominal pain, and changes in bowel habits, which are often mistaken for other conditions. Despite advances in treatment, the disease remains a major public health concern due to its high mortality rate. However, new data from a study funded by Cancer Research UK (CRUK) suggests that a seemingly unlikely tool – supermarket loyalty card surveillance – could help spot ovarian cancer early, when it is most treatable.
The study, which was published in JMIR Public Health and Surveillance, analysed data from supermarket loyalty card programs and found that changes in purchasing behaviour could be used to detect early signs of ovarian cancer.
Researchers found that women with ovarian cancer often experience a decline in their appetite and energy levels, which can result in changes in their grocery shopping habits. By monitoring these changes in real-time, it may be possible to detect the disease early and improve the chances of successful treatment.
This is an exciting development in the fight against ovarian cancer, and one that has the potential to revolutionise the way we detect and treat the disease. By leveraging the vast amounts of data generated by supermarket card programs, healthcare providers and public health officials could identify women who may be at risk of ovarian cancer and encourage them to seek early medical attention. This could help to improve the outcomes of treatment and reduce the overall impact of the disease on society.
One of the key benefits of supermarket card surveillance is that it allows for continuous monitoring of women’s purchasing behaviour. This means that healthcare providers can receive real-time alerts when changes occur, allowing them to act quickly and effectively. This level of monitoring is not possible with traditional screening methods, which are typically performed only once or twice per year and may miss early signs of the disease.
Additionally, supermarket card surveillance is a cost-effective way to monitor the population for signs of ovarian cancer. Unlike other screening methods, it does not require specialised equipment or trained personnel, and the cost of monitoring is negligible compared to the cost of treatment. This could make it possible to implement large-scale screening programs, even in resource-limited settings, and reach a greater number of women who may be at risk of ovarian cancer.
Of course, it’s important to keep in mind that supermarket card surveillance is not a substitute for traditional screening methods, such as ultrasound or CA-125 tests, or for regular self-reporting and awareness of symptoms. However, it could be used as an adjunct to these methods, helping to improve the accuracy of screening and reduce the number of missed cases.
Another important consideration is the privacy of women whose purchasing behaviour is being monitored. While supermarket card surveillance has the potential to help detect ovarian cancer early, it is important to ensure that women’s privacy is protected and that the data collected is used only for medical purposes. Healthcare providers and public health officials should work together to ensure that any monitoring programs are transparent, secure, and in compliance with privacy regulations.
In conclusion, the findings of this study are a major step forward in the fight against ovarian cancer. By leveraging supermarket card surveillance, it may be possible to detect the disease early, when it is most treatable, and improve the outcomes of treatment for women around the world. However, it is important to carefully consider the privacy implications of monitoring purchasing behaviour and to ensure that any programs implemented are transparent, secure, and in compliance with privacy regulations. The early detection of ovarian cancer is a critical goal, and we hope that this research will help to pave the way for new and innovative approaches to screening and treatment. Additionally, women should be encouraged to seek medical attention if they notice any changes.
Reference Source: https://publichealth.jmir.org/2023/1/e41762
Related services available at Fleet Street Clinic:
Women today lead incredibly busy lives. They run and organise homes and build successful careers, usually all whilst taking on the majority share of caring for their children and often their older relatives. It is therefore not uncommon for women to have little or no time to look after themselves, their health included.
In addition to not making time to prioritise their health, it seems that when women do put their health first and seek medical advice, they are less likely to feel heard and supported in comparison to their male counterparts.
A recent survey by The Department of Health and Social Care found that “more than 4 in 5 (84%) women they surveyed had experienced times when they (or the woman they had in mind) were not listened to by healthcare professionals.”
