Tag: Health Advice
Oropouche Virus Disease: A growing concern in Central and South America.
As of mid-2024, Central and South America are experiencing a significant outbreak of Oropouche virus disease, impacting countries such as Brazil, Bolivia, Colombia, Peru, and Cuba.
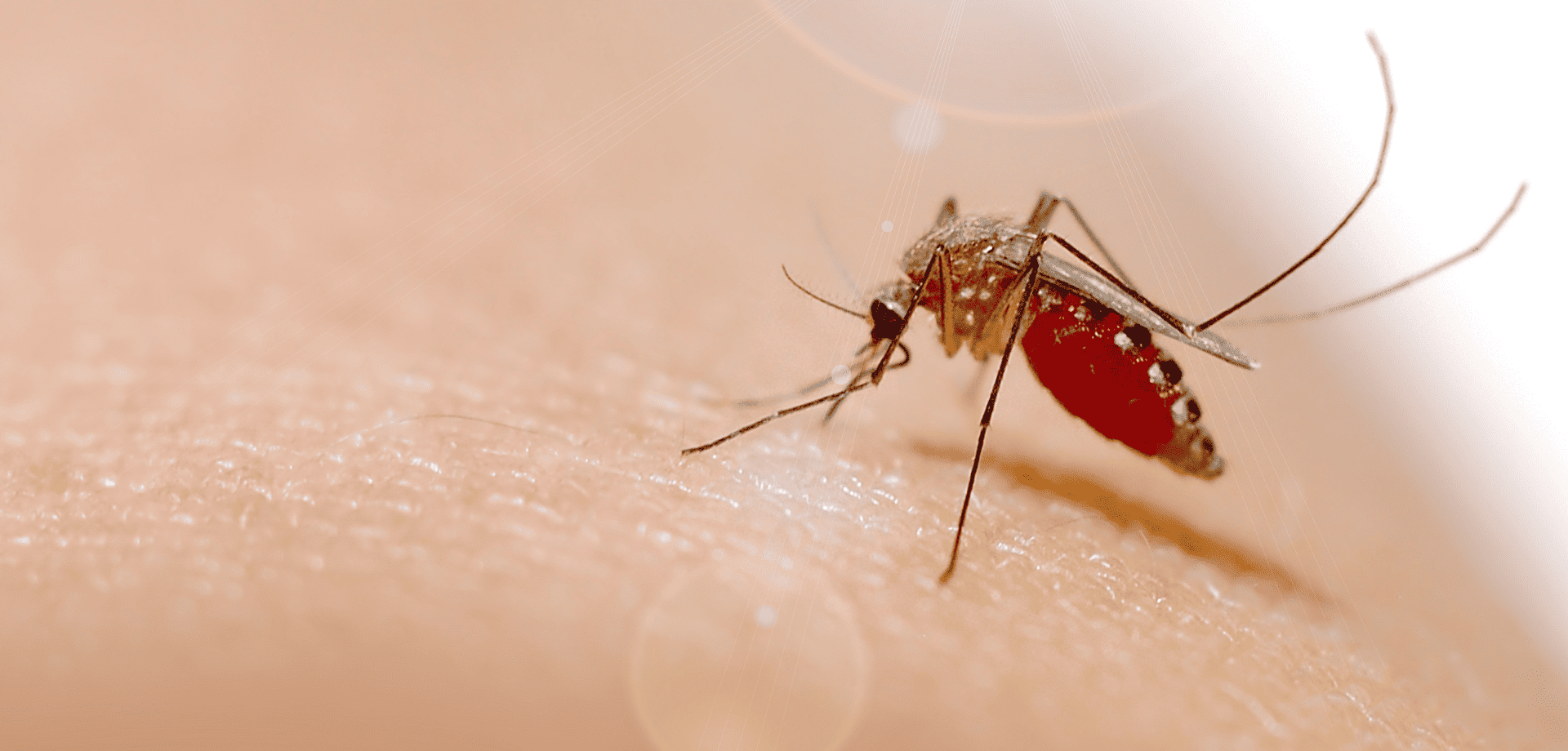
The Oropouche virus is primarily transmitted through the bites of infected midges (Culicoides paraensis) and mosquitoes. The virus is mainly spread in tropical and subtropical regions where these vectors are prevalent.
Symptoms of Oropouche virus disease include:
- sudden-onset fever,
- severe headaches,
- muscle and joint pain,
- rash,
- eye pain,
- nausea,
- and dizziness.
While most cases are mild and self-limiting, lasting 3 to 7 days, some individuals may experience more severe symptoms like meningitis and encephalitis.
There is no specific antiviral treatment or vaccine for the disease, so care focuses on symptom relief, such as rest, hydration, and pain management.
How to protect yourself from Oropouche virus
Preventing Oropouche virus disease involves reducing exposure to vector bites. Unlike mosquitoes, the main vector (midges) lacks a proboscis, and so is unable to bite through clothing.
Covering up, and wearing long-sleeved clothing, is therefore a keyway of preventing infective bites.
Other key measures include using plenty of insect repellent, impregnating clothing with Permethrin insecticide, using bed nets, and staying indoors during peak biting times.
Eliminating standing water where vectors breed is an important public health measure.
Prevention is key!
With no vaccine available, prevention remains the best defence against Oropouche virus disease.
Personal protective measures against insect bites also help protect against dengue, yellow fever, Zika, chikungunya, malaria, and a wide range of other tropical insect-borne infections, and should be followed carefully by travellers to tropical countries.
Cases found in Europe
Spain, Italy and Germany reported infections in numerous patients who had recently travelled to Cuba and Brazil.
The European Centre for Disease Prevention and Control (ECDC) warned of a moderate threat to travellers visiting Brazil, Bolivia, Colombia, Peru and Cuba, where Oropouche virus (Orov) is currently spreading.
If you’ve recently travelled to a known outbreak area and are experiencing any of the symptoms mentioned above, it is important to mention this to your doctor. This will help them rule out an Oropouche virus infection.
Worried about your upcoming travel plans?
Schedule a travel consultation with one of our specialist travel nurses.
They will guide you through potential health risks and recommend the necessary preventive measures and vaccinations to ensure your safety while travelling.
For more information on:
In the months since its release in the UK, we have seen a huge demand for the new Dengue vaccine, Qdenga.
For those with experience of the disease, the news of its licensing has been much anticipated and we are proud to be one of the first clinics in the UK to offer the vaccine.
What is Dengue Fever?
Dengue is a viral infection that is spread through the bite of an infected aedes mosquito, a species easily recognisable by its striped legs. It occurs in over 120 countries worldwide, mainly in the tropics and sub-tropics, and is the second most common cause of fever in the returning traveller.
The most seriously impacted regions are the Americas, South-East Asia, and Western Pacific, with Asia accounting for around 70% of the world’s disease burden.
It is also spreading to new areas, including Europe, where outbreaks have been increasing in recent years. Read more about this in our recent blog, Dengue Fever in Europe: Temperature Risk.
Since it is transmitted from person to person, via the mosquito vector, it is of particular concern in populated, urban areas.
What are the symptoms of Dengue Fever?
Whilst most cases are asymptomatic, some will develop a severe flu like illness that can require hospitalisation. In rare cases, this will be life threatening.
Common symptoms include;
a high fever,
severe headache,
pain behind the eyes,
muscle ache,
joint pains,
nausea,
vomiting and rash.
There are four serotypes of Dengue virus; for those infected by one type, a subsequent infection is more likely to be life threatening. The severe type of Dengue usually starts a few days after the initial symptoms began. After feeling a bit better, symptoms suddenly return and can include severe abdominal pain, persistent vomiting and bleeding.
Approximately 1 in 20 patients with Dengue will progress into the severe form of the disease.
Dengue Fever Vaccination
Historically, the only protection we could provide was advice surrounding mosquito bite avoidance. With the arrival of Qdenga, we now have the option of a vaccination which provides safe and effective protection.
Studies have shown Qdenga to offer 80% protection from the first dose, with long term immunity achieved after the second.
Who should get vaccinated?
Qdenga can be safely given to those who have previously had the disease, and it is especially important for this group. We would also encourage frequent or long stay travellers to consider the vaccine. The vaccine is licensed for the prevention of Dengue in individuals from 4 years of age and requires two doses, to be given three months apart.
It is a live vaccine, so it’s not suitable for everyone. To discuss your suitability with one of our specialist travel nurses, please book a travel consultation online, or call our reception team on +44 20 7353 5678.
We can usually accommodate same day bookings and suitable vaccinations can be given within the same appointment.
Related services available at Fleet Street Clinic
Travellers’ Diarrhoea Online Consultation
For further reading
If you have a heart condition you have a greater risk of becoming more seriously ill from flu (seasonal influenza) than the general population. In addition, having the flu can exacerbate pre-existing conditions like diabetes or asthma.
According to the NHS, “every year over 11,000 people in England die from complications caused by the flu virus. Many of these deaths could have been prevented by having the flu vaccination.”
Preventing the flu in the first place is the best option.
The best protection is to have a Flu Vaccine each winter.
What is the flu?
Many people think having influenza, also known as the flu, is like having a bad cold, but in reality flu is a nasty respiratory virus that can make you very unwell. Influenza causes inflammation in the body and can be very serious – sometimes leading to hospitalisation or even death.
There is evidence that heart attacks happen more often during or immediately after an acute inflammatory illness, such as flu.
A flu jab is the best protection against flu.
In general, the flu causes stress and inflammation on the body, increasing blood pressure, heart rate and heart function. This is not good for someone with heart or circulatory problems.
Flu vaccination is strongly recommended for anyone who has ever had a heart attack, stroke or has underlying heart disease. A previous diagnosis of heart or circulatory diseases is considered a high risk factor for complications or even another heart attack, for anyone who becomes ill with flu.
Does flu affect heart medication?
If you take warfarin, flu symptoms can affect your blood clotting rate (INR). You should speak to your doctor if this happens so they can monitor your situation closely. It does also mean if you do become unwell, it may take you longer to recover than the average person.
In addition, some over-the-counter flu medicines can’t be used when taking medicines for heart conditions, so contact your doctor before taking things like painkillers and cough medicines. It is better to check before beginning any new medications.
When is the best time to get the flu jab?
Flu vaccinations become available from mid to late September, and through the season until February. It’s best to get your flu vaccine in September or October. The peak time for catching flu runs from Christmas to Easter. The aim is to be vaccinated before flu transmission starts, and to allow at least a couple of weeks post-vaccination, for maximum immunity to develop. The sooner you have the vaccination, the sooner you will be protected.
You can book your flu jab online.
We have a range of flu vaccinations available, including the premium recombinant vaccine, cell-based vaccine, FluAd (for those aged 65 year and older), kids nasal spray and the standard flu jab.
It is important to have a flu jab every year because the flu virus can change. There are many strains of flu already and some are more dominant than others. Each year strains are analysed to determine which strains are likely to be the prevalent strains circulating that year. They can vary year to year so relying on a past vaccination for protection is risky. The previous year’s vaccine may not offer you the right protection against the strains in circulation this year.
In addition, immunity to flu decreases over time. Exposure to the flu virus strengthens the immune response and offers natural protection. With less flu circulating over the past few years due to covid restriction measures, natural immunity in the general population will have decreased.
A flu vaccine will boost immunity.
With most workers now returned to the office and social distancing restrictions long gone, there is a greater chance of the flu spreading and more people falling ill this winter. With both illnesses circulating around it is highly recommended to reduce the risk by getting the flu jab.
Protect yourself against the flu.
You can find more information on the types of flu vaccines available.
For more information on the premium recombinant flu jab.
_____________
Wanting to book a Workplace Flu Vaccination Programme?
Flujabs.org is part of Fleet Street Clinic and has been providing workplace flu vaccinations to UK businesses for many years.
Fill out the online form and one of our flu coordinators will get back to you with current availability and costs.
As a travel nurse based in London, I was concerned to hear the recent warning from health officials about the spread of tick-borne encephalitis (TBE) virus in several parts of the country. The UK Health Security Agency (UKHSA) has confirmed three cases of TBE virus in patients in Yorkshire, Norfolk, and on the border of Hampshire and Dorset. Further tests on ticks across the country have found that the disease, which was commonly found in parts of Europe and Asia until now, is now present in the UK. The experts have warned that it is unlikely that TBE virus will disappear, so it’s essential to establish a surveillance program.
Public health officials say the risk is low, but it’s essential for walkers to take precautions and seek medical help if they fall ill after being bitten, especially if by a tick.
As a clinic that specialises in travel, we are used to urging everyone to take precautions to protect themselves from tick bites anyway, but this news reinforces the importance of doing this at home as well as when travelling abroad. It is essential to cover your ankles and legs, apply insect repellent, and check clothes and your body for ticks, particularly when visiting areas with long grass such as woods, moorlands, and parks.
In most cases the TBE virus typically causes mild flu-like symptoms, but it can also lead to severe infection in the central nervous system resulting in meningitis or encephalitis a high fever with headache, neck stiffness, confusion, or reduced consciousness, and long-term impairment.
As a travel nurse, I think it is really important to educate people about the symptoms of TBE to encourage them to seek medical help immediately if they experience any of these symptoms, but also to emphasise the fact that infections are preventable.