Based on the data they collected, ‘not being listened to’ appears to be present at all stages of the healthcare pathway. Specifically, many women told them:
- their symptoms were not taken seriously and/or dismissed upon first contact with GPs and other health professionals
- they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years
- if they did secure a diagnosis, there were limited opportunities to discuss or ask questions about treatment options and their preferences were often ignored
Many women recalled their symptoms being dismissed upon first contact with GPs and other professionals; women felt they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years; and post-diagnosis, discussions about treatment options were often limited, and some said their preferences were ignored.
To make matters worse, there is some evidence that due to historical clinical trials being disproportionately male-orientated there is much less research into women-only health concerns and assumptions have been made that similar medical treatments will work for both sexes. The top reasons for the under-representation of women in trials were the belief that hormone fluctuations could influence results and concerns that fertility could be affected. A widely accepted negative repercussion, amongst others, being that women are much more likely to experience adverse side effects of medications because drug dosages have historically been based on clinical trials conducted on men.
A combination of these factors may explain why there is a gender gap in health outcomes, with women experiencing poorer health outcomes in comparison to men. We strongly believe in equality and ensuring health is a top priority for all.
Therefore, here are the top health symptoms women should never ignore:
1) Any change in bowel habit and/ or urination
This includes blood in the stools, unexplained persistent abdominal pain, weight loss, lumps around the anus, lack of appetite, blood in the urine or increased frequency of urination. These are all reasons for seeing your doctor ASAP as these symptoms could be due to bowel, bladder or ovarian cancer. All patients should have an annual faecal occult blood (FOB) test to exclude bowel cancer, which has increased in incidence in the UK for reasons unknown. Or if you are looking for a more in-depth investigation, you should request a colonoscopy which entails looking at the bowel with a colonoscopy. This is the gold standard, but an FOB is the next best thing and far less invasive as a first investigative option. It takes no time at all and is a good preventative check.
2) Any changes to the breast.
Any breast lumps, skin changes, nipple discharge, nipple changes or pain in the breast must be checked ASAP. Breast cancer is the most common type of cancer in the UK and often can present insidiously. Get to know what your breast feels like so that any subtle changes can be detected as early as possible.
3) Skin lesions that do not heal.
Any scab on the skin which does not heal, especially around the eyes, nose, ears and face should be checked. All these areas are the most sun-exposed, and, as such, are more at risk of skin cancer. If these lesions are picked up and treated early, scarring is minimal, but if left, then disfiguring scars and skin grafts may be necessary.
4) Bleeding after the menopause.
If you experience any bleeding after 1-year of your last menstrual period, you must visit your GP for further investigation. Bleeding after the menopause is not common and could be an indicator of cancer of the uterus, or the cervix. They will usually opt for a biopsy of the uterine lining to exclude both – don’t worry, this doesn’t hurt.
5) Always have regular cervical screens.
Most people don’t find cervical screens painful, although they can feel somewhat uncomfortable. If you are concerned about the pain or you have previously found the procedure painful with the NHS, you can opt to book a private appointment. It is important that you don’t miss your appointment.
6) Bleeding between periods.
At any age, you should never ignore bleeding between periods or after intercourse, as this can be a sign of cervical or uterine cancer. Whilst cervical cancer is monitored by regular screening, it is important to still get bleeding between periods checked out following a normal smear result. Cancer of the endometrium is becoming increasingly common in women who have not had children.
7) A persistent cough.
Regardless of gender, you should get a persistent cough checked out by your doctor, especially if you are coughing up discoloured sputum or blood.
8) Any unexplained changes to your body.
Any new indigestion, shortness of breath on exertion, neck or left arm pain requires follow up ASAP. Make sure a GP examines your chest and makes the appropriate investigations.
The same applies to calf pain or any pain in the chest. By taking a full history, examining you and doing quick and easy investigations, worrying conditions can be excluded, such as a pulmonary embolism or a heart attack.
Some recent examples of cases where other healthcare providers have failed our new female patients:
1) We saw a 36 year old who had not had a cervical screening for 5-years because the last one was so painful. The NHS advises a screening every 3-years but we advise yearly screenings to ensure any abnormalities are found as early as possible. 5-years is far too long!