Ticks are becoming more common in parts of the UK, mainly due to increasing deer numbers. They live in undergrowth and latch on to humans when they walk through long grass. It is thought infected ticks may have arrived in the UK via migrating birds. Scientists had suspected the virus had arrived in the UK in 2019, following a couple of cases, but complexities involved in testing meant these could not be confirmed.
It’s crucial to emphasise the significance of vaccination for individuals who are considered of a higher risk. You are much more likely to catch TBE if you work outdoors or if you enjoy outdoor activities such as camping, hiking, dog-walking, countryside rambling and even jogging. Children playing outside may be especially vulnerable.
Vaccines can provide protection, and as there is currently no known cure for tick-borne encephalitis virus, those individuals who would be considered at higher risk are advised to be vaccinated as a precaution.
It’s worth noting that a vaccine is used routinely in areas of high incidence in Europe, and its advisable to consider vaccination for individuals with outdoor occupations in regions where the virus is prevalent.
For the general public the risk of contracting TBE is relatively low. Therefore, it’s essential to educate people about TBE and encourage them to take precautions to protect themselves from tick bites, particularly when travelling to areas where the virus is found.
Related services available at Fleet Street Clinic
Tick Borne Encephalitis Vaccination
For further reading, more news coverage can be found here:
Gov.uk – Tick Borne Encephalitis detection in England
The Times – Tick-borne encephalitis warning to walkers
The Telegraph – First cases of rare tick disease found in England
Cholesterol is a type of fat that is found in the blood and plays an important role in our bodies. However, high levels of cholesterol can lead to serious health issues, such as heart disease, stroke, and other cardiovascular problems. Unfortunately, cholesterol is often referred to as a “silent killer” as there are usually no symptoms and the first indication that something is wrong may be a heart attack. That’s why it’s important to have your cholesterol levels checked regularly.
Instant cholesterol testing only requires a short nurse appointment that provides you with both the test and the results during the same appointment. This type of testing makes it easy and convenient for people to understand their cholesterol levels and take steps to keep them under control.
Statistics from the National Institute for Health and Care Excellence (NICE) show that cardiovascular disease (CVD) is the leading cause of death in the United Kingdom, accounting for around 26% of all deaths. The most common type of CVD is coronary heart disease, which is caused by a build-up of fatty deposits in the arteries leading to the heart. High cholesterol levels can contribute to the formation of these fatty deposits.
By knowing your cholesterol numbers through instant testing, you can understand your risk of developing CVD and take the necessary steps to keep your levels under control. NICE recommends that all adults in the UK should have their cholesterol levels checked at least once every five years, or more frequently if they are at increased risk of CVD. Those at increased risk include people with a family history of CVD, smokers, people with high blood pressure, and people with diabetes.
To keep your cholesterol levels under control, it is important to make changes to your diet. This includes eating more fruits, vegetables, whole grains, and lean proteins, and reducing your intake of saturated and trans fats. You should also aim to maintain a healthy weight and be physically active for at least 30 minutes a day.
If lifestyle changes are not enough, medication may be required. The most common type of cholesterol-lowering medication is statins, which work by reducing the production of cholesterol in the liver. Statins are widely used in the UK and are safe and effective.
The National Institute for Health and Care Excellence (NICE) has recently released updated guidelines on the use of statins, which now recommend that they can be considered for people at a lower risk threshold.
Further reading on “NICE recommends wider use of statins for prevention of cardiovascular disease (CVD)”.
In conclusion, instant cholesterol testing provides an easy and convenient way to understand your cholesterol levels and take steps to keep them under control. Regular testing is important for everyone in the UK, especially those who are at increased risk of CVD. By knowing your numbers, making changes to your diet, maintaining a healthy weight, and being physically active, you can help keep your cholesterol levels in the healthy range and reduce your risk of developing serious health problems.
Related services available at Fleet Street Clinic:
Instant Cholesterol Testing with a nurse
Blood Tests at Fleet St. Clinic
Well Person Medical
GP Services
With (hopefully!) sunnier and longer days upon us, summer is a great time of year to get your running shoes on. As a keen runner myself, I understand the appeal; it’s pure, it’s meditative, and it gets your blood pumping like little else.
Unfortunately, for all its positives, running can be problematic for the body and it tends to bring out minor issues and turn them into major ones. These often include achilles tendonitis, shin splints, plantar fasciitis, ITB syndrome, stress fractures, hip and lower back issues, and more knee problems than I have time to list.
Many of the problems from running come from two areas. Firstly, heel strike which is where the heel hits the ground repeatedly and sends a shock through the whole skeleton which causes issues from the heel itself all the way up to the lower back. Secondly, gait – which is the way a person walks; the whole lower limb (especially the knee) is quite finely tuned to work in certain ways, and anything that affects that can begin to cause problems. A dropped arch, tight muscle, old injury, slight one-sidedness etc can bring these issues on.
What can be done to prevent these issues?
Like always, the number one rule is to get any symptoms you are experiencing looked at as soon as possible. Early diagnosis, advice and treatment is vital.
One thing that can really help heel strike and gait is by getting the right trainers. Here’s a few things to consider:
- Don’t confuse fashion and effectiveness. Good running trainers generally don’t look cool! Some of the bigger brands will advertise to you that they are great for sports but do your research. I would usually recommend Asics or Brooks.
- Replace your shoes regularly. The soles of most trainers are good for about 200-250 miles maximum. So, if you’re running 20 miles per week, you’ll probably need to replace them after 4-6 months.
The shoe may still look okay after that but there is an increased risk of injury. It is, therefore, important to ensure that you are replacing your trainers as regularly as required. - You don’t need to buy the most recent model. Many of the best running trainers are on their 20th/30th or so iteration. When a new model is released the price of the last couple of iterations will drop quite significantly, and will still be an excellent option.
- Good arch support. Trainers largely work on preventing pronation etc. by the way they flex. Many have little if any arch support, even with good ones you may need an additional orthotic insole made for your specific needs. This may also mean you need half a size bigger.
- Speak to the experts. A running machine in a shoe shop is useful, but remember the shop assistant has probably only had a brief introduction in what to look for, and no idea of your other contributing factors. Speak to a specialist – an osteopath, podiatrist, or physio.
_____________
OSTEOPATH AT FLEET STREET CLINIC
Andrew Doody is an osteopath at Fleet Street Clinic and is fully registered with the General Osteopathic Council (GOSC).
Book an appointment with him if you have any musculoskeletal injuries by calling +44 20 7353 5678, email info@fleetstreetclinic.com or book an appointment online.
WHAT IS DIABETES?
Diabetes is a lifelong condition that occurs when the body is unable to properly regulate the amount of glucose (sugar) in your blood. Poor control of diabetes can lead to high blood sugar levels and cause long term damage to your overall health and organs.
WHAT HEALTH PROBLEMS DOES IT CAUSE?
High blood sugar levels can cause a lot of damage to your body and if not managed correctly, may lead to many diabetic complications. This will cause long term health problems, especially if they go untreated.
HOW DOES DIABETES AFFECT OTHER PARTS OF YOUR BODY?
Eyes: Retinopathy is a complication of diabetes caused by high blood sugar levels damaging the retina, often leading to vision impairment. It is the leading cause of blindness among working-age adults in the UK. As a consequence of diabetic retinopathy, swelling can take place, called diabetic macular oedema. People with diabetes are also more prone to develop cataracts and glaucoma at an earlier age, contributing to vision reduction.
Feet: Foot health is often a neglected area anyway but high blood glucose levels can lead to insensitivity in the foot and lower limbs, which means you lose the ability to feel pain and distinguish hot or cold. It can also lead to less blood supply to your feet leading to poor circulation.
Loss of sensitivity means that you may not notice if you have a minor cut, sore or wound and poor circulation means if you do get a cut or sore, it will take longer to heal and open wounds are more likely to become infected. This combination is why there is an increase in risk of amputation for those who are diabetic. Regular podiatry appointments are the best way to look after your foot health.
Heart: High blood sugar levels can also cause problems to your blood vessels which can sometimes lead to serious problems such as heart attacks and strokes.
Kidneys: High blood sugar levels creates more difficulty for the kidneys to clear waste. This may lead to Diabetic Nephropathy, the deterioration of the kidneys.
HOW CAN DIABETES BE TREATED?
There is currently no cure for diabetes, therefore, the best way to deal with diabetes is to get it properly managed and controlled. If you are diagnosed with type 1 diabetes, you must either inject or pump insulin into body to treat your diabetes. If you have type 2 diabetes, you may also have to use insulin, however, it can be managed through diet and lifestyle changes.
HOW CAN YOU TEST FOR DIABETES?
An instant HbA1c test can confirm if you’re within the recommended range, or are considered pre-diabetic or confirm that you have diabetes. Using a small blood sample it will measure how well your blood sugar has been controlled over the last 3 months and provide a numerical reading.
As the HbA1c test provides 3-months insight, it is an important blood test for diagnosed diabetics. It provides a good indication of how well they are managing their diabetes..
Many people are more familiar with the glucose blood test – it measures the concentration of glucose molecules in your blood at a single point in time. The amount of glucose in your blood could also indicate whether you could be diabetic or not. People with diabetes can also use this test to manage their condition on a daily basis alongside regular HbA1C testing.
You can book an instant HbA1C test online at a cost of £54.50.
WHAT ARE THE SYMPTOMS?
When it comes to diabetes the symptoms are not always obvious and can often go unnoticed for long periods of time before being diagnosed.
The most common symptoms include:
- Feeling constantly thirsty or dehydrated
- Unintentional loss of weight and increased appetite (type 1)
- Vision begins to blur
- Numbness in your hands or feet (type 2)
- Fatigue
- Urinating more frequently
WHO IS AT RISK?
In the UK, type 2 diabetes is the most common type of diabetes, affecting over 90% of sufferers. The symptoms of diabetes are often mild, therefore, it’s important to be aware of the risk factors that could make you more susceptible to diabetes in the future.
According to Diabetes UK, type 2 diabetes is twice more likely in people of African descent in comparison to people of European descent and six times more likely in South Asian communities, making them a high risk category in developing diabetes. Additionally, people of African – Caribbean and South Asian descent are also at risk of type 2 diabetes much earlier, usually over the age of 25. On the other hand, for Europeans the risk increases when over the age of 40. Other factors contributing to diabetes include being overweight, high blood pressure and genetics.
Other general risk factors include:
- Having high blood pressure
- Carrying extra weight around your middle
- Smoking
- Polycystic Ovary Syndrome (PCOS) sufferers
- Those with a sedentary lifestyle
- Drinking too much alcohol
- Those with disturbed sleep – this includes those who do not get enough sleep and those whose sleep too much
If you have symptoms of diabetes or general concerns about your diabetic risk, you can book a GP appointment to discuss in more detail.
Alternatively, you can book in for an instant HbA1c test with a nurse.
With monkeypox cases being recorded in over 20 countries across the globe, people are becoming increasingly concerned about its spread and transmission.
Following 2 years of the Covid-19 pandemic, this outbreak has reignited the public’s fear and uncertainty of infectious diseases.
Whilst the media coverage of the monkeypox outbreak is alarming, we would like to reassure our patients that as it stands, the risk is still very minimal and vaccination is not advised as a precautionary measure. Whilst vaccines will undoubtedly be a key part of containing the outbreak, for now, only people who may have been exposed are being offered vaccination.
Our Medical Director & Travel Medicine Specialist, Dr Richard Dawood explains;
“Lots of people have been getting in touch with us to ask about a monkeypox vaccination, but this is not available privately. It is currently only being offered to anyone identified as a direct, close contact of a confirmed case deemed to be at sufficient risk.
The current outbreak does, however, highlight the need to think about your vaccine protection more generally, whether for travel or simply to protect your health and well-being, taking advantage of the best vaccines currently available.”
In a more general sense, it is never too late to catch up on childhood vaccinations, incomplete vaccination courses or any required boosters.
Your immune system naturally decreases with age and certain diseases are also more prevalent in older adults so there may be new vaccinations which are now suitable for you to consider for preventable diseases. Some health conditions can also weaken the body’s immune response, making you more vulnerable to infectious diseases, complications and hospitalisation. Therefore, it is important to ask your GP which vaccinations would be suitable for keeping you healthy.
– For more information on wellness vaccinations.
If you are travelling soon and haven’t had a travel consultation with a travel nurse, perhaps it is time to consider one. Travel nurses are experts in travel health and will advise which travel vaccinations & medications you should consider based on the risk of where you are travelling to and your itinerary once there.
– For more information on travel consultations.
To conclude, we’d like to dismiss a couple of dangerous myths about monkeypox that are unnecessarily scaremongering the public:
Myth 1: Monkeypox is as contagious as COVID-19 or smallpox
Fact: Monkeypox is far less contagious compared to smallpox, measles, or COVID-19.Myth 2: Monkeypox is a new virus.
Fact: No, the monkeypox virus is not a novel virus. It’s a known virus and is generally seen in central and western African countries as localised outbreaks.In summary, we, like the rest of the medical field, will be keeping a close eye on the progression of the Monkeypox outbreak and should our advice change based on new information, we will update this statement accordingly.