2) We saw a woman who had a suspicious lump at her anal margin, which her usual GP had told her was part of her bladder. She wanted a second opinion because it had grown in size and was now painful. The patient was referred for an urgent assessment to exclude cancer.
3) We saw an 88 year old patient who was disfigured by a large basal cell carcinoma on her forehead, about which she was embarrassed. The patient had been seen by a dermatologist who had frightened her about having the lesion removed by saying she might not survive an anaesthetic. The patient wished that she had taken the risk and asked to be referred back, as the skin lesion was disfiguring and ruining her quality of life.
** The outcomes of these patients are yet unknown, but they are all certainly serious health concerns that should have been properly addressed long before now.
We want to encourage women to take ownership over their health and be assertive when they feel that something has changed from our normal. If they feel like they are not being taken seriously or not being heard, they should seek a second opinion.
If you cannot get an appointment with your usual GP or through the NHS, rather than waiting for weeks and worrying about what it could be, make an appointment with a private GP who can usually see you on the same day!
Put your mind at ease with private healthcare.
MARCH IS OVARIAN CANCER AWARENESS MONTH
A vital month raising awareness of ovarian cancer to improve early diagnosis to save lives.
More women died from ovarian cancer in the UK (4,227) than from all other gynaecological cancers combined in 2016, according to Cancer Research UK. However, worryingly one in five women in the UK (22%) mistakenly believe that a smear test (cervical screening) can detect ovarian cancer, according to research Target Ovarian Cancer carried out with YouGov.
We are committed to raising awareness of the disease.
Speak to one of our female GP’s about any concerns you may have about your gynaecological history and your families medical history. During your consultation, we will also conduct a breast check and pelvic examination.
“In the UK a woman dies every two hours from ovarian cancer, but the earlier the diagnosis the better the chances are”
Professor Hani Gabra – Director of Ovarian Cancer Action Research Centre
What is ovarian cancer?
Ovarian cancer is when abnormal cells in the ovary begin to grow and divide in an uncontrolled way and eventually form a growth (tumour). Every year 7,300 women in the UK are diagnosed with ovarian cancer.
Who can get ovarian cancer?
The risk of developing ovarian cancer increases as you get older. The most common type of ovarian cancer is epithelial ovarian cancer, this usually occurs in women older than 50 years old. We don’t know exactly what causes epithelial ovarian cancer. But some factors may increase or reduce the risk.
Factors that increase the risk include:
- getting older
- inherited faulty genes
- having breast cancer before
Factors that may reduce the risk include:
- taking the contraceptive pill
- having children
- breastfeeding
Ovarian Cancer is notoriously difficult to spot.
With non-specific symptoms in the early stages. It is hoped that this new method of early diagnosis could help save lives.
How to recognise the symptoms of Ovarian Cancer:
Early Ovarian Cancer symptoms can be similar to those of other conditions, these some to watch out for:
- Persistent bloating – not bloating that comes and goes
- Pain in the lower stomach and pelvis
- Difficulty Eating and feeling full quickly
- Back pain
- Fatigue
- Change in bowel habits
What should you do if you’re worried?
It is important to contact your GP as soon as possible if you spot any symptoms that are abnormal for you.
We understand talking about your concerns and having an examination can be quite worrying and for some, embarrassing, therefore, to make you as comfortable as possible, all our well woman services are booked with a female GP.
There is an Ovarian Cancer Blood Test – CA 125 available
Levels of protein CA125 in the blood are recognised as a marker for ovarian cancer. This simple and effective blood test will detect early stages of ovarian cancer. You can either have this as a stand-alone blood test or add it on to your medical for an additional cost. Please inquire for prices..
Links:
Target Ovarian Cancer
Cancer Research UK
For more information about Fleet Street Clinic’s Women’s Health Services.
You can also book a GP appointment online.