For more information on Monkeypox.
Women today lead incredibly busy lives. They run and organise homes and build successful careers, usually all whilst taking on the majority share of caring for their children and often their older relatives. It is therefore not uncommon for women to have little or no time to look after themselves, their health included.
In addition to not making time to prioritise their health, it seems that when women do put their health first and seek medical advice, they are less likely to feel heard and supported in comparison to their male counterparts.
A recent survey by The Department of Health and Social Care found that “more than 4 in 5 (84%) women they surveyed had experienced times when they (or the woman they had in mind) were not listened to by healthcare professionals.”
Based on the data they collected, ‘not being listened to’ appears to be present at all stages of the healthcare pathway. Specifically, many women told them:
- their symptoms were not taken seriously and/or dismissed upon first contact with GPs and other health professionals
- they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years
- if they did secure a diagnosis, there were limited opportunities to discuss or ask questions about treatment options and their preferences were often ignored
Many women recalled their symptoms being dismissed upon first contact with GPs and other professionals; women felt they had to persistently advocate for themselves to secure a diagnosis, often over multiple visits, months and years; and post-diagnosis, discussions about treatment options were often limited, and some said their preferences were ignored.
To make matters worse, there is some evidence that due to historical clinical trials being disproportionately male-orientated there is much less research into women-only health concerns and assumptions have been made that similar medical treatments will work for both sexes. The top reasons for the under-representation of women in trials were the belief that hormone fluctuations could influence results and concerns that fertility could be affected. A widely accepted negative repercussion, amongst others, being that women are much more likely to experience adverse side effects of medications because drug dosages have historically been based on clinical trials conducted on men.
A combination of these factors may explain why there is a gender gap in health outcomes, with women experiencing poorer health outcomes in comparison to men. We strongly believe in equality and ensuring health is a top priority for all.
Therefore, here are the top health symptoms women should never ignore:
1) Any change in bowel habit and/ or urination
This includes blood in the stools, unexplained persistent abdominal pain, weight loss, lumps around the anus, lack of appetite, blood in the urine or increased frequency of urination. These are all reasons for seeing your doctor ASAP as these symptoms could be due to bowel, bladder or ovarian cancer. All patients should have an annual faecal occult blood (FOB) test to exclude bowel cancer, which has increased in incidence in the UK for reasons unknown. Or if you are looking for a more in-depth investigation, you should request a colonoscopy which entails looking at the bowel with a colonoscopy. This is the gold standard, but an FOB is the next best thing and far less invasive as a first investigative option. It takes no time at all and is a good preventative check.
2) Any changes to the breast.
Any breast lumps, skin changes, nipple discharge, nipple changes or pain in the breast must be checked ASAP. Breast cancer is the most common type of cancer in the UK and often can present insidiously. Get to know what your breast feels like so that any subtle changes can be detected as early as possible.
3) Skin lesions that do not heal.
Any scab on the skin which does not heal, especially around the eyes, nose, ears and face should be checked. All these areas are the most sun-exposed, and, as such, are more at risk of skin cancer. If these lesions are picked up and treated early, scarring is minimal, but if left, then disfiguring scars and skin grafts may be necessary.
4) Bleeding after the menopause.
If you experience any bleeding after 1-year of your last menstrual period, you must visit your GP for further investigation. Bleeding after the menopause is not common and could be an indicator of cancer of the uterus, or the cervix. They will usually opt for a biopsy of the uterine lining to exclude both – don’t worry, this doesn’t hurt.
5) Always have regular cervical screens.
Most people don’t find cervical screens painful, although they can feel somewhat uncomfortable. If you are concerned about the pain or you have previously found the procedure painful with the NHS, you can opt to book a private appointment. It is important that you don’t miss your appointment.
6) Bleeding between periods.
At any age, you should never ignore bleeding between periods or after intercourse, as this can be a sign of cervical or uterine cancer. Whilst cervical cancer is monitored by regular screening, it is important to still get bleeding between periods checked out following a normal smear result. Cancer of the endometrium is becoming increasingly common in women who have not had children.
7) A persistent cough.
Regardless of gender, you should get a persistent cough checked out by your doctor, especially if you are coughing up discoloured sputum or blood.
8) Any unexplained changes to your body.
Any new indigestion, shortness of breath on exertion, neck or left arm pain requires follow up ASAP. Make sure a GP examines your chest and makes the appropriate investigations.
The same applies to calf pain or any pain in the chest. By taking a full history, examining you and doing quick and easy investigations, worrying conditions can be excluded, such as a pulmonary embolism or a heart attack.
Some recent examples of cases where other healthcare providers have failed our new female patients:
1) We saw a 36 year old who had not had a cervical screening for 5-years because the last one was so painful. The NHS advises a screening every 3-years but we advise yearly screenings to ensure any abnormalities are found as early as possible. 5-years is far too long!
2) We saw a woman who had a suspicious lump at her anal margin, which her usual GP had told her was part of her bladder. She wanted a second opinion because it had grown in size and was now painful. The patient was referred for an urgent assessment to exclude cancer.
3) We saw an 88 year old patient who was disfigured by a large basal cell carcinoma on her forehead, about which she was embarrassed. The patient had been seen by a dermatologist who had frightened her about having the lesion removed by saying she might not survive an anaesthetic. The patient wished that she had taken the risk and asked to be referred back, as the skin lesion was disfiguring and ruining her quality of life.
** The outcomes of these patients are yet unknown, but they are all certainly serious health concerns that should have been properly addressed long before now.
We want to encourage women to take ownership over their health and be assertive when they feel that something has changed from our normal. If they feel like they are not being taken seriously or not being heard, they should seek a second opinion.
If you cannot get an appointment with your usual GP or through the NHS, rather than waiting for weeks and worrying about what it could be, make an appointment with a private GP who can usually see you on the same day!
Put your mind at ease with private healthcare.
Ageing is an inevitable part of living. As we age, many physical and psychological changes affect our overall health and these vary from person to person.
The general myth is that as you age, you become more fragile and that this is unavoidable. This is most certainly not the case. There are always things we can do to help keep healthy in our older years and these changes can slow down or even prevent certain health conditions from developing.
The term “fragile” is defined as not “strong or sturdy; delicate and vulnerable” and is most often used to describe older ladies. One particular age-related health issue that supports this description would be osteoporosis.
Osteoporosis is a degenerative disease that weakens and thins the bones which makes them fragile and more likely to break and is becoming increasingly common. It is much more prevalent in women than men due to the menopause directly affecting hormone balances and this directly affects bone density. It is important to prevent osteoporosis as we age as 75% of fractures due to osteoporosis occur in people aged 65 and over.
There are several things you can do to help prevent osteoporosis:
1) Do regular, weight bearing physical activity.
The lack of regular exercise will result in loss of bone and muscle, so adults who are inactive are more likely to have a hip fracture than those who are more active. Adults should aim to do at least two and a half hours of moderate-intensity exercise every week. Weight bearing and resistance training are a particularly great way of improving bone density and helping to prevent osteoporosis.
2) Eat plenty of calcium and Vitamin D containing foods.
Your diet is very important and the nutrients we get from the food we consume will affect how strong our body is. Eat plenty of dairy, seeds, eggs, oily fish, protein, fruit and vegetables. Additionally, try to get at least 15-minutes of sun exposure per day to increase your Vitamin D intake. As we know in the UK, such sun exposure is not always possible during the winter months and, if this is the case, taking a daily Vitamin D supplement is advised.
3) Maintain a healthy weight.
As you get older, you start to lose lean body mass like muscle and bone density and this can start to happen yearly from the age of 30. Being underweight weakens your bones so it is important to keep your weight in a healthy range. A good indication, although not exact, is your BMI. For most adults, a healthy BMI range is between 18.5 and 24.9, so try not to let your BMI fall below 19.
Those who suffer from eating disorders such as anorexia and bulimia are at a higher risk of fragility due to the conditions causing further bone density loss. This can happen to anorexic and bulimic sufferers of all ages.
Older people should aim to consume a varied diet, consisting of enough calories for maintaining a healthy weight.
4) Limit your consumption of alcohol.
We’d recommend that you drink no more than a maximum of 2 units of alcohol per day. Any more than this has been demonstrated to increase the risk of bone fracture. Alcohol abuse has detrimental effects on bone health and increases a person’s risk of developing osteoporosis.
5) Stop smoking and definitely don’t start!
Smoking is a known risk factor for osteoporosis as it increases bone mass loss. In fact, smoking doubles the risk of hip fracture.
Generally, being healthy is the key to avoiding fragility and in particular preventing osteoporosis as we age. Having an annual health medical can highlight any areas of concern. They can monitor the progression of any pre-existing health issues, as well as detect arising conditions in the early stages. You can book your annual medical online
In addition to making healthy lifestyle choices, it is also important to book a doctor’s appointment should you notice any changes to your health. The sooner a health concern is addressed, the easier it is to treat. You can book a GP appointment online.
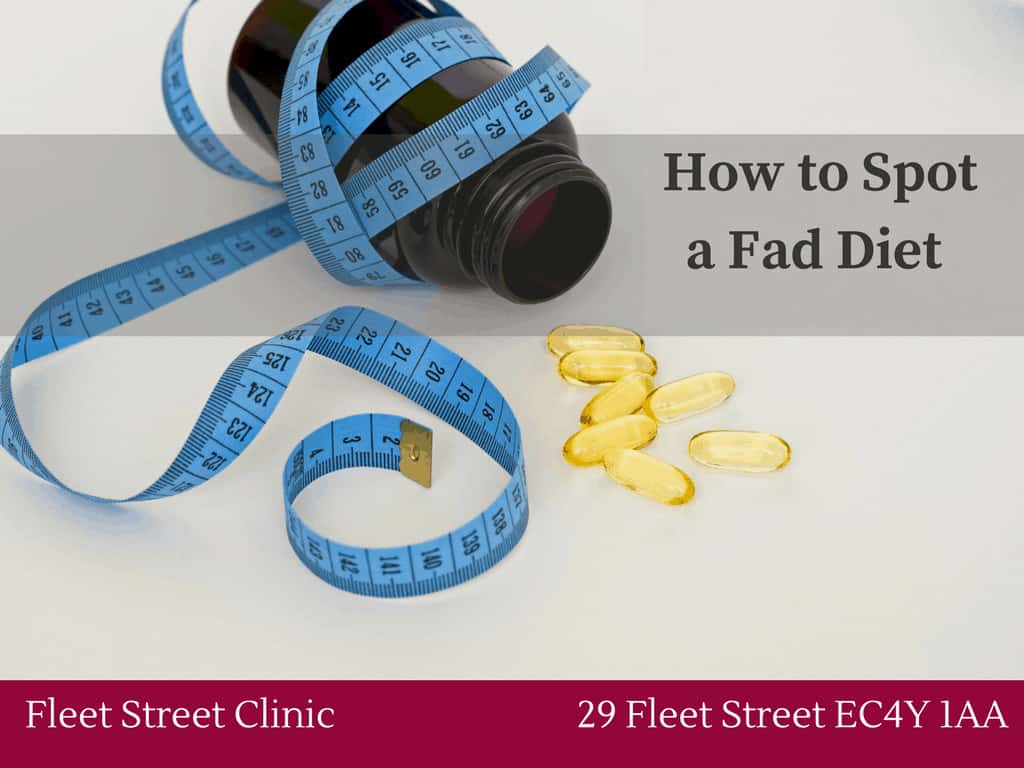
Weight loss has become a thriving industry and we’re bombarded constantly with unhealthy FAD diets, weight loss programmes, influencers selling teas and pills all promising to help us lose weight. Many of these are promoting quick fixes which are not advised by doctors or dieticians. It can be really hard to know what information to trust. To help navigate the sea of information (and misinformation!) surrounding weight loss, we have asked one of our GPs, Dr Belinda Griffiths, and our dietitian, Ruth Kander, their advice on how to lose weight safely and successfully.
Firstly, it is important to note that weight loss should be consistent and gradual as it can be dangerous to lose too much weight too quickly. Dr Griffiths suggests that “a safe weight loss is 1-2 lbs or 0.5-1kg per week… Greater weight loss than this per week can lead to malnutrition, exhaustion, increased risk of gout and gallstones.” There is also an increased risk of developing an unhealthy relationship with food which, in extreme circumstances, could lead to eating disorders.
Ruth added, “Losing weight gradually and at a healthy rate is key.” Remember, it’s all about consistency! Perseverance will amount to healthy lifestyle changes which will allow you to achieve your weight loss goal.
Don’t underestimate diet
Both Dr Griffiths and Ruth agree that diet is the most important factor when it comes to weight loss. As Ruth explains; “having a healthy balanced diet that is lower in calories than our body uses is a good way to start the weight loss journey. If we don’t reduce calorie intake, one won’t lose weight:.” – this is known as being in a calorie deficit. The amount of calories that will result in weight loss will vary from person to person and depend on the amount of exercise the individual does. In order to lose weight, you will need to burn more calories than are consumed and therefore restricting your calorie intake is the simplest way of losing weight.
Foods to focus on
Ruth recommends that “people should focus on a variety of foods when trying to lose weight”. While Dr Griffiths suggests, “focusing on a range of lean proteins (including meat and fish), vegetables, high fibre foods (such as quinoa, bran flakes etc) and fruit in moderation”. Vegetarians can substitute in lentils, nuts, beans and tofu instead of meat and fish. In general, high calorie foods such as fried food, cakes, biscuits, chocolate and sugary drinks should be avoided.
Let’s get physical!
Although weight loss is still achievable without much exercise, incorporating exercise into your lifestyle will not only aid weight loss, but will generally improve your overall health. Any exercise is better than none whether it be tennis, swimming, or even walking, “whatever you are capable of, just do it!” is Dr Griffiths advice. Ideally, a combination of exercise is best for weight loss – this includes cardio / fat burning and resistance or weight training. Get those steps in! An easy way to incorporate more exercise into your daily routine is by aiming to walk at least 10,000 steps per day. This easy change can make a big difference and remember, as Dr Griffiths says “the more exercise you do, the greater calories are burned” – it’s as simple as that!
Don’t forget about NEAT movements!
NEAT (or Non-exercise activity thermogenesis) movement refers to the physical movement we do day-to-day that isn’t necessarily planned exercise and “encompasses the energy that we expend by simply living”.This includes the calories we burn breathing, eating, sleeping etc. Dr Griffiths suggests that “you can increase NEAT movement easily in your everyday life by making simple changes such as taking the stairs rather than the lift, by standing rather than sitting, by walking instead of taking the train/ bus/ tube or even by carrying bags rather than having items delivered”. It all adds up! These simple swaps will increase the number of calories you burn and help facilitate weight loss.
What to do when you plateau
The first stint of weight loss can make it seem a little too easy as you tend to lose weight more easily in the beginning, but a common issue lots of people face is when weight loss reaches a plateau. This is where you stop losing weight to the same extent you were before, or stop losing weight for a period of time. This can feel disheartening and more often than not, people tend to give up at this stage. Dr Griffiths states at this point “it is a case of persevering with calorie restriction and regular exercise and gradually weight loss will resume.” If it doesn’t, Ruth suggests “ looking at what you’re eating to see if anything has slipped”. She states “maybe you’re not taking into consideration extra calories here and there” but they all add up. See if there are any areas of your diet where you could be a little stricter, or consider starting or upping your exercise.
Sleep and Stress
A good night’s sleep and keeping your stress levels down will be your friend when it comes to weight loss. “In order to lose weight, you need to be in the correct frame of mind and life circumstances” says Ruth. Research has shown that you tend to eat more and make poorer food choices, including seeking comfort food, when you are sleep deprived. This is because not getting enough sleep “disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite” says Dr Griffiths.
Stress can also play a part in weight loss as Dr Griffiths explains that “stress increases cortisol levels which increases gastric acid output and makes you feel anxious and hungry”. Ruth adds “there is also a theory that being stressed can limit weight loss in terms of hormonal activity in the hypothalamic-pituitary axis which can lead to the release of hormones that can limit weight loss”. Keeping it simple, “to lose weight, good sleep and minimal stress would be ideal”.
Final thoughts
Trying to lose weight can seem complicated, confusing and difficult, but when you really break it down, the ingredients to losing weight successfully are actually very straightforward. If you stick to these simple rules and you are patient and consistent, the weight will come off and you will achieve your goals.
If you feel that you are doing everything right and you still aren’t losing weight, or are even putting weight on, there could be something else causing this. You may have an undiagnosed underlying medical condition and we’d advise you to visit your GP to make sure everything is well.
If you would like any extra support with your weight loss, why not book an appointment with Ruth. Or if you have any concerns over your health, please book an appointment with one of our GPs.
Most people experience fluctuations with their weight and it is common to gain weight naturally as we age. For the most part, diet changes, eating more or reducing exercise are the main causes for gaining weight. However, if a person gains weight in a short period of time for no reason, this could be the sign of an undiagnosed, underlying health condition. There are several conditions and circumstances that are known to cause weight gain, some of which can be serious and require medical attention.
Here are just some medical conditions which can cause sudden weight gain:
Polycystic ovary syndrome (PCOS)
This is a hormonal condition which affects the way a woman’s ovaries work. A common symptom of PCOS is weight gain, particularly around one’s middle. Weight gain is rarely the sole symptom, it is usually part of multiple symptoms including acne, excessive hair, irregular periods and/ or thinning hair. PCOS makes women less sensitive to insulin or cause insulin-resistance which can lead to weight gain and secondary conditions such as diabetes.
Hypothyroidism
A common cause of unexplained weight gain in men and women comes from having an underactive thyroid. This is because when a thyroid is underactive it doesn’t produce enough thyroid hormones, which in turn affects your metabolism, slowing it down. Hypothyroidism can be diagnosed with a thyroid function test and if diagnosed, it can be easily treated with a replacement hormonal tablets.
Cushing’s syndrome
This is a rare hormonal disorder which is caused by elevated levels of cortisol in the body. Cortisol is responsible for regulating metabolism and appetite, which means elevated levels can slow down your metabolism as well as increase hunger, both of which can cause weight gain.
Insomnia / chronic lack of sleep
Being sleep deprived can result in making poor food choices, including seeking unhealthy foods and eating more than usual. This is thought to be because a lack of sleep disrupts the hormones in the brain (Leptin and Ghrelin) that are responsible for appetite.
Medication
Certain medications affect metabolism which can cause weight gain and weight loss. Medications such as steroid medication can cause weight gain, bloating and swelling due to water retention.
Lipoedema
This is a problem caused by an issue with the lymphatic system that causes an abnormal build-up of fat in the legs and sometimes the arms. This usually results in the upper body being generally a much smaller size compared to the lower half of the body but typically affects both sides of the body equally. This condition can also be painful and cause tenderness or heaviness in the limbs. Lipoedema mainly affects women and it is rare in men.
Chronic stress, depression and/ or anxiety
Mental health issues can sometimes cause people to turn to food as a coping mechanism, often triggering compulsive eating behaviours. Additionally, higher cortisol levels are often found in people with depression which is known to increase appetite and the motivation to eat. Antidepressant medication can also increase hunger as they interfere with serotonin levels – a neurotransmitter that regulates appetite.
Menopause
Women going through the menopause often experience weight gain. Changing hormone levels affect the way the body stores fat and can cause women’s bodies to store, rather than burn, calories. Women also generally need less calories after the menopause, and so, if you do not adjust your calorie intake, you are likely to put on weight.
PMS
During PMS (premenstrual syndrome), progesterone levels surge and dip which are known to increase appetite (the cause of which are unknown). PMS can also cause weight gain as a result of water retention.
While many of these causes are rare, they are possible and anyone experiencing unexplained weight gain should visit their GP to rule out anything that may require medical care or treatment. It’s always best to be on the safe side! And if everything is normal, your GP can provide you with tips and advice on how to manage your weight gain.
If you are experiencing unexplained or sudden weight gain, or think you might be displaying symptoms of the conditions mentioned above, please book a GP appointment today.
Sleep is one of our greatest allies when it comes to health and wellbeing. It is associated with a number of health benefits which can have a huge positive impact on our daily lives.
Conversely, a lack of sleep can be detrimental – research has even found that not getting enough sleep can negatively impact some aspects of brain function to a similar degree as alcohol intoxication!
Dr Belinda Griffiths discusses some of the mental and physical health benefits of getting a good night’s sleep.
Immune System
During sleep, your body releases cytokines, which are essential for the regulation of the immune system. Cytokines are required in increased amounts when you are attacked by a pathogen (when you’re ill) or under stress. The level of cytokines increases during sleep, and therefore lack of sleep hinders the body’s ability to fight infections. This is also the reason why the body tends to sleep more while suffering from an infection.
Weight Control
When you’re well-rested, you’re less hungry. Being sleep deprived disrupts the hormones in your brain (Leptin and Ghrelin) that control appetite.
With those out of balance, your resistance to the temptation of unhealthy foods goes way down. And when you’re tired, you’re less likely to want to get up and move your body. Together, it’s a recipe for putting on the pounds!
Athletic Achievement
If your sport requires quick bursts of energy, like wrestling or weightlifting, sleep loss may not affect you as much as endurance sports like running, swimming, and biking. But you’re not doing yourself any favours. Besides robbing you of your energy and time for muscle repair, lack of sleep saps your motivation, which is what gets you across the finish line. You’ll face a harder mental and physical challenge – and see slower reaction times. Proper rest sets you up for your best performance.
Memory
When you’re tired, you can have difficulty recalling information. That’s because sleep plays a big part in both learning and memory. Without sufficient sleep, the brain finds it difficult to focus and take in new information in the first place and then doesn’t have enough time to properly store information as short-term memories. Sleep helps enable you to retain memories and store information.
Sleep also allows for your mind to rest, repair and rebuild, the same way it does for your body. As you sleep, your brain begins to organise and process all the information you’ve taken in during the day. It converts these short-term memories into long-term memories – this helps you to learn.
Concentration
Not sleeping properly can mean that both your body and brain don’t function properly the next day. It can impair your attention span, concentration, strategic thinking, risk assessment, reaction times and problem-solving skills. This is particularly important if you have a big decision to make, are driving, or are operating heavy machinery. So, getting plenty of sleep can help you stay sharp and focused all day long.
Mood
Another thing your brain does while you sleep is process your emotions. Your mind needs this time in order to recognise and react in the right way. When you cut that short, you tend to have more negative emotional reactions and fewer positive ones. Lack of sleep can cause bad temper and anxiety, so the better you sleep, the better your ability to stay calm, controlled and reasonable.
Chronic lack of sleep can also raise your chance of having a mood disorder. One large study found that people with insomnia were five times more likely to develop depression, and the odds of having anxiety or panic disorders are even greater.
A refreshing slumber helps you hit the reset button on a bad day, improve your outlook on life, and be better prepared to meet the challenges of the next day.
Heart Health
While you sleep, your blood pressure goes down giving your heart and blood vessels a bit of a rest. The less sleep you get, the longer your blood pressure stays up during a 24-hour cycle. High blood pressure can lead to heart disease and strokes. Therefore, it is important to keep your blood pressure down.
Pain Threshold
Poor sleep and pain mutually reinforce each other. Sleep deprivation increases pain sensitivity and reduces pain tolerance. Therefore, something will feel more painful when you’re tired.
It is clear that sleep is an essential part of helping us stay physically and mentally healthy. What better excuse to have a few extra hours of sleep a day!
If have any concerns about your health, book a GP appointment today.
THE WORLD HEALTH ORGANISATION (WHO), HAS REPORTED THAT POPULATION EXPOSURE TO HEAT IS INCREASING DUE TO CLIMATE CHANGE.
The WHO states, ‘global temperatures and the frequency and intensity of heatwaves will rise in the 21st century as a result of climate change’. Extended periods of heat exposure during the day and night time can increase the amount of physiological stress on the human body.’
The stress caused by heat exposure exacerbates the top causes of death globally. This includes respiratory and cardiovascular diseases, diabetes mellitus and renal disease.
They go on to state, ‘Exposure to excessive heat has wide-ranging physiological impacts for all humans, often amplifying existing conditions and resulting in premature death and disability.’
With the temperature said to continue rising, the WHO also states, ‘Awareness remains insufficient of the health risks posed by heatwaves and prolonged exposure to increased temperatures.’
So, who is most affected by heat exposure and how will it impact your health?
Who is affected?
Rising temperatures affect the whole population. However, some populations are more vulnerable to exposure to excessive heat. Those include:
- Elderly people
- Infants and children
- Pregnant women
- Outdoor and manual workers
- Athletes
- Poorer communities
How does heat impact health?
With rapid increases in external temperatures, the body will struggle to regulate our internal temperatures. The knock-on effect of this can result in a number of heat-related illnesses such as heat cramps, heat exhaustion, heatstroke, and hyperthermia. Reported small differences in the seasonal changes have been reported to have increased the number of heat-related illness and even death. Rising temperatures can also worsen chronic conditions such as cardiovascular, respiratory, and cerebrovascular disease and diabetes-related conditions.
What actions can you take to stay cool?
- Aim to keep your living space cool. WHO suggests ‘below 32 °C during the day and 24 °C during the night’
- If it is safe, open your windows at night time to cool your living space.
- Stay out of the heat by staying in the shade and avoiding going outside during the hottest part of the day.
- Take cool showers and wear loose-fitting clothing.
- Drink regularly and avoid alcohol and caffeine.
- Check on vulnerable family members who may be affected by the heat.
What to do if someone shows signs of a heat emergency?
It is extremely important to know what to do when someone is showing signs of heat illness. Everyone should know how to respond to heat emergencies, this can be learnt in first aid courses.
If one of your family members or someone you assist is showing signs of hot dry skin and delirium, convulsions and/or unconsciousness, call a doctor/ambulance immediately.
Whilst you are waiting for help to arrive place them in a cool place in a horizontal position and elevate their legs. It is now important to initiate external cooling.
This can be done by:
- Removing clothing
- Placing cold packs on the neck and groin
- Spraying cool water on their skin
- Fanning them
- If they are unconscious, place them on their side
If you or someone you are with is displaying mild signs of heat illness that is not considered an emergency, you might want to consider a same-day GP appointment. You can book an appointment online.